Long-Term Follow-Up of Device-Assisted Clampless Off-Pump Coronary Artery Bypass Grafting Compared with Conventional On-Pump Technique
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Criteria to Choose C-OPCAB and C-CABG
2.3. Surgical Strategy and Patients’ Mangement
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. In-Hospital Outcomes
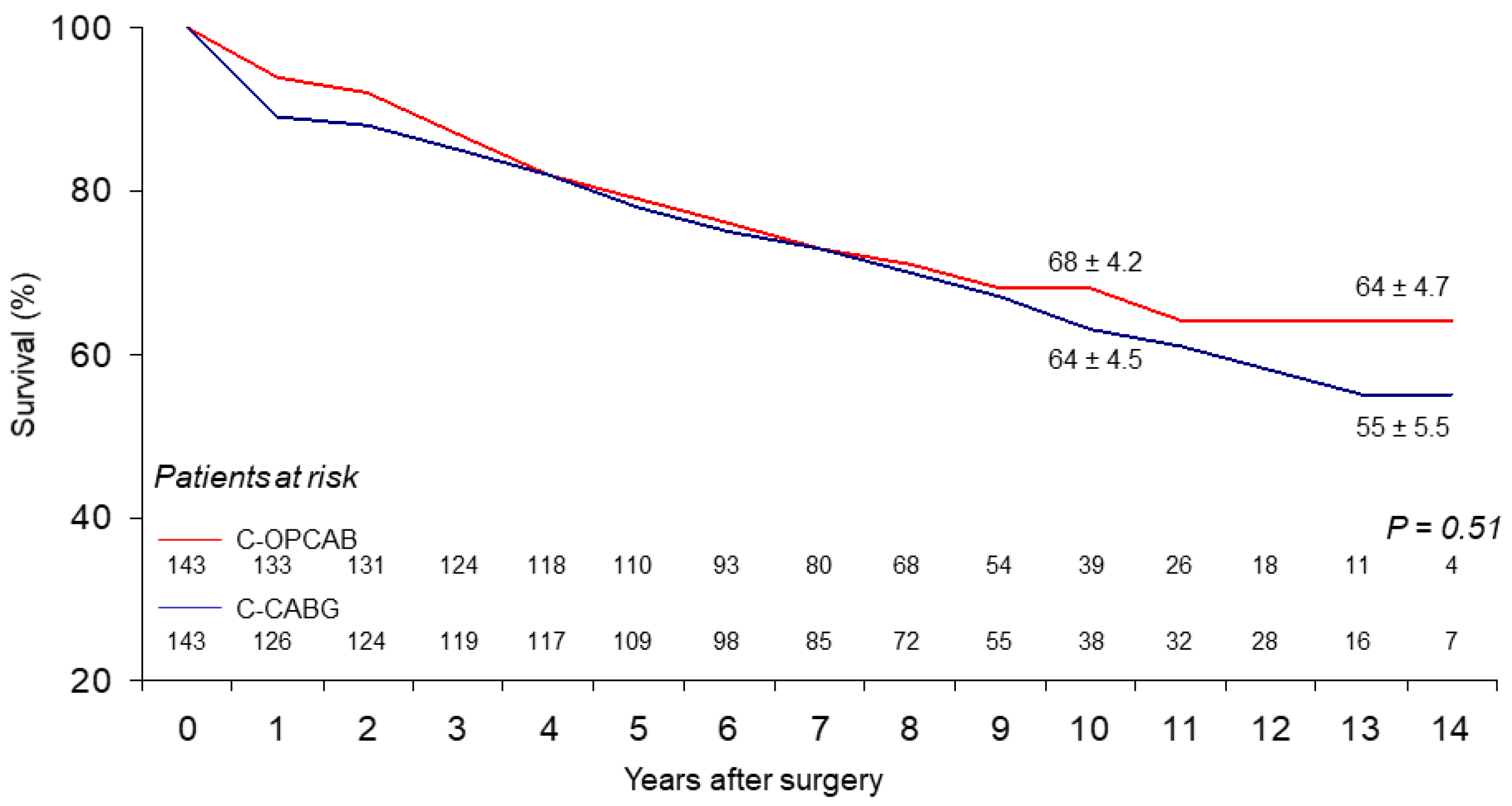
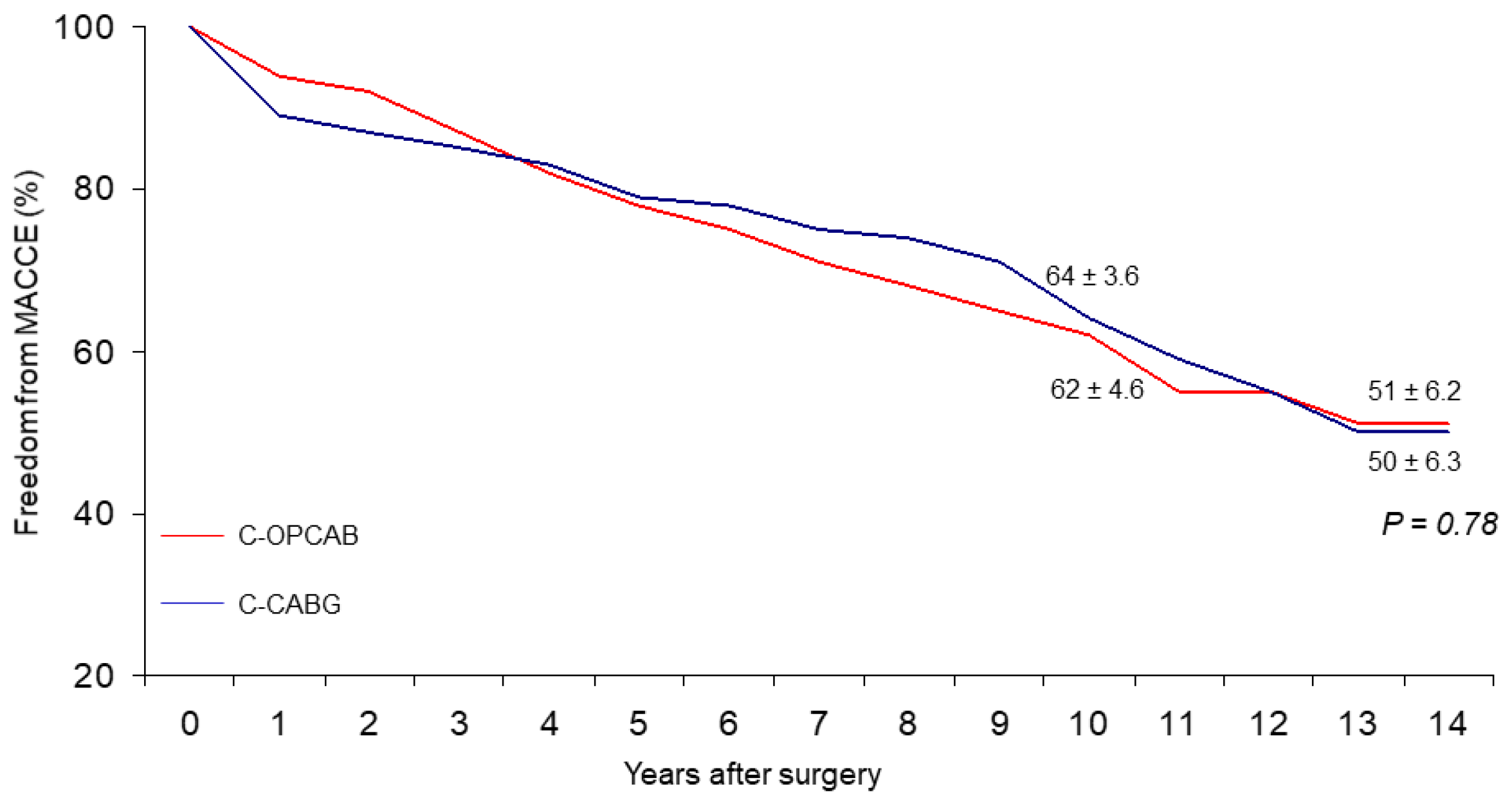
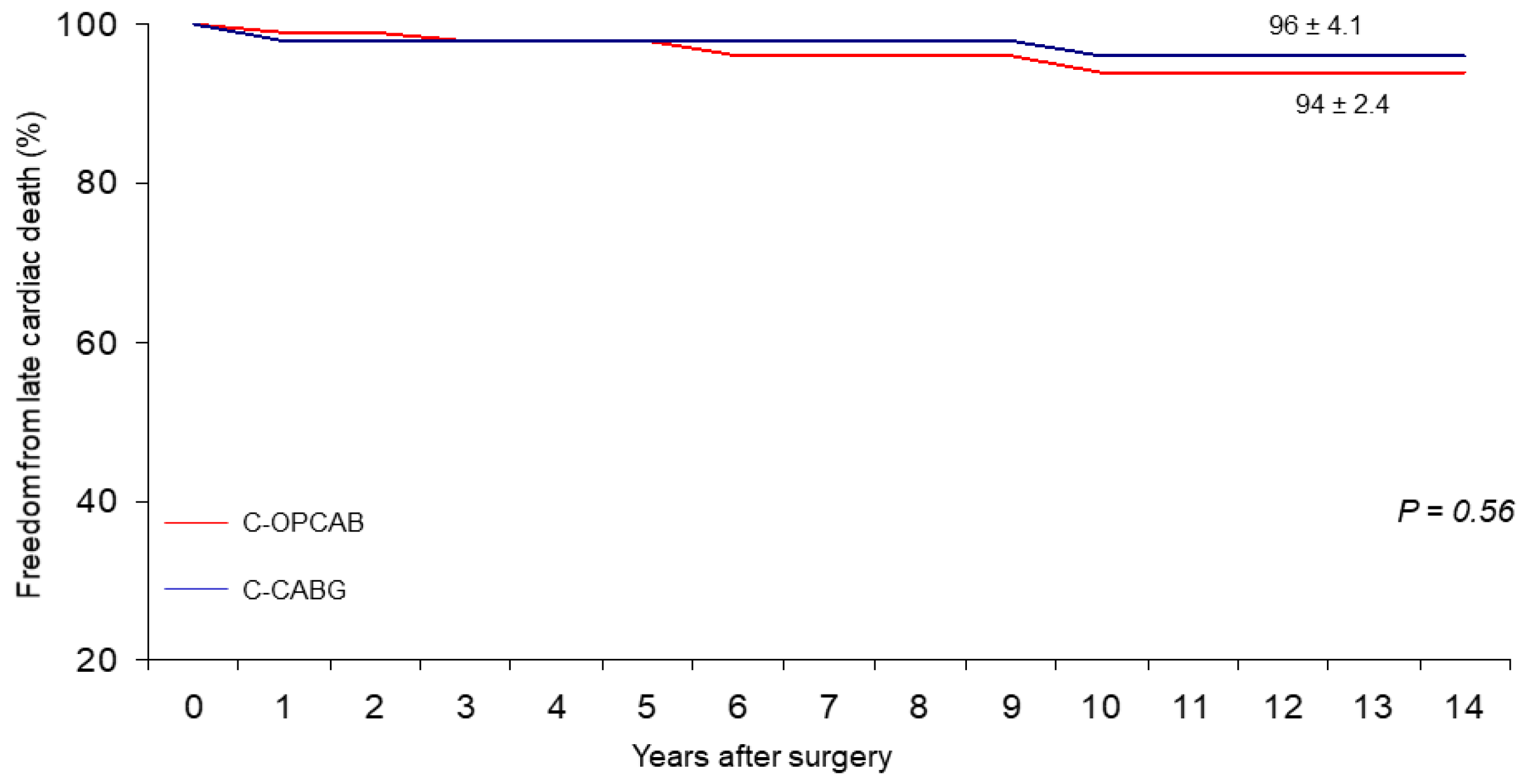
3.2. Follow-Up Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khan, N.E.; De Souza, A.; Mister, R.; Flather, M.; Clague, J.; Davies, S.; Collins, P.; Wang, D.; Sigwart, U.; Pepper, J. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N. Engl. J. Med. 2004, 350, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Nardi, P.; Pisano, C.; Bertoldo, F.; Vacirca, S.R.; Saitto, G.; Costantino, A.; Bovio, E.; Pellegrino, A.; Ruvolo, G. Warm blood cardioplegia versus cold crystalloid cardioplegia for myocardial protection during coronary artery bypass grafting surgery. Cell Death Discov. 2018, 4, 23. [Google Scholar] [CrossRef] [PubMed]
- Nardi, P.; Pellegrino, A.; Bassano, C.; Mani, R.; Chiariello, G.A.; Zeitani, J.; Chiariello, L. The fate at mid-term follow-up of the on-pump vs. off-pump coronary artery bypass grafting surgery. J. Cardiovasc. Med. 2015, 16, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Hannan, E.L.; Wu, C.; Smith, C.R.; Higgins, R.S.; Carlson, R.E.; Culliford, A.T.; Gold, J.P.; Jones, R.H. Off-pump versus on-pump coronary artery bypass graft surgery: Differences in short-term outcomes and in long term mortality and need for subsequent revascularization. Circulation 2007, 116, 1145–1152. [Google Scholar] [CrossRef]
