Mental Health in Women Victims of Gender Violence: Descriptive and Multivariate Analysis of Neuropsychological Functions and Depressive Symptomatology
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Ethical Aspects
2.4. Instruments
2.5. Data Analysis
3. Results
3.1. Neuropsychological Functions and Depressiove Symptomatology in Women Victims of Gender Violence
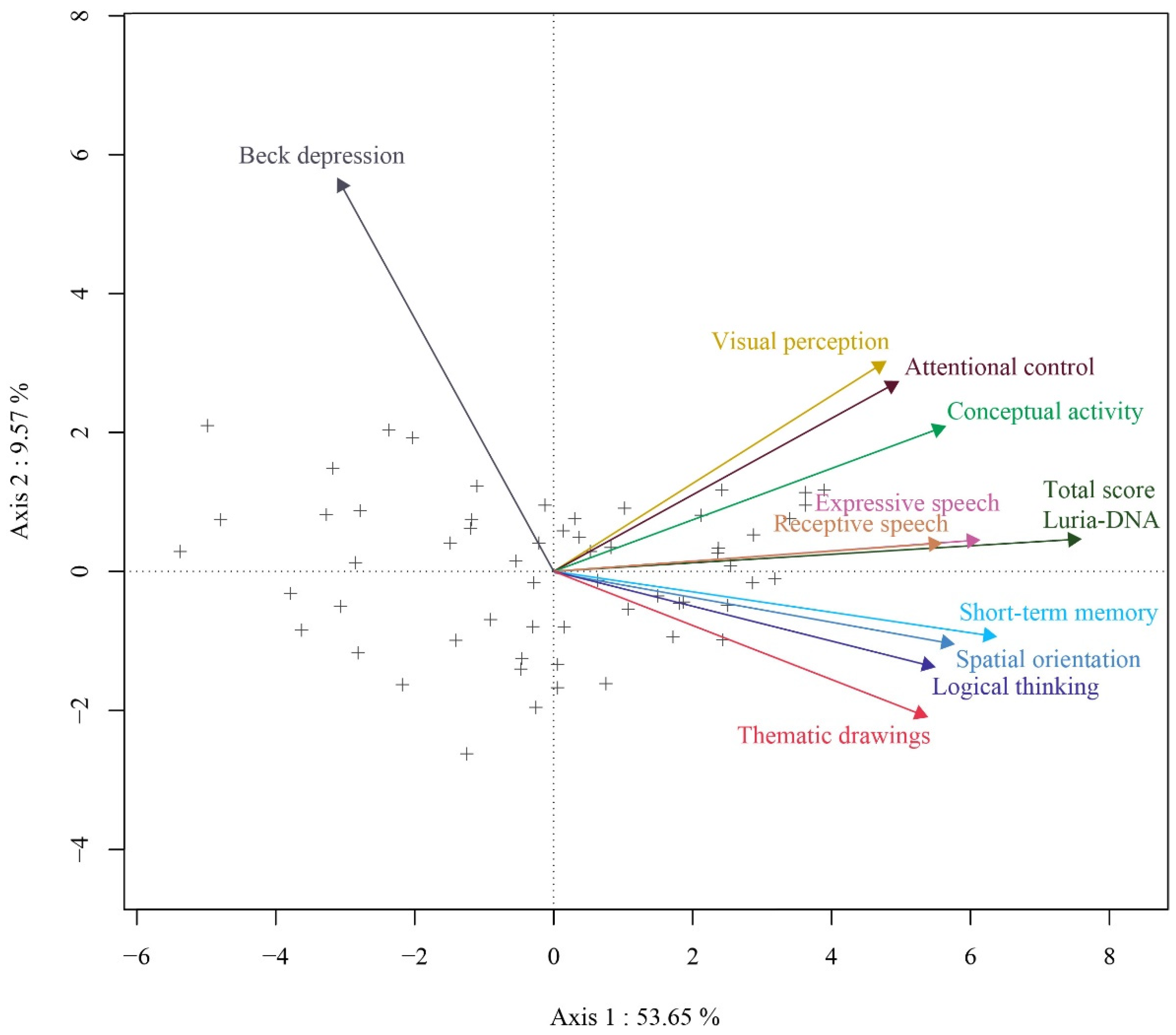
3.2. Association between Neuropsychological Sequelae and Depressive Symptomatology
- Cluster 1 consists of 23.3% of women in the analyzed sample who have high scores in all subscales scores of the Luria-DNA battery (with average scores above 50); and low scores in depressive symptomatology (M = 16.86, SD = 5.26).
