Current Knowledge, Attitudes, and Practice among Health Care Providers in OSCC Awareness: Systematic Review and Meta-Analysis
Abstract
1. Introduction
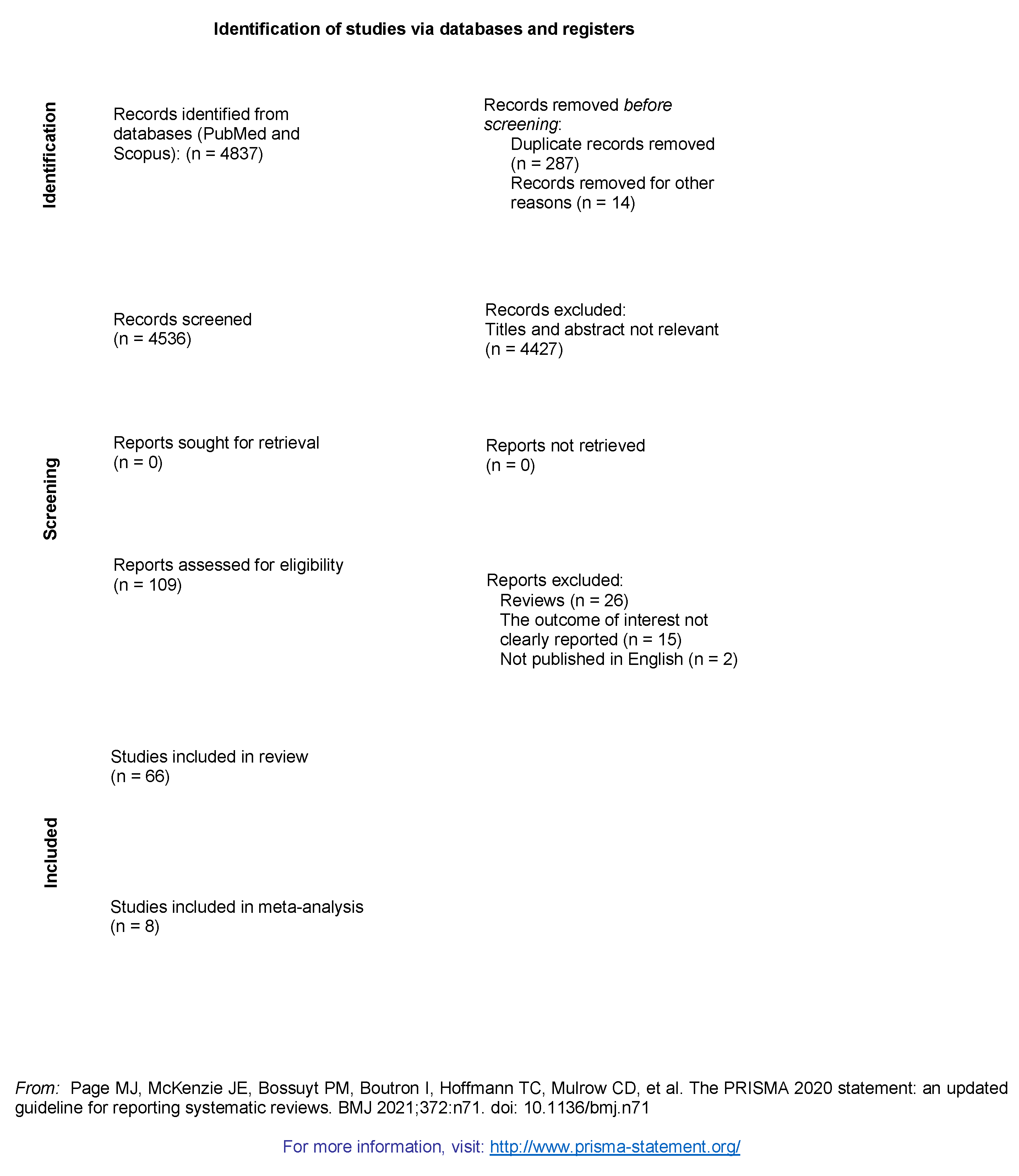
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction and Data Synthesis
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
3.1. Domain 1—Dental Practitioners