- Lemma, M.G.; Coscioni, E.; Tritto, F.P.; Centofanti, P.; Fondacone, C.; Salica, A.; Rossi, A.; De Santo, T.; Di Benedetto, G.; Piazza, L.; et al. On-pump versus off-pump coronary artery bypass surgery in high-risk patients: Operative results of a prospective randomized trial (on-off study). J. Thorac. Cardiovasc. Surg. 2012, 143, 625–631. [Google Scholar] [CrossRef]
- Börgermann, J.; Hakim, K.; Renner, A.; Parsa, A.; Aboud, A.; Becker, T.; Masshoff, M.; Zittermann, A.; Gummert, J.F.; Kuss, O. Clampless off-pump versus conventional coronary artery revascularization: A propensity score analysis of 788 patients. Circulation 2012, 126 (Suppl. 1), S176–S182. [Google Scholar] [CrossRef]
- Hedberg, M.; Boivie, P.; Engstroem, K.G. Early and delayed stroke after coronary surgery- an analysis of risk factors and the impact on short- and long-term survival. Eur. J. Cardiothorac. Surg. 2011, 40, 379–387. [Google Scholar] [CrossRef]
- Møller, C.H.; Penninga, L.; Wetterslev, J.; Steinbrüchel, D.A.; Gluud, C. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst. Rev. 2012, 3, CD007224. [Google Scholar] [CrossRef]
- Lamy, A.; Devereaux, P.; Prabhakaran, D.; Taggart, D.P.; Hu, S.; Paolasso, E.; Straka, Z.; Piegas, L.; Akar, A.R.; Jain, A.R.; et al. CORONARY Investigators. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N. Engl. J. Med. 2012, 366, 1489–1497. [Google Scholar] [CrossRef]
- Møller, C.H.; Perko, M.J.; Lund, J.T.; Steinbrüchel, D.A.; Andersen, L.W.; Kelbæk, H.; Madsen, J.K.; Winkel, P.; Gluud, C. No major differences in 30-day outcomes in high-risk patients randomized to off-pump versus on-pump coronary bypass surgery: The best bypass surgery trial. Circulation 2010, 121, 498–504. [Google Scholar] [CrossRef]
- Lim, E.; Drain, A.; Davies, W.; Edmonds, L.; Rosengard, B.R. A systematic review of randomized trials comparing revascularization rate and graft patency of off-pump and conventional coronary surgery. J. Thorac. Cardiovasc. Surg. 2006, 132, 1409–1413. [Google Scholar] [CrossRef]
