Spatial Patterns in Hospital-Acquired Infections in Portugal (2014–2017)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Study Design
2.3. Data Sources
2.4. Data Selection
2.5. Data Analysis
2.6. Ethics Statement
3. Results
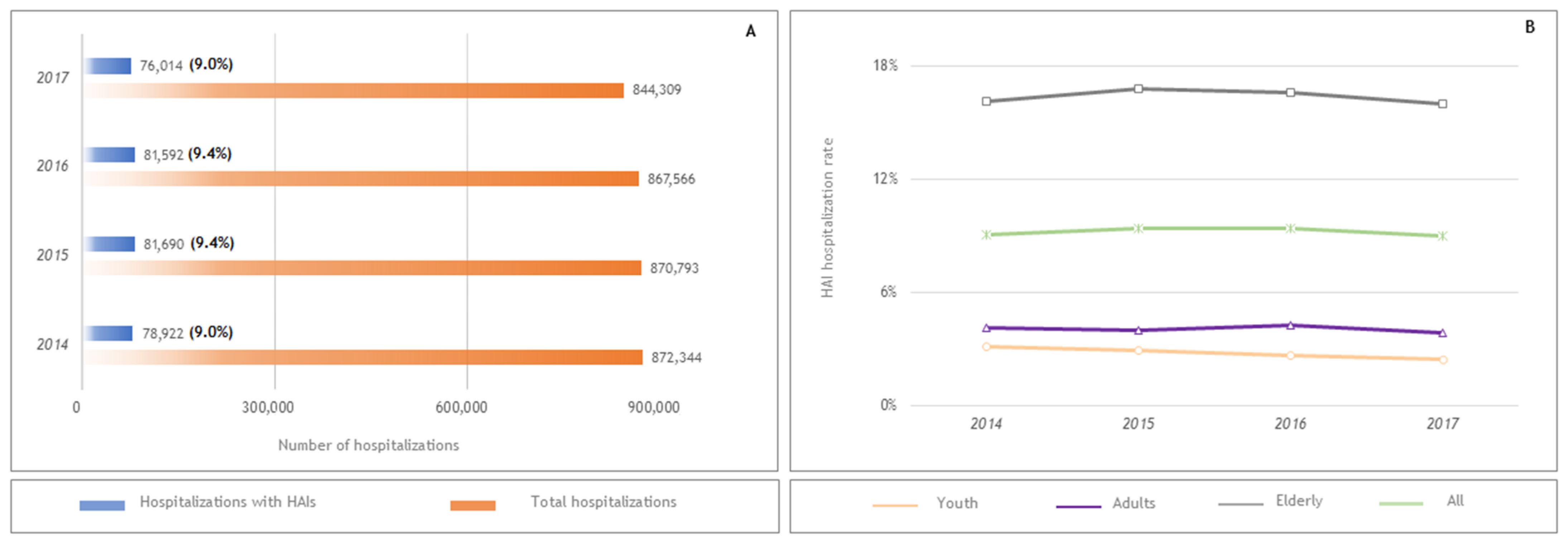
3.1. Profiles of HAI Cases and Their Sociodemographic and Clinical Characteristics
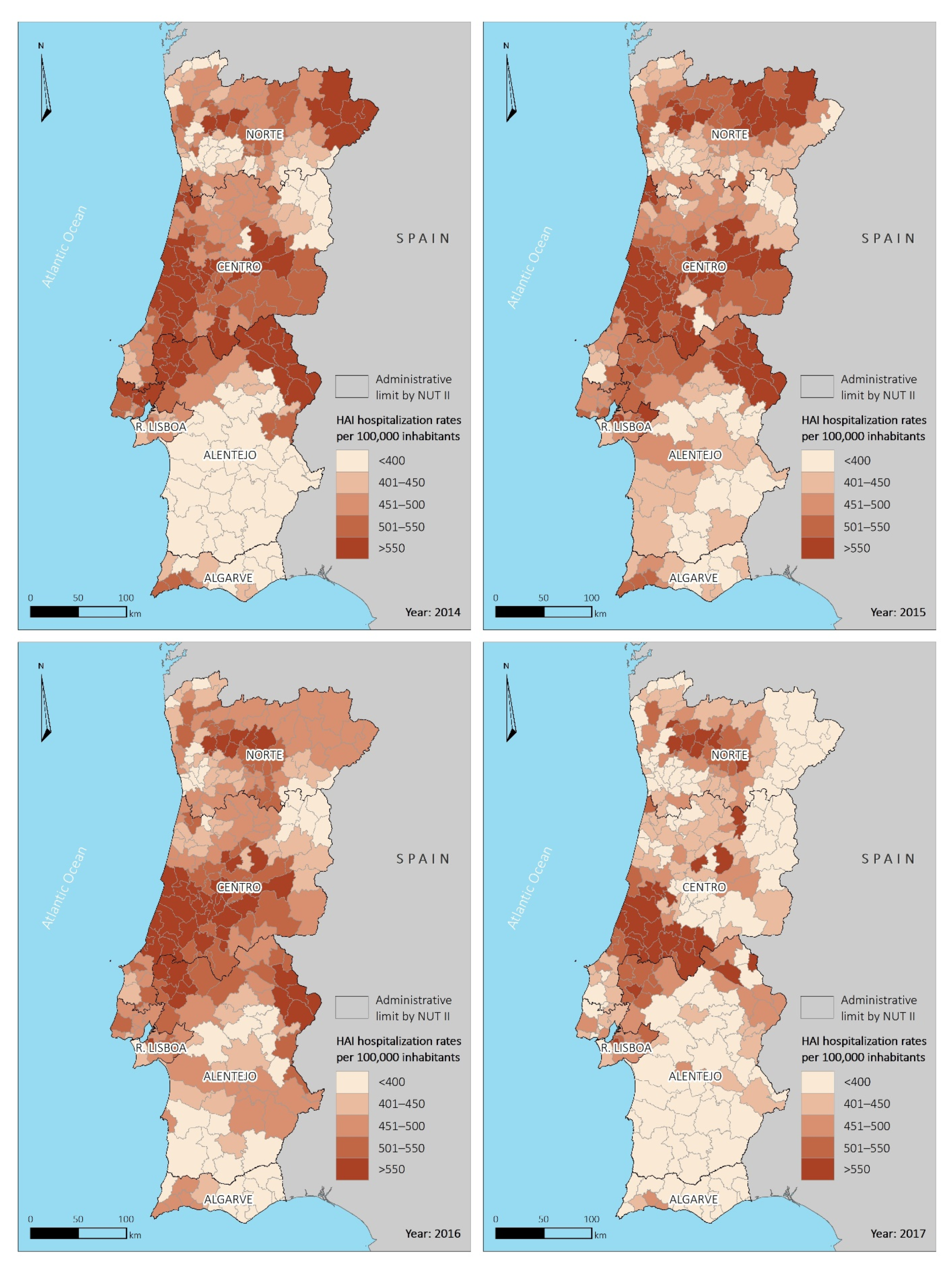
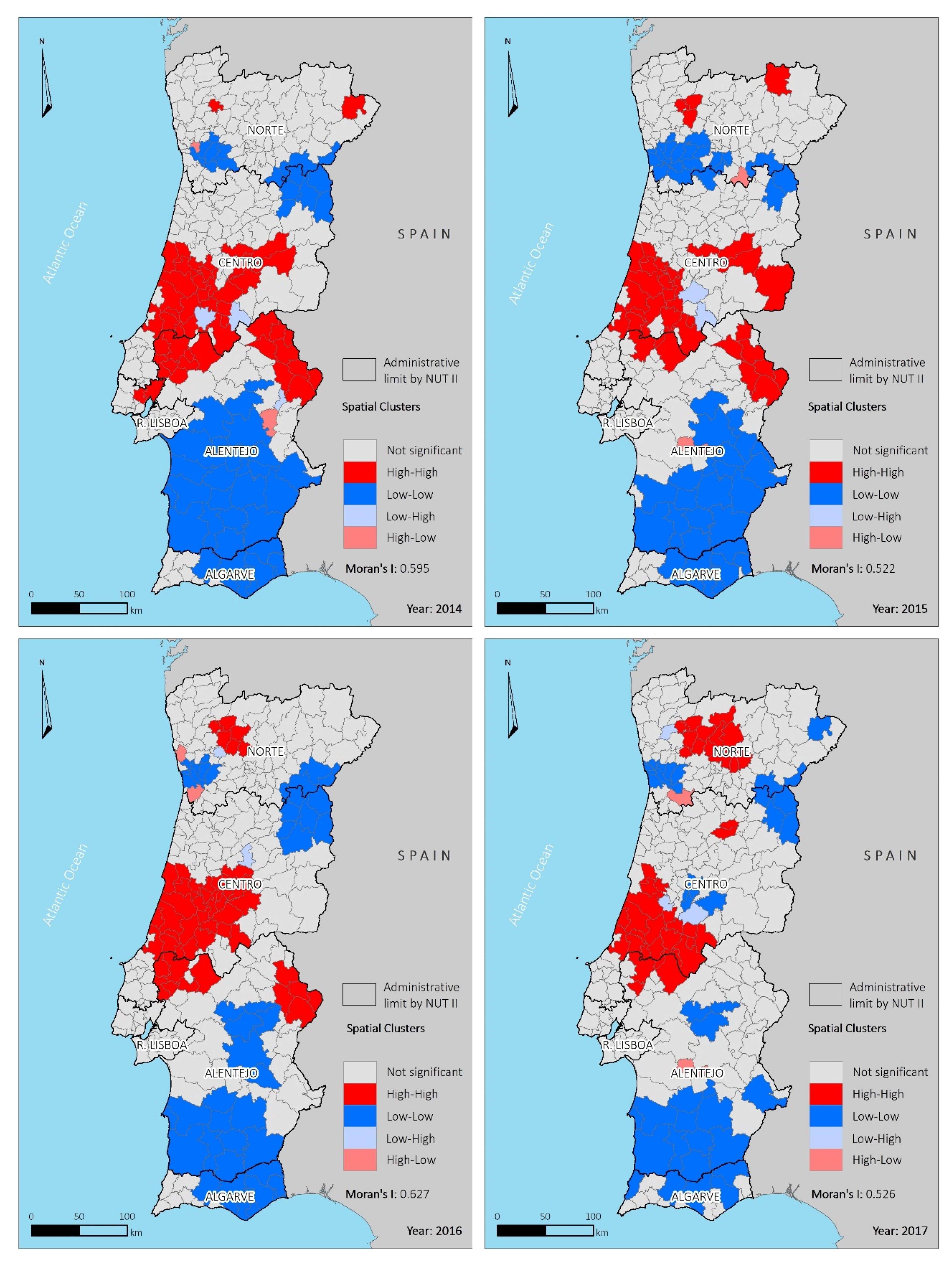
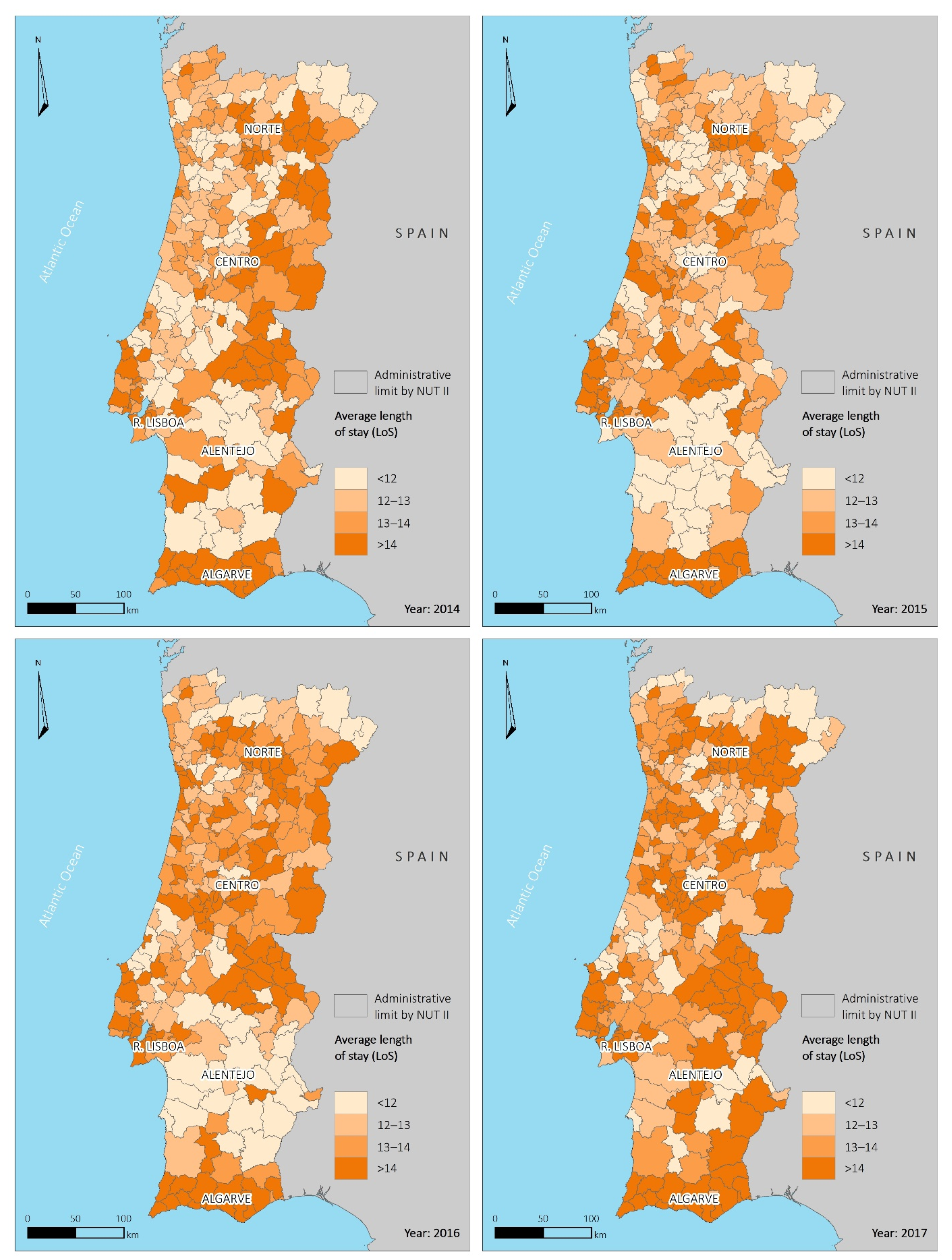
3.2. Spatial Distribution of Hospitalization Rates by Municipality
4. Discussion
4.1. Spatial Asymmetries
4.2. Limitations
4.3. Implications and Future Work
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haque, M.; Sartelli, M.; McKimm, J.; Bin Abu Bakar, M. Health care-associated infections–an overview. Infect. Drug Resist. 2018, 11, 2321–2333. [Google Scholar] [CrossRef]
- Habboush, Y.; Yarrarapu, S.N.S.; Guzman, N. Infection Control. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2020. [Google Scholar]
- Horan, T.C.; Andrus, M.; Dudeck, M.A. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Control 2008, 36, 309–332. [Google Scholar] [CrossRef]
- Benenson, A.S. Control of Communicable Diseases Manual, 16th ed.; Heymann, D.L., Ed.; American Public Health Association Press: Washington, DC, USA, 2008. [Google Scholar]
- Boucher, H.W.; Corey, G.R. Epidemiology of Methicillin-ResistantStaphylococcus aureus. Clin. Infect. Dis. 2008, 46, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Gahlot, R.; Nigam, C.; Kumar, V.; Yadav, G.; Anupurba, S. Catheter-related bloodstream infections. Int. J. Crit. Illn. Inj. Sci. 2014, 4, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Giardin, J.M.; Chamorro, I.O.; Ríos, L.V.; Aroca, J.J.; Arata, M.I.G.; López, J.V.S.; Santillán, M.G. Blood stream infections associated with central and peripheral venous catheters. BMC Infect. Dis. 2019, 19, 841. [Google Scholar] [CrossRef] [PubMed]
- Trouillet, J.-L. Ventilator-Associated Pneumonia: A Comprehensive Review. Hosp. Pract. 2012, 40, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Evans, S. Could a risk-assessment tool prevent hospital-acquired pneumonia? Br. J. Nurs. 2018, 27, 402–404. [Google Scholar] [CrossRef]
- Slimings, C.; Riley, T.V. Antibiotics and hospital-acquired Clostridium difficile infection: Update of systematic review and meta-analysis. J. Antimicrob. Chemother. 2014, 69, 881–891. [Google Scholar] [CrossRef]
- Czepiel, J.; Dróżdż, M.; Pituch, H.; Kuijper, E.J.; Perucki, W.; Mielimonka, A.; Goldman, S.; Wultańska, D.; Garlicki, A.; Biesiada, G. Clostridium difficile infection: Review. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1211–1221. [Google Scholar] [CrossRef]
- Garner, B.H.; Anderson, D.J. Surgical Site Infections. Infect. Dis. Clin. North Am. 2016, 30, 909–929. [Google Scholar] [CrossRef]
- Kolasiński, W. Surgical site infections-review of current knowledge, methods of prevention. Pol. J. Surg. 2018, 91, 41–47. [Google Scholar] [CrossRef]
- Ramanathan, R.; Duane, T.M. Urinary Tract Infections in Surgical Patients. Surg. Clin. N. Am. 2014, 94, 1351–1368. [Google Scholar] [CrossRef]
