Assessing SARS-CoV-2 Infection Rate among Romanian Dental Practitioners
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic and Professional Data of the Dental Practitioners who Completed the Survey
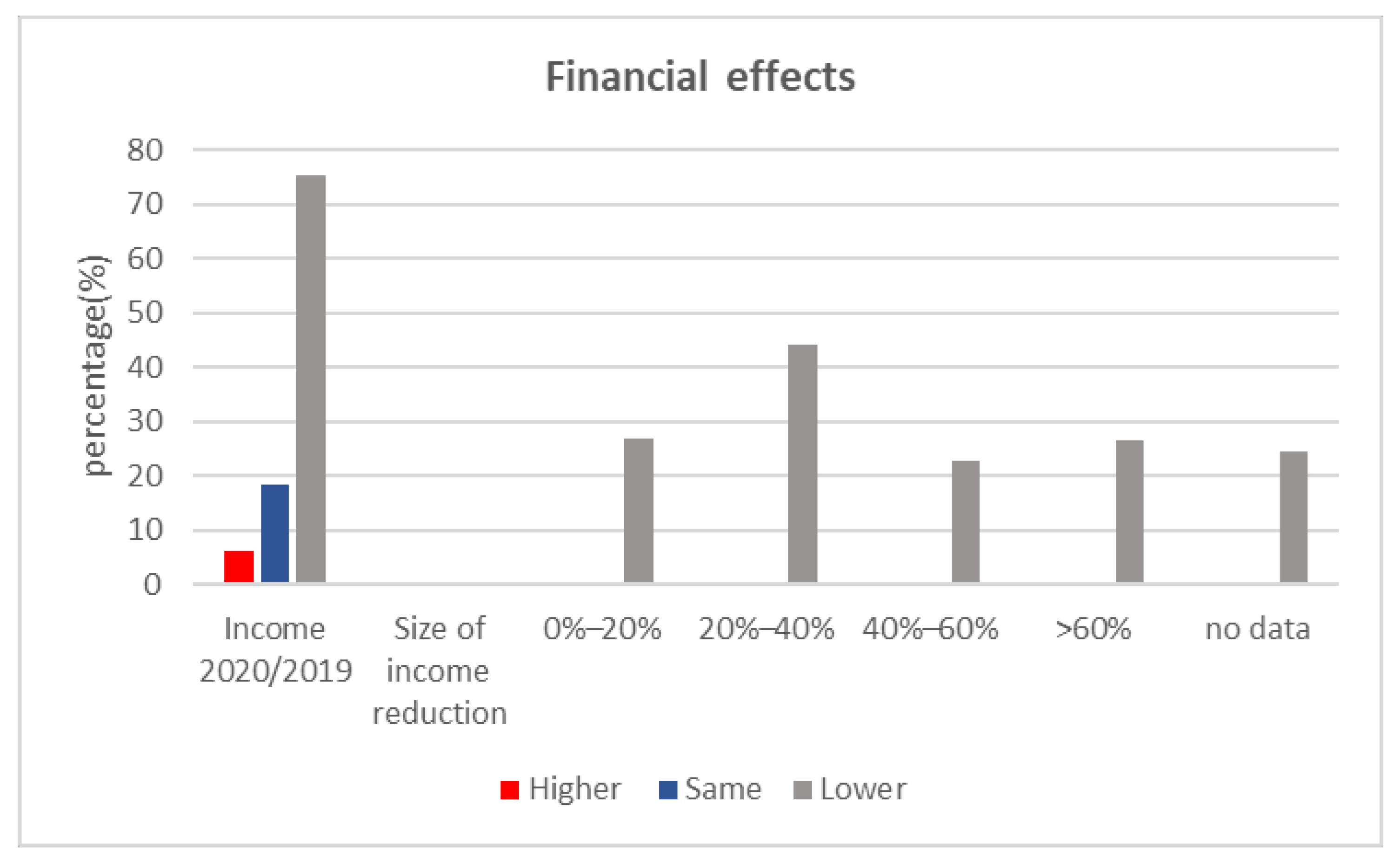
3.2. Economic Aspects Correlated with the COVID-19 Pandemic
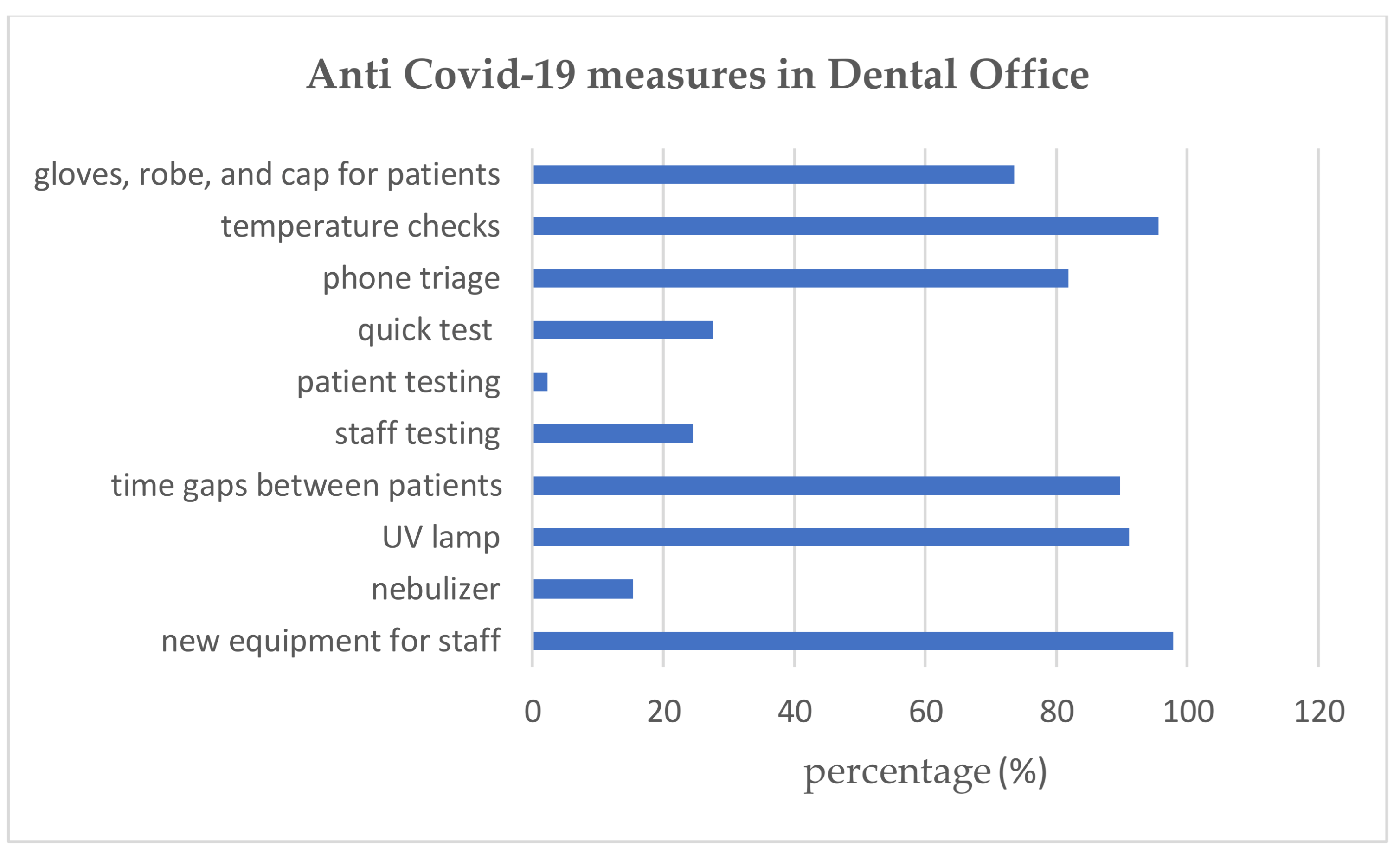
- Evidence suggests that using a nebulizer or a UV lamp and patient phone triage was not more efficient than temperature checks alone in the dental office;
- Testing the staff was more efficient than testing the patients (χ2 = 8.19, p = 0.0042);
- Enhanced personal protective equipment for dental staff was more efficient than the use of gloves, robe, and cap for patients (χ2 = 121.7, p = 0.0001);
- Patient phone triage was more efficient than equipment (gloves, robe, and cap) for patients (χ2 = 16.28, p = 0.00055);
