Internal Migration Experience and Depressive Symptoms among Middle-Aged and Older Adults: Evidence from China
Abstract
:1. Introduction
2. Methods
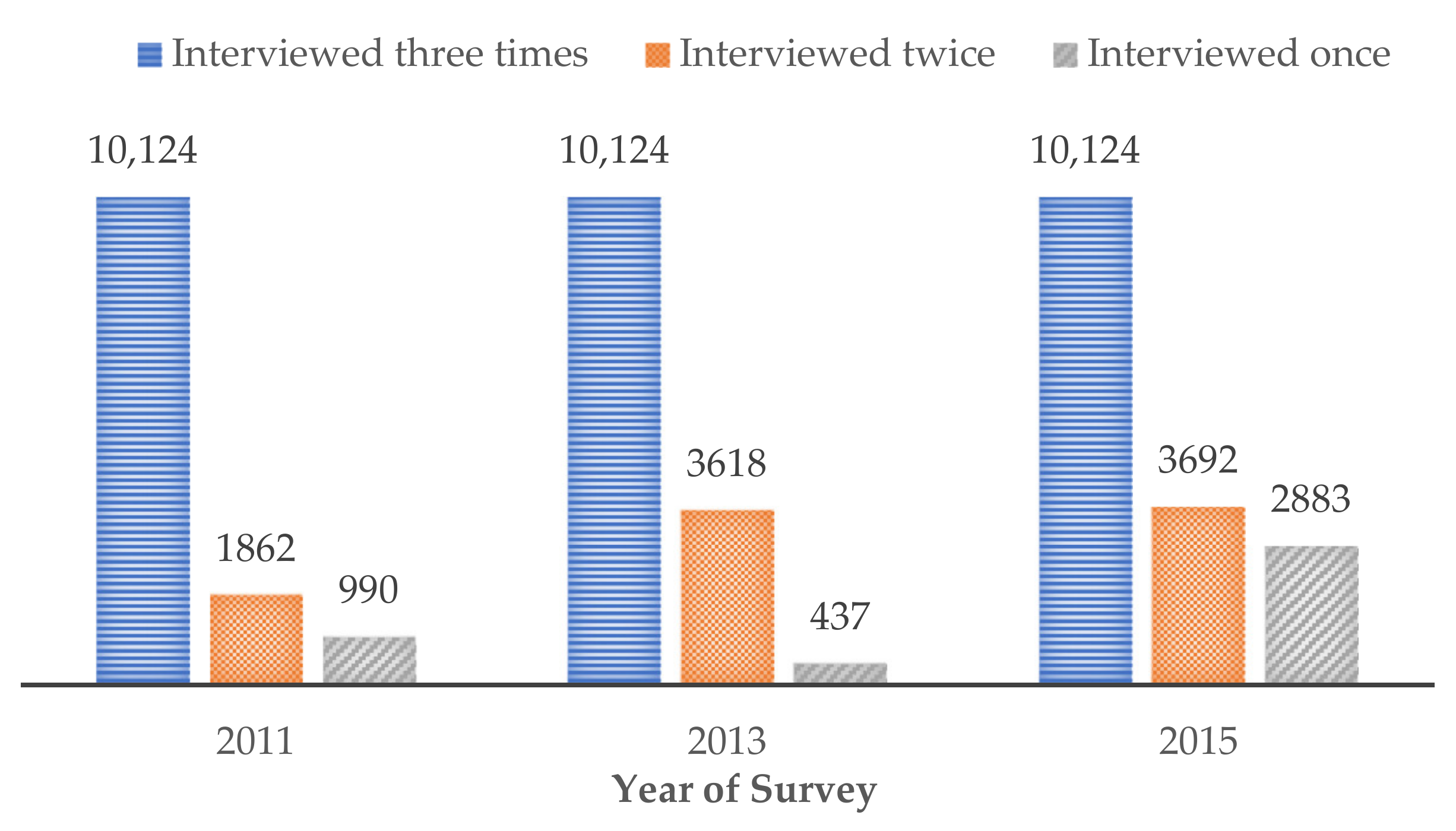
2.1. Participants
2.2. Measures
2.2.1. Internal Migration Experience
2.2.2. Depressive Symptoms
2.2.3. Mediators
2.2.4. Control Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Items | Rarely or None of the Time (<1 day) | Some or a Little of the Time (1–2 days) | Occasionally or a Moderate Amount of the Time (3–4 days) | Most or All of the Time (5–7 days) |
|---|---|---|---|---|
| ||||
| ||||
| ||||
| ||||
| ||||
| ||||
| ||||
| ||||
| ||||
| ||||
| Scoring | ||||
| Items 5 and 8 | 3 | 2 | 1 | 0 |
| All other items | 0 | 1 | 2 | 3 |
| Arthritis or Rheumatism | Stomach or Other Digestive Diseases | Hypertension | |
|---|---|---|---|
| Estimated value (components of indirect effects) | 0.007 (0.003–0.011) *** | 0.002 (−0.001–0.005) | 0.000 (−0.001–0.001) |
| Mediating effects (%) | 10.09% | 2.76% | 0.51% |
| Total effect | 0.073 (0.024–0.123) ** | ||
| Direct effect | 0.062 (0.015–0.108) ** | ||
| Indirect effect | 0.009 (0.004–0.015) *** | ||
References
- International Organization of Migration. World Migration Report. 2020. Available online: https://publications.iom.int/system/files/pdf/wmr_2020.pdf (accessed on 23 September 2021).
- National Bureau of Statistics of China. Press Conference on the Main Data Results of the Seventh National Census. 2021. Available online: http://www.chinanews.com/gn/2021/05-12/9475549.shtml (accessed on 25 September 2021). (In Chinese).
- Amin, A. The good city. Urban Stud. 2006, 43, 1009–1023. [Google Scholar] [CrossRef]
- Lederbogen, F.; Kirsch, P.; Haddad, L.; Streit, F.; Tost, H.; Schuch, P.; Wüst, S.; Pruessner, J.C.; Rietschel, M.; Deuschle, M.; et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011, 474, 498–501. [Google Scholar] [CrossRef]
- Li, J.; Rose, N. Urban social exclusion and mental health of China’s rural-urban migrants—A review and call for research. Health Place 2017, 48, 20–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J. Internal migration and health: Re-Examining the healthy migrant phenomenon in China. Soc. Sci. Med. 2011, 72, 1294–1301. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Kandilov, I.T.; Zhu, R. The Impact of internal migration on the health of rural migrants: Evidence from longitudinal data in China. J. Dev. Stud. 2020, 56, 840–855. [Google Scholar] [CrossRef]
- Yu, C.; Lou, C.; Cheng, Y.; Cui, Y.; Lian, Q.; Wang, Z.; Gao, E.; Wang, L. Young internal migrants’ major health issues and health seeking barriers in Shanghai, China: A qualitative study. BMC Public Health 2019, 19, 336. [Google Scholar] [CrossRef]
