A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management
Abstract
1. Introduction
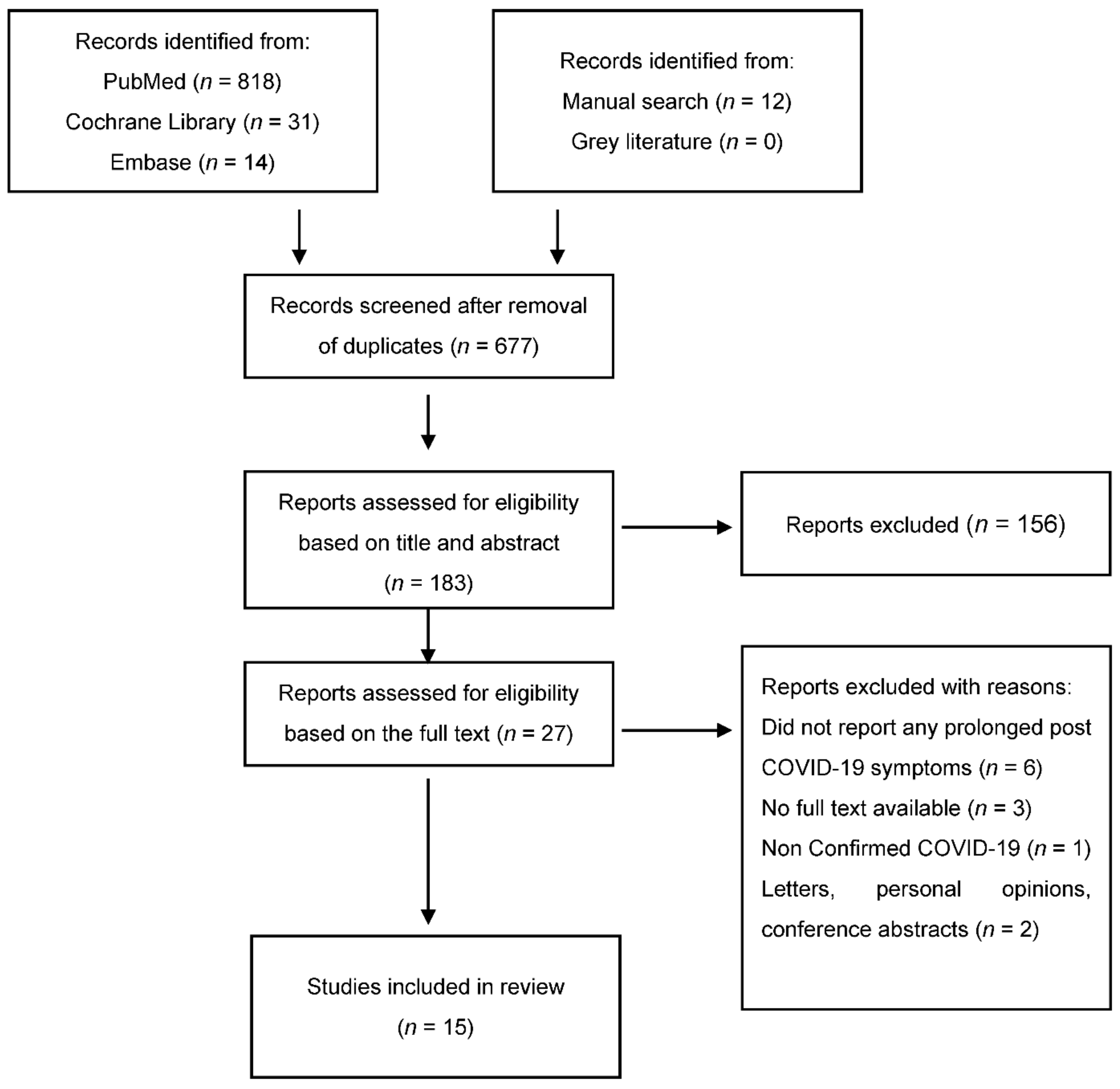
2. Materials and Methods
- What are the prolonged post-COVID-19 symptoms in recovered patients?
- What is the impact of COVID-19 on dental management?
- What are the clinical implications of prolonged post-COVID-19 symptoms during dental management?
- What could be the possible challenges for the dental team while treating patients who have prolonged symptoms?
