1. Introduction
Medical institutions are places to take care of patients’ health and treat diseases. Ensuring patient safety should be one of the core goals. Research has shown that while relevant rules, policies, procedures and training often existed, they were not sufficient to change corresponding behavior. Therefore, organizational climate approaches have been employed to highlight social aspects of the work environment, making certain characteristics more salient to employees, thus cueing a change toward desired behaviors. A successful example is the induction of information security climate in medical facilities [
1]. Similarly, having a good patient safety culture can reduce medical errors, improve patient prognosis and reduce the length of hospital stay and related medical expenses [
2]. Furthermore, it can also reduce the propensity of medical disputes, ameliorate psychological pressure and work stress on employees, thus preventing turnover by mitigating burnout, especially emotional exhaustion [
3]. In sum, research has shown that a good patient safety culture can contribute to patient outcomes, effectiveness of medical institutions and the well-being of hospital staff [
2].
The definition of safety culture is “the product of individual and group values, attitudes, perceptions, competencies and patterns of behavior that determine the commitment to, and the style and proficiency of, an organization’s health and safety management [
4]”. With increasing awareness of the importance of hospital-wide patient safety culture, tools have been developed to assess staff safety attitudes and inform initiatives to improve patient safety culture in health-providing organizations. Among these tools, the University of Texas Safety Attitudes Questionnaire (SAQ) [
5] is the most widely used internationally and in Taiwan, where we conducted the present study [
6]. The underlying theoretical view of the SAQ recognizes that many medical accidents and adverse incidents are not simply any individual’s errors. The root cause is the latent failures embedded in the organization and system [
7,
8]. Thus, a distinct advantage of the SAQ is its systematic assessment of a multifold of factors related to medical risk and errors, including organizational, work environment, team and staff factors [
8]. In Taiwan, the Joint Commission of Taiwan (JCT), an independent accreditation body for health care institutions, acts as the national leader in patient safety improvements and began its nationwide annual survey using SAQ to chart patient safety culture in all ranges of hospitals, and monitor the long-term change trajectories in the country [
6]. Thus, another advantage for using the SAQ is the availability of database for comparison to position our COVID-19 cohort against its own historic institutional performance. Despite the considerable interest and wide use of the SAQ, a recent review has raised concerns for the quality of measurement tools, level of analysis, and outcome measures [
2]. In the present study, we thus expand the scope to include staff burnout (exhaustion) as a critical indicator of individual well-being (the reverse of strain), which in aggregate contributes to staff turnover at the organizational level [
3,
9].
Burnout is defined as a combination of emotional exhaustion, cognitive weariness and physical fatigue and is clearly related to work stressors and strains [
10]. Emotional exhaustion (or briefly exhaustion), characterized as feelings of energy depletion or exhaustion, is the most important and widely studied dimension in the burnout literature [
11]. Burnout remains a persistent issue affecting healthcare staff worldwide [
3,
12]. Despite the urge to expand the SAQ research to include more outcome measures [
13], very few studies have examined the relation between staff exhaustion and patient safety culture. One study found that staff exhaustion affected the patient safety culture, and it was mainly related to factors at the team level of the work, rather than the individual level [
14]. Evidence is also very limited about the direct impact of staff burnout on patient outcomes. One recent study reported that higher odds of patient mortality, failure to rescue and prolonged length of stay were found in US hospitals that had, on average, higher nurse burnout scores. The same study also noted that good work environments attenuated the relationships between nurse burnout and mortality, failure to rescue and length of stay. The SAQ encompasses dimensions assessing the work environment in terms of job satisfaction, perception of management and work conditions. It is poignant that improving the work environment could help hospitals to simultaneously improve staff well-being and patient outcomes.
