Maternal Mental Health under COVID-19 Pandemic in Thailand
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaire Design
- (1)
- Socio-demographic characteristics—age, ethnicity, marital status, education, employment status, household income, household members, type of accommodation (e.g., own house, apartment/condominium, dormitory, and rental house), number of rooms in the accommodation, and pets at home. Moreover, we collected the infant age, mother’s alcohol drinking during the last 7 days, and smoking in the last 2 days. The answers to these questions are “yes” or “no”.
- (2)
- Experiences of COVID-19 symptoms and investigation—the questions in this section asked about the experience of COVID-19, if mothers and other members in the household had COVID-19 symptoms, and if the mothers had been investigated for COVID-19. The answers to these questions are “yes” or “no”.
- (3)
- Perception of COVID-19 lockdown impacts—the questions in this section about how the lockdown impacted mothers’ life and activities in negative ways during the COVID-19 lockdown consisted of 6 questions. The answers to these questions were given on a 4-point Likert scale as major, moderate, minor, and no impact.
- (3.1)
- “Your employment/In what ways has your work been affected by COVID-19”.
- (3.2)
- “Your partner’s employment/In what ways has his work been affected by COVID-19”.
- (3.3)
- “Your household’s ability to pay for other essentials, such as utilities and medication”.
- (3.4)
- “Your household’s ability to pay for food”.
- (3.5)
- “Your household’s ability to pay for rent/to make mortgage payments”.
- (3.6)
- “Household crowding after lockdown”.
- (4)
- Activities during the nationwide COVID-19 lockdown period—the questions in this section asked about the frequency of different activities, and the answers to these questions were given on a 4-point Likert scale as every day, more than 5 times per week, 4–5 times per week, 1–3 times per week, and never. These questions are in two parts, as follows:
- (4.1)