3. Results
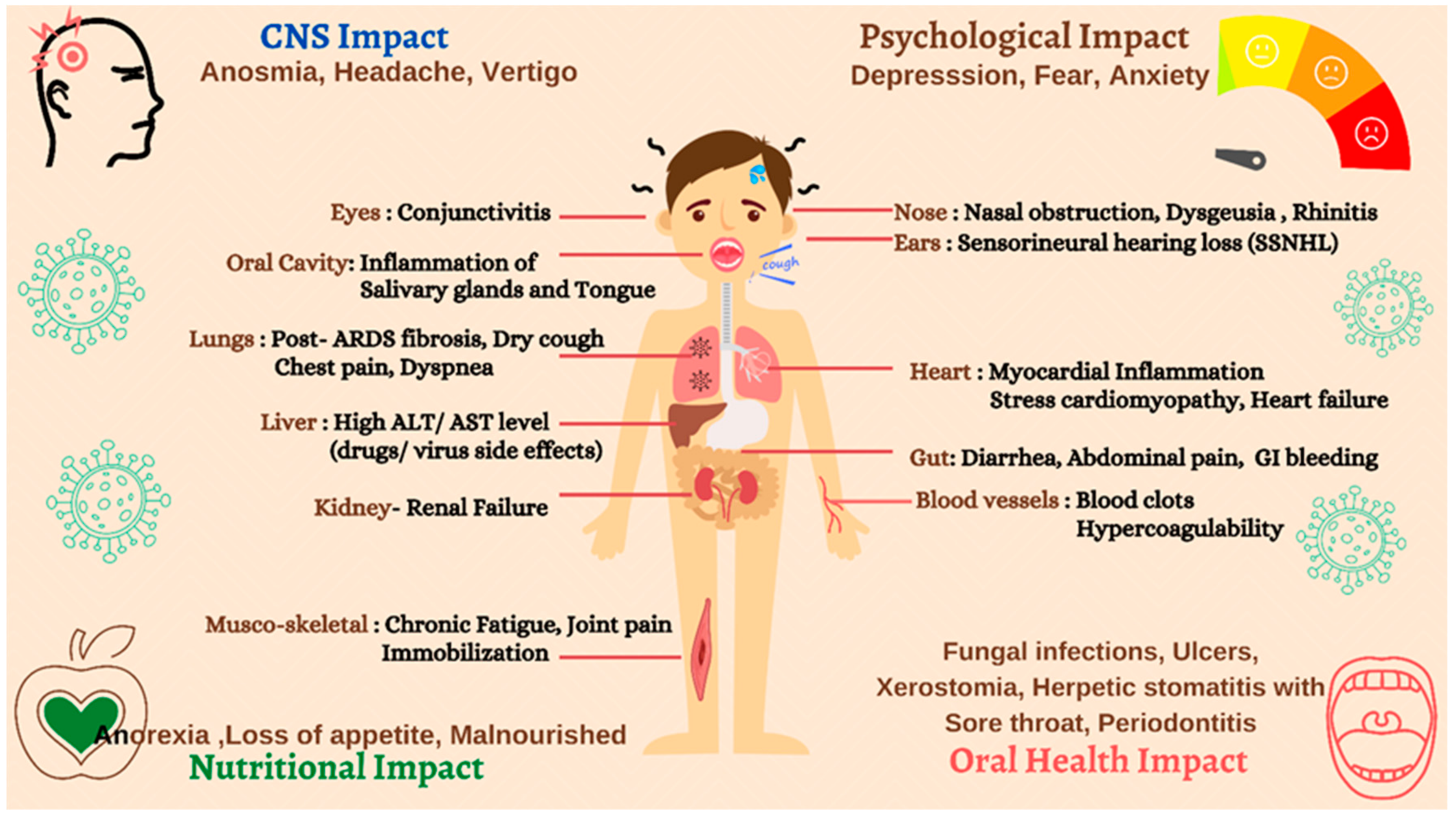
3.1. Prolonged COVID-19 Symptoms in Post-COVID Patients
3.2. Impact of COVID-19 on Dental Management
4. Discussion
4.1. Implications of COVID-19 on Online Triaging and Patients Management
4.2. Dental Treatment Considerations for Post-COVID-19 Patients with Prolonged Symptoms
4.3. Oral Manifestations of COVID-19 and Its Management
- -
- Probably pre-existing conditions: Geographic tongue, fissured tongue.
