Interactions with Home and Health Environments Discourage Physical Activity: Reports from Children with Complex Congenital Heart Disease and Their Parents
Abstract
:1. Introduction
2. Methods
2.1 Research Approach
2.2. Study Design
2.3. Participants
2.4. Focus Groups and Interviews
2.5. Data Analyses
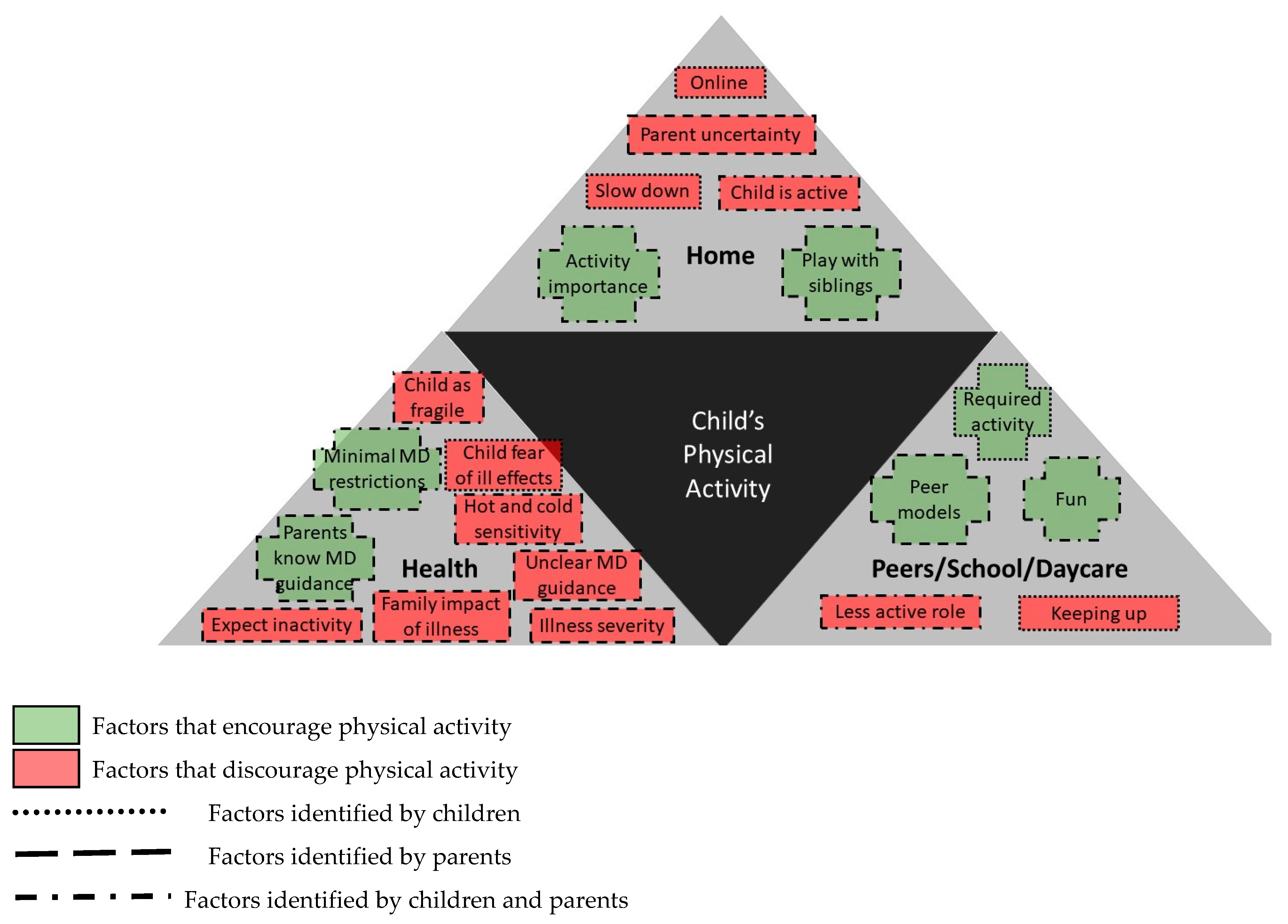
3. Results
3.1. Peer Physical and Social Environments (School/Daycare) Support Physical Activity
3.2. The Social Home Environment Encourages and Discourages Activity
Girl10: ‘Cause there’s a hill … in the wintertime there’s snow and we can slide down. And in the summertime we go to a really close park.