- Indoor/outdoor activities e.g., “went outside for a walk or for exercise”, “went shopping at the grocery store or pharmacy”, “participated in an online activity”, and “practiced a relaxation technique”.
- (4.2)
- Supportive activities e.g., “contact with a mother and baby support group or breastfeeding support group”, “contact with a health professional (general practioner (GP), health visitor, midwife), in person, by phone or online”, and “Attended an online, phone, or in person appointment with a mental health professional”.
- (5)
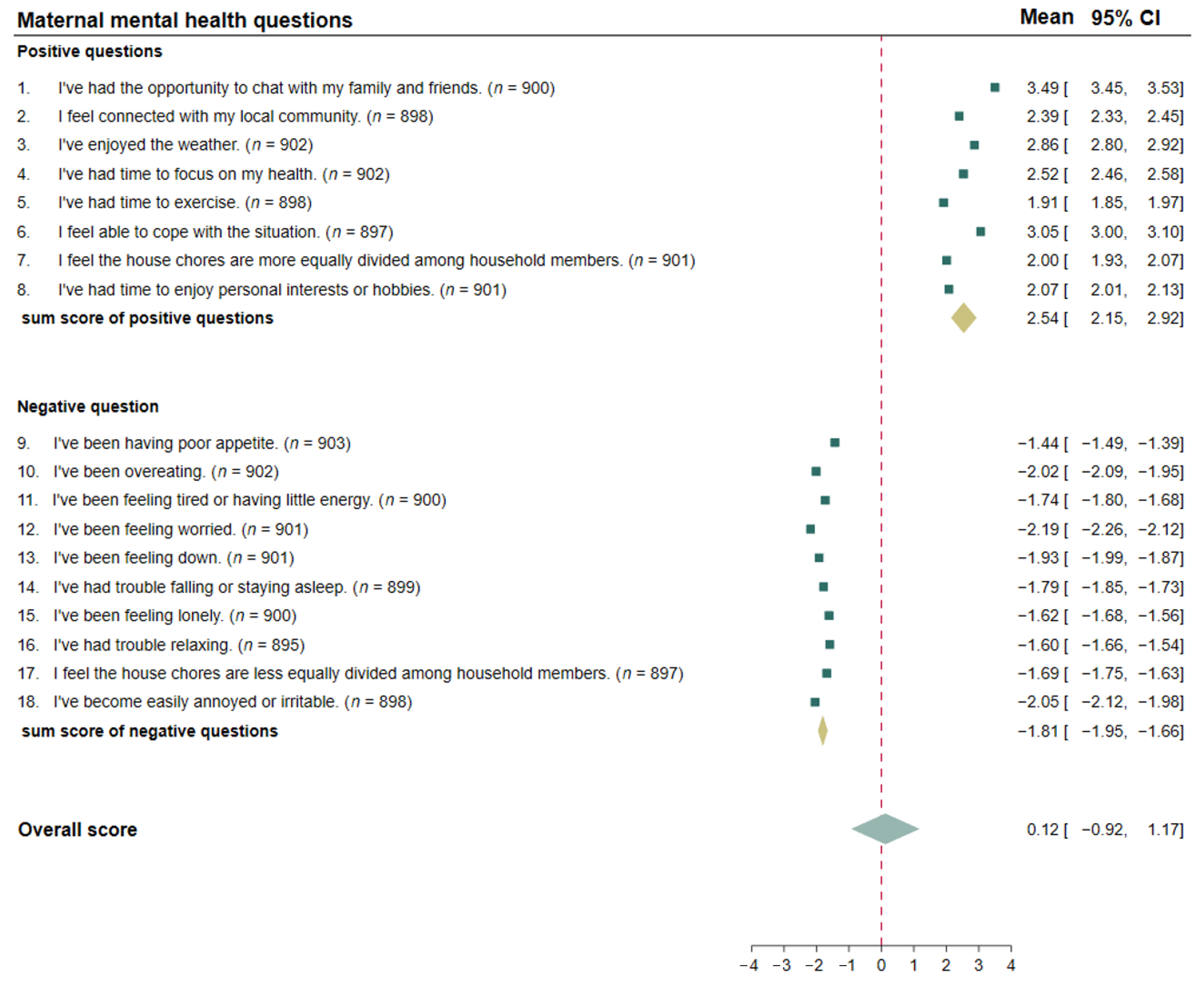
- Maternal mental health—the questions in this section regarded the participants’ mood during the lockdown period. This tool was a 4-point Likert scale; to a high extent, to some extent, very little, and not at all. The overall score was calculated by the sum score of positive questions (no. 1–8) minus the sum score of negative questions (no. 9–18). This individual score will represent the maternal mood status and is used as the dependent variable in the exploratory analysis by Multivariable Linear Regression. The alpha coefficient for the reliability test of the mother’s mood questionnaire was 0.78 (Supplementary Table S1). There are two subsections of questions, positive and negative questions, as follows:
- (5.1)
- Positive ways had 8 items: “I’ve had the opportunity to chat with my family and friends”, “I feel connected with my local community”, “I’ve enjoyed the weather”, “I’ve had time to focus on my health”, “I’ve had time to exercise”, “I feel able to cope with the situation”, “I feel the house chores are more equally divided among household members”, and “I’ve had time to enjoy personal interests or hobbies”.
- (5.2)
- Negative ways had 10 items: “I’ve been having a poor appetite”, “I’ve been overeating”, “I’ve been feeling tired or having little energy”, “I’ve been feeling worried”, “I’ve been feeling down”, “I’ve had trouble falling or staying asleep”, “I’ve been feeling lonely”, “I’ve had trouble relaxing”, “I feel the house chores are less equally divided among household members”, and “I’ve become easily annoyed or irritable”.