- Tandogdu, Z.; Wagenlehner, F.M. Global epidemiology of urinary tract infections. Curr. Opin. Infect. Dis. 2016, 29, 73–79. [Google Scholar] [CrossRef]
- Cassini, A.; Plachouras, D.; Eckmanns, T.; Abu Sin, M.; Blank, H.-P.; Ducomble, T.; Haller, S.; Harder, T.; Klingeberg, A.; Sixtensson, M.; et al. Burden of Six Healthcare-Associated Infections on European Population Health: Estimating Incidence-Based Disability-Adjusted Life Years through a Population Prevalence-Based Modelling Study. PLoS Med. 2016, 13, e1002150. [Google Scholar] [CrossRef] [PubMed]
- Barrasa-Villar, J.I.; Aibar-Remón, C.; Prieto-Andrés, P.; Mareca-Doñate, R.; Moliner-Lahoz, J. Impact on Morbidity, Mortality, and Length of Stay of Hospital-Acquired Infections by Resistant Microorganisms. Clin. Infect. Dis. 2017, 65, 644–652. [Google Scholar] [CrossRef]
- WHO. Report on the Burden of Endemic Health Care-Associated Infection Worldwide; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Allegranzi, B.; Nejad, S.B.; Combescure, C.; Graafmans, W.; Attar, H.; Donaldson, L.; Pittet, D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011, 377, 228–241. [Google Scholar] [CrossRef]
- WHO. Healthcare-Associated Infections: Fact Sheet. Available online: http://www.who.int/gpsc/country_work/gpsc_ccisc_fact_sheet_en.pdf (accessed on 24 November 2020).
- Barbato, D.; Castellani, F.; Angelozzi, A.; Isonne, C.; Baccolini, V.; Migliara, G.; Marzuillo, C.; De Vito, C.; Villari, P.; Romano, F.; et al. Prevalence survey of healthcare-associated infections in a large teaching hospital. Ann. Ig. Med. Prev. Comunita 2019, 31, 423–435. [Google Scholar]
- Gori, F.; Vonci, N.; Santoriello, G.; Quercioli, C.; Messina, G.; Sancasciani, S. Hospital acquired infection, evaluation of point of prevalence in a 147 beds italian hospital. Eur. J. Public Health 2019, 29, 29. [Google Scholar] [CrossRef]
- Saleem, Z.; Godman, B.; Hassali, M.A.; Hashmi, F.K.; Azhar, F.; Rehman, I.U. Point prevalence surveys of health-care-associated infections: A systematic review. Pathog. Glob. Health 2019, 113, 191–205. [Google Scholar] [CrossRef] [PubMed]
- DGS. Programa de Prevenção e Controlo de Infeções e de Resistência Aos Antimicrobianos; Direção-Geral da Saúde: Lisboa, Portugal, 2017; p. 23. [Google Scholar]
- DGS. Infeções e Resistências aos Antimicrobianos: Relatório Anual do Programa Prioritário; Direção-Geral da Saúde: Lisboa, Portugal, 2018. [Google Scholar]
- Costa, R.D.; Baptista, J.P.; Freitas, R.; Martins, P.J. Hospital-Acquired Pneumonia in a Multipurpose Intensive Care Unit: One-Year Prospective Study. Acta Médica Port. 2019, 32, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Klevens, R.M.; Edwards, J.R.; Richards, C.L.; Horan, T.C.; Gaynes, R.P.; Pollock, D.A.; Cardo, D.M. Estimating Health Care-Associated Infections and Deaths in U.S. Hospitals, 2002. Public Health Rep. 2007, 122, 160–166. [Google Scholar] [CrossRef]
- WHO. The burden of health care-associated infection. In Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care; World Health Organization: Geneva, Switzerland, 2009; Volume 3. [Google Scholar]