3.1.1. Knowledge
3.1.2. Practice
3.1.3. Attitude
3.2. Domain 2—Medical Practitioners
3.2.1. Knowledge
3.2.2. Practice
3.2.3. Attitude
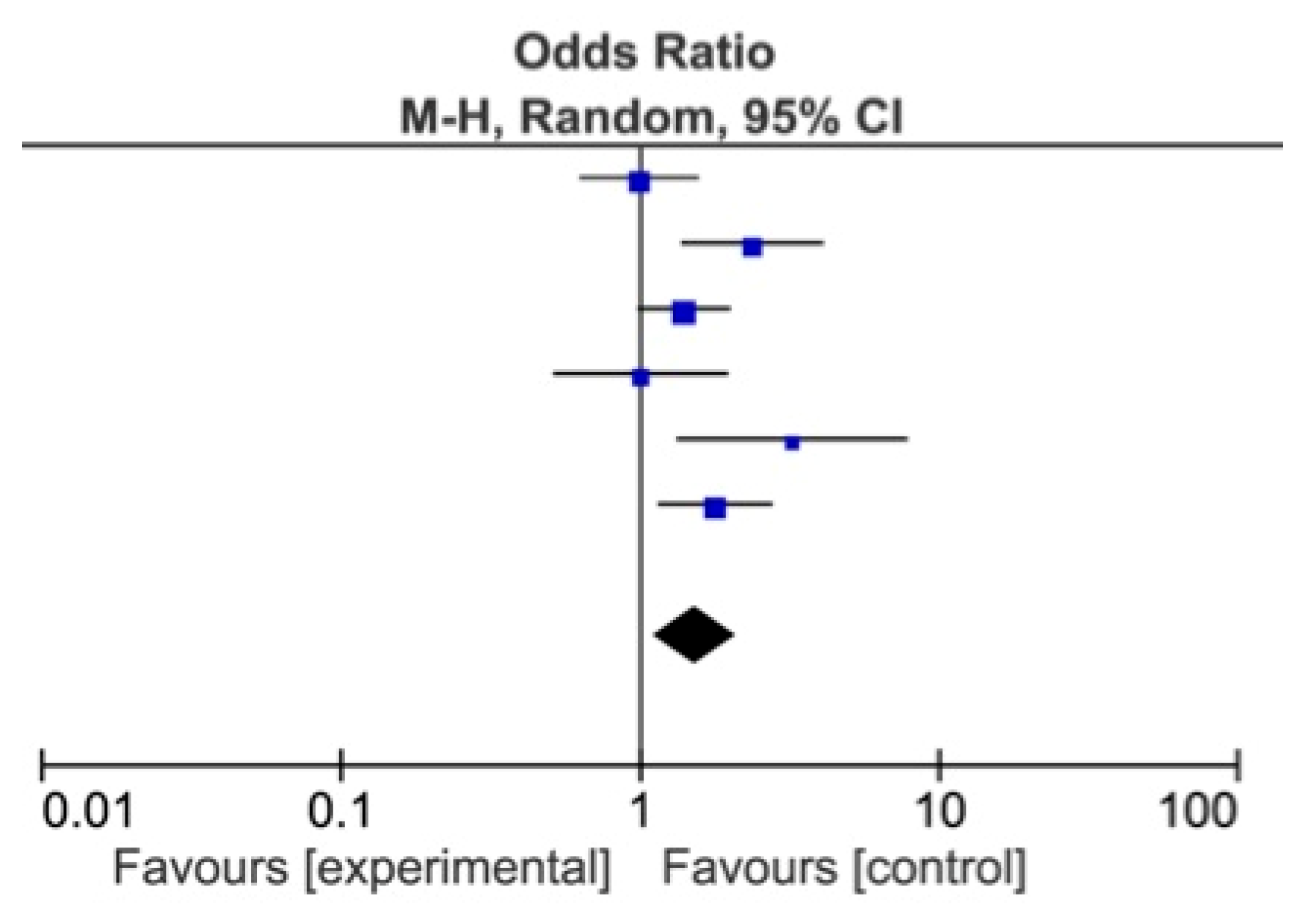
3.3. Meta-Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Globocan 2020. Available online: https://gco.iarc.fr/today/fact-sheets-cancers (accessed on 28 February 2021).