- Ivanov, J.; Borger, M.A.; Tu, J.V.; Rao, V.; David, T.E. Mid-term outcomes of off-pump versus on-pump coronary artery bypass graft surgery. Can. J. Cardiol. 2008, 24, 279–284. [Google Scholar] [CrossRef][Green Version]
- Thourani, V.H.; Guyton, R.A. Graft patency after off-pump coronary artery bypass surgery. Circulation 2012, 125, 2806–2808. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Afilalo, J.; Rasti, M.; Ohayon, S.M.; Shimony, A.; Eisenberg, M.J. Off-pump vs. on-pump coronary artery bypass surgery: An updated meta-analysis and meta-regression of randomized trials. Eur. Heart J. 2012, 33, 1257–1267. [Google Scholar] [CrossRef] [PubMed]
- Shroyer, A.L.; Grover, F.L.; Hattler, B.; Collins, J.F.; McDonald, G.O.; Kozora, E.; Lucke, J.C.; Baltz, J.H.; Novitzky, D. Veterans Affairs Randomized On/Off Bypass (ROOBY) Study. On-Pump versus Off-Pump Coronary Artery Bypass Surgery. N. Engl. J. Med. 2009, 361, 1827–1837. [Google Scholar] [CrossRef]
- Hattler, B.; Messenger, J.C.; Shroyer, A.L.; Collins, J.F.; Haugen, S.J.; Garcia, J.A.; Baltz, J.H.; Cleveland, J.C., Jr.; Novitzky, D.; Grover, F.L. Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. Off-pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: Results from the Veterans Affairs Randomized On/Off Bypass (ROOBY) trial. Circulation 2012, 125, 2827–2835. [Google Scholar]
- Angelini, G.D.; Culliford, L.; Smith, D.K.; Hamilton, M.C.; Murphy, G.J.; Ascione, R.; Baumbach, A.; Reeves, B.C. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: Long-term follow-up of 2 randomized controlled trials. J. Thorac. Cardiovasc. Surg. 2009, 137, 295–303. [Google Scholar] [CrossRef]