Mom13: I want her to think of physical activity first rather than second. Generally, we have to encourage her to be physically active. … She would rather watch TV or play computer games, etc. But when she’s being active, she enjoys it, it is just the second thought, not the first thought.
Dad5: Convincing him that it’s a good thing to do. … When he’s comfortable that’s when he engages. If you try to force him, it’s impossible. He freaks out.
Boy20: I really wanted to take baseball but it’s “No”, my Mom and Dad said, because um, like, in case the ball comes towards me and it hits my chest.
Mom3: His father is like, “oh, I am scared”.Boy3: Nothing will happen. I play soccer every day and I’m good at it. I got nine goals.Researcher: So, did you play on a soccer team this summer?Boy3: [shakes head] My dad and, uh, like when we play soccer, it’s rough. … But I just keep passing. Two persons coming and I just go through them and then they bump into each other.
Girl8: Just keep trying and if you need a break just slow down or stop.Boy1: I think you need to be careful sometimes, like me.Boy6: Run about a 100m and then stop … and then run again.
3.3. Health Environment Interactions were Interpreted as Discouraging Physical Activity
Mom A: We were told by [cardiologist] that if she is physically not capable of doing something her body will just naturally slow down or suggest that she sit down and rest. She won’t have a choice. So, she can go as hard as she wants, as much as she wants. That body itself will let her know if it’s had too much, but no limitations.
Dad D: At Sick Kids, they said he’s going to be lethargic. They said he’s going to be tired all the time or like …Dad B: Exhausted.Mom D: It hasn’t happened. It never happened.
Mom A: If she says, “I can’t do something ‘cause I’m tired” or, you know, she’ll put her hand to her chest and, of course, I immediately think, ‘oh, so here’s one of those parenting moments. Do I force her to do it ‘cause I think she’s playing with me or, you know, or do you allow her that opportunity or not to let her do it?’.
Mom E: I have to remember when he’s running, he’s going to sweat. Profusely, potentially, if that should be just his natural thing. But then I get scared because then I see the sweating and then I have to [chuckle] remind myself that his heart rate will increase ‘cause he’s physically active. But I’m always going there and I’m checking it and, you know, seeing what his heart rate is and things. … I have to remind myself there’s all those normal things, but it’s always in the back of my mind … So, it is very anxious for me. And I think I’m growing out of it ‘cause you can see by his scraped knees and stuff that [chuckles] he is getting active. But I’m having separation anxiety between the role of constantly mother hen-ing over him and realizing that exercise is good and I have to allow him to do that. So, it’s a balancing act for me.
Mom A: She just reached an age where sleepovers are happening. A couple of parents have said, “Do I need to know anything? If anything were to happen what do I do?”
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hillman, C.H.; Biggan, J.R. A Review of Childhood Physical Activity, Brain, and Cognition: Perspectives on the Future. Pediatr. Exerc. Sci. 2017, 29, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loprinzi, P.D.; Cardinal, B.J.; Loprinzi, K.L.; Lee, H. Benefits and Environmental Determinants of Physical Activity in Children and Adolescents. Obes. Facts 2012, 5, 597–610. [Google Scholar] [CrossRef]