- Cluster 2 consists of 50.0% of women in the sample who have scores around 40 points in the subscales scores of the Luria-DNA battery; and very low scores in depressive symptomatology (M = 12.93, SD = 7.97).
- Cluster 3 consists of 26.7% of women in the sample who have very low scores in all subscales scores of the Luria-DNA battery; and high scores in depressive symptomatology (M = 28.88, SD = 15.13).
4. Discussion
5. Conclusions
- The first cluster comprises of women who score high on all subscales of the Luria-DNA battery and obtain low scores in depressive symptomatology
- The second cluster includes women who obtain intermediate scores in all subscales of the Luria-DNA battery and score very low in depressive symptoms.
- And the third cluster is made up of women in the sample who have very low scores on the subscales of the Luria-DNA battery and score high in depressive symptomatology.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ley Orgánica 1/2004, de 28 de Diciembre, de Medidas de Protección Integral Contra la Violencia de Género. Boletín Oficial del Estado, 313 sec. I de 29 de Diciembre de 2004, 42166 a 42197. Available online: https://www.boe.es/eli/es/lo/2004/12/28/1/con (accessed on 30 September 2021).
- Arias, I.; Ikeda, R.M. Etiología y vigilancia de la violencia de pareja. Prevención de violencia. In Prevención de Violencia. Investigación y Estrategias de Intervención Basadas en la Evidencia; Lutzker, J.R., Ed.; Manual Moderno: Ciudad de Mexico, Mexico, 2008; pp. 165–184. [Google Scholar]
- McLaughlin, J.; O’Carrol, R.E.; O’Connor, R.C. Intimate partner abuse and suicidality. A systematic review. Clin. Psychol. Rev. 2012, 3, 677–689. [Google Scholar] [CrossRef] [PubMed]
- Echeburúa, E.; de Corral Gargallo, P.; Amor, P.J.; Sarasua, B.; Zubizarreta, I. Repercusiones psicopatológicas de la violencia doméstica en la mujer: Un estudio descriptivo. Rev. Psicopatol. Psicol. Clín. 1997, 2, 7–19. [Google Scholar] [CrossRef]
- Hirigoyen, M.F. Mujeres Maltratadas: Los Mecanismos de la Violencia en Pareja; Paidós: Barcelona, Spain, 2006. [Google Scholar]
- Labrador, F.J.; Rincón, P.P.; De Luis, P.; Fernández-Velasco, R. Mujeres Víctimas de Violencia Doméstica; Pirámide: Madrid, Spain, 2004. [Google Scholar]
- Porrúa, C.; Rodríguez-Carballeria, A.; Almendros, C.; Escartín, J.; Martín-Peña, J.; Santaña, O. Análisis de las estrategias de abuso psicológico en la violencia de pareja. Inf. Psicol. 2010, 99, 53–63. [Google Scholar]
- Marín Torices, M.I.M.; Hidalgo-Ruzzante, N.; Sabio, V.T. Neuropsicología forense en un caso de violencia de género. Psicol. Conduct. 2016, 24, 361–376. [Google Scholar]
- Portellano Pérez, J.A. Neuropsicología Infantil; Síntesis: Madrid, Spain, 2007. [Google Scholar]
- Rodríguez, D.M.; Campos, F.R. Evaluación neuropsicológica. Clin. Health 1999, 10, 331–376. [Google Scholar]
- Rodríguez, D.M.; Campos, F.R. Batería Luria-DNA: Diagnóstico neuropsicológico de adultos. Ediciones 2000. Available online: https://dialnet.unirioja.es/servlet/libro?codigo=50642 (accessed on 30 September 2021).