- Widimsky, P.; Straka, Z.; Stros, P. One-year coronary bypass graft patency: A randomized comparison between off-pump and on-pump surgery angiographic results of the PRAGUE-4 trial. Circulation 2004, 110, 3418–3423. [Google Scholar] [CrossRef]
- Filardo, G.; Grayburn, P.A.; Hamilton, C.; Hebeler, R.F.; Cooksey, W.B.; Hamman, B. Comparing long-term survival between patients undergoing off-pump and on-pump coronary artery bypass graft operations. Ann. Thorac. Surg. 2011, 92, 571–578. [Google Scholar] [CrossRef]
- Sousa Uva, M.; Cavaco, S.; Oliveira, A.G.; Matias, F.; Silva, C.; Mesquita, A.; Aguiar, P.; Bau, J.; Pedro, A.; Magalhaes, M.P. Early graft patency after off-pump and on-pump coronary bypass surgery: A prospective randomized study. Eur. Heart J. 2010, 31, 2492–2499. [Google Scholar] [CrossRef]
- Gaudino, M.; Angelini, G.D.; Antoniades, C.; Bakaeen, F.; Benedetto, U.; Calafiore, A.M.; Di Franco, A.; Di Mauro, M.; Fremes, S.E.; Girardi, L.N.; et al. Off-Pump Coronary Artery Bypass Grafting: 30 Years of Debate. J. Am. Heart Assoc. 2018, 7, e009934. [Google Scholar] [CrossRef] [PubMed]
- Marczin, N.; Raja, S.G. Off-pump coronary artery bypass grafting. AME Med. J. 2020, 5, 21. [Google Scholar] [CrossRef]
- Neumann, A.; Vöhringer, L.; Fischer, J.; Mustafi, M.; Schneider, W.; Krüger, T.; Schlensak, C. Off-Pump Coronary Artery Bypass Grafting in Acute Coronary Syndrome: Focus on Safety and Completeness of Revascularization. Thorac. Cardiovasc. Surg. 2020, 68, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Lazar, H.L. Should Off-Pump Coronary Artery Bypass Grafting Be Abandoned? Circulation 2013, 128, 406. [Google Scholar] [CrossRef]
- Guida, G.A.; Chivasso, P.; Fudulu, D.; Rapetto, F.; Sedmakov, C.; Marsico, R.; Zakkar, M.; Bryan, A.J.; Angelini, G.D. Off- pump coronary artery bypass grafting in high-risk patients: A review. J. Thorac. Dis. 2016, 8 (Suppl. 10), S795–S798. [Google Scholar] [CrossRef]