During the COVID-19 pandemic, the burden on and challenges to the medical system and personnel has been unprecedented. The uncertainties about the diagnosis and treatment of this unknown emerging disease, unfamiliarity with new tasks due to redeployment and changes in models of care delivery, increasing workload and restrictions on and off work can all cause stress. At the same time, the medical staff must protect themselves from infection and avoid infecting their family members. Research has shown that working in such challenging conditions can hinder the ability of hospital staff to deliver safe and effective care, amplify exhaustion, contributing to poor patient safety [
15]. Although Taiwan has a very low COVID-19 death toll (11 deaths of today, 21 April 2021), heath workers are at greater risk of being exposed to death at close quarters, and may suffer from post-traumatic stress disorder [
16]. Scholars have warned that working in the unprecedented pandemic situations may cause some health care workers to experience moral injuries or mental health problems, such as depression, post-traumatic stress disorder and even suicidal ideation [
16]. A latest systematic review of studies on the impact of COVID-19 on mental health indeed found that health care workers suffered from increased depression/depressive symptoms, anxiety, psychological distress and poor sleep quality [
17]. A recent comparative study in Italy and Spain, the two countries badly hit by the COVID-19, found no cross-country differences of grief during the pandemic [
18]. It is thus imperative to monitor the state of well-being of health care workers, irrespective of the country they are working in, in order to support the frontline soldiers in this long haul fight against the pandemic.
At the beginning of the COVID-19 outbreak, the Taiwanese government swiftly decided to close the border (31 December 2019), execute a strict 14-day quarantine (21 March 2020), make mask wearing mandatory in public and introduce other mass prevention measures. Owing to hard lessons learned from the previous 2003 SARS epidemic, the decisive activation of the national command center (20 January 2020) helped with the diligent cooperation of citizens across the country, Taiwan has been praised as a success model in this pandemic and ranked third internationally for “COVID Resilience” by Bloomberg. At the time of the current study (September-October 2020), Taiwan with the population of 23,561,236, had 552 confirmed cases and 7 deaths. Due to the successful containment of the virus and very low risk community infection, Taiwan has escaped any forms of shutdown and daily life remained the “norm” except for wearing of masks and trace tracking [
19]. The impressive record of success held with no interruption up to the time of writing this paper (19 April 2021), with 1076 confirmed cases and 11 deaths. Taiwan now has just started the vaccination program with 32,389 having the first dose.
Despite the international acclaimed success, medical staff are still under increased pressure to safeguard the nation through this evolving health crisis. Modeled after the National Health Service (NHS) of the UK, Taiwan boasts a world standard high-quality and low-cost national health insurance system (NHIS) that is accessible to every citizen. Historically, Taiwan’s hospitals have never shut down their services even in the height of war time (spring of 1945); except that during 2003’s SARS outbreak, Taiwan learned bitter experiences when several big hospitals collapsed due to serious in-hospital infection. Hence, protection of healthcare workers to secure hospital capacity has become top priority in 2020 COVID-19 pandemic. The central command center maintains steady personal protection equipment supply through national security stockpile program, quickly re-configures hospital workflow and ensures sufficient manpower supply for duty shift. Thus, throughout this pandemic, medical facilities remained operational, while the “COVID prevention mode” is enacted. Using our study organization (Taipei City Hospital, TPECH) as an example, the following changes were made by the hospital group. (1) All people entering the vicinity must wear medical masks at all time; (2) The designated personnel serving at the front door manage the admittance to patients and visitors, with justified reasons only. All entrants must have their temperatures taken and disinfect their hands; (3) If anyone has a fever, he/she must be transferred to the screening station immediately; (4) A screening station is set outside the emergency room. Emergency room staff take turns to man the station; (5) Any patients who have a fever when entering the hospital will be transferred to the fever screening stations for preliminary examination and treatment; (6) Use special passages and separate elevators to transport any suspected and confirmed COVID patients. Disinfect the used paths immediately after transportation; (7) Establish a special negative pressure isolation ward for COVID-19; (8) Assign specialized staff from each unit to care for suspected and confirmed COVID patients. Before entering the ward, the staff must wear a full set of protective clothing. More stringent restrictions were introduced such as a total ban of visitors, when the pandemic escalated intermittently. A way of obtaining valuable insight into the state of patient safety in the current unprecedented crisis situation, is thus to assess the prevailing patient safety culture and staff well-being in the frontline health institutions.