- Allowing proper time gaps between patients was more efficient than using enhanced protective equipment for doctors (χ2 = 15.53, p = 0.00081) or patients (χ2 = 16.28, p = 0.00055);
- The difference in the infections between offices who respect a rigorous interval between patients and those who do not respect it is in favor of the former (fewer infections) χ2 = 16.28, p = 0.00042;
- Dental offices that performed mandatory testing for staff reported a higher number of infections than those that did not implement such a requirement, and the difference was significant χ2 = 6.12, p = 0.01336.
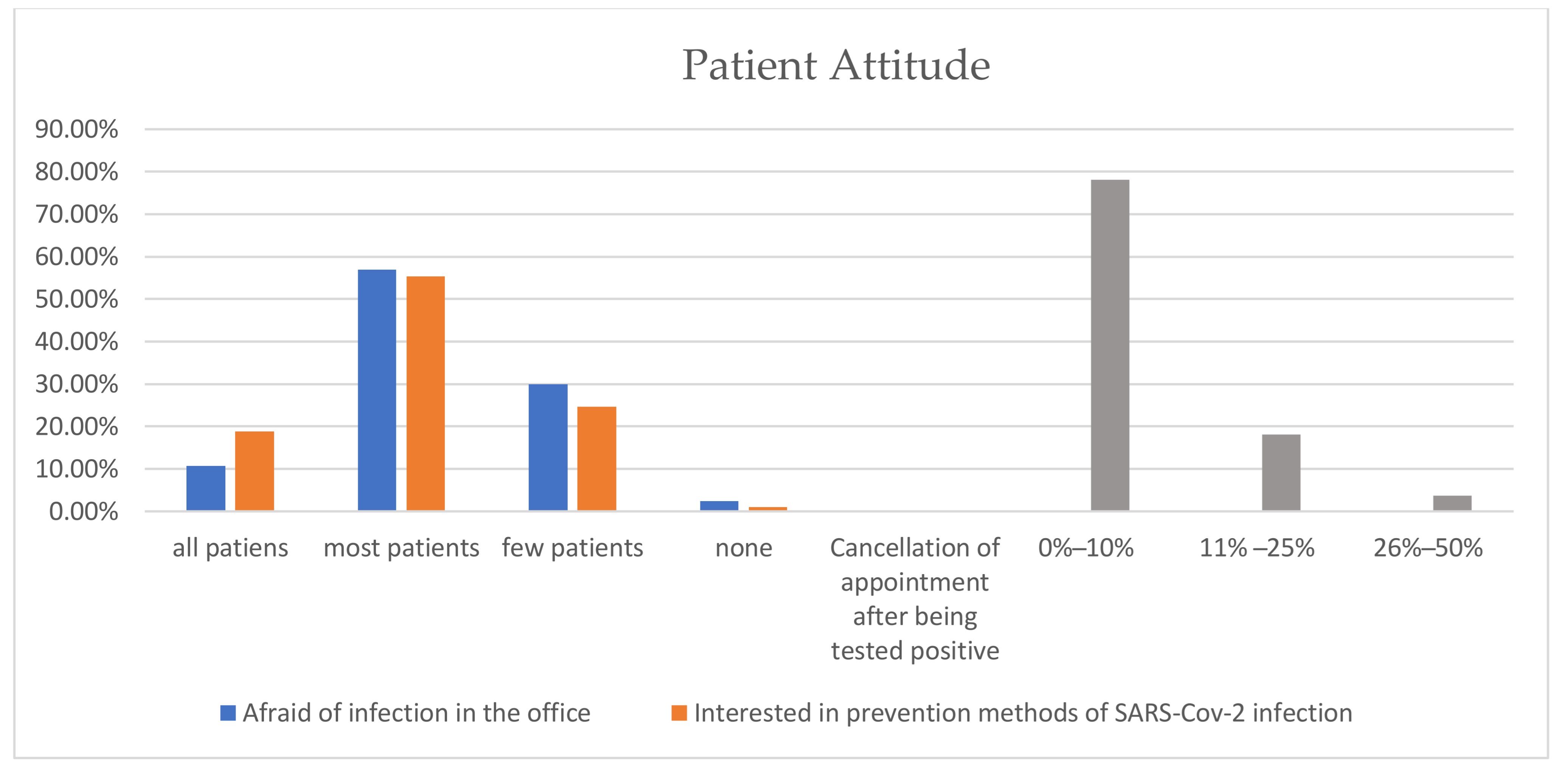
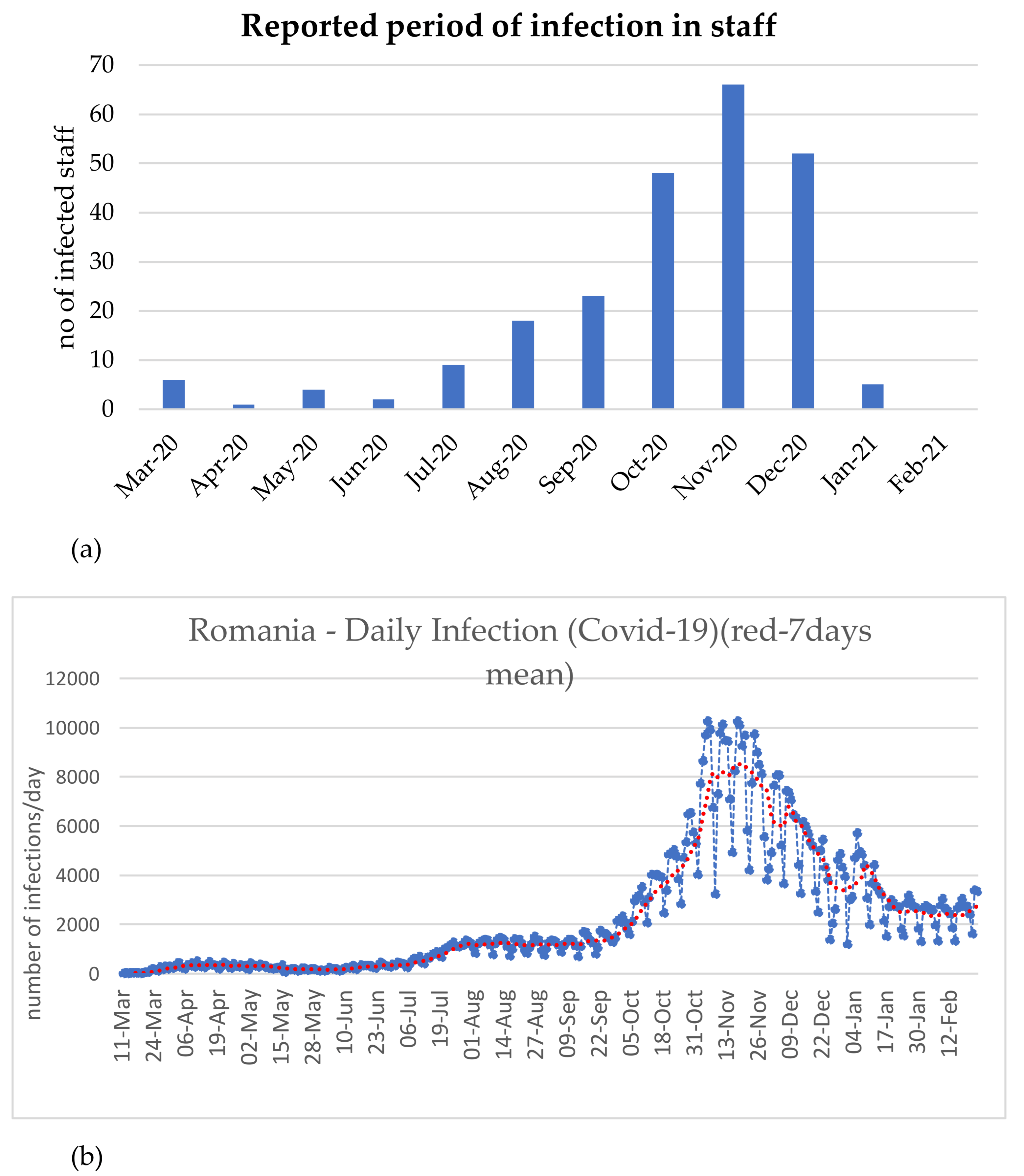
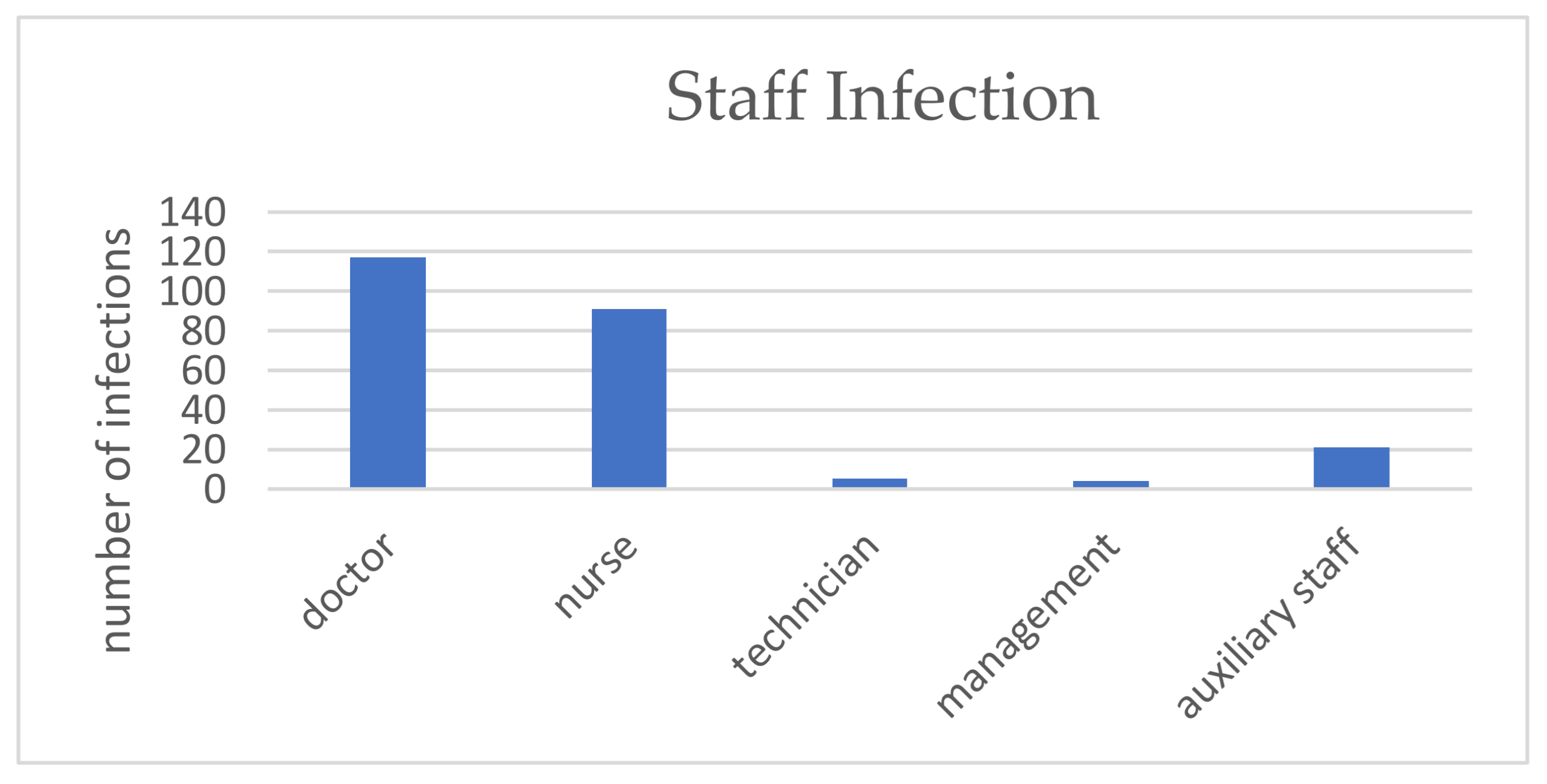
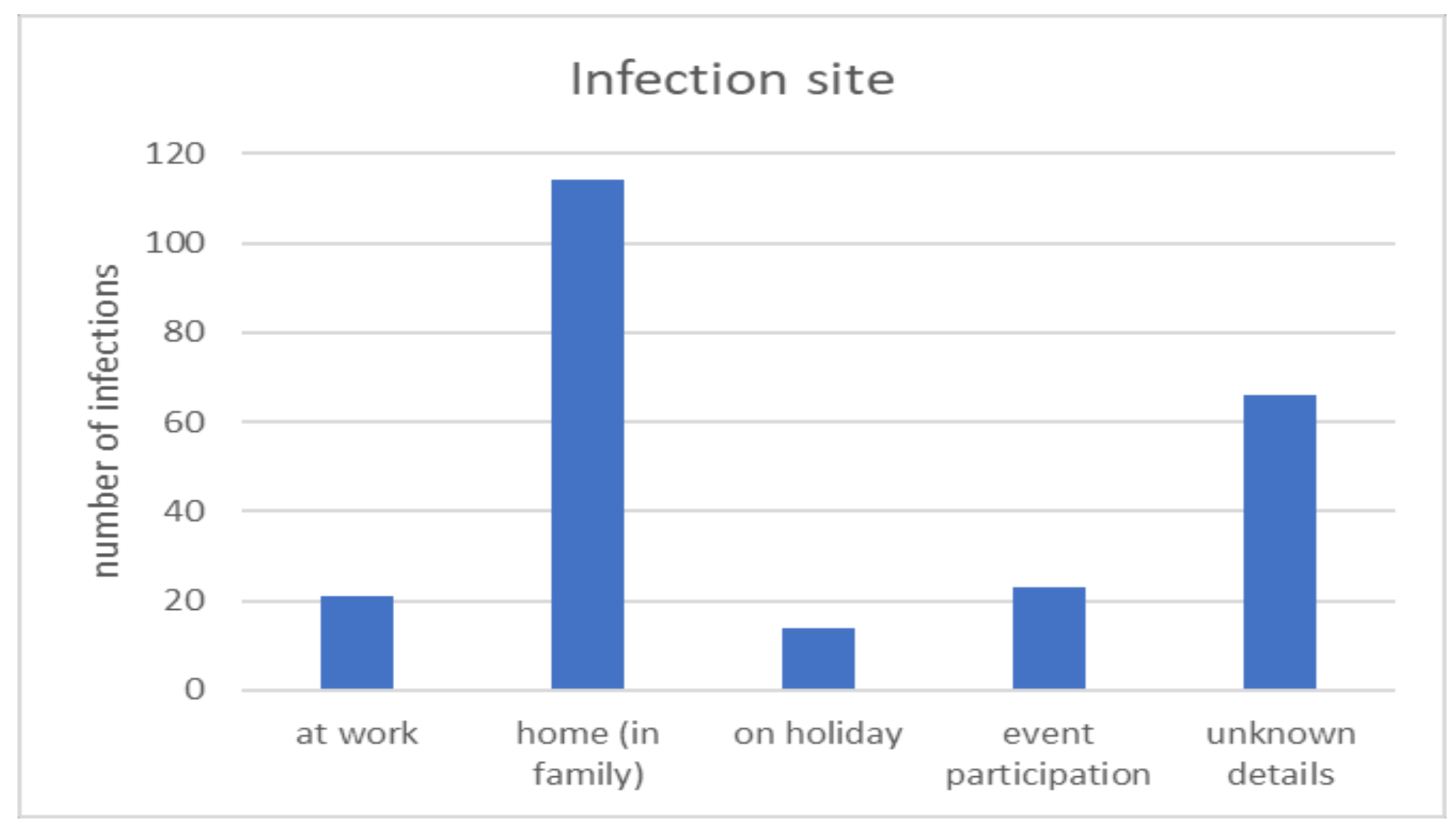