- Monegro, A.F.; Muppidi, V.; Regunath, H. Hospital Acquired Infections. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2021. [Google Scholar]
- Collins, A. Preventing Health Care–Associated Infections. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R., Ed.; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- Ducel, G.; Fabry, J.; Nicolle, L. Prevention of Hospital-Acquired Infections: A Practical Guide, 2nd ed.; World Health Organization: Geneva, Switzerland, 2002; p. 64. [Google Scholar]
- Evans, R.S. Electronic Health Records: Then, Now, and in the Future. Yearb. Med. Inform. 2016, 25, 48–61. [Google Scholar] [CrossRef]
- Redondo-González, O.; Tenías, J.M.; Arias, Á.; Lucendo, A.J. Validity and Reliability of Administrative Coded Data for the Identification of Hospital-Acquired Infections: An Updated Systematic Review with Meta-Analysis and Meta-Regression Analysis. Health Serv. Res. 2018, 53, 1919–1956. [Google Scholar] [CrossRef] [PubMed]
- Jhung, M.A.; Banerjee, S.N. Administrative Coding Data and Health Care–Associated Infections. Clin. Infect. Dis. 2009, 49, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Schmiedeskamp, M.; Harpe, S.; Polk, R.; Oinonen, M.; Pakyz, A. Use of International Classification of Diseases, Ninth Revision Clinical Modification Codes and Medication Use Data to Identify Nosocomial Clostridium difficile Infection. Infect. Control. Hosp. Epidemiol. 2009, 30, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, A.; Souza, J.; Freitas, A. The Use of Artificial Intelligence for Clinical Coding Automation: A Bibliometric Analysis. In Proceedings of the Advances in Human Factors, Business Management, Training and Education, L’Aquila, Italy, 6–8 October 2020; J.B. Metzler: L’Aquila, Italy, 2020; pp. 274–283. [Google Scholar]
- Alonso, V.; Santos, J.V.; Pinto, M.; Ferreira, J.; Lema, I.; Lopes, F.; Freitas, A. Health records as the basis of clinical coding: Is the quality adequate? A qualitative study of medical coders’ perceptions. Health Inf. Manag. J. 2020, 49, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Alonso, V.; Santos, J.V.; Pinto, M.; Ferreira, J.; Lema, I.; Lopes, F.; Freitas, A. Problems and Barriers during the Process of Clinical Coding: A Focus Group Study of Coders’ Perceptions. J. Med. Syst. 2020, 44, 62. [Google Scholar] [CrossRef]
- Van Mourik, M.S.M.; Van Duijn, P.J.; Moons, K.G.M.; Bonten, M.J.M.; Lee, G.M. Accuracy of administrative data for surveillance of healthcare-associated infections: A systematic review. BMJ Open 2015, 5, e008424. [Google Scholar] [CrossRef]
- Goto, M.; Ohl, M.E.; Schweizer, M.L.; Perencevich, E.N. Accuracy of Administrative Code Data for the Surveillance of Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2014, 58, 688–696. [Google Scholar] [CrossRef]
- Sousa-Pinto, B.; Marques, B.; Lopes, F.; Freitas, A. Frequency and Impact of Adverse Events in Inpatients: A Nationwide Analysis of Episodes between 2000 and 2015. J. Med. Syst. 2018, 42, 48. [Google Scholar] [CrossRef]