- Gupta, N.; Gupta, R.; Acharya, A.K.; Patthi, B.; Goud, V.; Reddy, S.; Garg, A.; Singla, A. Changing Trends in oral cancer—A global scenario. Nepal J. Epidemiol. 2016, 6, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Joseph, B.K. Oral cancer: Prevention and detection. Med. Princ. Pract. 2002, 11 (Suppl. S1), 32–35. [Google Scholar] [CrossRef]
- Chakraborty, D.; Natarajan, C.; Mukherjee, A. Advances in oral cancer detection. Adv. Clin. Chem. 2019, 91, 181–200. [Google Scholar] [PubMed]
- Petersen, P.E. Oral cancer prevention and control—The approach of the World Health Organization. Oral Oncol. 2009, 45, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Q.A.; Awan, K.H. Role of dental profession in oral cancer prevention and diagnosis. J. Contemp. Dent. Pract. 2016, 17, 963–964. [Google Scholar] [CrossRef]
- Aubertin, M.A. Oral cancer screening in the elderly: The home healthcare nurse’s role. Home Healthc. Nurse 1997, 15, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.B.; Gorsky, M.; Cabay, R.J.; Day, T.; Gonsalves, W. Screening for and diagnosis of oral premalignant lesions and oropharyngeal squamous cell carcinoma: Role of primary care physicians. Can. Fam. Physician 2008, 54, 870–875. [Google Scholar]
- Kaliyaperumal, K. Guideline for conducting a knowledge, attitude and practice (KAP) study. AECS Illum. 2005, 4, 7–9. [Google Scholar]
- Fan, Y.; Zhang, S.; Li, Y.; Li, Y.; Zhang, T.; Liu, W.; Jiang, H. Development and psychometric testing of the Knowledge, Attitudes and Practices (KAP) questionnaire among student Tuberculosis (TB) Patients (STBP-KAPQ) in China. BMC Infect. Dis. 2018, 18, 213. [Google Scholar] [CrossRef]
- Papadiochou, S.; Papadiochos, I.; Perisanidis, C.; Papadogeorgakis, N. Medical practitioners’ educational competence about oral and oropharyngeal carcinoma: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2020, 58, 3–24. [Google Scholar] [CrossRef]
- Rodríguez-Feria, P.; Hernández-Flórez, L.J.; Rodríguez-Feria, D. Knowledge, attitudes and practices of prevention for cervical cancer and breast cancer among medical students. Rev. Salud Publica 2016, 18, 354–366. [Google Scholar] [CrossRef][Green Version]
- Colella, G.; Gaeta, G.M.; Moscariello, A.; Angelillo, I.F. Oral cancer and dentists: Knowledge, attitudes, and practices in Italy. Oral Oncol. 2008, 44, 393–399. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. Standards & Guidelines PRISMA Statement for reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. Ann. Intern. Med. 2009, 151, 65–94. [Google Scholar]
- Methley, A.M.; Campbel, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef]
- Aldossri, M.; Okoronkwo, C.; Dodd, V.; Manson, H.; Singhal, S. Dentists’ Capacity to Mitigate the Burden of Oral Cancers in Ontario, Canada. J. Can. Dent. Assoc. 2020, 86, k2. [Google Scholar] [PubMed]
- Leonel, A.C.L.D.S.; Soares, C.B.R.B.; Lisboa de Castro, J.F.; Bonan, P.R.F.; Ramos-Perez, F.M.M.; Perez, D.E.D.C. Knowledge and Attitudes of Primary Health Care Dentists Regarding Oral Cancer in Brazil. Acta Stomatol. Croat. 2019, 53, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Jboor, D.H.; Al-Darwish, M.S.; Nur, U. Oral Cancer Knowledge, Attitude, and Practice of Dentists in the State of Qatar. Dent. J. 2019, 7, 43. [Google Scholar] [CrossRef]
- Nazar, H.; Shyama, M.; Ariga, J.; El-Salhy, M.; Soparkar, P.; Alsumait, A. Oral Cancer Knowledge, Attitudes and Practices among Primary Oral Health Care Dentists in Kuwait. Asian Pac. J. Cancer Prev. 2019, 20, 1531–1536. [Google Scholar] [CrossRef] [PubMed]
- Khattab, N.M.A.; Elheeny, A.A.H.; Tony, G.A. Oral-cancer knowledge, practice, and attitude assessment of dentists in Upper Egypt: A cross-sectional study. Clin. Exp. Dent. Res. 2019, 5, 121–127. [Google Scholar] [CrossRef]