- Li, J.; Liu, Z. Housing stress and mental health of migrant populations in urban China. Cities 2018, 81, 172–179. [Google Scholar] [CrossRef]
- Ma, Z.; Xia, Y. Acculturation strategies, age at migration, and self-rated health: An empirical study on internal migrants in China. Soc. Sci. Res. 2021, 93, 102487. [Google Scholar] [CrossRef]
- Cable, N. Life Course approach in social epidemiology: An overview, application and future implications. J. Epidemiol. 2014, 24, 347–352. [Google Scholar] [CrossRef] [Green Version]
- Peele, M.E. Domains of childhood disadvantage and functional limitation trajectories among midlife men and women in China. J. Aging Health 2020, 32, 501–512. [Google Scholar] [CrossRef]
- Huang, C.; Phillips, M.R.; Zhang, Y.; Zhang, J.; Shi, Q.; Song, Z.; Ding, Z.; Pang, S.; Martorell, R. Malnutrition in early life and adult mental health: Evidence from a natural experiment. Soc. Sci. Med. 2013, 97, 259–266. [Google Scholar] [CrossRef] [Green Version]
- Rostila, M.; Saarela, J.; Kawachi, I. Birth order and suicide in adulthood: Evidence from Swedish population data. Am. J. Epidemiol. 2014, 179, 1450–1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Lachman, M.E. Socioeconomic Status and Parenting Style from Childhood: Long-Term Effects on Cognitive Function in Middle and Later Adulthood. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2019, 74, e13–e24. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Shangguan, S.; Fang, Z.; Fang, X. Early-Life exposure to parental mental distress and adulthood depression among middle-aged and elderly Chinese. Econ. Hum. Biol. 2021, 41, 100994. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.W. China’s hukou system at 60: Continuity and reform. In Handbook on Urban Development in China; Edward Elgar Publishing Ltd.: Cheltenham, UK, 2019; pp. 59–79. [Google Scholar] [CrossRef]
- Song, Q.; Smith, J.P. Hukou system, mechanisms, and health stratification across the life course in rural and urban China. Health Place 2019, 58, 102150. [Google Scholar] [CrossRef]
- Tong, Y.; Piotrowski, M.; Ye, H. Differences in the health–age profile across rural and urban sectors: A study on migrants and non-migrants in China. Public Health 2018, 158, 124–134. [Google Scholar] [CrossRef]
- Liu, J.; Chen, H.; Chen, Y.; Li, Z. Exploring the relationship between migrants’ purchasing of commercial medical insurance and urbanisation in China. BMC Health Serv. Res. 2018, 18, 679. [Google Scholar] [CrossRef]
- Sun, N.; Yang, F. Impacts of internal migration experience on health among middle-aged and older adults-Evidence from China. Soc. Sci. Med. 2021, 284, 114236. [Google Scholar] [CrossRef] [PubMed]
- Vendryes, T. Migration constraints and development: Hukou and capital accumulation in China. China Econ. Rev. 2011, 22, 669–692. [Google Scholar] [CrossRef]