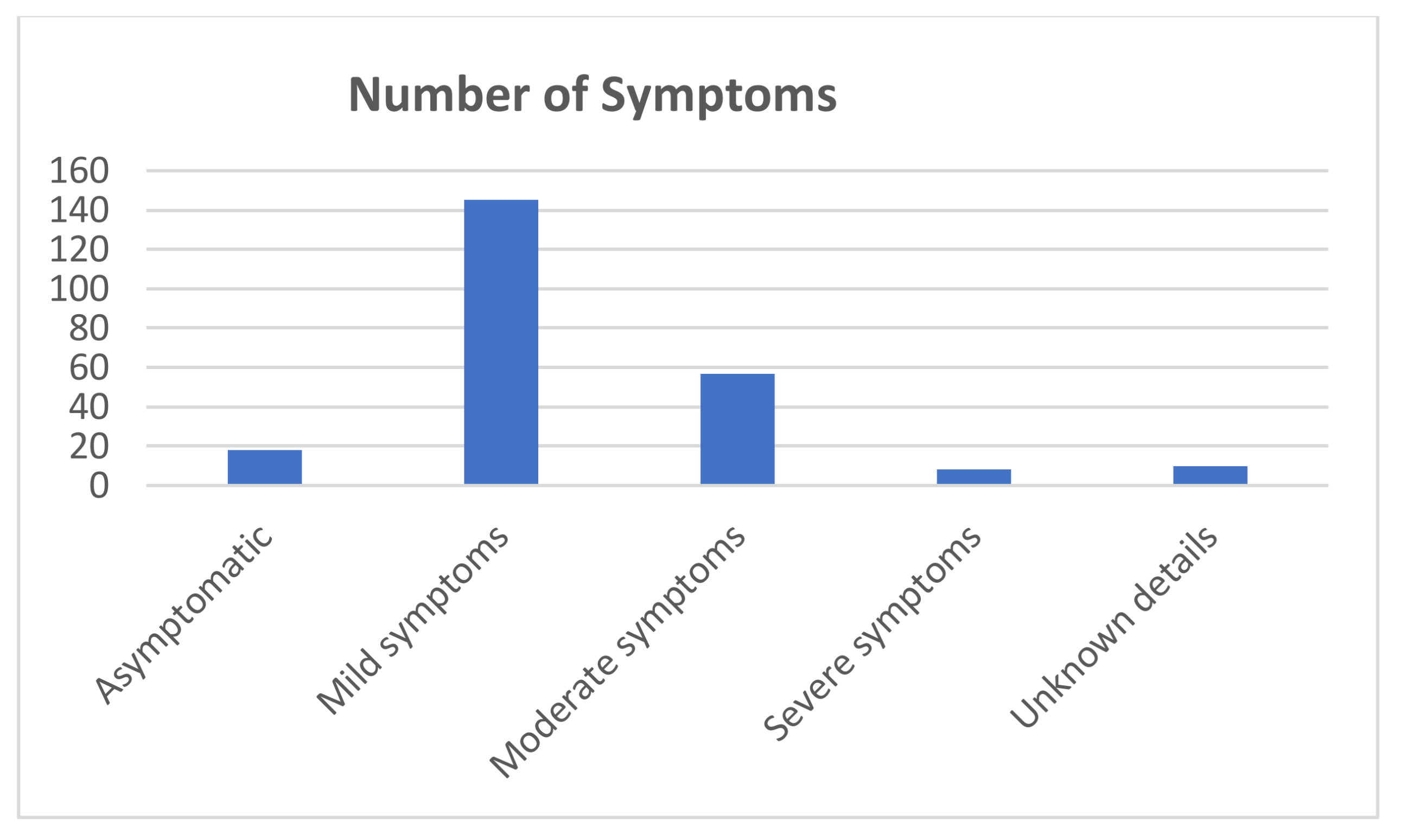
3.3. Epidemiological Aspects Related to SARS-CoV-2 Infection among Dental Practitioners
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A.
Appendix A1
Appendix A2
Appendix A3
Appendix A4
Appendix A5
- Specific/modified protection equipment compared to the period before the COVID-19 pandemic.
- Nebulizer.
- UV lamp
- Strict compliance with the intervals between patients
- Increasing treatment prices
- Establishment of a COVID-19 fee for patients
- Periodic mandatory testing of staff
- Mandatory testing of patients
- Possibility to perform quick COVID-19 tests at the office
- Telephone patient triage prior to appointment
- Body temperature measurement for all patients upon arrival at the dental office
- Provide protective equipment to patients (gloves, gowns, caps)Were there any other measures taken? Describe them briefly.