2.3. Statistical Analysis
2.4. Ethical Consideration
3. Results
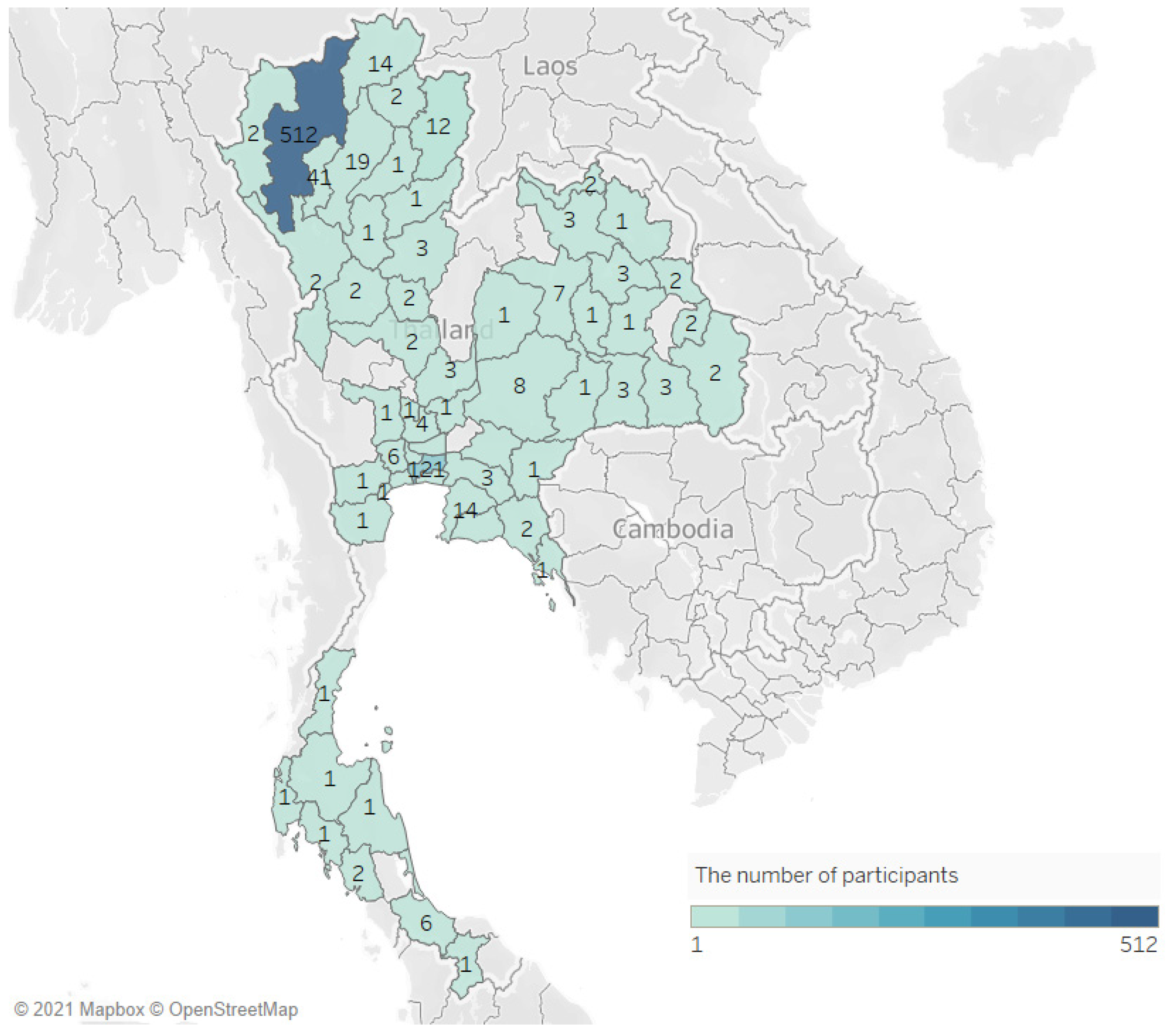
3.1. Characteristics of Participants
3.2. Mothers’ Perception of Impacts of COVID-19 Lockdown
3.3. Mothers’ Activities during the COVID-19 Lockdown Period
3.4. The Maternal Mental Health during the COVID-19 Lockdown Period
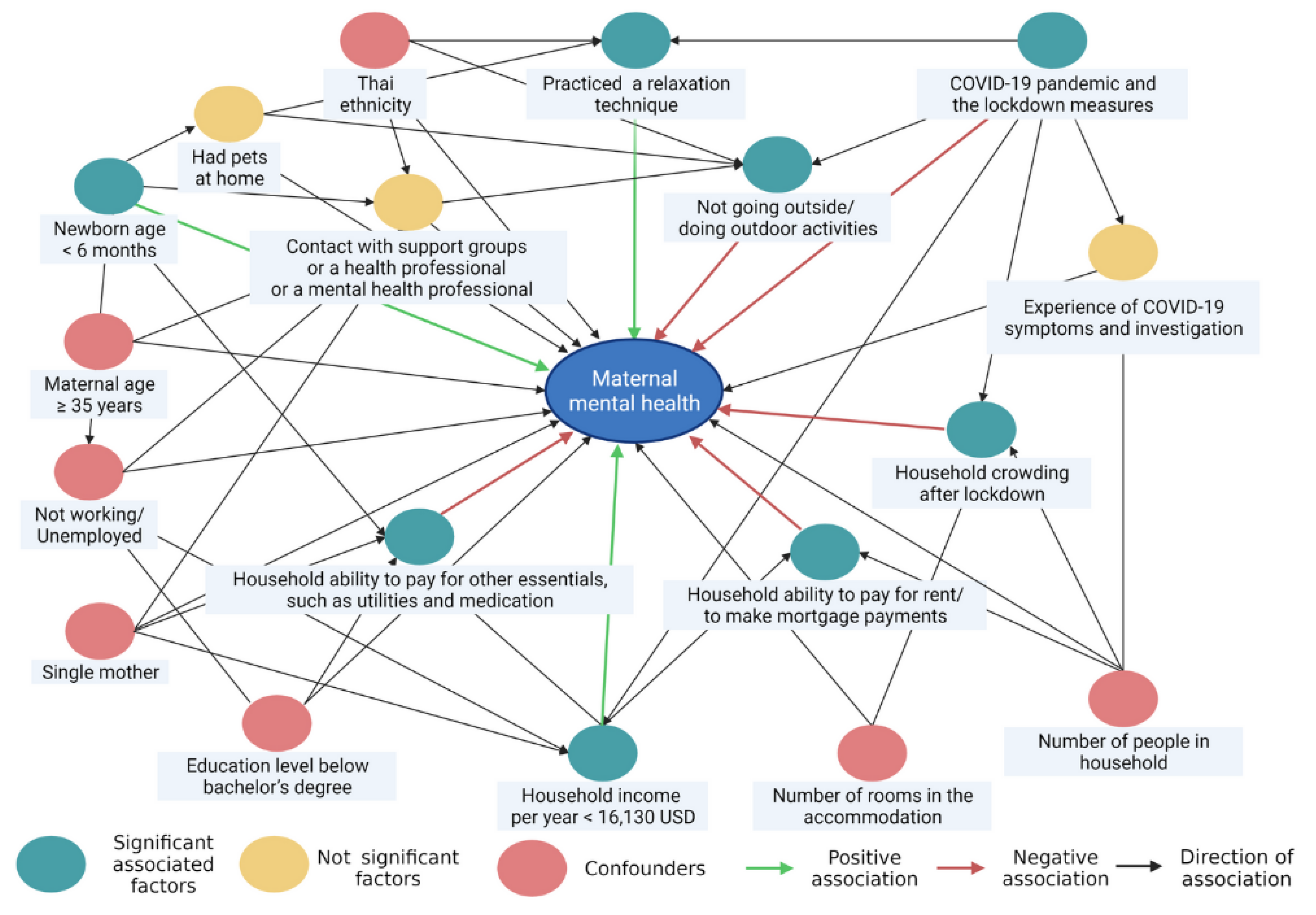
3.5. The Associated Factors of Maternal Mental Health during the COVID-19 Lockdown Period
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sen-Crowe, B.; McKenney, M.; Elkbuli, A. Social distancing during the COVID-19 pandemic: Staying home save lives. Am. J. Emerg. Med. 2020, 38, 1519–1520. [Google Scholar] [CrossRef] [PubMed]
- Teslya, A.; Pham, T.M.; Godijk, N.G.; Kretzschmar, M.E.; Bootsma, M.C.J.; Rozhnova, G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med. 2020, 17, e1003166. [Google Scholar] [CrossRef] [PubMed]
- Lesourd, B.M. Nutrition and immunity in the elderly: Modification of immune responses with nutritional treatments. Am. J. Clin. Nutr. 1997, 66, 478s–484s. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Miller, M.; Yaxley, A.; Isenring, E. Malnutrition in the elderly: A narrative review. Maturitas 2013, 76, 296–302. [Google Scholar] [CrossRef] [Green Version]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [Green Version]
- Alkhamees, A.A.; Alrashed, S.A.; Alzunaydi, A.A.; Almohimeed, A.S.; Aljohani, M.S. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr. Psychiatry 2020, 102, 152192. [Google Scholar] [CrossRef]
- Adams-Prassl, A.; Boneva, T.; Golin, M.; Rauh, C. The Impact of the Coronavirus Lockdown on Mental Health: Evidence from the US; University of Cambridge: Cambridge, UK, 2020. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Biroli, P.; Bosworth, S.; Della Giusta, M.; Di Girolamo, A.; Jaworska, S.; Vollen, J. Family Life in Lockdown. Front. Psychol. 2021, 12, 687570. [Google Scholar] [CrossRef]
- Giuntella, O.; Hyde, K.; Saccardo, S.; Sadoff, S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2016632118. [Google Scholar] [CrossRef] [PubMed]
- Piankusol, C.; Sirikul, W.; Ongprasert, K.; Siviroj, P. Factors Affecting Breastfeeding Practices under Lockdown during the COVID-19 Pandemic in Thailand: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 8729. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.; Xu, X. The Mental Health Effects of the First Two Months of Lockdown and Social Distancing during the COVID-19 Pandemic in the UK; IFS Working Paper W20/16; Institute for Fiscal Studies (IFS): London, UK, 2020. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Riley, V.; Ellis, N.; Mackay, L.; Taylor, J. The impact of COVID-19 restrictions on women’s pregnancy and postpartum experience in England: A qualitative exploration. Midwifery 2021, 101, 103061. [Google Scholar] [CrossRef]