- Orsini, D.L.; van Gorp, W.G.; Boone, K.B. Head Injury. In The Neuropsychology Casebook; Springer: New York, NY, USA, 1988; pp. 1–39. [Google Scholar]
- Lezak, M.D. Psychological implications of traumatic brain damage for the patient’s family. Rehabil. Psychol. 1986, 31, 241. [Google Scholar] [CrossRef]
- Bilder, R.M.; Kane, J.M. Evaluación de los trastornos mentales orgánicos. Med. Las Enferm. Ment. Eval. Psicométrica Para Los Clín. 1991, 183–203. [Google Scholar]
- Austin, M.P.; Mitchell, P.; Goodwin, G.M. Cognitive deficits in depression: Possible implications for functional neuropathology. Br. J. Psychiatry 2001, 178, 200–206. [Google Scholar] [CrossRef]
- Herrera-Guzmán, I.; Gudayol-Ferré, E.; Herrera-Abarca, J.E.; Herrera-Guzmán, D.; Montelongo-Pedraza, P.; Blázquez, F.P.; Guàrdia-Olmos, J. Major depressive disorder in recovery and neuropsychological functioning: Effects of selective serotonin reuptake inhibitor and dual inhibitor depression treatments on residual cognitive deficits in patients with major depressive disorder in recovery. J. Affect. Disord. 2010, 123, 341–350. [Google Scholar] [CrossRef]
- Rogers, M.A.; Kasai, K.; Matsuo, K.; Fukuda, R.; Iwanami, A.; Nakagome, K.; Fukuda M y Nobumasa, K. Executive and prefrontal dysfunction in unipolar depression: A review of neuropsychological and imaging evidence. Neurosci. Res. 2004, 50, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Weiland-Fiedler, P.; Erickson, K.; Waldeck, T.; Luckenbaugh, D.A.; Pike, D.; Bonne, O.; Charney, D.S.; Neumeister, A. Evidence for continuing neuropsychological impairments in depression. J. Affect. Disord. 2004, 82, 253–258. [Google Scholar] [CrossRef]
- Egeland, J.; Rund, B.O.; Sundet, K.; Landro, N.I.; Asbjornsen, A.; Lund, A.; Rones, A.; Stordal, K.I.; Hughdahl, K. Attention profile in schizophrenia compared with depression: Differential effects of processing speed, selective attention and vigilance. Acta Psychiatr. Scand. 2003, 108, 276–284. [Google Scholar] [CrossRef]
- Airaksinen, E.; Larsson, M.L.; Lundberg, I.; Forsell, Y. Cognitive functions in depressive disorders: Evidence from a population based study. Psychol. Med. 2004, 34, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Harvey, P.O.; LeBastard, G.; Pochon, J.B.; Levy, R.; Alliaire, J.F.; Dubois, B.; Fossati, P. Executive functions and updating the contents of working memory in unipolar depression. J. Psychiatr. Res. 2004, 38, 567–576. [Google Scholar] [CrossRef]
- Henry, J.D.; Crawford, J.R. A Meta-analytic review of verbal fluency deficits in depresión. J. Clin. Exp. Neuropsychol. 2005, 27, 78–101. [Google Scholar] [CrossRef]
- Michopoulos, I.; Zervas, I.M.; Papakosta, V.M.; Tsaltsas, E.; Papageorgiu, C.; Manéis, T.; Papakostas, Y.G.; Lykouras, L.; Soldatos, C.R. Set Shifting deficits in melancholic vs. Nonmelancholic depresion: Preliminary findings. Eur. Psychiatry 2006, 21, 361–363. [Google Scholar] [CrossRef]
- Paelecke-Habermann, I.; Pohl, J.; Leplow, B. Attention and executive functions in remitted major depression patients. J. Affect. Disord. 2005, 89, 125–135. [Google Scholar] [CrossRef] [PubMed]
- De la Ossa, C.A.; Díaz, R.M.; Romero-Acosta, K.; Giraldo, A.F.R. Desempeño neurocognitivo de la atención, memoria y función ejecutiva en una población infanto-juvenil escolarizada con y sin presencia de sintomatología internalizante. Psicogente 2018, 21, 403–421. [Google Scholar]
- Toren, P.; Sadeh, M.; Wolmer, L.; Sofia, E.; Koren, S.; Weizman, R.; Laor, N. Neurocognitive Correlates of Anxiety Disorders in Children: A Preliminary Report. J. Anxiety Disord. 2000, 14, 242–246. [Google Scholar] [CrossRef]
- Günther, T.; Holtkamp, K.; Jolles, J.; Herpertz-Dahlmann, B.; Konrad, K. Verbal memory and aspects of attentional control in children and adolescents with anxiety disorders or depressive disorders. J. Affect. Disord. 2004, 82, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Muris, P.; van der Pennen, E.; Sigmond, R.; Mayer, B. Symptoms of anxiety, depression, and aggression in non-clinical children: Relationships with self-report and performance-based measures of attention and effortful control. Child Psychiatry Hum. Dev. 2008, 39, 455–467. [Google Scholar] [CrossRef]