- -
- Sars-CoV-2-related lesions: Early ulcerative lesions, blisters, early erythema multiforme-like lesions, and petechiae.
- -
- Treatment-related lesions: Late ulcerative lesions, late erythema multiforme-like lesions, Candidiasis, angina bullosa, spontaneous oral hemorrhage, and petechiae.
- -
- Lesions related to poor oral hygiene: Ulcero-necrotic gingivitis.
- Miconazole Nitrate twice a day in patients with cytological diagnosis of candidiasis.
- Tranexamic acid for local hemorrhages [50].
- Previous studies have suggested a biopsy in the absence of healing after 14 days among mild COVID-19 patients with prior rinsing with chlorhexidine 2% mouthwash for at least 1 min.
4.4. Dental Implications of Prolonged COVID-19 Symptoms in Geriatric Dentistry
5. Conclusions
- -
- The lesions in oral mucosa in long COVID patients due to various therapeutic approaches of COVID-19.
- -
- The impact of prolonged symptoms in post-COVID-19 patients on urgent dental care.
- -
- Dental considerations and clinical management of COVID-19 recovered patients.
- -
- Implications of online triaging post-COVID-19 patients.
- -
- Classifications of oral manifestations of COVID-19 and its management.
- -
- Implications of AI-based dental screening software in geriatric consultations.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Chintalapudi, N.; Battineni, G.; Amenta, F. COVID-19 virus outbreak forecasting of registered and recovered cases after sixty day lockdown in Italy: A data driven model approach. J. Microbiol. Immunol. Infect. 2020, 53, 396–403. [Google Scholar] [CrossRef]
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; Holden, K.A.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ 2020, 369, m1985. [Google Scholar] [CrossRef] [PubMed]
- Balachandar, V.; Mahalaxmi, I.; Subramaniam, M.; Kaavya, J.; Kumar, N.S.; Laldinmawii, G.; Narayanasamy, A.; Reddy, P.J.K.; Sivaprakash, P.; Kanchana, S.; et al. Follow-up studies in COVID-19 recovered patients—is it mandatory? Sci. Total Environ. 2020, 729, 139021. [Google Scholar] [CrossRef]
- Elshazli, R.M.; Toraih, E.A.; Elgaml, A.; El-Mowafy, M.; El-Mesery, M.; Amin, M.N.; Hussein, M.H.; Killackey, M.T.; Fawzy, M.S.; Kandil, E. Diagnostic and prognostic value of hematological and immunological markers in COVID-19 infection: A meta-analysis of 6320 patients. PLoS ONE 2020, 15, e0238160. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Kim, S.S.; Lindsell, C.J.; Rose, E.B.; Shapiro, N.I.; Files, D.C.; Gibbs, K.W.; Erickson, H.L.; Steingrub, J.S.; Smithline, H.A.; et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network—United States, March–June. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 993–998. [Google Scholar] [CrossRef]
- Toscano, G.; Palmerini, F.; Ravaglia, S.; Ruiz, L.; Invernizzi, P.; Cuzzoni, M.G.; Franciotta, D.; Baldanti, F.; Daturi, R.; Postorino, P.; et al. Guillain–Barré Syndrome Associated with SARS-CoV-2. N. Engl. J. Med. 2020, 382, 2574–2576. [Google Scholar] [CrossRef]
- Adam, E.; Zacharowski, K.; Miesbach, W. A comprehensive assessment of the coagulation profile in critically ill COVID-19 patients. Thromb. Res. 2020, 194, 42–44. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Gemelli Against COVID-19 Post-Acute Care Study Group. Post-COVID-19 global health strategies: The need for an interdisciplinary approach. Aging Clin. Exp. Res. 2020, 32, 1613–1620. [Google Scholar] [CrossRef]
- Mahdi, S.; Ahmed, Z.; Allana, R.; Peretti, A.; Amenta, F.; Bijle, M.N.; Seow, L.; Daood, U. Pivoting Dental Practice Management during the COVID-19 Pandemic—A Systematic Review. Medicina 2020, 56, 644. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 1–6. [Google Scholar] [CrossRef]
- Cao, Y.; Liu, X.; Xiong, L.; Cai, K. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2: A systematic review and meta-analysis. J. Med. Virol. 2020, 92, 1449–1459. [Google Scholar] [CrossRef]
