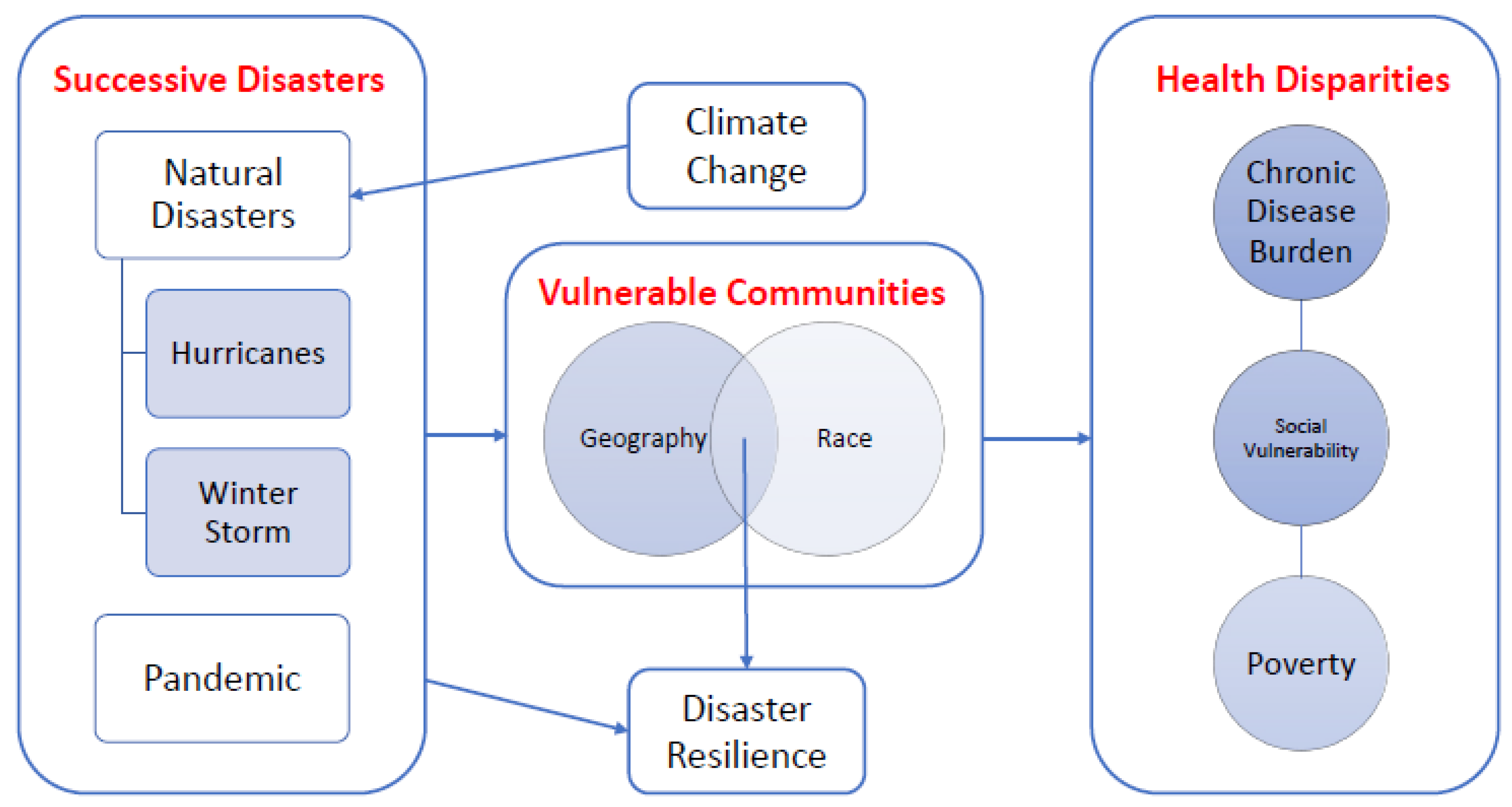
Health Disparities and Climate Change: The Intersection of Three Disaster Events on Vulnerable