Appendix A6
- Diabetes
- Obesity
- cardio-pulmonary illness
- digestive illness
- neuro-muscular disorders
- kidney disease
- blood vessel diseases
- oncologic diseases
- no comorbidities
- I do not know the details
References
- Coronavirus Update (Live): 124,038,188 Cases and 2,729,894 Deaths from COVID-19 Virus Pandemic—Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 24 March 2021).
- Prather, K.A.; Wang, C.C.; Schooley, R.T. Reducing Transmission of SARS-CoV-2. Science 2020, 368, 1422–1424. [Google Scholar] [CrossRef]
- Wei, W.E. Presymptomatic Transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 411–415. [Google Scholar] [CrossRef] [Green Version]
- Kutter, J.S.; Spronken, M.I.; Fraaij, P.L.; Fouchier, R.A.; Herfst, S. Transmission Routes of Respiratory Viruses among Humans. Curr. Opin. Virol. 2018, 28, 142–151. [Google Scholar]
- Gamio, L. The Workers Who Face the Greatest Coronavirus Risk; New York Times: New York, NY, USA, 2020. [Google Scholar]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef]
- Giudice, A.; Bennardo, F.; Antonelli, A.; Barone, S.; Fortunato, L. COVID-19 Is a New Challenge for Dental Practitioners: Advice on Patients’ Management from Prevention of Cross Infections to Telemedicine. Open Dent. J. 2020, 14, 298–304. [Google Scholar]
- Ge, Z.-Y.; Yang, L.-M.; Xia, J.-J.; Fu, X.-H.; Zhang, Y.-Z. Possible Aerosol Transmission of COVID-19 and Special Precautions in Dentistry. J. Zhejiang Univ. Sci. B 2020, 21, 361–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC Healthcare Workers. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed on 23 March 2021).
- ADA Interim Guidance for Minimizing Risk of COVID. Available online: https://web.archive.org/web/20200506114732/https:/www.ada.org/~/media/CPS/Files/COVID/ADA_COVID_Int_Guidance_TrTre_Pts.pdf?utm_source=cpsorg&utm_medium=covid-cps=virus-lp&utm_content=cv-pm-ebd-interim-response&utm_campaica=covid-19 (accessed on 23 March 2021).
- Negucioiu, M.; Bucur, A.; Lucaciu, O.; Soanca, A.; Roman, A. Management of SARS-CoV-2 Transmission in Emergency Dental Settings: Current Knowledge and Personal Experience. Disaster Med. Public Health 2020, 22, 1–8. [Google Scholar]
- Military Ordinance. Available online: https://www.mai.gov.ro/wp-content/uploads/2020%9Ba-militar%C4%83-nr.-1-2020-m%C4%83suri-de-prima-urgen%C8%9B%C4%83-Decret.pdf (accessed on 23 March 2021).