- Kobza, J.; Pastuszka, J.S.; Brągoszewska, E. Do exposures to aerosols pose a risk to dental professionals? Occup. Med. 2018, 68, 454–458. [Google Scholar] [CrossRef]
- D’Amico, C.; Bocchieri, S.; De Stefano, R.; Gorassini, F.; Surace, G.; Amoroso, G.; Scoglio, C.; Mastroieni, R.; Gambino, D.; Amantia, E.M.; et al. Dental Office Prevention of Coronavirus Infection. Eur. J. Dent. 2020, 14, 146–151. [Google Scholar] [CrossRef]
- Avasthi, A. High Volume Evacuator (HVE) in reducing aerosol- an exploration worth by clinicians. J. Dent. Health Oral Disord. Ther. 2018, 9, 1–2. [Google Scholar] [CrossRef]
- Carfì, A.; Bernabei, R.; Landi, F.; For the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef]
- Del Rio, C.; Collins, L.F.; Malani, P. Long-term Health Consequences of COVID-19. JAMA 2020, 324, 1723. [Google Scholar] [CrossRef]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef]
- Halpin, S.J.; McIvor, C.; Whyatt, G.; Adams, A.; Harvey, O.; McLean, L.; Walshaw, C.; Kemp, S.; Corrado, J.; Singh, R.; et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 2021, 93, 1013–1022. [Google Scholar] [CrossRef]
- Koumpa, F.S.; Forde, C.T.; Manjaly, J.G. Sudden irreversible hearing loss post COVID-19. BMJ Case Rep. 2020, 13, e238419. [Google Scholar] [CrossRef]
- Moreno-Pérez, O.; Merino, E.; Leon-Ramirez, J.-M.; Andres, M.; Ramos, J.M.; Arenas-Jiménez, J.; Asensio, S.; Sanchez, R.; Ruiz-Torregrosa, P.; Galan, I.; et al. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J. Infect. 2021, 82, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, J.A.; Normando, A.G.C.; Da Silva, R.L.C.; De Paula, R.M.; Cembranel, A.C.; Santos-Silva, A.R.; Guerra, E.N.S. Oral mucosal lesions in a COVID-19 patient: New signs or secondary manifestations? Int. J. Infect. Dis. 2020, 97, 326–328. [Google Scholar] [CrossRef] [PubMed]
- Perrin, R.; Riste, L.; Hann, M.; Walther, A.; Mukherjee, A.; Heald, A. Into the looking glass: Post-viral syndrome post COVID-19. Med. Hypotheses 2020, 144, 110055. [Google Scholar] [CrossRef]
- Sardari, A.; Tabarsi, P.; Borhany, H.; Mohiaddin, R.; Houshmand, G. Myocarditis detected after COVID-19 recovery. Eur. Hear. J. Cardiovasc. Imaging 2021, 22, 131–132. [Google Scholar] [CrossRef]
- Wang, X.; Xu, H.; Jiang, H.; Wang, L.; Lu, C.; Wei, X.; Liu, J.; Xu, S. Clinical features and outcomes of discharged coronavirus disease 2019 patients: A prospective cohort study. QJM Int. J. Med. 2020, 113, 657–665. [Google Scholar] [CrossRef]
- Weerahandi, H.; Hochman, K.A.; Simon, E.; Blaum, C.; Chodosh, J.; Duan, E.; Garry, K.; Kahan, T.; Karmen-Tuohy, S.L.; Karpel, H.C.; et al. Post-Discharge Health Status and Symptoms in Patients with Severe COVID-19. J. Gen. Intern. Med. 2021, 36, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Samara, E.; Paul, R.; Ko, Y.Y.; Ameerally, P. The effect of COVID-19 outbreak on hospital admissions for dental infections. Adv. Oral Maxillofac. Surg. 2021, 2, 100025. [Google Scholar] [CrossRef]
- Petrescu, N.; Aghiorghiesei, O.; Mesaros, A.; Lucaciu, O.; Dinu, C.; Campian, R.; Negucioiu, M. Impact of COVID-19 on Dental Emergency Services in Cluj-Napoca Metropolitan Area: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 7716. [Google Scholar] [CrossRef]
- Kateeb, E.T.; Juniedi, R.N.; Warren, J.J. Reopening Dental Offices for Routine Care Amid the COVID-19 Pandemic: Report From Palestine. Int. Dent. J. 2021. [Google Scholar] [CrossRef]
- Lee, Y.-L.; Hu, H.-Y.; Yen, Y.-F.; Chu, D.; Yang, N.-P.; Chou, S.-Y.; Lin, S.-Y.; Chu, C.-M.; Huang, S.-J. Impact of the COVID-19 pandemic on the utilization of medical and dental services in Taiwan: A cohort study. J. Dent. Sci. 2021. [Google Scholar] [CrossRef]
- Mittal, M.; Battineni, G.; Goyal, L.M.; Chhetri, B.; Oberoi, S.V.; Chintalapudi, N.; Amenta, F. Cloud-based framework to mitigate the impact of COVID-19 on seafarers’ mental health. Int. Marit. Health 2020, 71, 213–214. [Google Scholar] [CrossRef]