- Frazier, M.W.; Li, Y. Stemming the tide of demographic transformation through social inclusion: Can universal pension rights help finance an ageing population. In Handbook of Welfare in China; Edward Elgar Publishing Ltd.: Cheltenham, UK, 2017; pp. 410–428. [Google Scholar] [CrossRef]
- Gao, Q.; Yang, S.; Li, S. Labor contracts and social insurance participation among migrant workers in China. China Econ. Rev. 2012, 23, 1195–1205. [Google Scholar] [CrossRef]
- Mou, J.; Griffiths, S.M.; Fong, H.; Dawes, M.G. Health of China’s rural-urban migrants and their families: A review of literature from 2000 to 2012. Br. Med. Bull. 2012, 106, 19–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, L.; Yuen, L.W.; Buhs, E.S.; Newman, I.M. Depression among Chinese Left-Behind Children: A systematic review and meta-analysis. Child Care Health Dev. 2019, 109, 19–43. [Google Scholar] [CrossRef]
- Ye, J.; Pan, L. Differentiated childhoods: Impacts of rural labor migration on left-behind children in China. J. Peasant. Stud. 2011, 38, 355–377. [Google Scholar] [CrossRef]
- Xu, H.; Xie, Y. The causal effects of rural-to-urban migration on children’s well-being in China. Eur. Sociol. Rev. 2015, 31, 502–519. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Zheng, X.; Parker, M.; Fang, X. Childhood left-behind experience and employment quality of new-generation migrants in China. Popul. Res. Policy Rev. 2020, 39, 691–718. [Google Scholar] [CrossRef]
- Birur, B.; Amrock, E.M.; Shelton, R.C.; Li, L. Sex differences in the peripheral immune system in patients with depression. Front. Psychiatry 2017, 8, 108. [Google Scholar] [CrossRef] [Green Version]
- Gao, W.; Ping, S.; Liu, X. Gender differences in depression, anxiety, and stress among college students: A longitudinal study from China. J. Affect. Disord. 2020, 263, 292–300. [Google Scholar] [CrossRef]
- Ye, J. Stayers in China’s “hollowed-out” villages: A counter narrative on massive rural-urban migration. Popul. Space Place 2018, 24, e2128. [Google Scholar] [CrossRef]
- Zhang, L.; Sharpe, R.V.; Li, S.; Darity, W.A., Jr. Wage differentials between urban and rural-urban migrant workers in China. China Econ. Rev. 2016, 41, 222–233. [Google Scholar] [CrossRef]
- Zhao, Y.; Strauss, J.; Yang, G.; Giles, J.; Hu, P.; Hu, Y.; Wang, Y. China Health and Retirement Longitudinal Study—2011–2012 National Baseline Users’ Guide. In National School of Development; Peking University: Beijing, China, 2013. [Google Scholar]
- Zhao, Y.; Wang, Y.; Chen, X.; Meng, Q.; Tang, Y.; Zhang, T.; Liang, C.; Hou, D.; Liu, X.; Zhang, X.; et al. China Health and Retirement Report. 2019. Available online: http://charls.pku.edu.cn/Public/ashelf/public/uploads/document/public_documents/application/china-health-retirement-report.pdf (accessed on 15 June 2021).