- OECD. Divided We Stand: Why Inequality Keeps Rising. An Overview of Growing Income Inequalities in OECD Countries: Main Findings. Available online: http://www.oecd.org/social/inequality.htm (accessed on 3 December 2020).
- Costa, J.; Alarcão, J.; Araujo, F.; Ascenção, R.; Caldeira, D.; Fiorentino, F.; Gil, V.; Gouveia, M.; Lourenço, F.; Mello, E.S.A.; et al. The burden of atherosclerosis in Portugal. European heart journal. Qual. Care Clin. Outcomes 2020. [Google Scholar] [CrossRef]
- INE. População Residente (N.º) por Local de Residência (NUTS-2013), Sexo e Grupo Etário; Anual. Available online: https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_indicadores&indOcorrCod=0008273&contexto=bd&selTab=tab2 (accessed on 15 November 2020).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Li, B.; Evans, D.; Faris, P.; Dean, S.; Quan, H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv. Res. 2008, 8, 12. [Google Scholar] [CrossRef]
- Freitas, A.; Lema, I.; Da Costa-Pereira, A. Comorbidity Coding Trends in Hospital Administrative Databases. In Proceedings of the Advances in Human Factors, Business Management, Training and Education, Orlando, FL, USA, 27–31 July 2016; pp. 609–617. [Google Scholar]
- Eurostat. Revision of the European Standard Population; European Comission: Luxembourg, 2013. [Google Scholar]
- Kennedy, S. The small number problem and the accuracy of spatial databases. In Accuracy of Spatial Databases; Goodchild, M., Gopal, S., Eds.; Taylor and Francis: London, UK, 1994; pp. 187–196. [Google Scholar]
- Bailey, T.C. Spatial statistical methods in health. Cadernos de Saúde Pública 2001, 17, 1083–1098. [Google Scholar] [CrossRef] [PubMed]
- Gatrell, A.; Bailey, T. Interactive spatial data analysis in medical geography. Soc. Sci. Med. 1996, 42, 843–855. [Google Scholar] [CrossRef]
- Assunção, R. Estatística Espacial com Aplicações em Epidemiologia, Economia e Sociologia; Associação Brasileira de Estatística: São Paulo, Brazil, 2001. [Google Scholar]
- Câmara, G.; Carvalho, M.S.; Cruz, O.G.; Correa, V. Análise espacial de áreas. In Análise Espacial de Dados Geográficos; Druck, S., Carvalho, M.S., Câmara, G., Vieira, A.M., Eds.; Divisão de Processamentos de Imagens–Instituto Nacional de Pesquisas Espaciais: São José dos Campos, Brazil, 2002. [Google Scholar]
- Anselin, L. Local Indicators of Spatial Association-LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Gravel, D.; Taylor, G.; Ofner, M.; Johnston, L.; Loeb, M.; Roth, V.R.; Stegenga, J.; Bryce, E.; Matlow, A.; Canadian Nosocomial Infection Surveillance Program. Point prevalence survey for healthcare-associated infections within Canadian adult acute-care hospitals. J. Hosp. Infect. 2007, 66, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Danasekaran, R.; Mani, G.; Annadurai, K. Prevention of healthcare-associated infections: Protecting patients, saving lives. Int. J. Commun. Med. Public Health 2014, 1, 67–68. [Google Scholar] [CrossRef]