- Otte, M.; Klussmann, J.; Luers, J. Persisting olfactory dysfunction in patients after recovering from COVID-19. J. Infect. 2020, 81, e58. [Google Scholar] [CrossRef]
- Wang, C.; Miao, L.; Wang, Z.; Xiong, Y.; Jiao, Y.; Liu, H. Emergency Management in a Dental Clinic During the Coronavirus Disease 2019 (COVID-19) Epidemic in Beijing. Int. Dent. J. 2021, 71, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S. Teledentistry during COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 933–935. [Google Scholar] [CrossRef]
- Giudice, A.; Barone, S.; Muraca, D.; Averta, F.; Diodati, F.; Antonelli, A.; Fortunato, L. Can Teledentistry Improve the Monitoring of Patients during the COVID-19 Dissemination? A Descriptive Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 3399. [Google Scholar] [CrossRef] [PubMed]
- Czajkowska, S.; Rupa-Matysek, J.; Gil, L.; Surdacka, A. Practical Recommendations for Treatment of Dental Patients with Congenital Bleeding Disorders during the COVID-19 Pandemic: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7245. [Google Scholar] [CrossRef]
- Flaczyk, A.; Rosovsky, R.P.; Reed, C.T.; Bankhead-Kendall, B.K.; Bittner, E.A.; Chang, M.G. Comparison of published guidelines for management of coagulopathy and thrombosis in critically ill patients with COVID 19: Implications for clinical practice and future investigations. Crit. Care 2020, 24, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Abed, H.; Ainousa, A. Dental management of patients with inherited bleeding disorders: A multidisciplinary approach. Gen. Dent. 2017, 65, 56–60. [Google Scholar] [PubMed]
- Long, B.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Cardiovascular complications in COVID-19. Am. J. Emerg. Med. 2020, 38, 1504–1507. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Knight, M.; A’Court, C.; Buxton, M.; Husain, L. Management of post-acute COVID-19 in primary care. BMJ 2020, 370, m3026. [Google Scholar] [CrossRef] [PubMed]
- Abramovitz, I.; Palmon, A.; Levy, D.; Karabucak, B.; Kot-Limon, N.; Shay, B.; Kolokythas, A.; Almoznino, G. Dental care during the coronavirus disease 2019 (COVID-19) outbreak: Operatory considerations and clinical aspects. Quintessence Int. 2020, 51, 418–429. [Google Scholar]
- John, T.; Jacob, C.; Kontoyiannis, D. When Uncontrolled Diabetes Mellitus and Severe COVID-19 Converge: The Perfect Storm for Mucormycosis. J. Fungi 2021, 7, 298. [Google Scholar] [CrossRef]
- Carreras-Presas, C.M.; Sánchez, J.A.; López-Sánchez, A.F.; Jané-Salas, E.; Pérez, M.L.S. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. 2021, 27, 710–712. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.N.; De Mello, T.P.; Ramos, L.D.S.; Branquinha, M.H.; Roudbary, M.; Dos Santos, A.L.S. Fungal Infections in COVID-19-Positive Patients: A Lack of Optimal Treatment Options. Curr. Top. Med. Chem. 2020, 20, 1951–1957. [Google Scholar] [CrossRef] [PubMed]
- Favia, G.; Tempesta, A.; Barile, G.; Brienza, N.; Capodiferro, S.; Vestito, M.C.; Crudele, L.; Procacci, V.; Ingravallo, G.; Maiorano, E.; et al. COVID-19 Symptomatic Patients with Oral Lesions: Clinical and Histopathological Study on 123 Cases of the University Hospital Policlinic of Bari with a Purpose of a New Classification. J. Clin. Med. 2021, 10, 757. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, H. Oral Symptoms Associated with COVID-19 and Their Pathogenic Mechanisms: A Literature Review. Dent. J. 2021, 9, 32. [Google Scholar] [CrossRef]
- Capodiferro, S.; Tempesta, A.; Bucci, S.; Maiorano, E.; Favia, G.; Limongelli, L. Aminogam® Gel Allows Faster Wound Healing after Oral Surgery by Formation of Mature Connective Tissue with Low Vascular Density and Reducing Inflammatory Infiltration. A Retrospective Study on 580 Cases with Histological and Confocal Laser Investigation. Appl. Sci. 2020, 10, 1105. [Google Scholar] [CrossRef]