- Mocan, O.; Stanciu, O.; Visu-Petra, L. Relating individual differences in internalizing symptoms to emotional attention set-shifting in children. Anxiety Stress Coping 2014, 27, 509–526. [Google Scholar] [CrossRef]
- Emerson, C.S.; Mollet, G.A.; Harrison, D.W. Anxious-depression in boys: An evaluation of executive functioning. Arch. Clin. Neuropsychol. 2005, 20, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Baune, B.T.; Czira, M.E.; Smith, A.L.; Mitchell, D.; Sinnamon, G. Neuropsychological performance in a sample of 13–25 year olds with a history of non-psychotic major depressive disorder. J. Affect. Disord. 2012, 141, 441–448. [Google Scholar] [CrossRef]
- Reinholdt-Dunne, M.L.; Mogg, K.; Benson, V.; Bradley, B.P.; Hardin, M.G.; Liversedge, S.P.; Pine, D.S.; Ernst, M. Anxiety and selective attention to angry faces: An antisaccade study. J. Cogn. Psychol. 2012, 24, 54–65. [Google Scholar] [CrossRef]
- Barrera, M.; Calderón, L.; Bell, V. The cognitive impact of sexual abuse and PTSD in children: A neuropsychological study. J. Child Sex. Abus. 2013, 22, 625–638. [Google Scholar] [CrossRef] [PubMed]
- Torres García, A.V. Evaluación Neuropsicológica en Mujeres Víctimas de Violencia de Género [Tesis Doctoral, Universidad de Salamanca]. 2014. Available online: https://gredos.usal.es/handle/10366/127895 (accessed on 30 September 2021).
- Fonzo, G.A.; Simmons, A.N.; Thorp, S.R.; Norman, S.B.; Paulus, M.P.; Stein, M.B. Exaggerated and disconnected insular-amygdalar blood oxygenation level-dependent response to threat-related emotional faces in women with intimate-partner violence posttraumatic stress disorder. Biol. Psychiatry 2010, 68, 433–441. [Google Scholar] [CrossRef]
- Simmons, A.N.; Paulus, M.P.; Thorp, S.R.; Matthews, S.C.; Norman, S.B.; Stein, M.B. Functional activation and neural networks in women with posttraumatic stress disorder related to intimate partner violence. Biol. Psychiatry 2008, 64, 681–690. [Google Scholar] [CrossRef]
- Valera, E.M.; Berenbaum, H. Brain injury in battered women. J. Consult. Clin. Psychol. 2003, 71, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Pedraza-Linares, O.L.; Cedeño-Izquierdo, M.I.; Sarmiento-Borda, L.C.; Santamaría-Ávila, L.A.; González-Arteaga, J.J.; Salazar-Montes, A.M.; Montalvo-Villegas, M.C.; Lozano-Ruiz, A.G.; Camacho-Bermúdez, I.N.; Castillo-Homez, P.C.; et al. Progresión del deterioro cognitivo y su relación con factores de riesgo modificables en una cohorte de adultos de bogotá. Acta Méd. Colomb. 2019, 44, 66–67. [Google Scholar] [CrossRef][Green Version]
- Boira, S.; Carbajosa, P.; Méndez, R. Miedo, conformidad y silencio: La violencia en las relaciones de pareja en áreas rurales de Ecuador. Psychosoc. Interv. 2016, 25, 9–17. [Google Scholar] [CrossRef]
- Campbell, J.C. Health consequences of intimate partner violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef]
- Ellsberg, M.; Jansen, H.A.F.M.; Heise, L.; Watts, C.H.; García-Moreno, C. Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: An observational study. Lancet 2008, 371, 1165–1172. [Google Scholar] [CrossRef]
- Glasier, A.; Gülmezoglu, A.M.; Schmid, G.P.; Moreno, C.G.; Van Look, P.F.A. Sexual and reproductive health: A matter of life and death. Lancet 2006, 368, 1595–1607. [Google Scholar] [CrossRef]
- Sugg, N. Intimate partner violence: Prevalence, health consequences, and intervention. Med. Clin. N. Am. 2015, 99, 629–649. [Google Scholar] [CrossRef]
- Valera, E.; Kucyi, A. Brain injury in women experiencing intimate partner-violence: Neural mechanistic evidence of an «invisible» trauma. Brain Imaging Behav. 2017, 11, 1664–1677. [Google Scholar] [CrossRef]