- Su, Y.; Tesfazion, P.; Zhao, Z. Where are the migrants from? Inter- vs. intra-provincial rural-urban migration in China. China Econ. Rev. 2018, 47, 142–155. [Google Scholar] [CrossRef] [Green Version]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged: The Index of ADL: A Standardized measure of biological and psychosocial function. JAMA J. Am. Med. Assoc. 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Shelkey, M.; Wallace, M. Katz index of independence in activities of daily living. J. Gerontol. Nurs. 1999, 25, 8–9. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H. Experiences of falling and depression: Results from the Korean Longitudinal Study of Ageing. J. Affect. Disord. 2021, 281, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Su, H.; Xia, Y.; Zhao, Y. The association between water source and depressive symptoms in China: A cross-sectional and longitudinal study. J. Affect. Disord. 2021, 295, 56–62. [Google Scholar] [CrossRef]
- Karlson, K.B.; Holm, A. Decomposing primary and secondary effects: A new decomposition method. Res. Soc. Stratif. Mobil. 2011, 29, 221–237. [Google Scholar] [CrossRef]
- Lombardo, P.; Jones, W.; Wang, L.; Shen, X.; Goldner, E.M. The fundamental association between mental health and life satisfaction: Results from successive waves of a Canadian national survey. BMC Public Health 2018, 18, 342. [Google Scholar] [CrossRef] [Green Version]
- Cheung, N.W.T. Rural-to-Urban migrant adolescents in Guangzhou, China: Psychological health, victimization, and local and trans-local ties. Soc. Sci. Med. 2013, 93, 121–129. [Google Scholar] [CrossRef]
- Familiar, I.; Borges, G.; Orozco, R.; Medina-Mora, M.E. Mexican migration experiences to the US and risk for anxiety and depressive symptoms. J. Affect. Disord. 2011, 130, 83–91. [Google Scholar] [CrossRef]
- Donato, K.M.; Caron, L.; Hamilton, E. Migration and mental health in Mexico: Domestic migrants, return U.S. migrants, and non-Migrants. Front. Psychiatry 2020, 10, 970. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wang, X.; Liu, Y.; Liu, Y. Migrants’ choice of household split or reunion in China’s urbanisation process: The effect of objective and subjective socioeconomic status. Cities 2020, 102, 102669. [Google Scholar] [CrossRef]
- Liu, Y.; Sangthong, R.; Ingviya, T.; Wan, C. Nothing like living with a family: A qualitative study of subjective well-being and its determinants among migrant and local elderly in Dongguan, China. Int. J. Environ. Res. Public Health 2019, 16, 4874. [Google Scholar] [CrossRef] [Green Version]
- Zhong, B.L.; Liu, T.B.; Huang, J.X.; Fung, H.H.; Chan, S.S.M.; Conwell, Y.; Chiu, H.F.K. Acculturative stress of Chinese rural-to-urban migrant workers: A qualitative study. PLoS ONE 2016, 11, e0157530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, Z.; Sakellariou, C. Social insurance, income and subjective well-being of rural migrants in China—An application of unconditional quantile regression. J. Happiness Stud. 2016, 17, 1635–1657. [Google Scholar] [CrossRef]