- DECRET 195 16/03/2020—Portal Legislativ. Available online: http://legislatie.just.ro/Public/DetaliiDocument/223831 (accessed on 23 March 2021).
- ORDIN 873 22/05/2020—Portal Legislativ. Available online: http://legislatie.just.ro/Public/DetaliiDocumentAfis/226057 (accessed on 23 March 2021).
- Lucaciu, O.; Tarczali, D.; Petrescu, N. Oral Healthcare during the COVID-19 Pandemic. J. Dent. Sci. 2020, 15, 399–402. [Google Scholar] [CrossRef]
- Petrescu, N.B.; Aghiorghiesei, O.; Mesaros, A.S.; Lucaciu, O.P.; Dinu, C.M.; Campian, R.S.; Negucioiu, M. Impact of COVID-19 on Dental Emergency Services in Cluj-Napoca Metropolitan Area: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 7716. [Google Scholar]
- Analiza-de-Situatie-Campania-Sanatatea-Orala-2020.pdf. Available online: https://insp.gov.ro/sites/cnepss/wp-content/uploads/2020/02/Analiza-de-situatie-Campania-Sanatatea-Orala-2020.pdf?fbclid=IIwA0BnwHzSMDy9vqeXE_VoublxwIwlpU0psp_H87wI15QNgssTVGW8Pi5k3c (accessed on 23 March 2021).
- Dalewski, B.; Palka, L.; Kiczmer, P.; Sobolewska, E. The Impact of SARS-CoV-2 Outbreak on the Polish Dental Community’s Standards of Care—A Six-Month Retrospective Survey-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 1281. [Google Scholar] [CrossRef]
- Consolo, U.; Bellini, P.; Bencivenni, D.; Iani, C.; Checchi, V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int. J. Environ. Res. Public Health 2020, 17, 3459. [Google Scholar] [CrossRef]
- Chamorro-Petronacci, C.; Martin Carreras-Presas, C.; Sanz-Marchena, A.; A Rodríguez-Fernández, M.; María Suárez-Quintanilla, J.; Rivas-Mundiña, B.; Suárez-Quintanilla, J.; Pérez-Sayáns, M. Assessment of the Economic and Health-Care Impact of COVID-19 (SARS-CoV-2) on Public and Private Dental Surgeries in Spain: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 5139. [Google Scholar]
- Giudice, A.; Barone, S.; Muraca, D.; Averta, F.; Diodati, F.; Antonelli, A.; Fortunato, L. Can Teledentistry Improve the Monitoring of Patients during the Covid-19 Dissemination? A Descriptive Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 3399. [Google Scholar] [CrossRef]
- Bennardo, F.; Antonelli, A.; Barone, S.; Figliuzzi, M.M.; Fortunato, L.; Giudice, A. Change of Outpatient Oral Surgery during the COVID-19 Pandemic: Experience of an Italian Center. Int. J. Dent. 2020, 2020, 8893423. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Zhou, Y.; Liu, X.; Tan, J. The Impact of the COVID-19 Epidemic on the Utilization of Emergency Dental Services. J. Dent. Sci. 2020, 15, 564–567. [Google Scholar] [CrossRef] [PubMed]
- Long, L.; Corsar, K. The COVID-19 Effect: Number of Patients Presenting to the Mid Yorkshire Hospitals OMFS Team with Dental Infections before and during the COVID-19 Outbreak. Br. J. Oral. Maxillofac. Surg. 2020, 58, 713–714. [Google Scholar] [CrossRef]
- Wang, C.; Miao, L.; Wang, Z.; Xiong, Y.; Jiao, Y.; Liu, H. Emergency Management in a Dental Clinic During the Coronavirus Disease 2019 (COVID-19) Epidemic in Beijing. Int. Dent. J. 2021, 71, 32–39. [Google Scholar] [CrossRef] [PubMed]
- González-Olmo, M.J.; Delgado-Ramos, B.; Ortega-Martínez, A.R.; Romero-Maroto, M.; Carrillo-Díaz, M. Fear of COVID-19 in Madrid. Will Patients Avoid Dental Care? Int. Dent. J. 2021, 1–7. [Google Scholar] [CrossRef]
- Peloso, R.M.; Pini, N.I.P.; Sundfeld Neto, D.; Mori, A.A.; Oliveira, R.C.G.D.; Valarelli, F.P.; Freitas, K.M.S.; Peloso, R.M.; Pini, N.I.P.; Sundfeld Neto, D.; et al. How Does the Quarantine Resulting from COVID-19 Impact Dental Appointments and Patient Anxiety Levels? Braz. Oral Res. 2020, 34, e84. [Google Scholar] [CrossRef]
- Ahmadi, H.; Ebrahimi, A.; Ghorbani, F. The Impact of COVID-19 Pandemic on Dental Practice in Iran: A Questionnaire-Based Report. BMC Oral Health 2020, 20, 354. [Google Scholar]
- Sarkarat, F.; Tootoonchian, A.; Haraji, A.; Rastegarmoghaddam Shaldoozi, H.; Mostafavi, M.; Naghibi Sistani, S.M.M. Evaluation of Dentistry Staff Involvement with COVID-19 in the First 3 Month of Epidemiologic Spreading in Iran. Res. Dent. Sci. 2020, 17, 137–145. [Google Scholar]
- Arellano-Cotrina, J.J.; Marengo-Coronel, N.; Atoche-Socola, K.J.; Peña-Soto, C.; Arriola-Guillén, L.E. Effectiveness and Recommendations for the Use of Dental Masks in the Prevention of COVID-19: A Literature Review. Disaster Med. Public Health Prep. 2020, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Bizzoca, M.E.; Campisi, G.; Lo Muzio, L. Covid-19 Pandemic: What Changes for Dentists and Oral Medicine Experts? A Narrative Review and Novel Approaches to Infection Containment. Int. J. Environ. Res. Public Health 2020, 17, 3793. [Google Scholar] [CrossRef] [PubMed]
- Estrich, C.G.; Mikkelsen, M.; Morrissey, R.; Geisinger, M.L.; Ioannidou, E.; Vujicic, M.; Araujo, M.W.B. Estimating COVID-19 Prevalence and Infection Control Practices among US Dentists. J. Am. Dent. Assoc. 2020, 151, 815–824. [Google Scholar] [CrossRef]
- Finer, N.; Garnett, S.P.; Bruun, J.M. COVID-19 and Obesity. Clin. Obes. 2020, 10, e12365. [Google Scholar] [CrossRef] [PubMed]
- Cazurile de infectare în rândul personalului medical au scăzut cu peste 87.7% după vaccinare. Available online: https://www.mediafax.ro/coronavirus/cazurile-de-infectare-in-randul-personalului-medical-au-scazut-cu-peste-87-7-dupa-vaccinare-19923921 (accessed on 23 March 2021).