- Pavão Spaulonci, G.; Salgado de Souza, R.; Gallego Arias Pecorari, V.; Lauria Dib, L. Oral Cancer Knowledge Assessment: Newly Graduated versus Senior Dental Clinicians. Int. J. Dent. 2018, 2018, 9368918. [Google Scholar] [CrossRef] [PubMed]
- Hashim, R.; Abo-Fanas, A.; Al-Tak, A.; Al-Kadri, A.; Abu Ebaid, Y. Early Detection of Oral Cancer- Dentists’ Knowledge and Practices in the United Arab Emirates. Asian Pac. J. Cancer Prev. 2018, 19, 2351–2355. [Google Scholar] [PubMed]
- Kogi, S.; DaSilva, J.; Mikasa, Y.; Lee, C.; Ishikawa-Nagai, S.; Yang, Q.; Kihara, H.; Abe, R.; Yamada, H. Knowledge and Practice of Oral Cancer Screening in Teaching Faculty-Comparison of Specialty and Year of Clinical Experience. J. Cancer Educ. 2019, 34, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.H.M.; Naidoo, S. Oral Cancer Knowledge, Attitudes, and Practices among Dentists in Khartoum State, Sudan. J. Cancer Educ. 2019, 34, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Mariño, R.; Haresaku, S.; McGrath, R.; Bailey, D.; Mccullough, M.; Musolino, R.; Kim, B.; Chinnassamy, A.; Morgan, M. Oral cancer screening practices of oral health professionals in Australia. BMC Oral Health 2017, 17, 151. [Google Scholar] [CrossRef] [PubMed]
- Kebabcıoğlu, Ö.; Pekiner, F.N. Assessing Oral Cancer Awareness Among Dentists. J. Cancer Educ. 2018, 33, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Haresaku, S.; Makino, M.; Sugiyama, S.; Naito, T.; Mariño, R.J. Comparison of Practices, Knowledge, Confidence, and Attitude toward Oral Cancer among Oral Health Professionals between Japan and Australia. J. Cancer Educ. 2018, 33, 429–435. [Google Scholar] [CrossRef]
- Navabi, N.; Hashemipour, M.A.; Roughani, A. Validation of a Persian Short-Form Version of a Standardised Questionnaire Assessing Oral Cancer Knowledge, Practice and Attitudes Among Dentists. Sultan Qaboos Univ. Med. J. 2017, 17, e80–e87. [Google Scholar] [CrossRef]
- Akbari, N.; Raeesi, V.; Khazaei, T.; Ramezanzadeh, K.; Ebrahimipour, S. Evaluation of General Dentists’ and Dental Specialists’ Knowledge about Oral Cancer in South Khorasan-Iran 2014. Asian Pac. J. Cancer Prev. 2015, 16, 6987–6990. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.; Farah, C.S. Screening and referral of oral mucosal pathology: A check-up of Australian dentists. Aust. Dent. J. 2015, 60, 52–58. [Google Scholar] [CrossRef]
- Anandani, C.; Metgud, R.; Ramesh, G.; Singh, K. Awareness of General Dental Practitioners about Oral Screening and Biopsy Procedures in Udaipur, India. Oral Health Prev. Dent. 2015, 13, 523–530. [Google Scholar] [PubMed]
- Alaizari, N.A.; Al-Maweri, S.A. Oral cancer: Knowledge, practices and opinions of dentists in yemen. Asian Pac. J. Cancer Prev. 2014, 15, 5627–5631. [Google Scholar] [CrossRef]
- Mehdizadeh, M.; Seyed Majidi, M.; Sadeghi, S.; Hamzeh, M. Evaluation of knowledge, attitude and practice of general dentists regarding oral cancer in sari, iran. Iran. J. Cancer Prev. 2014, 7, 101–104. [Google Scholar]
- Saleh, A.; Kong, Y.H.; Vengu, N.; Badrudeen, H.; Zain, R.B.; Cheong, S.C. Dentists’ perception of the role they play in early detection of oral cancer. Asian Pac. J. Cancer Prev. 2014, 15, 229–237. [Google Scholar] [CrossRef]
- Ramaswamy, P.; Uday, G.; Sreenivasulu, P.; Kumar, B.P.; Khaitan, T.; Geethika, V.R. Awareness about oral cancer among dental postgraduate students in the State of Andhra Pradesh, India. J. Cancer Educ. 2014, 29, 665–668. [Google Scholar] [CrossRef]
- Razavi, S.M.; Zolfaghari, B.; Foroohandeh, M.; Doost, M.E.; Tahani, B. Dentists’ knowledge, attitude, and practice regarding oral cancer in Iran. J. Cancer Educ. 2013, 28, 335–341. [Google Scholar] [CrossRef]