- Hall, B.J.; Garabiles, M.R.; Latkin, C.A. Work life, relationship, and policy determinants of health and well-being among Filipino domestic workers in China: A qualitative study. BMC Public Health 2019, 19, 229. [Google Scholar] [CrossRef]
- Wen, M.; Wang, G. Demographic, psychological, and social environmental factors of loneliness and satisfaction among rural-to-urban migrants in Shanghai, China. Int. J. Comp. Sociol. 2009, 50, 155–182. [Google Scholar] [CrossRef]
| Variables | Full Sample (n = 43,854) | With Internal Migration Experience (n = 14,093) | Without Internal Migration Experience (n = 29,761) | p-Value (Chi-square Test/t Test) |
|---|---|---|---|---|
| Depressive symptoms | ||||
| No, n (%) | 28,702 (65.4%) | 9438 (67.0%) | 19,264 (64.7%) | <0.001 |
| Yes, n (%) | 15,152 (34.6%) | 4655 (33.0%) | 10,497 (35.3%) | |
| Gender | ||||
| Female, n (%) | 22,759 (51.9%) | 7180 (50.9%) | 15,579 (52.3%) | 0.006 |
| Male, n (%) | 21,095 (48.1%) | 6913 (49.1%) | 14,182 (47.7%) | |
| Age (years), Mean (SD) | 59.97 (9.56) | 60.31 (9.83) | 59.81 (9.43) | <0.001 |
| Years of education, Mean (SD) | 5.30 (4.20) | 6.13 (4.37) | 4.91 (4.06) | <0.001 |
| Marriage | ||||
| Living without spouse, n (%) | 7542 (17.2%) | 2585 (18.3%) | 4957 (16.7%) | <0.001 |
| Living with spouse, n (%) | 36,312 (82.8%) | 11,508 (81.7%) | 24,804 (83.3%) | |
| First hukou as rural hukou | ||||
| No, n (%) | 3906 (8.9%) | 2036 (14.4%) | 1870 (6.3%) | <0.001 |
| Yes, n (%) | 39,948 (91.1%) | 12,057 (85.6%) | 27,891 (93.7%) | |
| Having changed to urban hukou | ||||
| No, n (%) | 34,344 (78.3%) | 9930 (70.5%) | 24,414 (82.0%) | <0.001 |
| Yes, n (%) | 9510 (21.7%) | 4163 (29.5%) | 5347 (18.0%) | |
| Childhood SES (PCA score) | −0.36 (0.80) | −0.20 (0.93) | −0.44 (0.72) | <0.001 |
| Childhood health status | ||||
| Much less healthy, n (%) | 2253 (5.1%) | 670 (4.8%) | 1583 (5.3%) | <0.001 |
| Somewhat less healthy, n (%) | 3478 (7.9%) | 1178 (8.4%) | 2300 (7.7%) | |
| About average, n (%) | 22,689 (51.7%) | 7027 (49.9%) | 15,662 (52.6%) | |
| Somewhat healthier, n (%) | 8171 (18.6%) | 2837 (20.1%) | 5334 (17.9%) | |
| Much healthier, n (%) | 7263 (16.6%) | 2381 (16.9%) | 4882 (16.4%) | |
| Having difficulty in ADLs | ||||
| No, n (%) | 20,795 (47.4%) | 6743 (47.8%) | 14,052 (47.2%) | 0.220 |
| Yes, n (%) | 23,059 (52.6%) | 7350 (52.2%) | 15,709 (52.8%) | |
| Cognitive function, Mean (SD) | 10.84 (4.43) | 11.54 (4.27) | 10.50 (4.47) | <0.001 |
| Personal income (RMB yuan, in logarithm form), Mean (SD) | 1.38 (3.36) | 1.48 (3.48) | 1.33 (3.30) | <0.001 |
| Family size (number of family members), Mean (SD) | 3.26 (1.86) | 3.17 (1.69) | 3.31 (1.93) | <0.001 |
| Year of survey | ||||
| 2011, n (%) | 12,978 (29.6%) | 4067 (28.9%) | 8911 (29.9%) | 0.001 |
| 2013, n (%) | 14,177 (32.3%) | 4486 (31.8%) | 9691 (32.6%) | |