- Collin, J.; Byström, E.; Carnahan, A.; Ahrne, M. Public Health Agency of Sweden’s Brief Report: Pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in Sweden. Acta Obstet. Gynecol. Scand. 2020, 99, 819–822. [Google Scholar] [CrossRef]
- Perzow, S.E.D.; Hennessey, E.-M.P.; Hoffman, M.C.; Grote, N.K.; Davis, E.P.; Hankin, B.L. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. J. Affect. Disord. Rep. 2021, 4, 100123. [Google Scholar] [CrossRef]
- Vazquez-Vazquez, A.; Dib, S.; Rougeaux, E.; Wells, J.C.; Fewtrell, M.S. The impact of the COVID-19 lockdown on the experiences and feeding practices of new mothers in the UK: Preliminary data from the COVID-19 New Mum Study. Appetite 2021, 156, 104985. [Google Scholar] [CrossRef] [PubMed]
- Dib, S.; Rougeaux, E.; Vázquez-Vázquez, A.; Wells, J.C.K.; Fewtrell, M. Maternal mental health and coping during the COVID-19 lockdown in the UK: Data from the COVID-19 New Mum Study. Int. J. Gynecol. Obstet. 2020, 151, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Gao, M.Y.; Fewtrell, M.; Wells, J.; Yu, J.Y. Maternal mental health and well-being during the COVID-19 pandemic in Beijing, China. World J. Pediatr. 2021, 17, 280–289. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Maternal Mental Health and Child Health and Development in Low and Middle Income Countries: Report of the Meeting, Geneva, Switzerland, 30 January–1 February, 2008; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef]
- Sedov, I.D.; Cameron, E.E.; Madigan, S.; Tomfohr-Madsen, L.M. Sleep quality during pregnancy: A meta-analysis. Sleep Med. Rev. 2018, 38, 168–176. [Google Scholar] [CrossRef]
- Racine, N.; Hetherington, E.; McArthur, B.A.; McDonald, S.; Edwards, S.; Tough, S.; Madigan, S. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: A longitudinal analysis. Lancet Psychiatry 2021, 8, 405–415. [Google Scholar] [CrossRef]
- Yan, H.; Ding, Y.; Guo, W. Mental Health of Pregnant and Postpartum Women During the Coronavirus Disease 2019 Pandemic: A Systematic Review and Meta-Analysis. Front. Psychol. 2020, 11, 3324. [Google Scholar] [CrossRef] [PubMed]