Communities in Houston, Texas
Abstract
:1. Introduction
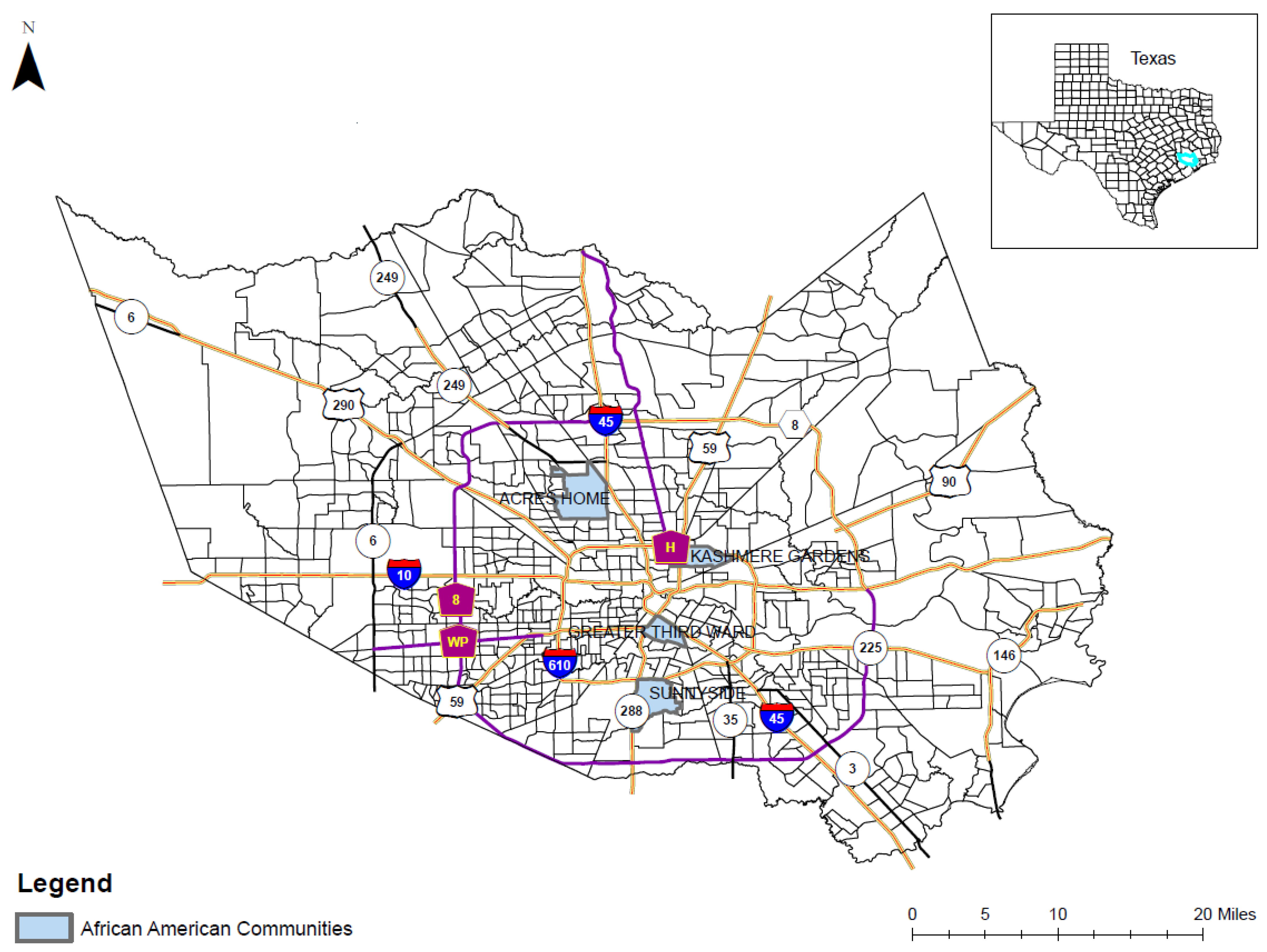
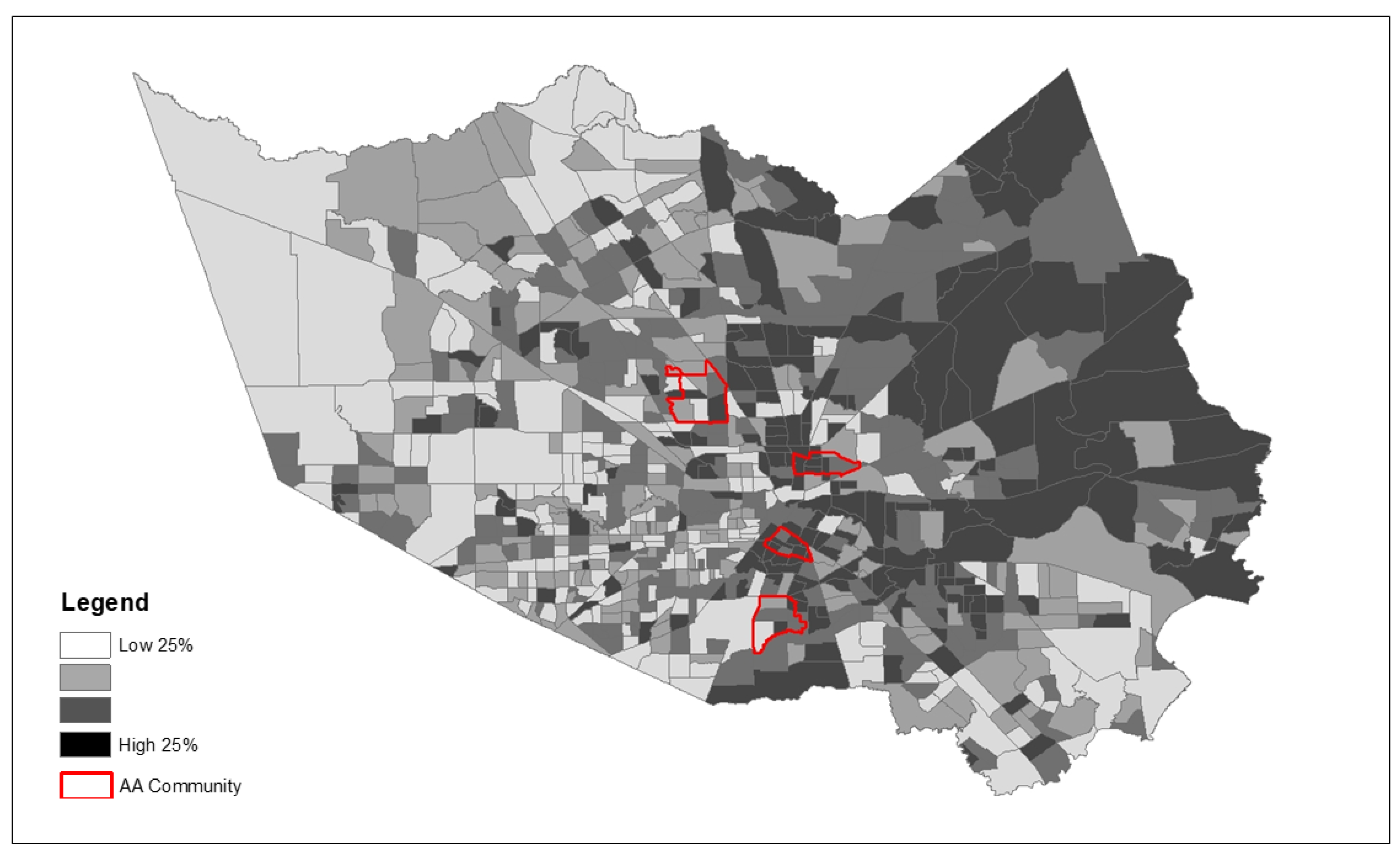