- Dimitri, P.; Joshi, K.; Jones, N. Moving more: Physical activity and its positive effects on long term conditions in children and young people. Arch. Dis. Child. 2020, 105, 1035–1040. [Google Scholar] [CrossRef]
- Massin, M.M.; Hövels-Gürich, H.H.; Gérard, P.; Seghaye, M.C.; Hovels-Gurich, H.H.; Gerard, P.; Seghaye, M.C.; Hövels-Gürich, H.H.; Gérard, P.; Seghaye, M.C. Physical activity patterns of children after neonatal arterial switch operation. Ann. Thorac. Surg. 2006, 81, 665–670. [Google Scholar] [CrossRef]
- Hovels-Gurich, H.H.; Konrad, K.; Skorzenski, D.; Nacken, C.; Minkenberg, R.; Messmer, B.J.; Seghaye, M.C.; Hövels-Gürich, H.H.; Konrad, K.; Skorzenski, D.; et al. Long-term neurodevelopmental outcome and exercise capacity after corrective surgery for tetralogy of Fallot or ventricular septal defect in infancy. Ann. Thorac. Surg. 2006, 81, 958–966. [Google Scholar] [CrossRef]
- McCrindle, B.W.; Williams, R.V.; Mital, S.; Clark, B.J.; Russell, J.L.; Klein, G.; Eisenmann, J.C. Physical activity levels in children and adolescents are reduced after the Fontan procedure, independent of exercise capacity, and are associated with lower perceived general health. Arch. Dis. Child. 2007, 92, 509–514. [Google Scholar] [CrossRef] [Green Version]
- Reybrouck, T.; Mertens, L. Physical performance and physical activity in grown-up congenital heart disease. Eur. J. Cardiovasc Prev. Rehabil. 2005, 12, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Longmuir, P.E.; Wang, S.; Timmons, B.W.; Mondal, T.; Cinanni, N.L.; Di Cristofaro, N.A.; Dillenburg, R.; Adamo, K.; Tremblay, M.S.; Lee, S. Inactive Lifestyles among Young Children with Innocent Murmurs or Congenital Heart Disease Regardless of Disease Severity or Treatment. Can. J. Cardiol. 2021. Revision submitted. [Google Scholar]
- Longmuir, P.E.; Turner, J.A.P.; Rowe, R.D.; Olley, P.M. Postoperative exercise rehabilitation benefits children with congenital heart disease. Clin. Investig. Med. 1985, 8, 232–238. [Google Scholar]
- Rhodes, J.; Curran, T.J.; Camil, L.; Rabideau, N.; Fulton, D.R.; Gauthier, N.S.; Gauvreau, K.; Jenkins, K.J. Impact of cardiac rehabilitation on the exercise function of children with serious congenital heart disease. Pediatrics 2005, 116, 1339–1345. [Google Scholar] [CrossRef] [PubMed]
- Opocher, F.; Varnier, M.; Sanders, S.P.; Tosoni, A.; Zaccaria, M.; Stellin, G.; Milanesi, O. Effects of aerobic exercise training in children after the Fontan operation. Am. J. Cardiol. 2005, 95, 150–152. [Google Scholar] [CrossRef]
- Rhodes, J.; Curran, T.J.; Camil, L.; Rabideau, N.; Fulton, D.R.; Gauthier, N.S.; Gauvreau, K.; Jenkins, K.J. Sustained effects of cardiac rehabilitation in children with serious congenital heart disease. Pediatrics 2006, 118, e586–e593. [Google Scholar] [CrossRef]
- Longmuir, P.E.; Tremblay, M.S.; Goode, R.C. Postoperative exercise training develops normal levels of physical activity in a group of children following cardiac surgery. Pediatr. Cardiol. 1990, 11, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Longmuir, P.E.; Russell, J.L.; Corey, M.; Faulkner, G.; McCrindle, B.W. Factors associated with the physical activity level of children who have the Fontan procedure. Am. Heart J. 2011, 161, 411–417. [Google Scholar] [CrossRef]
- Voss, C.; Duncombe, S.L.; Dean, P.H.; De Souza, A.M.; Harris, K.C. Physical activity and sedentary behavior in children with congenital heart disease. J. Am. Heart Assoc. 2017, 6, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization Determinants of Health. Available online: https://www.who.int/news-room/q-a-detail/determinants-of-health (accessed on 14 March 2021).