- Giraldi, G.; Montesano, M.; Sandorfi, F.; Iachini, M.; Orsi, G.B. Excess length of hospital stay due to healthcare acquired infections: Methodologies evaluation. Ann. Ig. Med. Prev. Comunita 2019, 31, 507–516. [Google Scholar]
- Ohannessian, R.; Gustin, M.-P.; Bénet, T.; Gerbier-Colomban, S.; Girard, R.; Argaud, L.; Rimmelé, T.; Guerin, C.; Bohé, J.; Piriou, V.; et al. Estimation of Extra Length of Stay Attributable to Hospital-Acquired Infections in Adult ICUs Using a Time-Dependent Multistate Model*. Crit. Care Med. 2018, 46, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, G.; Murthy, A.; Beyersmann, J.; Harbarth, S.J. Estimating the impact of healthcare-associated infections on length of stay and costs. Clin. Microbiol. Infect. 2010, 16, 1729–1735. [Google Scholar] [CrossRef] [PubMed]
- Manoukian, S.; Stewart, S.; Dancer, S.; Graves, N.; Mason, H.; McFarland, A.; Robertson, C.; Reilly, J. Estimating excess length of stay due to healthcare-associated infections: A systematic review and meta-analysis of statistical methodology. J. Hosp. Infect. 2018, 100, 222–235. [Google Scholar] [CrossRef] [PubMed]
- DGS. Prevenção e Controlo de Infeções e de Resistência aos Antimicrobianos em Números; Direção-Geral da Saúde: Lisboa, Portugal, 2015. [Google Scholar]
- Iosifidis, E.; Pitsava, G.; Roilides, E. Ventilator-associated pneumonia in neonates and children: A systematic analysis of diagnostic methods and prevention. Future Microbiol. 2018, 13, 1431–1446. [Google Scholar] [CrossRef]
- Zingg, W.; Hopkins, S.; Gayet-Ageron, A.; Holmes, A.; Sharland, M.; Suetens, C.; Almeida, M.; Asembergiene, J.; Borg, M.A.; Budimir, A.; et al. Health-care-associated infections in neonates, children, and adolescents: An analysis of paediatric data from the European Centre for Disease Prevention and Control point-prevalence survey. Lancet Infect. Dis. 2017, 17, 381–389. [Google Scholar] [CrossRef]
- Aelami, M.; Lotfi, M.; Zingg, W. Ventilator-associated pneumonia in neonates, infants and children. Antimicrob. Resist. Infect. Control 2014, 3, 30. [Google Scholar] [CrossRef]
- Burgos, J.; Falcó, V.; Almirante, B. Chemical pharmacotherapy for hospital-acquired pneumonia in the elderly. Expert Opin. Pharmacother. 2019, 20, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, J.D.; Rother, C.; Salih, W.; Ewig, S. Healthcare-Associated Pneumonia Does Not Accurately Identify Potentially Resistant Pathogens: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2014, 58, 330–339. [Google Scholar] [CrossRef]
- Burton, L.A.; Price, R.; Barr, K.E.; McAuley, S.M.; Allen, J.B.; Clinton, A.M.; Phillips, G.; Marwick, C.A.; McMurdo, M.E.T.; Witham, M.D. Hospital-acquired pneumonia incidence and diagnosis in older patients. Age Ageing 2016, 45, 171–174. [Google Scholar] [CrossRef]
- Xia, J.; Gao, J.; Tang, W. Nosocomial infection and its molecular mechanisms of antibiotic resistance. Biosci. Trends 2016, 10, 14–21. [Google Scholar] [CrossRef]