- Lee, J.H.; Jung, J.Y.; Bang, D. The efficacy of topical 0.2% hyaluronic acid gel on recurrent oral ulcers: Comparison between recurrent aphthous ulcers and the oral ulcers of Behçet’s disease. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 590–595. [Google Scholar] [CrossRef]
- Boccio, E.; Hultz, K.; Wong, A.H. Topical Tranexamic Acid for Hemostasis of an Oral Bleed in a Patient on a Direct Oral Anticoagulant. Clin. Pract. Cases Emerg. Med. 2020, 4, 146–149. [Google Scholar] [CrossRef]
- Cicciù, M.; Cervino, G.; Baldari, S. The Use of Protective Visors in the Dentistry Degree Course of Dental Prosthetics Technology at the University of Messina. Prosthesis 2020, 2, 321–324. [Google Scholar] [CrossRef]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Öst, L.-G. Applied relaxation: Description of a coping technique and review of controlled studies. Behav. Res. Ther. 1987, 25, 397–409. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef] [PubMed]
- Campus, G.; Diaz-Betancourt, M.; Cagetti, M.G.; Carvalho, J.C.; Carvalho, T.S.; Cortés-Martinicorena, J.F.; Deschner, J.; Douglas, G.V.A.; Giacaman, R.A.; Machiulskiene, V.; et al. Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey. Int. J. Environ. Res. Public Health 2020, 17, 5598. [Google Scholar] [CrossRef]
- Soltani, P.; Baghaei, K.; Tafti, K.T.; Spagnuolo, G. Science Mapping Analysis of COVID-19 Articles Published in Dental Journals. Int. J. Environ. Res. Public Health 2021, 18, 2110. [Google Scholar] [CrossRef]
| Author and Year | Sample | Study Type | Prolonged Symptoms of COVID-19 |
|---|---|---|---|
| Carfi et al., 2020 [17] | 143 | Case Series |
|
| C D Rio et al., 2020 [18] | 292 | Cross sectional |
|
| E Garrigues et al., 2020 [19] | 120 | Cross sectional | Fatigue, dyspnoea, loss of memory, concentration and sleep disorders, ageusia, anosmia, hair loss, memory loss. |
| Halpin et al., 2020 [20] | 100 | Cross sectional | Fatigue, breathlessness, persistent cough, concentration problems, post- traumatic stress disorder (PTSD), voice changes, anxiety, depression, continence problems, memory problems, dysphagia. |
| Koumpa et al., 2020 [21] | 45-year-old patient | Case report | Sudden onset sensorineural hearing loss (SSNHL). |
| Moreno-Perez et al., 2021 [22] | 277 | Cohort study | Fatigue, dyspnoea, anosmia, amnesic complaints, cough, dysgeusia, headache. |
| Amorim dos Santos et al., 2020 [23] | 77-year-old male patient | Case report | Fungus infection, Herpetic recurrent oral lesion, Fibroma and geographic tongue as a result of COVID-19 specific treatment. |
| R Perrin et al., 2020 [24] | 42-year-old male patient | Case report | CFS/ME symptomatology such as persistent fatigue, diffuse myalgia, depressive symptoms, and non-restorative sleep. |
| A Sardasi et al., 2020 [25] | 31-year-old patient | Case report | Myocarditis due to residual myocardial inflammation. |
| Wang et al., 2020 [26] | 131 | Cohort study | Cough, fatigue, expectoration, chest tightness, dyspnoea, chest pain, dizziness, palpitation. Other rare symptoms, including pharyngeal pain, nausea, inappetence and vomiting. |
| Weerahandi et al., 2021 [27] | 161 | Cohort Study | Dyspnoea, altered mental status. |
| Author and Year | Sample | Study Type | COVID-19 Impact on Dental Management |
|---|---|---|---|
| Samara et al., 2021 [28] | 11 | Cross-sectional | The number of hospital admissions for cervicofacial infections decreased by 35% during the COVID-19 pandemic when dental practices were closed. There was an increase in cases treated with intravenous antibiotics and extraction under local anesthetic in 2020. The mean CRP during the period of lockdown was significantly higher compared to the same period 1 year ago. |