- Woody, C.A.; Ferrari, A.J.; Siskind, D.J.; Whiteford, H.A.; Harris, M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017, 219, 86–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topothai, C.; Tangcharoensathien, V. Achieving global targets on breastfeeding in Thailand: Gap analysis and solutions. Int. Breastfeed. J. 2021, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- Kaewsarn, P.; Moyle, W.; Creedy, D. Traditional postpartum practices among Thai women. J. Adv. Nurs. 2003, 41, 358–366. [Google Scholar] [CrossRef] [Green Version]
- Aikawa, T.; Pavadhgul, P.; Chongsuwat, R.; Sawasdivorn, S.; Boonshuyar, C. Maternal return to paid work and breastfeeding practices in Bangkok, Thailand. Asia Pac. J. Public Health 2015, 27, Np1253–Np1262. [Google Scholar] [CrossRef] [PubMed]
- Silverman, M.E.; Burgos, L.; Rodriguez, Z.I.; Afzal, O.; Kalishman, A.; Callipari, F.; Pena, Y.; Gabay, R.; Loudon, H. Postpartum mood among universally screened high and low socioeconomic status patients during COVID-19 social restrictions in New York City. Sci. Rep. 2020, 10, 22380. [Google Scholar] [CrossRef]
- Fullana, M.A.; Hidalgo-Mazzei, D.; Vieta, E.; Radua, J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020, 275, 80–81. [Google Scholar] [CrossRef]
- Oyarzabal, E.A.; Seuferling, B.; Babbar, S.; Lawton-O’Boyle, S.; Babbar, S. Mind-Body Techniques in Pregnancy and Postpartum. Clin. Obstet. Gynecol. 2021, 64, 683–703. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total (n = 903) | |
|---|---|---|
| n | % | |
| Maternal age | ||
| ≤18 years | 2 | 0.2 |
| 19–35 years | 705 | 78.1 |
| >35 years | 196 | 21.7 |
| Infant age | ||
| ≤6 months | 572 | 63.3 |
| 6–12 months | 331 | 36.7 |
| Marital status | ||
| Single mother | 132 | 14.6 |
| Nuclear family | 771 | 85.4 |
| Education | ||
| Below bachelor’s degree | 628 | 69.5 |
| Bachelor’s degree or above | 275 | 30.4 |
| Employment | ||
| Not working/Unemployed | 80 | 11.4 |
| Employed | 514 | 73.3 |
| Business owner | 107 | 15.3 |
| Household members, mean ± SD | 3 | ±1 |
| Type of accommodation | ||
| Own house | 722 | 80.0 |
| Apartment/Condominium | 46 | 5.1 |
| Dormitory | 114 | 12.6 |
| Rental house | 21 | 2.3 |
| Number of rooms in the accommodation, mean ± SD | 6 | ±2 |
| Living conditions | ||
| Can access to a private space/garden for doing an activity | 423 | 47.8 |
| Can access to a community space/garden for doing an activity | 144 | 16.0 |
| Not going outside/Doing outdoor activities | 327 | 36.2 |
| Household income per year | ||
| Less than USD 16,130 | 314 | 34.9 |
| More than USD 16,130 | 588 | 65.1 |
| Had pets at home | 359 | 39.8 |
| Alcohol drunk during the last 7 days | 18 | 2.0 |
| Smoking in the last 2 days | 2 | 0.2 |
| Experience of COVID-19 symptoms and investigation | ||
| Had symptoms | 8 | 0.9 |
| Any other member of household had symptoms | 5 | 0.5 |