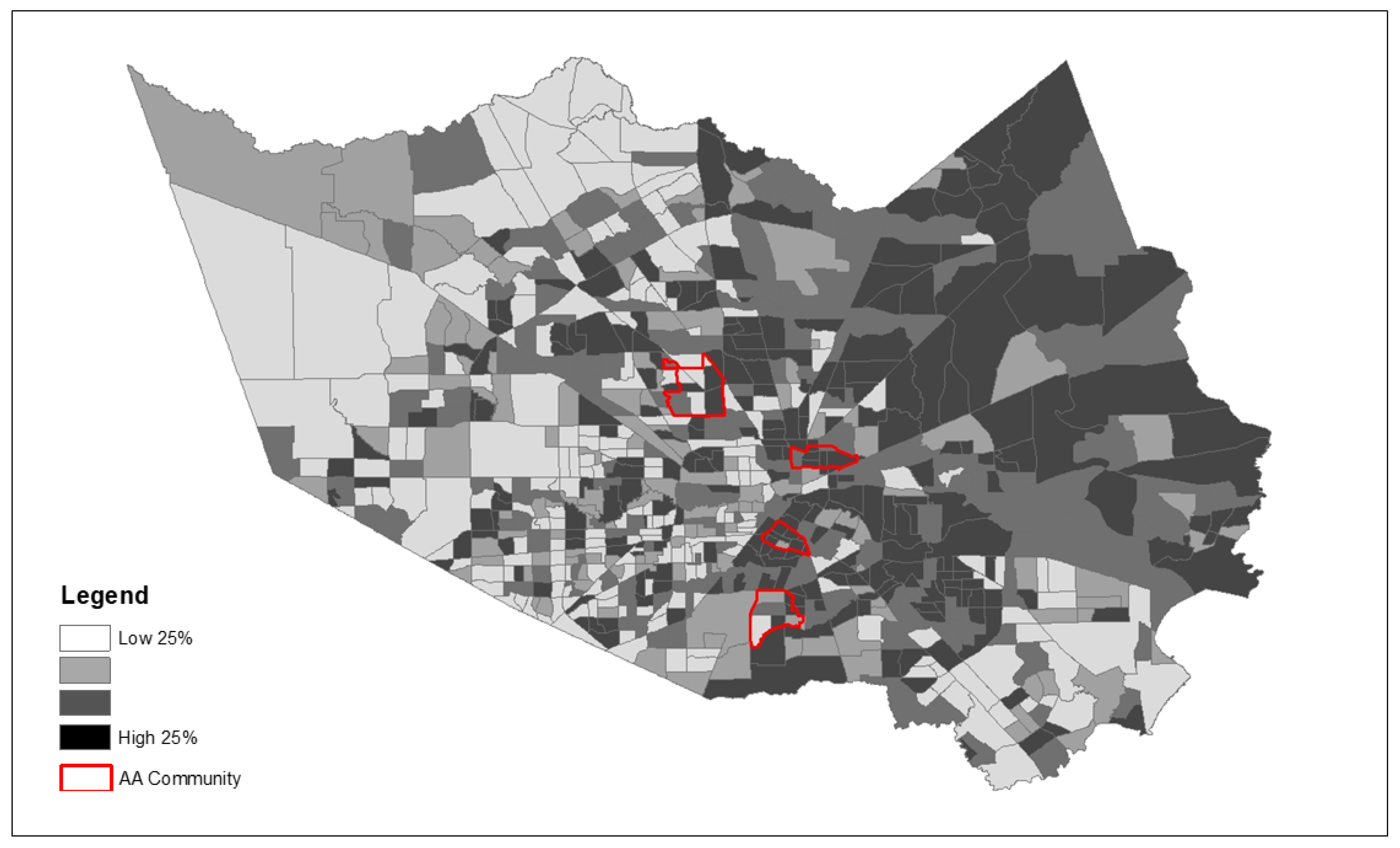
2. Methodology
2.1. Qualitative Design and Eligibility
2.2. Qualitative Procedures and Analysis
3. Results
“(Hurricane) Harvey prepared me better. Harvey prepared me mentally and physically better (for the winter storm).”(Participant L).