- De Oliveira, T.F.L.; Filho, I.S.G.; Passos, J.D.S.; Da Cruz, S.S.; Oliveira, M.T.; Trindade, S.C.; Machado, A.D.S.; Coelho, J.M.F.; Santos, C.M.L.; Cerqueira, E.D.M.M. Fatores associados à pneumonia nosocomial em indivíduos hospitalizados. Rev. Assoc. Méd. Bras. 2011, 57, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, A.; Lobo, M.; Duarte, L.; Souza, J.; Santos, P.; Freitas, A. Landscapes on Prevention Quality Indicators: A Spatial Analysis of Diabetes Preventable Hospitalizations in Portugal (2016–2017). Int. J. Environ. Res. Public Health 2020, 17, 8387. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.K.; Vakharia, N.; Pile, J.; Howell, E.H.; Rothberg, M.B. Preventable Admissions on a General Medicine Service: Prevalence, Causes and Comparison with AHRQ Prevention Quality Indicators—A Cross-Sectional Analysis. J. Gen. Intern. Med. 2016, 31, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, A.; Castro, P.; Gonçalves-Pinho, M.; Teixeira, J.; Santos, J.V.; Viana, J.; Lobo, M.; Santos, P.; Freitas, A. Primary health care quality indicators: An umbrella review. PLoS ONE 2019, 14, e0220888. [Google Scholar] [CrossRef] [PubMed]
- Sarmento, J.; Alves, C.; Oliveira, P.; Sebastião, R.; Santana, R. Caracterização e Evolução dos Internamentos Evitáveis em Portugal: Impacto de Duas Abordagens Metodológicas. Acta Médica Port. 2015, 28, 590–600. [Google Scholar] [CrossRef][Green Version]
- Van Loenen, T.; Berg, M.J.V.D.; Westert, G.P.; Faber, M.J. Organizational aspects of primary care related to avoidable hospitalization: A systematic review. Fam. Pract. 2014, 31, 502–516. [Google Scholar] [CrossRef]
- Wen, T.; Attenello, F.J.; He, S.; Cen, Y.; Kim-Tenser, M.A.; Sanossian, N.; Amar, A.P.; Mack, W.J. Racial and Socioeconomic Disparities in Incidence of Hospital-Acquired Complications Following Cerebrovascular Procedures. Neurosurgery 2014, 75, 43–50. [Google Scholar] [CrossRef]
- Chauhan, A.; Walton, M.; Manias, E.; Walpola, R.L.; Seale, H.; Latanik, M.; Leone, D.; Mears, S.; Harrison, R. The safety of health care for ethnic minority patients: A systematic review. Int. J. Equity Health 2020, 19, 1–25. [Google Scholar] [CrossRef]
- Fernando, S.A.; Gray, T.J.; Gottlieb, T. Healthcare-acquired infections: Prevention strategies. Intern. Med. J. 2017, 47, 1341–1351. [Google Scholar] [CrossRef]
- Boev, C.; Kiss, E. Hospital-Acquired Infections. Crit. Care Nurs. Clin. N. Am. 2017, 29, 51–65. [Google Scholar] [CrossRef]
- Umscheid, C.A.; Mitchell, M.D.; Doshi, J.A.; Agarwal, R.; Williams, K.; Brennan, P.J. Estimating the Proportion of Healthcare-Associated Infections That Are Reasonably Preventable and the Related Mortality and Costs. Infect. Control Hosp. Epidemiol. 2011, 32, 101–114. [Google Scholar] [CrossRef] [PubMed]
- McKibben, L.; Fowler, G.; Horan, T.; Brennan, P. Ensuring rational public reporting systems for health care–associated infections: Systematic literature review and evaluation recommendations. Am. J. Infect. Control 2006, 34, 142–149. [Google Scholar] [CrossRef]
- Friedrich, A.W. Control of hospital acquired infections and antimicrobial resistance in Europe: The way to go. Wien. Med. Wochenschr. 2019, 169, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Miguel, A.; Marques, B.; Freitas, A.; Lopes, F.; Azevedo, L.; Pereira, A.C. Detection of adverse drug reactions using hospital databases-a nationwide study in Portugal. Pharmacoepidemiol. Drug Saf. 2013, 22, 907–913. [Google Scholar] [CrossRef] [PubMed]