- Van Deutekom, A.W.; Lewandowski, A.J. Physical activity modification in youth with congenital heart disease: A comprehensive narrative review. Pediatr. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Moola, F.; Faulkner, G.E.J.; Kirsh, J.A.; Kilburn, J. Physical activity and sport participation in youth with congenital heart disease: Perceptions of children and parents. Adapt. Phys. Act. Q. 2007, 25, 49–70. [Google Scholar] [CrossRef] [Green Version]
- Bennett, E.V.; Voss, C.; Faulkner, G.; Harris, K.C. From ‘it makes me feel free’ to ‘they won’t let me play’: The body and physical activity-related perceptions and experiences of children with congenital heart disease and their parents. Qual. Res. Sport. Exerc. Health 2021, 13, 325–341. [Google Scholar] [CrossRef]
- Trigueros, R.; Aguilar-Parra, J.M.; Cangas, A.J.; Fernández-Batanero, J.M.; Álvarez, J.F. The Influence of the Social Context on Motivation towards the Practice of Physical Activity and the Intention to be Physically Active. Int. J. Environ. Res. Public Health 2019, 16, 4212. [Google Scholar] [CrossRef] [Green Version]
- Casey, F.A.; Craig, B.G.; Mulholland, H.C. Quality of life in surgically palliated complex congenital heart disease. Arch. Dis. Child. 1994, 70, 382–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longmuir, P.E.; McCrindle, B.W. Physical activity restrictions for children after the Fontan operation: Disagreement between parent, cardiologist, and medical record reports. Am. Heart J. 2009, 157, 853–859. [Google Scholar] [CrossRef] [PubMed]
- Takken, T.; Giardini, A.; Reybrouck, T.; Gewillig, M.; Hövels-Gürich, H.H.H.; Longmuir, P.E.; McCrindle, B.W.; Paridon, S.M.; Hager, A. Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: A report from the Exercise, Basic & Translational Research Section of the European Association of Cardiovascular Preve. Eur. J. Prev. Cardiol. 2012, 19, 1034–1065. [Google Scholar] [CrossRef]
- Sparacino, P.S.; Tong, E.M.; Messias, D.K.; Foote, D.; Chesla, C.A.; Gilliss, C.L. The dilemmas of parents of adolescents and young adults with congenital heart disease. Hear. Lung 1997, 26, 187–195. [Google Scholar] [CrossRef]
- Moola, F.; Fusco, C.; Kirsh, J.A. The perceptions of caregivers toward physical activity and health in youth with congenital heart disease. Qual. Health Res. 2011, 21, 278–291. [Google Scholar] [CrossRef] [PubMed]
- Jaeschke, L.; Steinbrecher, A.; Luzak, A.; Puggina, A.; Aleksovska, K.; Buck, C.; Burns, C.; Cardon, G.; Carlin, A.; Chantal, S.; et al. Socio-cultural determinants of physical activity across the life course: A ‘Determinants of Diet and Physical Activity’ (DEDIPAC) umbrella systematic literature review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 173. [Google Scholar] [CrossRef] [Green Version]
- Carlin, A.; Perchoux, C.; Puggina, A.; Aleksovska, K.; Buck, C.; Burns, C.; Cardon, G.; Chantal, S.; Ciarapica, D.; Condello, G.; et al. A life course examination of the physical environmental determinants of physical activity behaviour: A “Determinants of Diet and Physical Activity” (DEDIPAC) umbrella systematic literature review. PLoS ONE 2017, 12, e0182083. [Google Scholar] [CrossRef]
- Denzin, N.K. Interpretive Interactionism; Applied social Research Methods; Sage Publications: London, UK, 1989. [Google Scholar]
- Shearer, K.; Rempel, G.R.; Norris, C.M.; Magill-Evans, J. “It’s No Big Deal”: Adolescents With Congenital Heart Disease. J. Pediatr. Nurs. 2013, 28, 28–36. [Google Scholar] [CrossRef]
- Longmuir, P.E.; Tyrrell, P.N.; Corey, M.; Faulkner, G.; Russell, L.; Mccrindle, B.W.; Russell, J.L.; Mccrindle, B.W.; Russell, L.; Mccrindle, B.W.; et al. Home-based rehabilitation enhances daily physical activity and motor skill in children who have undergone the fontan procedure. Pediatr. Cardiol. 2013, 34, 1130–1151. [Google Scholar] [CrossRef]
- Hoppe, M.J.; Wells, E.A.; Morrison, D.M.; Gillmore, M.R.; Wilsdon, A. Using focus groups to discuss sensitive topics with children. Eval. Rev. 1995, 19, 102–114. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Evaluation and Research Methods; Sage Publications: Thousand Oaks, CA, USA, 1990; Volume 2. [Google Scholar]
- Freedom, R.M.; Hamilton, R.; Yoo, S.J.; Mikailian, H.; Benson, L.; McCrindle, B.W.; Justino, H.; Williams, W.G. The Fontan procedure: Analysis of cohorts and late complications. Cardiol Young 2000, 10, 307–331. [Google Scholar] [CrossRef]
- Canadian Society for Exercise Physiology; Healthy Activing Living and Obesity Research Group; Conference Board of Canada; Public Health Agency of Canada; ParticipAction. Canadian 24-hour Movement Guidelines for Children and Youth: An integration of physical activity, sedentary behaviour, and sleep. Can. Soc. Exerc. Physiol. 2017, 41, S311–S327. [Google Scholar]
- Sterdt, E.; Liersch, S.; Walter, U. Correlates of physical activity of children and adolescents: A systematic review of reviews. Health Educ. J. 2014, 73, 72–89. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, physical activity, and self-determination theory: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Active Healthy Kids Global Alliance The Global Matrix 3.0 on Physical Activity for Children and Youth. Available online: https://www.activehealthykids.org/3-0/ (accessed on 14 March 2021).