“Harvey prepared us because we were already in disaster mode and how do we take care of this and how do we take care of our families and make sure we are prepared next time. In the ice storm, as soon as they made the weather reports and projects, it was like ‘make sure these things are done’—fill tank, fill tub just like a hurricane. I had charged all devices, and I charged the chargers, and I already had candles and I have flashlights. Same prep for a hurricane you did for the ice storm.”(Participant C).
“We have to stay prepared. It could happen tomorrow or in a couple of months, we just have to stay prepared.” (Participant D). Another participant further emphasized this point. “Disasters and emergencies can be anything, it doesn’t have to be a pandemic or ice storm. Just naturally always being prepared.”(Participant B).
“We know now that if something is coming, not to wait until the last minute, not to wait until everybody is in the store grabbing things off the shelves. As soon as you hear of something you, you go and make your preparations.”(Participant C).
“We need to check on the elders more. There were people that have been found since the thaw, who were just dead at home and people were not aware of that. If someone had said ‘we haven’t heard from him and the power is out’ but then nobody went to check and the person was already frozen to death (…). That was during this (winter storm) but even during COVID, I think we need to check (on each other) more frequently because anything can happen and we shouldn’t go days (without) talking to them.”(Participant L).
“We need to start talking about things that we can do, and think about others all the time, always thinking about how we can better help others survive this. Because we may be doing ok, but somebody else may not.”(Participant L).
“Because I was prepared in the sense that I could help my son who was in his apartment without power for four days.”(Participant P).
“When (Hurricane) Harvey came, I got lucky and bought a generator. (…) So I had a generator when this thing (the winter storm) happened so that helped us tremendously. (…) I charged my next-door neighbor’s battery with the generator.”(Participant C).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leighton, H. Not Only Is Houston Getting More Diverse, But Residents’ Households Are, Too; Rice Kinder Institute for Kinder Research: Houston, TX, USA, 2019. [Google Scholar]
- City of Houston. City of Houston, Texas. Available online: https://www.houstontx.gov/abouthouston/houstonfacts.html (accessed on 15 October 2021).
- United States Census. Quick Facts: Houston City, Texas. Available online: https://www.census.gov/quickfacts/houstoncitytexas (accessed on 15 October 2021).
- Cooper, R. Poverty in Texas: Million Texans Live in Poverty; The Center for Public Policy Priorities: Austin, TX, USA, 2019. [Google Scholar]
- Understanding Houston. Understanding Disasters in Houston; Understanding Houston: Houston, TX, USA, 2020. [Google Scholar]
- Davidson, T.M.; Price, M.; McCauley, J.L.; Ruggiero, K.J. Disaster impact across cultural groups: Comparison of Whites, African Americans, and Latinos. Am. J. Community Psychol. 2013, 52, 97–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lozano, J.A. 3 Years after Harvey, Some in Houston Still Waiting for Help. Available online: https://apnews.com/article/virus-outbreak-ap-top-news-tx-state-wire-us-news-c3e84ee0327c293bf167d818c8b25f7d (accessed on 7 September 2021).