- Seedat, S.; Stein, M.B.; Forde, D.R. Association between Physical Partner Violence, Posttraumatic Stress, Childhood Trauma, and Suicide Attempts in a Community Sample of Women. Violence Vict. 2005, 20, 87–98. [Google Scholar] [CrossRef]
- García Navarro, C.; Gordillo León, F.; Pérez Nieto, M.Á. Análisis de las consecuencias cognitivas y afectivas de la violencia de género en relación con el tipo de maltrato. Ansiedad Y Estrés 2020, 26, 39–45. [Google Scholar] [CrossRef]
- Twamley, E.W.; Allard, C.B.; Thorp, S.R.; Norman, S.B.; Cissell, S.H.; Berardi, K.H.; Grimes, E.M.; Stein, M.B. Cognitive impairment and functioning in PTSD related to intimate partner violence. J. Int. Neuropsychol. Soc. 2009, 15, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Browne, A. Violence against women by male partners: Prevalence, outcomes, and policy implications. Am. Psychol. 1993, 48, 1077–1087. [Google Scholar] [CrossRef]
- Jackson, H.; Philp, E.; Nuttall, R.L.; Diller, L. Traumatic brain injury: A hidden consequence for battered women. Prof. Psychol. Res. Pract. 2002, 33, 39–45. [Google Scholar] [CrossRef]
- Stein, M.B.; Kennedy, C.M.; Twamley, E.W. Neuropsychological function in female victims of intimate partner violence with and without posttraumatic stress disorder. Biol. Psychiatry 2002, 52, 1079–1088. [Google Scholar] [CrossRef]
- Torres García, A.V.; Pérez Fernández, M.P. La evaluación Neuropsicológica de las Mujeres Víctimas de Violencia de Género Como Herramienta en los Procesos Judiciales. En Políticas Públicas en Defensa de la Inclusión, la Diversidad y el Género. Universidad de Salamanca. 2019, pp. 477–490. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=6929322 (accessed on 30 September 2021).
- Billoux, S.; Arbus, C.; Telmon, N.; Voltzenlogel, V. Autobiographical memory impairment in female victims of intimate partner violence. J. Fam. Violence 2016, 31, 897–902. [Google Scholar] [CrossRef]
- Kwako, L.E.; Glass, N.; Campbell, J.; Melvin, K.C.; Barr, T.; Gill, J.M. Traumatic brain injury in intimate partner violence: A critical review of outcomes and mechanisms. Trauma Violence Abus. 2011, 12, 115–126. [Google Scholar] [CrossRef]
- Hidalgo, N.; Medialdea, P.; Bueso-Izquierdo, N.; González, P.; Moral, E.; Perez-Garcia, M. Secuelas Cognitivas en Mujeres Víctimas de Violencia de Género. In Cognitive Effects in Women Victims of Intimate Partner Violence; III Congreso para el Estudio de la Violencia Contra las Mujeres: Justicia y Seguridad. Nuevos Retos; 2012; Available online: http://www.congresoestudioviolencia.com/2012/articulo20.php (accessed on 30 September 2021).
- Delara, M.D. Mental Health Consequences and Risk Factors of Physical Intimate Partner Violence. Ment. Health Fam. Med. 2016, 12, 119–125. [Google Scholar] [CrossRef]
- González-Ortega, I.; Echeburúa, E.; de Corral, P.; Polo-López, R. Pathological gambling: Clinical gender differences. In Psychopathology in Women; Springer: Cham, Switzerland, 2015; pp. 713–726. [Google Scholar]
- Kolb, B.; Whishaw, I.Q. Neuropsicología Humana; España, Ed.; Médica Panamericana: Madrid, Spain, 2006. [Google Scholar]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Beck, A.T.; Rush, A.J.; Shaw, B.F.; Emery, G. Cognitive Therapy of Depression; Trad. esp. en Bilbao: Desclée de Brower, 1983; Guilford Press: New York, NY, USA, 1979. [Google Scholar]
- Galindo-Villardón, P. Una alternativa de representación simultánea: HJ-Biplot. Questiió Quad. D’estadística Sist. Inform. I Investig. Oper. 1986, 10, 13–23. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows; Version 26.0; IBM Corp [Computer Software]: Armonk, NY, USA, 2019. [Google Scholar]
- Nieto-Librero, A.B.; Galindo-Villardón, P.; Freitas, A. Package ‘biplotbootGUI’: Bootstrap on Classical Biplots and Clustering Disjoint Biplot. 1.2. 2019. Available online: http://bioconductor.statistik.tu-dortmund.de/cran/web/packages/biplotbootGUI/biplotbootGUI.pdf (accessed on 30 September 2021).