| Petrescu et al., 2020 [29] | 884 | Cross-sectional | Acute apical periodontitis (42.3%), acute pulpitis (33.3%), and cellulitis/abscess (9.3%) were the most frequent diagnosis. The percentage of patients receiving sedative filling for acute pulpitis treatment in 2020 was significantly higher than in 2019. Dental emergencies were higher for the age group of 20–50 years. The most frequent treatment performed for the abscess was endodontic drainage, both in 2020 and 2019. |
| Kateeb et al., 2021 [30] | 488 | Cross-sectional | Almost 13% reported a lack of confidence in dealing with patients with COVID-19, while 64% had “little to moderate” confidence. Most dentists (88%) preferred not to treat patients with COVID-19, while 40% were willing to provide care. 75% reported financial hardships due to the pandemic. 61.2% of the participants felt confused about the protocol’s procedures, while 78% demanded updating of the current protocol to reopen dental clinics to routine care. |
| Lee et al., 2021 [31] | 6681 medical visits | Cohort | The highest reduction in ambulatory medical visits was at clinics, while the most severe dental visits reduction was at hospitals. Due to the postponement of non-emergency or highly infectious dental procedures, the investigators anticipate that more severe dental problems or complications may occur in the post-COVID-19 period. |
| Dental Care Phases | Suggested Evaluation and Dental Setting Guidelines |
|---|---|
| Primary Teledentisty Examination | Ask the patient to upload intra oral pictures in different perspectives using phone camera and tablespoons in the SmileMate |
| Ask for the medical and medication history | |
| Ask the patient about the past and present signs and symptoms of COVID-19 | |
| Ask the patient about the treatment received for COVID-19 (supplemental oxygen, antibiotics, anti-retroviral, HCQ, immunomodulators) | |
| Check the past diagnostic reports of COVID-19 | |
| Share the comprehensive dental report based on Online dental screening software (SmileMate) with the patient | |
| Patient counselling and treatment recommendation should be advised | |
| Comprehensive COVID-19 post-acute assessment | Oxygen saturation, Heart rate, Blood pressure assessment |
| Lifestyle assessment (physical activity, diet, alcohol consumption) | |
| Ask for gastrointestinal symptoms | |
| Physical perfomance test (6 min walking, hand grip and chair side stand) for the elderly patients | |
| Psychiatric history and quality or life assessment | |
| Dental facility considerations for COVID-19 recovered patient | The appointments for the patients who have persistent symptoms should be preplanned (either first or the last appointment) |
| Shorter waiting time | |
| Mandatory use of facemasks in the waiting room | |
| Waiting area should allow social distancing (6-feet/2 m) apart | |
| Provision for tissue paper dispenser and foot operated waster bin | |
| Use of HEPA filters in dental care facilities with commercial split and centralized/window Acs | |
| Proper ventilated dental operatory rooms | |
| Administer frequent disinfection of touched surfaces with NaOCl and ethanol | |
| Disinfecting the floors or the operatory room with 1000 mg/L chlorine | |
| ’Critical’ heat sensitive instruments should de disinfected with 2 %glutaraldehyde | |
| Waste disposal in accordance to the CDC guidelines | |
| Dental radiography | Extraoral radiography (panoramic radiography or cone-beam CT) |
| Succesive follow-ups | Providing the patient with cheek-retractors |
| Regular follow-ups by using oral health assessment forms or SmileMate monitoring |
| Clinical Consideration | Clinical Condition/Situation | Suggested Dental Recommendations and Management |
|---|---|---|
| Respiratory | Breathlessness | Periodic recording of oxygen saturation for a week by the patient prior to treatment |