- Schwartz, R.M.; Tuminello, S.; Kerath, S.M.; Rios, J.; Lieberman-Cribbin, W.; Taioli, E. Preliminary assessment of Hurricane Harvey exposures and mental health impact. Int. J. Environ. Res. Public Health 2018, 15, 974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, R. Survey: One Year after Hurricane Harvey, 3 in 10 Affected Texas Gulf Coast Residents Say Their Lives Remain Disrupted; Kaiser Family Foundation: San Francisco, CA, USA, 2018. [Google Scholar]
- Hamel, L.; Wu, B.; Brodie, M.; Sim, S.-C.; Marks, E. An Early Assessment of Hurricane Harvey’s Impact on Vulnerable Texans in the Gulf Coast Region: Their Voices and Priorities to Inform Rebuilding Efforts; Kaiser Family Foundation: San Francisco, CA, USA, 2017. [Google Scholar]
- George, C. Texas Studying COVID-19′s Uneven Impact on Communities of Color; Texas Medical Center: Houston, TX, USA, 2020. [Google Scholar]
- O’Brien, R.; Neman, T.; Seltzer, N.; Evans, L.; Venkataramani, A. Structural racism, economic opportunity and racial health disparities: Evidence from US counties. SSM-Popul. Health 2020, 11, 100564. [Google Scholar] [CrossRef] [PubMed]
- Odoms-Young, A.M. Examining the impact of structural racism on food insecurity: Implications for addressing racial/ethnic disparities. Fam. Community Health 2018, 41, S3. [Google Scholar] [CrossRef] [PubMed]
- Heguehag, N. Minorities Confronting Environmental Racism through the Furtherance of Environmental Justice Movement in the United States. Master’s Thesis, University of Guelma, Guelma, Algeria, 2019. [Google Scholar]
- Watson, K.P.; Buttorff, G.; Cross, R.; Granato, J.; Jones, M.P.; Pinto, P.M.; Sipole, S.; Vallejo, A. Winter Storm 2021 and the Lifting of COVID-19 Restrictions in Texas; University of Houston: Houston, TX, USA, 2021. [Google Scholar]
- Dexheimer, E. The Hidden Costs of Texas’ Deadly Winter Storm for Taxpayers. Available online: https://www.houstonchronicle.com/politics/texas/article/winter-storm-uri-hidden-costs-taxpayers-texas-16255974.php (accessed on 10 September 2021).
- Dobbins, J.; Tabuchi, H. Texas Blackouts Hit Minority Neighborhoods Especially Hard. Available online: https://docs.house.gov/meetings/IF/IF03/20210218/111210/HHRG-117-IF03-20210218-SD004.pdf (accessed on 10 September 2021).
- Trovall, E.; Vasquez, L. Racial Inequities Emerge As Houston Recovers From Last Week’s Winter Storm. Available online: https://www.houstonpublicmedia.org/articles/news/weather/2021/02/22/391862/as-houston-area-folks-recover-from-the-winter-storm-racial-inequities-emerge/ (accessed on 10 September 2021).
- Frank, T. Flooding Disproportionately Harms Black Neighborhoods; Scientific American: Houston, TX, USA, 2020. [Google Scholar]
- Funes, Y. Survey Reveals Hurricane Harvey Hit Blacks and Latinos Hardest; Gizmodo: Houston, TX, USA, 2017. [Google Scholar]
- World Meteorological Organization. Weather-Related Disasters Increase Over Past 50 Years, Causing more Damage but Fewer Deaths; World Meteorological Organization: New York, NY, USA, 2021. [Google Scholar]
- Houston Chronicle. Ethnicity: City of Houston Super Neighborhood; Houston Chronicle: Houston, TX, USA, 2017. [Google Scholar]
- Centers for Disease Control and Prevention. PLACES Census Tract Data 2020 Release; USA Center for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion: Atlanta, GA, USA, 2020.
- Thakur, B.; Dubey, P.; Benitez, J.; Torres, J.P.; Reddy, S.; Shokar, N.; Aung, K.; Mukherjee, D.; Dwivedi, A.K. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci. Rep. 2021, 11, 1–13. [Google Scholar]
- Wang, B.; Li, R.; Lu, Z.; Huang, Y. Does comorbidity increase the risk of patients with COVID-19: Evidence from meta-analysis. Aging (Albany NY) 2020, 12, 6049. [Google Scholar] [CrossRef] [PubMed]
- Menard, L.A.; Slater, R.O.; Flaitz, J. Disaster preparedness and educational attainment. J. Emerg. Manag. 2011, 9, 45–52. [Google Scholar] [CrossRef]
- Services, T.D. 2016 Heart Disease and Stroke Fact Sheet; Office of Surveillance, Evaluation, and Research: Austin, TX, USA, 2016.