- St Ivany, A.; Schminkey, D. Intimate partner violence and traumatic brain injury. Fam. Community Health 2016, 39, 129–137. [Google Scholar] [CrossRef]
- Zieman, G.; Bridwell, A.; Cardenas, J.F. Traumatic brain injury in domestic violence victims: A retrospective study at the Barrow neurological institute. J. Neurotrauma 2017, 34, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Vetere, G.; Tran, L.M.; Moberg, S.; Steadman, P.E.; Restivo, L.; Morrison, F.G.; Ressler, K.J.; Josselyn, S.A.; Frankland, P.W. Memory formation in the absence of experience. Nat. Neurosci. 2019, 22, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, A.; Saeedi, M.; Maghsoudi, A.; Shalbaf, A. Major depressive disorder diagnosis based on effective connectivity in EEG signals: A convolutional neural network and long short-term memory approach. Cogn. Neurodyn. 2021, 15, 239–252. [Google Scholar] [CrossRef]
- Echeburúa, E.; Corral, P. Trastorno de estrés postraumático. In Manual de Psicopatología; Belloch, A., Sandín, B., Ramos, F., Eds.; McGraw-Hill: Madrid, Spain, 1995; Volume 2. [Google Scholar]
- Otálvaro, L.E.O. Autoestima y adaptación en víctimas de maltrato psicológico por parte de la pareja. Psicol. Desde Caribe 2015, 32, 145–168. [Google Scholar]
- Cerezo, A.I. El Homicidio en la Pareja: Tratamiento Criminológico; Tirant lo Blanch: Valencia, Spain, 2000. [Google Scholar]
- Barnett, O.W. Why Battered Women Do Not Leave, Part 2: External Inhibiting Factors-Social Support and Internal Inhibiting Factors. Trauma Violence Abus. 2001, 2, 3–35. [Google Scholar] [CrossRef]
- Amor, P.J.; Echeburúa, E.; Corral, P.; Zubizarreta, I.; Sarasua, B. Repercusiones psicopatológicas de la violencia doméstica en la mujer en función de las circunstancias del maltrato. Revista Internacional de Psicología Clínica y de la Salud. Int. J. Clin. Health Psychol. 2002, 2, 227–246. (In Prensa) [Google Scholar]
- Mertin, P.; Mohr, P.B. A follow-up study of posttraumatic stress disorder, anxiety, and depression in Australian victims of domestic violence. Violence Vict. 2001, 16, 645–654. [Google Scholar]
- Davins, M.; Bartolomé, D.; Salamero, M.; Pérez-Testor, C. Mujeres Maltratadas y Calidad de la Relación de Pareja. Aloma: Revista de Psicología, Ciències de l’Educació i de l’Esport, (27). Recuperado a Partir de. 2011. Available online: http://revistaaloma.net/index.php/aloma/article/view/18 (accessed on 30 September 2021).