- INE. Estatísticas da Saúde. Available online: https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=inepublicacoes&PUBLICACOESpubboui=320460040&PUBLICACOESmodo=2 (accessed on 4 April 2021).
| Hospital-Acquired Infections | ICD-9-CM Codes | ICD-10-CM Codes | ||||
|---|---|---|---|---|---|---|
| Catheter-related bloodstream infections | 038.12 | 038.11 | 041.11 | A41.01 | A41.02 | B95.61 |
| 041.12 | 996.62 | 999.3x | B95.62 | T80.2- | T82.7- | |
| Infection by Clostridium difficile | 008.45 | A04.7- | ||||
| Nosocomial Pneumonia | 480x | 481 | 482x | A48.1 | B01.2 | B05.2 |
| 483x | 485 | 486 | J10.0- | J11.0- | J12- | |
| 487.0 | 997.3x | J13 | J14 | J15- | ||
| J16- | J17 | J18- | ||||
| Surgical site infection | 483x | 485 | 486 | J10.0- | J11.0- | J12- |
| 487.0 | 569.61 | 682x | J13 | J14 | J15- | |
| 996.6x | 997.3x | 996.7x | J16- | J17 | J18- | |
| 998.5x | 998.6 | 999.34 | O86.0- | T81.4- | T81.8- | |
| 999.39 | T84.5 | T84.6 | T84.7 | |||
| T88.0- | T88.8- | Z48.8- | ||||
| Urinary tract infection | 590.1x | 590.2 | 590.8x | N10 | N15- | N16 |
| 590.9 | 595.0 | 595.4 | N30- | N30.81 | N39.0 | |
| 599.0 | 996.64 | 997.5 | N99.89 | T83.5- | ||
| Age Category | ||||
|---|---|---|---|---|
| Characteristics | Total | Youth | Adults | Elderly |
| Total HAI hospitalizations, n (%) | 318,218 (100.0) | 14,851 (4.7) | 57,700 (18.1) | 245,667 (77.2) |
| Age, (years), Median, (IQR) | 79 (20.0) | 2 (7.0) | 54 (15.0) | 82 (11.0) |
| Length of stay (LoS), (days), Median, (IQR) | 9 (10.0) | 6 (5.0) | 10 (11.0) | 10 (10.0) |
| Sex, n (%) | ||||
| Men | 158,552 (49.8) | 7921 (53.3) | 33,822 (58.6) | 116,809 (47.5) |
| Women | 159,666 (50.2) | 6930 (46.6) | 23,878 (41.4) | 128,858 (52.5) |
| Charlson comorbidity index, n (%) | ||||
| 0 | 80,401 (25.3) | 12,934 (87.1) | 22,736 (39.4) | 44,731 (18.2) |
| 1–2 | 137,858 (43.3) | 1751 (11.8) | 21,054 (36.5) | 115,053 (46.8) |
| 3–4 | 63,897 (20.1) | 110 (0.7) | 6868 (11.9) | 56,919 (23.2) |
| >4 | 36,062 (11.3) | 56 (0.4) | 7042 (12.2) | 28,964 (11.8) |
| Destination after discharge, n (%) | ||||
| Residence | 248,069 (78.0) | 14,250 (96.0) | 48,349 (83.8) | 185,470 (75.5) |
| Hospital transfer | 7484 (2.4) | 421 (2.8) | 2408 (4.2) | 4655 (1.9) |
| Discharge against medical advice | 881 (0.3) | 23 (0.2) | 505 (0.9) | 353 (0.1) |
| Transfer to continuous care | 11,697 (3.7) | 58 (0.4) | 1676 (2.9) | 9963 (4.1) |
| Deceased | 50,087 (15.7) | 99 (0.7) | 4762 (8.3) | 45,226 (18.4) |
| Admission type, n (%) | ||||
| Scheduled | 17,916 (5.6) | 1280 (8.6) | 6525 (11.3) | 10,111 (4.1) |
| Unplanned | 300,181 (94.4) | 13,569 (91.4) | 51,133 (88.6) | 235,479 (95.9) |
| Others | 121 (0.0) | 2 (0.0) | 42 (0.1) | 77 (0.0) |
| Admissions by NUT II, n (%) | ||||
| North | 100,933 (31.7) | 4851 (32.7) | 19,922 (34.5) | 76,160 (31.0) |
| Center | 87,719 (27.6) | 3266 (22.0) | 12,651 (21.9) | 71,802 (29.2) |