- Bassano, C.; Bovio, E.; Uva, F.; Iacobelli, S.; Iasevoli, N.; Farinaccio, A.; Ruvolo, G. Partially anaortic clampless off-pump coronary artery bypass prevents neurologic injury compared to on-pump coronary surgery: A propensity score-matched study on 286 patients. Heart Vessels 2016, 31, 1412–1417. [Google Scholar] [CrossRef][Green Version]
- Bassano, C.; Bovio, E.; Sperandio, M.; Uva, F.; Farinaccio, A.; Prati, P.; Chiariello, L. Five-Year Cinical Outcome and Patency Rate of Device-Dependent Venous Grafts After Clampless OPCAB with PAS-Port Automated Proximal Anastomosis: The PAPA Study. J. Card Surg. 2014, 29, 325–332. [Google Scholar] [CrossRef]
- Lamy, A.; Devereaux, P.J.; Prabhakaran, D.; Taggart, D.P.; Hu, S.; Straka, Z.; Piegas, L.S.; Avezum, A.; Akar, A.R.; Lanas Zanetti, F.; et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N. Engl. J. Med. 2016, 375, 2359–2368. [Google Scholar] [CrossRef]
- Shroyer, A.L.; Hattler, B.; Wagner, T.H.; Collins, J.F.; Baltz, J.H.; Quin, J.A.; Almassi, G.H.; Kozora, E.; Bakaeen, F.; Cleveland, J.C., Jr.; et al. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N. Engl. J. Med. 2017, 377, 623–632. [Google Scholar] [CrossRef]
- Lattouf, O.M.; Thourani, V.H.; Kilgo, P.D.; Halkos, M.E.; Baio, K.T.; Myung, R.; Cooper, W.A.; Guyton, R.A.; Puskas, J.D. Influence of on-pump versus off-pump techniques and completeness of revascularization on long-term survival after coronary artery bypass. Ann. Thorac. Surg. 2008, 86, 797–805. [Google Scholar] [CrossRef]
- Kirmani, B.H.; Holmes, M.V.; Muir, A.D. Long-term survival and freedom from reintervention after off-pump coronary artery bypass grafting: A propensity-matched study. Circulation 2016, 134, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Smart, N.A.; Dieberg, G.; King, N. Long-term outcomes of on- versus off-pump coronary artery bypass grafting. J. Am. Coll. Cardiol. 2018, 71, 983–991. [Google Scholar] [CrossRef] [PubMed]