- Duddu, V. Prevalence of Obesity among Adults, by Demographic Characteristics, Risk Factors/Comorbid Conditions, and Place of Residence, Texas, 2018; Texas Health and Human Services: Austin, TX, USA, 2018.
- Services, T.H. Texas Behavioral Risk Factor Surveillance System; Texas Department of State Health Services: Austin, TX, USA, 2020.
- Harris County Texas. Harris County- City of Houston COVID-19 Data Tracking; Harris County Public Health: Houston, TX, USA, 2021.
- Dart, T. Houston Fears Climate Change will Cause Catastrophic Flooding: ‘It’s not If, It’s When’; The Guardian: Warrendale, PA, USA, 2017. [Google Scholar]
- Watson, K.; Cross, R.; Granato, J.; Jones, M.P.; Murray, R.; Pinto, P.M.; Stein, R.; Wong, S.M.C. Hurricane Harvey: Three Years Later; University of Houston School of Public Affairs: Houston, TX, USA, 2020. [Google Scholar]
- Srikanth, A. Texas Blackouts Disproportionately Affect Low-Income, Nonwhite Communities; The Hill: Washington, DC, USA, 2021. [Google Scholar]
- Chae, M.; Adepoju, O. Racial Disparities in COVID-19 Cases across Zip Codes in Harris County. Available online: https://web.s.ebscohost.com/ehost/pdfviewer/pdfviewer?vid=1&sid=29ff6c9d-14e1-4a5b-ace8-4377571eeb12%40redis (accessed on 12 September 2021).
- Olshansky, S.J.; Antonucci, T.; Berkman, L.; Binstock, R.H.; Boersch-Supan, A.; Cacioppo, J.T.; Carnes, B.A.; Carstensen, L.L.; Fried, L.P.; Goldman, D.P. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff. 2012, 31, 1803–1813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adepoju, O.E.; Ojinnaka, C.O. County-Level Determinants of COVID-19 Testing and Cases: Are there Racial/Ethnic Disparities in Texas? Popul. Health Manag. 2021, 24, 589–594. [Google Scholar] [CrossRef] [PubMed]

| Harris County | Kashmere Gardens | Sunnyside | Acres Home | Third Ward | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| COVID-19 Risk Factors | ||||||||||
| Population Age > 65 (%) | 12.1 * | 5.2 | 13.3 | 3.1 | 13.4 | 5.3 | 11.5 | 4.5 | 10.5 | 6.8 |
| Smoking (%) | 20.2 ** | 4.9 | 23.0 | 1.4 | 21.7 | 5.3 | 19.7 | 4.7 | 16.9 | 5.9 |
| Obesity (%) | 43.7 ** | 6.2 | 47.5 | 1.7 | 46.0 | 6.9 | 42.6 | 6.4 | 39.5 | 9.3 |
| Hypertension (%) | 40.3 ** | 5.5 | 44.8 | 4.4 | 43.7 | 9.6 | 38.5 | 6.4 | 35.0 | 12.4 |
| Diabetes (%) | 18.7 ** | 4.0 | 22.5 | 1.7 | 20.1 | 5.8 | 17.5 | 4.4 | 14.9 | 7.3 |
| Cancer (%) | 5.3 | 1.4 | 5.5 | 0.5 | 5.5 | 1.2 | 5.5 | 1.0 | 4.5 | 1.6 |
| Stroke (%) | 5.4 ** | 1.1 | 6.5 | 0.9 | 6.2 | 2.1 | 4.8 | 1.4 | 4.2 | 1.6 |
| Coronary Heart Disease (%) | 7.9 ** | 1.7 | 9.6 | 0.8 | 8.5 | 2.6 | 7.6 | 1.4 | 6.1 | 3.0 |
| Chronic Obstructive Pulmonary Disease (%) | 8.1 ** | 1.8 | 9.7 | 0.9 | 8.9 | 2.9 | 7.8 | 1.7 | 6.2 | 3.0 |
| Asthma (%) | 11.0 ** | 1.2 | 11.4 | 0.8 | 11.8 | 1.8 | 10.5 | 1.6 | 10.6 | 2.0 |