| Had been tested for COVID-19 | 69 | 7.6 |
| COVID-19 Lockdown Impacts (n = 903) | Levels of Impact | |||
|---|---|---|---|---|
| Moderate to Major | No or Minor | |||
| n | % | n | % | |
| Your employment/In what ways has your work been affected by COVID-19 | 425 | 47.1 | 478 | 52.9 |
| Your household’s ability to pay for other essentials, such as utilities and medication | 406 | 45.0 | 497 | 55.0 |
| Your partner’s employment/In what ways has their work been affected by COVID-19 | 395 | 43.7 | 508 | 56.3 |
| Your household’s ability to pay for food | 385 | 42.6 | 518 | 57.4 |
| Your household’s ability to pay for rent/To make mortgage payments | 261 | 28.9 | 642 | 71.1 |
| Household crowding after lockdown | 133 | 14.7 | 770 | 85.3 |
| Activities (n = 903) | Levels of Activity (Times per Week), n (%) | |||
|---|---|---|---|---|
| >5 Times/Every Day | 4–5 Times | 1–3 Times | Never | |
| Indoor/outdoor activity | ||||
| Participated in an online activity | 283 (31.3) | 90 (10.0) | 182 (20.2) | 348 (38.5) |
| Went outside for a walk or for exercise | 172 (19.1) | 105 (11.6) | 309 (34.3) | 316 (35.0) |
| Practiced a relaxation technique | 160 (17.8) | 99 (11.0) | 282 (31.3) | 359 (39.9) |
| Went shopping to the grocery store or pharmacy | 67 (7.4) | 101 (11.2) | 501 (55.5) | 233 (25.8) |
| Supportive activity | ||||
| Contact with a mother and baby support group or breastfeeding support group | 83 (9.2) | 58 (6.4) | 211 (23.4) | 548 (60.9) |
| Contact with a health professional (GP, Health Visitor, Midwife), in person, by phone or online | 4 (0.4) | 17 (1.9) | 180 (20.0) | 698 (77.6) |
| Attended an online, phone, or in person appointment with a mental health professional | 0 (0.0) | 6 (0.7) | 22 (2.4) | 871 (96.9) |
| Variables | β-coef. | 95% CI | p-Value |
|---|---|---|---|
| Age ≥ 35 years | −0.29 | −1.40 to 0.82 | 0.607 |
| Newborn age < 6 months | 1.14 | 0.13 to 2.15 | 0.026 * |
| Thai ethnicity | −0.98 | −2.91 to 0.94 | 0.317 |
| Single mother | 0.10 | −1.3 to 1.49 | 0.891 |
| Education level below bachelor’s degree | 0.85 | −0.47 to 2.17 | 0.205 |
| Not working/Unemployed | −1.33 | −3.09 to 0.43 | 0.139 |
| Household income per year < 16,130 USD | 2.59 | 1.45 to 3.73 | <0.001 ** |
| Number of rooms in the accommodation | −0.10 | −0.27 to 0.08 | 0.272 |
| Number of people in household | 0.38 | −0.06 to 0.82 | 0.091 |
| Had pets at home | −0.40 | −1.42 to 0.62 | 0.439 |
| Experience of COVID-19 symptoms and investigation | |||
| Had symptoms | 0.22 | −5.12 to 5.56 | 0.936 |
| Any other member of household had symptoms | −0.05 | −6.4 to 6.3 | 0.988 |