| Variables | Overall Population (n = 366) | Propensity Score-Matched (n = 286) | ||||
|---|---|---|---|---|---|---|
| C-OPCAB (n = 223) | C-CABG (n = 143) | p-Value | C-OPCAB (n = 143) | C-CABG (n = 143) | p-Value | |
| Age, years | 67.9 ± 9.7 | 67.4 ± 9.4 | 0.90 | 67.4 ± 9.4 | 67.4 ± 9.4 | 0.86 |
| Female gender (%) | 16.2 | 16.1 | 0.97 | 16.1 | 16.1 | 1 |
| BMI (mean v. Kg/m2) | 27.2 ± 3.7 | 27.5 ± 3.5 | 0.33 | 27.2 ± 3.7 | 27.5 ± 3.5 | 0.36 |
| Hypertension (%) | 85.1 | 89.5 | 0.23 | 88.1 | 89.5 | 0.71 |
| Smoking habit (%) | 28.8 | 31.5 | 0.59 | 29.4 | 31.5 | 0.71 |
| Diabetes mellitus (%) | 33.8 | 44.8 | 0.03 | 41.3 | 44.8 | 0.53 |
| LVEF (mean v.) | 0.51 ± 0.85 | 0.50 ± 0.99 | 0.03 | 0.52 ± 0.89 | 0.51 ± 0.99 | 0.46 |
| Recent MI (%) | 37.4 | 35 | 0.64 | 35.7 | 35 | 0.90 |
| Previous PCI (%) | 18 | 9.8 | 0.03 | 9.1 | 9.8 | 0.81 |
| Renal failure (%) * | 5.4 | 2.8 | 0.23 | 2.8 | 2.8 | 1 |
| Previous CA stent (%) | 2.7 | 2.8 | 0.96 | 2.1 | 2.8 | 0.65 |
| CA stenosis 50–70% (%) | 16.7 | 25.9 | 0.03 | 22.4 | 25.9 | 0.43 |
| Stroke/TIA (%) | 10.8 | 10.5 | 0.92 | 11.2 | 10.5 | 0.85 |
| LMD ≥ 50% (%) | 37.8 | 31.5 | 0.21 | 30.1 | 31.5 | 0.70 |
| PVD (%) | 27.5 | 39.9 | 0.01 | 35.7 | 39.9 | 0.40 |
| Urgency (%) | 30.2 | 28.7 | 0.76 | 31.5 | 28.7 | 0.60 |
| Adverse Events | C-OPCAB (n = 141) | C-CABG (n = 136) | p-Value |
|---|---|---|---|
| Death for any causes, n (%) | 40 (28.4) | 40 (29.4) | NS |
| New MI, n (%) | 4 (2.9) | 7 (5.0) | NS |
| New revascularization, n (%) | 4 (2.9) | 9 (6.4) | NS |
| Stroke, n (%) | 1 (0.7) | 0 | NS |
| Pacemaker/ICD implantation, n (%) | 3 (2.1) | 10 (7.4) | NS |