- Larouche, R.; Garriguet, D.; Gunnell, K.E.; Goldfield, G.S.; Tremblay, M.S. Outdoor time, physical activity, sedentary time, and health indicators at ages 7 to 14: 2012/2013 Canadian Health Measures Survey. Health Rep. 2016, 27, 3–13. [Google Scholar]
- Mooses, K.; Mäestu, J.; Riso, E.-M.; Hannus, A.; Mooses, M.; Kaasik, P.; Kull, M. Different Methods Yielded Two-Fold Difference in Compliance with Physical Activity Guidelines on School Days. PLoS ONE 2016, 11, e0152323. [Google Scholar] [CrossRef]
- Sinha, M. Child Care in Canada; Statistics Canada: Ottawa, ON, Canada, 2014.
- Corder, K.; van Sluijs, E.M.F.; McMinn, A.M.; Ekelund, U.; Cassidy, A.; Griffin, S.J. Perception Versus Reality. Awareness of Physical Activity Levels of British Children. Am. J. Prev. Med. 2010, 38, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lemire, O.; Yaraskavitch, J.; Lougheed, J.; Mackie, A.S.; Norozi, K.; Graham, J.; Willan, A.R.; Longmuir, P.E. Impacting child health outcomes in congenital heart disease: Cluster randomized controlled trial protocol of in-clinic physical activity counselling. Contemp. Clin. Trials 2020, 91, 105994. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Wolfson, A.; Mumme, D.; Guskin, K. Helplessness in children of depressed and nondepressed mothers. Dev. Psychol. 1995, 31, 377–387. [Google Scholar] [CrossRef]
- Hokoda, A.; Fincham, F.D. Origins of children’s helpless and mastery achievement patterns in the family. J. Educ. Psychol. 1995, 87, 375–385. [Google Scholar] [CrossRef]
- Kolaitis, G.A.; Meentken, M.G.; Utens, E.M.W.J. Mental Health Problems in Parents of Children with Congenital Heart Disease. Front. Pediatr. 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Berant, E.; Mikulincer, M.; Shaver, P.R. Mothers’ attachment style, their mental health, and their children’s emotional vulnerabilities: A 7-year study of children with congenital heart disease. J. Pers. 2008, 76, 31–65. [Google Scholar] [CrossRef]
- Best, K.; Ball, K.; Zarnowiecki, D.; Stanley, R.; Dollman, J. In Search of Consistent Predictors of Children’s Physical Activity. Int. J. Environ. Res. Public Health 2017, 14, 1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longmuir, P.E.; Brothers, J.A.; De Ferranti, S.D.; Hayman, L.L.; Van Hare, G.F.; Matherne, G.P.P.; Davis, C.K.; Joy, E.A.; McCrindle, B.W. Promotion of physical activity for children and adults with congenital heart disease: A scientific statement from the Atherosclerosis, Hypertension and Obesity in Youth Committee, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2013, 127, 2147–2159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guest, G.; Bunce, A.; Johnson, L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
| Mother A | Father B | Mother C | Mother D & Father D | Mother E | |
|---|---|---|---|---|---|
| Child Sex | Female | Female | Male | Male | Male (non-participant) |
| Child Age | 11.5 years | 9.8 years | 10.5 years | 8.6 years | 4.9 years |
| Child Diagnosis | Tetralogy of Fallot | Pulmonary Atresia, Hypoplastic Tricuspid Valve | Ventricular Septal Defect, Coarctation of Aorta | Aortic Stenosis | Hypoplastic Left Heart Syndrome |
| Child Surgical History | Biventricular Tetralogy Repair | Fontan | Coarctation & VSD repair | Valvotomy | Fontan |
| Pacemaker | No | Yes | Yes | No | No |