| Continous monitoring of oxygen saturation by "pulse oximeter" during the treatment | ||
| Practice and train breathing techniques (inspiration to expiration ratio of 1:2) | ||
| Bilateral mandibular blocks should not be administered | ||
| Clinics must include medical emergency first aid kits (oxygen cylinders) | ||
| Cough | Practice and train breathing techniques (inspiration to expiration ratio of 1:2) | |
| Antitussives or lozenges for immediate cough suppression. | ||
| Chair position during the treatment: Upright or semi supine position | ||
| Psychosocial | Fear in COVID-19 recovered pts. | Virtual consultations using AI based patient management screening tools |
| Fear and Anxiety in COVID-19 recovered pts | Appointments to be scheduled after complete health assessment | |
| Family members should also accompany during the appointment. | ||
| First or last time slot should be scheduled | ||
| Screen the patients using "The Seattle System for anxiety and fear | ||
| To be treated with utmost care and empathy | ||
| Stress in COVID-19 recovered pts. | Psychotherapeutic interventions can be used | |
| Fear in Dentists | Learning about the virus and post-COVID symptoms | |
| Oral health | Inflammatory reactions (salivary glands, tongue) | Dental follow-ups of recovered patients |
| Pain | Acetaminophen (not exceeding 60 mg/kg/day or 3 mg/day) | |
| Periodontal | Oral health hygiene training (online, if necessary) | |
| Regular online follow ups (patient management software can be used) | ||
| Musco-skeletal | Associated sleeplessness and anxiety | Non-pharmacological (3 ps Technique by RCOT) |
| Pharmacological interventions (tranquilizers, muscle relaxants or anxiolytics) | ||
| Fatigue | Pre-planning the treatment | |
| Short appointments and relaxing setting | ||
| Bleeding disorders | Active Bleeding | ASH guidelines for controlling bleeding (who are not under thromboprophylaxis) |
| Bleeding disorders | Pain | Acetaminophen (not exceeding 60 mg/kg/day or 3 mg/day) |
| (Hypercoagulability thromboembolic disorders/Congenital Bleeding Diathesis) cardiac Damages (Stress cardiomyopathy) | Pain due to Irreversible Pulpitis/necrosis | Endodontic treatment should be considered over extraction |
| Endodontic consideration: Copious irrigation with sodium hypochlorite sol. | ||
| Endodontic consideration: lntracanal dressing to limit the bleeding from canals | ||
| Surgical consideration: Short appointments | ||
| Safe anaesthsia: Infiltration from the vestibule side of the mouth | ||
| Surgical consideration: Resorbable sutures and haemostatic agent to be used | ||
| Instruction to patient.: Maintain a pressure tampon for 1–2 h after extraction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chakraborty, T.; Jamal, R.F.; Battineni, G.; Teja, K.V.; Marto, C.M.; Spagnuolo, G. A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management. Int. J. Environ. Res. Public Health 2021, 18, 5131. https://doi.org/10.3390/ijerph18105131
Chakraborty T, Jamal RF, Battineni G, Teja KV, Marto CM, Spagnuolo G. A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management. International Journal of Environmental Research and Public Health. 2021; 18(10):5131. https://doi.org/10.3390/ijerph18105131
Chicago/Turabian StyleChakraborty, Trishnika, Rizwana Fathima Jamal, Gopi Battineni, Kavalipurapu Venkata Teja, Carlos Miguel Marto, and Gianrico Spagnuolo. 2021. "A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management" International Journal of Environmental Research and Public Health 18, no. 10: 5131. https://doi.org/10.3390/ijerph18105131
APA StyleChakraborty, T., Jamal, R. F., Battineni, G., Teja, K. V., Marto, C. M., & Spagnuolo, G. (2021). A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management. International Journal of Environmental Research and Public Health, 18(10), 5131. https://doi.org/10.3390/ijerph18105131