| Had been under investigated for COVID-19 | −0.42 | −2.24 to 1.4 | 0.653 |
| COVID-19 lockdown impacts (moderate to major impacts) | |||
| Household’s ability to pay for rent/to make mortgage payments | −1.59 | −2.81 to −0.36 | 0.011 * |
| Household’s ability to pay for food | −0.52 | −1.7 to 0.67 | 0.392 |
| Household’s ability to pay for other essentials, such as utilities and medication | −1.99 | −3.16 to −0.81 | 0.001 ** |
| Impact on your employment/In what ways has your work been affected by COVID-19 | −0.32 | −1.37 to 0.74 | 0.554 |
| Impact on your partner’s employment/In what ways has their work been affected by COVID-19 | −0.54 | −1.57 to 0.49 | 0.305 |
| Household crowding after lockdown | −3.46 | −4.86 to −2.06 | <0.001 ** |
| Not going outside/doing outdoor activities | −2.22 | −3.35 to −1.08 | <0.001 ** |
| Activity during COVID-19 lockdown (times/week) | |||
| Went shopping to the grocery store or pharmacy | −0.16 | −0.75 to 0.43 | 0.591 |
| Went outside for a walk or for exercise | −0.06 | −0.54 to 0.42 | 0.796 |
| Participated in an online activity | −0.21 | −0.6 to 0.18 | 0.291 |
| Contact with a mother and baby support group or breastfeeding support group? | 0.01 | −0.98 to 1 | 0.980 |
| Contact with a health professional (GP, Health Visitor, Midwife), in person, by phone or online | −0.21 | −0.74 to 0.32 | 0.443 |
| Attended an online, phone, or in person appointment with a mental health professional | −1.48 | −3.96 to 1 | 0.241 |
| Practiced a relaxation technique | 1.05 | 0.57 to 1.52 | <0.001 ** |
| Constant | 5.33 | −10.98 to 21.63 | 0.521 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirikul, W.; Ongprasert, K.; Piankusol, C.; Siviroj, P. Maternal Mental Health under COVID-19 Pandemic in Thailand. Int. J. Environ. Res. Public Health 2022, 19, 347. https://doi.org/10.3390/ijerph19010347
Sirikul W, Ongprasert K, Piankusol C, Siviroj P. Maternal Mental Health under COVID-19 Pandemic in Thailand. International Journal of Environmental Research and Public Health. 2022; 19(1):347. https://doi.org/10.3390/ijerph19010347
Chicago/Turabian StyleSirikul, Wachiranun, Krongporn Ongprasert, Chanodom Piankusol, and Penprapa Siviroj. 2022. "Maternal Mental Health under COVID-19 Pandemic in Thailand" International Journal of Environmental Research and Public Health 19, no. 1: 347. https://doi.org/10.3390/ijerph19010347
APA StyleSirikul, W., Ongprasert, K., Piankusol, C., & Siviroj, P. (2022). Maternal Mental Health under COVID-19 Pandemic in Thailand. International Journal of Environmental Research and Public Health, 19(1), 347. https://doi.org/10.3390/ijerph19010347