| Child | Sex | Age | Diagnosis | Years from Fontan | Pacemaker | Parent |
|---|---|---|---|---|---|---|
| 1 | M | 9.6 | DORV | 5.5 | No | Father |
| 2 F | M | 10.5 | HLHS | 1.4 | No | Both GP |
| 3 F | M | 10.8 | DILV | 4.4 | No | Father |
| 4 | M | 8.6 | HLHS | 6.3 | No | Mother |
| 5 | M | 7.2 | DILV | 4.7 | No | Both |
| 6 | M | 9.0 | Tri. Atresia | 6.8 | No | Mother |
| 7 | M | 10.4 | DORV | 7.1 | No | Mother |
| 8 | M | 7.1 | Tri. Atresia | 4.4 | Yes | Mother |
| 9 | M | 8.3 | DORV | 3.8 | No | Mother |
| 10 | M | 11.2 | DILV | 6.6 | No | Both |
| 11 | M | 6.2 | Tri. Atresia | 4.2 | No | Mother |
| 12 | M | 6.4 | HLHS | 3.3 | No | Mother |
| 13 | M | 8.2 | HLHS | 5.9 | No | Mother |
| 15 | M | 7.8 | Tri. Atresia | 5.2 | No | Mother |
| 16 | M | 6.4 | Pul. Atresia | 2.5 | No | Both |
| 19 F | M | 11.6 | HLHS | 9.1 | No | Both GP |
| 20 | M | 8.3 | HLHS | 5.1 | No | Mother |
| 25 F | M | 11.2 | HLHS | 8.9 | No | Mother |
| 27 | M | 9.7 | HLHS | 3.4 | No | Mother |
| 30 F | M | 9.1 | HLHS | 5.3 | No | Father |
| 33 F | M | 7.9 | Tri. Atresia | 5.0 | No | Mother |
| 201 | M | 11.4 | Tri. Atresia | 9.2 | No | Both |
| 202 | M | 9.7 | DILV | 6.8 | No | Both |
| 203 | M | 7.9 | Tri. Atresia | 5.2 | No | Mother |
| 1 F | F | 10.5 | DORV | 7.7 | No | Both |
| 2 | F | 7.7 | DILV | 4.8 | No | Both |
| 3 | F | 7.1 | DILV | 3.3 | No | Both |
| 4 F | F | 7.0 | HLHS | 2.6 | No | Mother |
| 5 | F | 6.0 | DILV | 3.1 | No | Mother |
| 6 | F | 10.6 | DORV | 4.4 | No | Mother |
| 7 | F | 6.7 | Tri. Atresia | 4.0 | No | Both |
| 8 | F | 11.1 | DORV | 9.6 | No | Father |
| 9 F | F | 6.1 | DORV | 1.0 | Yes | Mother |
| 10 | F | 10.2 | Tri. Atresia | 7.6 | No | Mother |
| 11 | F | 9.7 | DORV | 7.5 | No | Father |
| 17 | F | 10.5 | Pul. Atresia | 7.4 | No | Mother |
| 18 F | F | 6.4 | DILV | 3.4 | No | Grandmother |
| 19 F | F | 9.1 | DILV | 7.2 | No | Both |
| 20 | F | 9.2 | DORV | 7.3 | No | Mother |
| 23 | F | 9.9 | DILV | 7.0 | No | Mother |
| 24 | F | 10.9 | DILV | 8.9 | No | Mother |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longmuir, P.E.; Corey, M.; McCrindle, B.W. Interactions with Home and Health Environments Discourage Physical Activity: Reports from Children with Complex Congenital Heart Disease and Their Parents. Int. J. Environ. Res. Public Health 2021, 18, 4903. https://doi.org/10.3390/ijerph18094903
Longmuir PE, Corey M, McCrindle BW. Interactions with Home and Health Environments Discourage Physical Activity: Reports from Children with Complex Congenital Heart Disease and Their Parents. International Journal of Environmental Research and Public Health. 2021; 18(9):4903. https://doi.org/10.3390/ijerph18094903
Chicago/Turabian StyleLongmuir, Patricia E., Mary Corey, and Brian W. McCrindle. 2021. "Interactions with Home and Health Environments Discourage Physical Activity: Reports from Children with Complex Congenital Heart Disease and Their Parents" International Journal of Environmental Research and Public Health 18, no. 9: 4903. https://doi.org/10.3390/ijerph18094903
APA StyleLongmuir, P. E., Corey, M., & McCrindle, B. W. (2021). Interactions with Home and Health Environments Discourage Physical Activity: Reports from Children with Complex Congenital Heart Disease and Their Parents. International Journal of Environmental Research and Public Health, 18(9), 4903. https://doi.org/10.3390/ijerph18094903