| Chronic Kidney Disease (%) | 4.2 ** | 0.8 | 4.9 | 0.4 | 4.6 | 1.3 | 3.9 | 0.8 | 3.4 | 1.5 |
| Non-Hispanic African American (%) | 12.1 * | 79.5 | 80.0 | 65.1 | 64.6 | |||||
| Standardized Mortality Ratio (SMR) | 20.2 ** | 0.3 | 1.6 | 1.5 | 1.3 | 1.2 | ||||
| Disaster Risk Factors | ||||||||||
| Below Poverty (%) | 27.8 ** | 13.6 | 29.8 | 7.1 | 31.2 | 14.3 | 27.9 | 17.2 | 23.5 | 13.8 |
| Unemployed (%) | 10.2 ** | 6.8 | 9.5 | 4.0 | 15.2 | 9.8 | 10.5 | 5.2 | 6.6 | 4,0 |
| No High School Diploma (%) | 22.8 | 12.0 | 33.7 | 7.5 | 21.4 | 10.7 | 12.4 | 9.7 | 24.5 | 10.3 |
| Disabled (%) | 15.3 ** | 7.0 | 20.1 | 6.9 | 18.4 | 8.4 | 12 | 5.8 | 12.1 | 3.0 |
| Crowded Housing (%) | 5.4 | 3.6 | 6.7 | 4.2 | 4.6 | 2.9 | 3.0 | 2.8 | 6.9 | 3.1 |
| No Vehicle (%) | 15.4 ** | 10.9 | 14.8 | 6.0 | 16 | 12.7 | 21.4 | 14.9 | 16.9 | 6.7 |
| No Health Insurance (%) | 31.6 | 8.4 | 38.8 | 4.9 | 31.2 | 6.8 | 24.7 | 6.9 | 32.1 | 8.7 |
| Per capita income ($) | 22,235 ** | 14,298 | 16,276 | 18,752 | 27,810 | 24,930 | ||||
| Median Household Income ($) | 30,149 | 25,240 | 40,442 | 27,860 | ||||||
| Homes Flooded during Harvey (%) | 22 | 82 | 37 | 32 | 23 | |||||
| COVID Incidence (per 1000) | 54.5 | 19.7 | 50–74 | 50–74 | 50–74 | <25 | ||||
| COVID Case Fatality Rate (%) | 0.9 | 0.7 | 1–1.5 | 1–1.5 | 1–1.5 | >1.5 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adepoju, O.E.; Han, D.; Chae, M.; Smith, K.L.; Gilbert, L.; Choudhury, S.; Woodard, L. Health Disparities and Climate Change: The Intersection of Three Disaster Events on Vulnerable Communities in Houston, Texas. Int. J. Environ. Res. Public Health 2022, 19, 35. https://doi.org/10.3390/ijerph19010035
Adepoju OE, Han D, Chae M, Smith KL, Gilbert L, Choudhury S, Woodard L. Health Disparities and Climate Change: The Intersection of Three Disaster Events on Vulnerable Communities in Houston, Texas. International Journal of Environmental Research and Public Health. 2022; 19(1):35. https://doi.org/10.3390/ijerph19010035
Chicago/Turabian StyleAdepoju, Omolola E., Daikwon Han, Minji Chae, Kendra L. Smith, Lauren Gilbert, Sumaita Choudhury, and LeChauncy Woodard. 2022. "Health Disparities and Climate Change: The Intersection of Three Disaster Events on Vulnerable Communities in Houston, Texas" International Journal of Environmental Research and Public Health 19, no. 1: 35. https://doi.org/10.3390/ijerph19010035
APA StyleAdepoju, O. E., Han, D., Chae, M., Smith, K. L., Gilbert, L., Choudhury, S., & Woodard, L. (2022). Health Disparities and Climate Change: The Intersection of Three Disaster Events on Vulnerable Communities in Houston, Texas. International Journal of Environmental Research and Public Health, 19(1), 35. https://doi.org/10.3390/ijerph19010035