| Activity in Dental Offices | |||
|---|---|---|---|
| Dental offices providing dental services during the state of emergency period | Yes | No | |
| 39 (7.7%) | 468 (92.3%) | ||
| Number of emergency treatments after lockdown | Higher | Lower | Same 270 (53.3%) |
| 89 (17.6%) | 148 (29.92%) | ||
| Activity in the dental office | Major changes | Partial changes | No changes 15 (3%) |
| 185 (36.5%) | 307 (60.6%) | ||
| Demand for elective dental services | Higher | Lower | Same 272(53.6%) |
| 22 (4.3%) | 213 (42%) | ||
| Effect on the Team Size | |||
| Team size | Reduced team | Enlarged team | Same size 435 (85.8%) |
| 50 (9.9%) | 22 (4.3%) | ||
| 20-May | 20-June | 20-July | 20-August | 20-September | 20-October | 20-November | 20-December | 21-January | 21-February | |
|---|---|---|---|---|---|---|---|---|---|---|
| No/% | No/% | No/% | No/% | No/% | No/% | No/% | No/% | No/% | No/% | |
| lower | 367 | 300 | 269 | 278 | 270 | 259 | 276 | 302 | 180 | 128 |
| 72.39% | 59.17% | 53.06% | 54.83% | 53.25% | 51.08% | 54.44% | 59.57% | 35.50% | 25.25% | |
| higher | 42 | 64 | 66 | 56 | 56 | 61 | 65 | 56 | 28 | 16 |
| 8.28% | 12.62% | 13.02% | 11.05% | 11.05% | 12.03% | 12.82% | 11.05% | 5.52% | 3.16% | |
| same | 31 | 96 | 124 | 120 | 134 | 138 | 119 | 104 | 56 | 42 |
| 6.11% | 18.93% | 24.40% | 23.67% | 26.43% | 27.22% | 23.47% | 20.51% | 11.05% | 8.28% | |
| no data/no response | 67 | 47 | 48 | 53 | 47 | 49 | 47 | 45 | 243 | 321 |
| 13.02% | 9.27% | 9.47% | 10.45 | 9.47% | 9.67% | 9.27% | 8.88% | 47.93% | 63.31% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucaciu, O.; Boca, A.; Mesaros, A.S.; Petrescu, N.; Aghiorghiesei, O.; Mirica, I.C.; Hosu, I.; Armencea, G.; Bran, S.; Dinu, C.M. Assessing SARS-CoV-2 Infection Rate among Romanian Dental Practitioners. Int. J. Environ. Res. Public Health 2021, 18, 4897. https://doi.org/10.3390/ijerph18094897
Lucaciu O, Boca A, Mesaros AS, Petrescu N, Aghiorghiesei O, Mirica IC, Hosu I, Armencea G, Bran S, Dinu CM. Assessing SARS-CoV-2 Infection Rate among Romanian Dental Practitioners. International Journal of Environmental Research and Public Health. 2021; 18(9):4897. https://doi.org/10.3390/ijerph18094897
Chicago/Turabian StyleLucaciu, Ondine, Antonia Boca, Anca Stefania Mesaros, Nausica Petrescu, Ovidiu Aghiorghiesei, Ioana Codruta Mirica, Ioan Hosu, Gabriel Armencea, Simion Bran, and Cristian Mihail Dinu. 2021. "Assessing SARS-CoV-2 Infection Rate among Romanian Dental Practitioners" International Journal of Environmental Research and Public Health 18, no. 9: 4897. https://doi.org/10.3390/ijerph18094897
APA StyleLucaciu, O., Boca, A., Mesaros, A. S., Petrescu, N., Aghiorghiesei, O., Mirica, I. C., Hosu, I., Armencea, G., Bran, S., & Dinu, C. M. (2021). Assessing SARS-CoV-2 Infection Rate among Romanian Dental Practitioners. International Journal of Environmental Research and Public Health, 18(9), 4897. https://doi.org/10.3390/ijerph18094897