| Lisboa Region | 94,190 (29.6) | 5422 (36.5) | 19,768 (34.3) | 69,000 (28.1) |
| Alentejo | 22,944 (7.2) | 718 (4.8) | 3211 (5.6) | 19,015 (7.8) |
| Algarve | 12,432 (3.9) | 594 (4.0) | 2148 (3.7) | 9690 (3.9) |
| Hospital-acquired infections context 1 | ||||
| Total, n (%) | 340,125 (100.0) | 15,074 (4.4) | 60,608 (17.8) | 264,443 (77.7) |
| Catheter-related bloodstream infections | 19,581 (5.8) | 1448 (9.6) | 6435 (10.5) | 11,698 (4.4) |
| Intestinal infection by Clostridium difficile | 3822 (1.1) | 49 (0.3) | 609 (1.0) | 3164 (1.2) |
| Nosocomial pneumonia | 197,188 (58.0) | 10,957 (72.7) | 33,064 (54.6) | 153,167 (57.9) |
| Surgical site infection | 11,883 (3.5) | 522 (3.5) | 5795 (9.6) | 5566 (2.1) |
| Urinary tract infection | 107,651 (31.7) | 2098 (13.9) | 14,705 (24.3) | 90,848 (34.4) |
| Hospital-Acquired Infections | Total n (%) | Alive n (%) | Deceased n (%) | IL (%) |
|---|---|---|---|---|
| Catheter-related bloodstream infections | 19,581 (5.8) | 16,845 (5.9) | 2736 (4.9) | 14.0 |
| Infection by Clostridium difficile | 3822 (1.1) | 3186 (1.1) | 636 (1.1) | 16.6 |
| Nosocomial pneumonia | 197,188 (58.0) | 160,762 (56.4) | 36,426 (65.8) | 18.5 |
| Surgical site infection | 11,883 (3.5) | 11,296 (4.0) | 587 (1.1) | 5.0 |
| Urinary tract infection | 107,651 (31.7) | 92,707 (32.6) | 14,944 (27.0) | 13.9 |
| Hospital-Acquired Infections | 0 | 1–2 | 3–4 | >4 |
|---|---|---|---|---|
| Catheter-related bloodstream infections | 5398 (27.6) | 6964 (35.5) | 4101 (20.9) | 3128 (16.0) |
| Infection by Clostridium difficile | 929 (24.3) | 1592 (41.7) | 823 (21.5) | 478 (12.5) |
| Nosocomial pneumonia | 47,862 (24.3) | 90,414 (45.8) | 38,779 (19.7) | 20,133 (10.2) |
| Surgical site infection | 6453 (54.3) | 3480 (29.3) | 948 (8.0) | 1002 (8.4) |
| Urinary tract infection | 24,013 (22.3) | 45,178 (42.0) | 24,338 (22.6) | 14,122 (13.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teixeira, H.; Freitas, A.; Sarmento, A.; Nossa, P.; Gonçalves, H.; Pina, M.d.F. Spatial Patterns in Hospital-Acquired Infections in Portugal (2014–2017). Int. J. Environ. Res. Public Health 2021, 18, 4703. https://doi.org/10.3390/ijerph18094703
Teixeira H, Freitas A, Sarmento A, Nossa P, Gonçalves H, Pina MdF. Spatial Patterns in Hospital-Acquired Infections in Portugal (2014–2017). International Journal of Environmental Research and Public Health. 2021; 18(9):4703. https://doi.org/10.3390/ijerph18094703
Chicago/Turabian StyleTeixeira, Hugo, Alberto Freitas, António Sarmento, Paulo Nossa, Hernâni Gonçalves, and Maria de Fátima Pina. 2021. "Spatial Patterns in Hospital-Acquired Infections in Portugal (2014–2017)" International Journal of Environmental Research and Public Health 18, no. 9: 4703. https://doi.org/10.3390/ijerph18094703
APA StyleTeixeira, H., Freitas, A., Sarmento, A., Nossa, P., Gonçalves, H., & Pina, M. d. F. (2021). Spatial Patterns in Hospital-Acquired Infections in Portugal (2014–2017). International Journal of Environmental Research and Public Health, 18(9), 4703. https://doi.org/10.3390/ijerph18094703