| Survival | |||
| Covariates | HR | 95% CI | p-Value |
| Age at operation time (70.3 vs. 65.7 yrs) | 4.5 | 1.041–1.109 | <0.0001 |
| Preoperative LVEF (0.50 vs. 0.52) | −2.4 | 0.940–0.993 | 0.015 |
| Late cardiac death | |||
| Covariate | |||
| Preoperative LVEF (0.49 vs. 0.52) | −4.1 | 0.887–0.959 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bassano, C.; Nardi, P.; Buioni, D.; Asta, L.; Pisano, C.; Bertoldo, F.; Altieri, C.; Ruvolo, G. Long-Term Follow-Up of Device-Assisted Clampless Off-Pump Coronary Artery Bypass Grafting Compared with Conventional On-Pump Technique. Int. J. Environ. Res. Public Health 2022, 19, 275. https://doi.org/10.3390/ijerph19010275
Bassano C, Nardi P, Buioni D, Asta L, Pisano C, Bertoldo F, Altieri C, Ruvolo G. Long-Term Follow-Up of Device-Assisted Clampless Off-Pump Coronary Artery Bypass Grafting Compared with Conventional On-Pump Technique. International Journal of Environmental Research and Public Health. 2022; 19(1):275. https://doi.org/10.3390/ijerph19010275
Chicago/Turabian StyleBassano, Carlo, Paolo Nardi, Dario Buioni, Laura Asta, Calogera Pisano, Fabio Bertoldo, Claudia Altieri, and Giovanni Ruvolo. 2022. "Long-Term Follow-Up of Device-Assisted Clampless Off-Pump Coronary Artery Bypass Grafting Compared with Conventional On-Pump Technique" International Journal of Environmental Research and Public Health 19, no. 1: 275. https://doi.org/10.3390/ijerph19010275
APA StyleBassano, C., Nardi, P., Buioni, D., Asta, L., Pisano, C., Bertoldo, F., Altieri, C., & Ruvolo, G. (2022). Long-Term Follow-Up of Device-Assisted Clampless Off-Pump Coronary Artery Bypass Grafting Compared with Conventional On-Pump Technique. International Journal of Environmental Research and Public Health, 19(1), 275. https://doi.org/10.3390/ijerph19010275