| 2015, n (%) | 16,699 (38.1%) | 5540 (39.3%) | 11,159 (37.5%) | |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Overall | Men | Women | Age: 45–64 | Age ≥ 65 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Internal migration experience | |||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.07 (1.02–1.12) ** | 1.07 (1.00–1.15) | 1.08 (1.01–1.14) * | 1.12 (1.06–1.19) *** | 0.98 (0.90–1.07) |
| Gender | |||||
| Female | Ref. | Ref. | Ref. | Ref. | Ref. |
| Male | 0.75 (0.72–0.78) *** | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 0.75 (0.71–0.80) *** | 0.72 (0.66–0.78) *** |
| Age | 0.99 (0.98–0.99) *** | 0.98 (0.98–0.99) *** | 0.99 (0.98–0.99) *** | 0.99 (0.99–1.00) ** | 0.97 (0.96–0.98) *** |
| Years of education | 0.99 (0.98–1.00) * | 0.99 (0.98–1.00) * | 0.99 (0.98–1.00) | 0.99 (0.98–1.00) ** | 1.01 (1.00–1.02) |
| Marriage | |||||
| Living without spouse | Ref. | Ref. | Ref. | Ref. | Ref. |
| Living with spouse | 0.72 (0.68–0.77) *** | 0.64 (0.59–0.71) *** | 0.78 (0.72–0.83) *** | 0.65 (0.61–0.70) *** | 0.79 (0.73–0.87) *** |
| First hukou as rural hukou | |||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.25 (1.13–1.37) *** | 1.23 (1.06–1.42) ** | 1.27 (1.12–1.45) *** | 1.17 (1.04–1.31) ** | 1.51 (1.27–1.79) *** |
| Having changed to urban hukou | |||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 0.83 (0.79–0.88) *** | 0.87 (0.80–0.95) ** | 0.80 (0.75–0.87) *** | 0.86 (0.80–0.92) *** | 0.78 (0.71–0.87) *** |
| Childhood SES | 0.89 (0.86–0.92) *** | 0.87 (0.82–0.92) *** | 0.91 (0.87–0.95) *** | 0.89 (0.86–0.93) *** | 0.93 (0.87–0.99) * |
| Childhood health status | 0.82 (0.80–0.84) *** | 0.84 (0.81–0.87) *** | 0.80 (0.78–0.83) *** | 0.80 (0.78–0.83) *** | 0.85 (0.82–0.89) *** |
| Having difficulty in ADLs | |||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 3.44 (3.25–3.64) *** | 3.50 (3.23–3.78) *** | 3.41 (3.15–3.69) *** | 3.43 (3.21–3.66) *** | 3.40 (3.06–3.78) *** |
| Cognitive function | 0.93 (0.93–0.94) *** | 0.93 (0.92–0.94) *** | 0.93 (0.92–0.94) *** | 0.93 (0.92–0.94) *** | 0.93 (0.92–0.94) *** |
| Personal income | 0.96 (0.96–0.97) *** | 0.96 (0.95–0.97) *** | 0.97 (0.96–0.98) *** | 0.96 (0.96–0.97) *** | 0.98 (0.96–1.01) |
| Family size | 0.98 (0.97–0.99) ** | 0.99 (0.97–1.01) | 0.98 (0.96–0.99) ** | 0.98 (0.96–0.99) ** | 0.99 (0.97–1.01) |
| Year of survey | |||||
| 2011 | Ref. | Ref. | Ref. | Ref. | Ref. |
| 2013 | 0.40 (0.38–0.43) *** | 0.43 (0.39–0.47) *** | 0.38 (0.35–0.42) *** | 0.42 (0.39–0.45) *** | 0.36 (0.32–0.40) *** |
| 2015 | 0.42 (0.40–0.45) *** | 0.44 (0.40–0.48) *** | 0.41 (0.38–0.45) *** | 0.44 (0.41–0.47) *** | 0.39 (0.35–0.43) *** |
| Pseudo-R-squared | 0.109 | 0.097 | 0.090 | 0.115 | 0.097 |
| Number of observations | 43,854 | 21,095 | 22,759 | 30,577 | 13,277 |
| Model 6 | Model 7 | Model 8 | |
|---|---|---|---|
| Always Rural hukou | Changed to Urban hukou | Always Urban hukou | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Internal migration experience | |||
| No | Ref. | Ref. | Ref. |
| Yes | 1.13 (1.07, 1.19) *** | 1.01 (0.91, 1.11) | 0.95 (0.81, 1.12) |
| Control variables | Yes | Yes | Yes |
| Pseudo-R-squared | 0.099 | 0.106 | 0.083 |