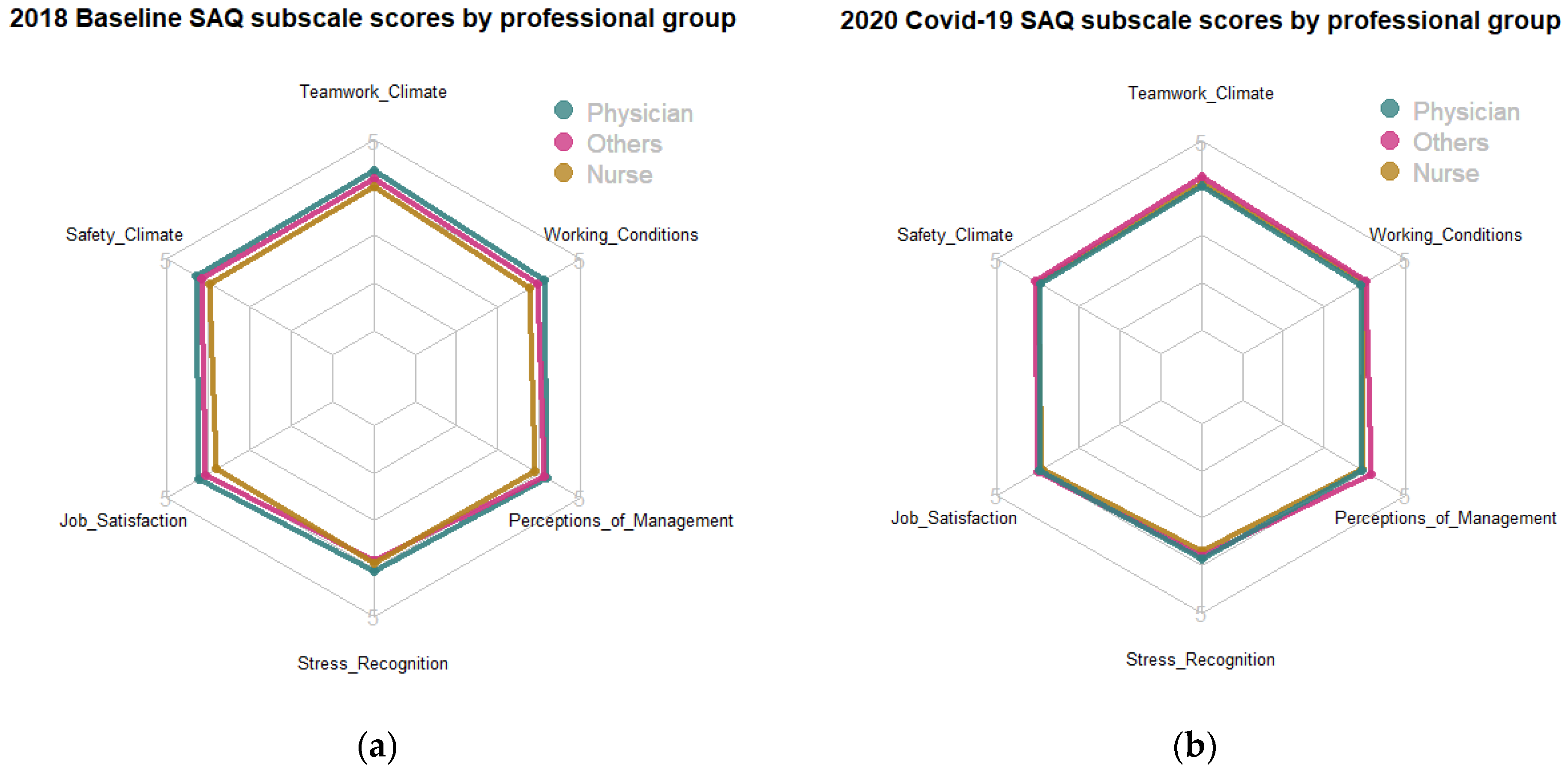
Objective: This study aims to evaluate the patient safety culture and employee well-being of a large hospital group in the capital metropolitan of Taiwan during the COVID-19 pandemic (data collection: September–October 2020). As a pulse survey, we systematically explore personal background factors as predictors of the patient safety culture and well-being. Furthermore, being the first study post-pandemic, we aim to gain insights on the impact of the crisis on both staff patient safety attitudes and well-being by comparing the COVID-19 cohort against the historic data in the same institution.