- Echeburúa Odriozola, E.; Corral Gargallo, P.D.; Amor Andrés, P.J. Mujeres maltratadas en convivencia prolongada con el agresor: Variables relevantes. Acción Psicol. 2002, 1, 135–150. [Google Scholar]

| Visual Perception | Spatial Orientation | Receptive Speech | Expressive Speech | Short-term Memory | Logical Thinking | Thematic Drawings | Conceptual Activity | Attentional Control | Total Score Luria-DNA | Beck Depression | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Visual perception | 1 | 0.462 ** | 0.446 ** | 0.428 ** | 0.466 ** | 0.355 ** | 0.278 * | 0.466 ** | 0.387 ** | 0.601 ** | −0.125 |
| Spatial orientation | 1 | 0.383 ** | 0.452 ** | 0.552 ** | 0.542 ** | 0.551 ** | 0.480 ** | 0.361 ** | 0.711 ** | −0.338 ** | |
| Receptive speech | 1 | 0.595 ** | 0.596 ** | 0.370 ** | 0.486 ** | 0.518 ** | 0.335 ** | 0.725 ** | −0.278 * | ||
| Expressive speech | 1 | 0.650 ** | 0.653 ** | 0.489 ** | 0.558 ** | 0.474 ** | 0.782 ** | −0.260 * | |||
| Short-term memory | 1 | 0.517 ** | 0.494 ** | 0.525 ** | 0.448 ** | 0.816 ** | −0.445 ** | ||||
| Logical thinking | 1 | 0.531 ** | 0.418 ** | 0.355 ** | 0.708 ** | −0.289 * | |||||
| Thematic drawings | 1 | 0.448 ** | 0.354 ** | 0.702 ** | −0.312 * | ||||||
| Conceptual activity | 1 | 0.489 ** | 0.748 ** | −0.177 | |||||||
| Attentional control | 1 | 0.640 ** | −0.148 | ||||||||
| Total score Luria-DNA | 1 | −0.328 * | |||||||||
| Beck depression | 1 |
| Model | B | SEB | Beta | t | p | R2 | F | p | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | (Constant) | 26.228 | 3.399 | 7.717 | <0.001 | 0.108 | 7.013 | 0.010 | |
| Total score Luria-DNA | −0.211 | 0.080 | −0.328 | −2.648 | 0.01 | ||||
| 2 | (Constant) | 31.463 | 7.512 | 4.188 | <0.001 | 0.122 | 2.368 | 0.042 | |
| Spatial orientation | −0.060 | 0.143 | −0.071 | −0.421 | 0.675 | ||||
| Receptive speech | 0.001 | 0.181 | 0.001 | 0.005 | 0.996 | ||||
| Expressive speech | 0.138 | 0.210 | 0.128 | 0.658 | 0.513 | ||||
| Short-term memory | −0.320 | 0.144 | −0.404 | −2.221 | 0.031 | ||||
| Logical thinking | −0.016 | 0.109 | −0.026 | −0.147 | 0.884 | ||||
| Thematic drawings | −0.095 | 0.127 | −0.123 | −0.745 | 0.460 | ||||
| Axis 1 | Axis 2 | Axis 3 | |
|---|---|---|---|
| Visual perception | 692.73 | 276.94 | 30.33 |
| Spatial orientation | 804.98 | 26.19 | 168.83 |
| Receptive speech | 759.38 | 4.32 | 236.31 |
| Expressive speech | 993.30 | 5.27 | 1.43 |
| Short-term memory | 900.87 | 19.45 | 79.68 |
| Logical thinking | 669.34 | 42.04 | 288.62 |
| Thematic drawings | 769.56 | 117.7 | 112.74 |
| Conceptual activity | 871.69 | 117.13 | 11.18 |
| Attentional control | 766.81 | 233.16 | 0.03 |
| Total score Luria-DNA | 995.54 | 3.73 | 0.73 |
| Beck depression | 195.08 | 645.69 | 159.24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres García, A.V.; Vega-Hernández, M.C.; Antón Rubio, C.; Pérez-Fernández, M. Mental Health in Women Victims of Gender Violence: Descriptive and Multivariate Analysis of Neuropsychological Functions and Depressive Symptomatology. Int. J. Environ. Res. Public Health 2022, 19, 346. https://doi.org/10.3390/ijerph19010346
Torres García AV, Vega-Hernández MC, Antón Rubio C, Pérez-Fernández M. Mental Health in Women Victims of Gender Violence: Descriptive and Multivariate Analysis of Neuropsychological Functions and Depressive Symptomatology. International Journal of Environmental Research and Public Health. 2022; 19(1):346. https://doi.org/10.3390/ijerph19010346
Chicago/Turabian StyleTorres García, Ana Victoria, María Concepción Vega-Hernández, Concha Antón Rubio, and Miguel Pérez-Fernández. 2022. "Mental Health in Women Victims of Gender Violence: Descriptive and Multivariate Analysis of Neuropsychological Functions and Depressive Symptomatology" International Journal of Environmental Research and Public Health 19, no. 1: 346. https://doi.org/10.3390/ijerph19010346
APA StyleTorres García, A. V., Vega-Hernández, M. C., Antón Rubio, C., & Pérez-Fernández, M. (2022). Mental Health in Women Victims of Gender Violence: Descriptive and Multivariate Analysis of Neuropsychological Functions and Depressive Symptomatology. International Journal of Environmental Research and Public Health, 19(1), 346. https://doi.org/10.3390/ijerph19010346