| Number of observations | 30,417 | 9499 | 3938 |
| Model 9 | Model 10 | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Frequency of internal migration experience | ||
| No migration experience | Ref. | – |
| Once | 1.09 (1.02–1.15) ** | – |
| Twice | 1.11 (1.03–1.19) ** | – |
| Three times or above | 1.01 (0.92–1.10) | – |
| Age at the first migration experience | ||
| No migration experience | – | Ref. |
| 0–17 years old | – | 1.08 (0.99–1.18) |
| 18–34 years old | – | 1.05 (0.99–1.11) |
| 35 years old or above | – | 1.14 (1.05–1.25) ** |
| Control variables | Yes | Yes |
| Pseudo-R-squared | 0.109 | 0.109 |
| Number of observations | 43,854 | 43,854 |
| Chronic Disease | Physical Injury | Medical Expenditure | Pension Insurance | Low Frequency of Parent–Child Interaction | |
|---|---|---|---|---|---|
| Estimated value (components of indirect effects) | 0.013 (0.008–0.018) *** | 0.005 (0.002–0.008) *** | 0.006 (0.003–0.009) *** | 0.004 (0.002–0.006) *** | 0.003 (0.001–0.006) ** |
| Mediating effects (%) | 17.98% | 7.04% | 7.98% | 4.91% | 4.45% |
| Total effect | 0.073 (0.024–0.123) ** | ||||
| Direct effect | 0.042 (−0.007–0.092) | ||||
| Indirect effect | 0.031 (0.024–0.038) *** | ||||
| Model 11 | Model 12 | Model 13 | Model 14 | |
|---|---|---|---|---|
| Depressive Symptoms (Balanced Panel) | CES-D Score (OLS) | Self-Reported Health (Ordered Logit) | Life Satisfaction (Ordered Logit) | |
| OR (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | |
| Internal migration experience | ||||
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.09 (1.03, 1.16) ** | 0.17 (0.05–0.29) ** | −0.12 (−0.16–−0.08) *** | −0.10 (−0.14–−0.06) *** |
| Control variables | Yes | Yes | Yes | Yes |
| R-squared/Pseudo-R-squared | 0.105 | 0.176 | 0.063 | 0.035 |
| Number of observations | 30,372 | 43,854 | 43,854 | 43,854 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, X.; Zhang, Y.; Chen, Y.; Fang, X. Internal Migration Experience and Depressive Symptoms among Middle-Aged and Older Adults: Evidence from China. Int. J. Environ. Res. Public Health 2022, 19, 303. https://doi.org/10.3390/ijerph19010303
Zheng X, Zhang Y, Chen Y, Fang X. Internal Migration Experience and Depressive Symptoms among Middle-Aged and Older Adults: Evidence from China. International Journal of Environmental Research and Public Health. 2022; 19(1):303. https://doi.org/10.3390/ijerph19010303
Chicago/Turabian StyleZheng, Xiaodong, Yue Zhang, Yu Chen, and Xiangming Fang. 2022. "Internal Migration Experience and Depressive Symptoms among Middle-Aged and Older Adults: Evidence from China" International Journal of Environmental Research and Public Health 19, no. 1: 303. https://doi.org/10.3390/ijerph19010303
APA StyleZheng, X., Zhang, Y., Chen, Y., & Fang, X. (2022). Internal Migration Experience and Depressive Symptoms among Middle-Aged and Older Adults: Evidence from China. International Journal of Environmental Research and Public Health, 19(1), 303. https://doi.org/10.3390/ijerph19010303