- Pentenero, M.; Chiecchio, A.; Gandolfo, S. Impact of academic and continuing education on oral cancer knowledge, attitude and practice among dentists in north-western Italy. J. Cancer Educ. 2014, 29, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Rocha-Buelvas, A.; Hidalgo-Patiño, C.; Collela, G.; Angelillo, I. Oral cancer and dentists: Knowledge, attitudes and practices in a South Colombian context. Acta Odontol. Latinoam. 2012, 25, 155–162. [Google Scholar] [PubMed]
- Joseph, B.K.; Sundaram, D.B.; Sharma, P. Oral cancer awareness among dentists in Kuwait. Med. Princ. Pract. 2012, 21, 164–170. [Google Scholar] [CrossRef]
- Vijay Kumar, K.V.; Suresan, V. Knowledge, attitude and screening practices of general dentists concerning oral cancer in Bangalore city. Indian J. Cancer 2012, 49, 33–38. [Google Scholar] [PubMed]
- Seoane, J.; Varela-Centelles, P.; Tomás, I.; Seoane-Romero, J.; Diz, P.; Takkouche, B. Continuing education in oral cancer prevention for dentists in Spain. J. Dent. Educ. 2012, 76, 1234–1240. [Google Scholar] [CrossRef]
- Maybury, C.; Horowitz, A.M.; Yan, A.F.; Green, K.M.; Wang, M.Q. Maryland dentists’ knowledge of oral cancer prevention and early detection. J. Calif. Dent. Assoc. 2012, 40, 341–350. [Google Scholar] [PubMed]
- Hertrampf, K.; Wenz, H.J.; Koller, M.; Grund, S.; Wiltfang, J. Early detection of oral cancer: Dentists’ opinions and practices before and after educational interventions in Northern-Germany. J. Craniomaxillofac. Surg. 2013, 4, e201–e207. [Google Scholar] [CrossRef] [PubMed]
- Decuseara, G.; MacCarthy, D.; Menezes, G. Oral cancer: Knowledge, practices and opinions of dentists in Ireland. J. Ir. Dent. Assoc. 2011, 57, 209–214. [Google Scholar] [PubMed]
- Hertrampf, K.; Wiltfang, J.; Koller, M.; Klosa, K.; Wenz, H.J. Dentists’ perspectives on oral cancer: A survey in Northern Germany and a comparison with international data. Eur. J. Cancer Prev. 2010, 19, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Klosa, K.; Wiltfang, J.; Wenz, H.J.; Koller, M.; Hertrampf, K. Dentists’ opinions and practices in oral cancer prevention and early detection in Northern Germany. Eur. J. Cancer Prev. 2011, 20, 313–319. [Google Scholar] [CrossRef]
- López-Jornet, P.; Camacho-Alonso, F.; Molina-Miñano, F. Knowledge and attitudes about oral cancer among dentists in Spain. J. Eval. Clin. Pract. 2010, 16, 129–133. [Google Scholar] [CrossRef]
- Seoane-Lestón, J.; Velo-Noya, J.; Warnakulasuriya, S.; Varela-Centelles, P.; Gonzalez-Mosquera, A.; Villa-Vigil, M.A.; Rodríguez-Lozano, F.; Diz-Dios, P. Knowledge of oral cancer and preventive attitudes of Spanish dentists. Primary effects of a pilot educational intervention. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e422–e426. [Google Scholar] [CrossRef]
- Mahalaha, S.A.; Cheruvu, V.K.; Smyth, K.A. Oral cancer screening: Practices, knowledge, and opinions of dentists working in Ohio nursing homes. Spec. Care Dent. 2009, 29, 237–243. [Google Scholar] [CrossRef]
- LeHew, C.W.; Kaste, L.M. Oral cancer prevention and early detection knowledge and practices of Illinois dentists—A brief communication. J. Public Health Dent. 2007, 67, 89–93. [Google Scholar] [CrossRef]
- Gajendra, S.; Cruz, G.D.; Kumar, J.V. Oral cancer prevention and early detection: Knowledge, practices, and opinions of oral health care providers in New York State. J. Cancer Educ. 2006, 21, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Kujan, O.; Duxbury, A.J.; Glenny, A.M.; Thakker, N.S.; Sloan, P. Opinions and attitudes of the UK’s GDPs and specialists in oral surgery, oral medicine and surgical dentistry on oral cancer screening. Oral Dis. 2006, 12, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Seoane, J.; Warnakulasuriya, S.; Varela-Centelles, P.; Esparza, G.; Dios, P.D. Oral cancer: Experiences and diagnostic abilities elicited by dentists in North-western Spain. Oral Dis. 2006, 12, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Patton, L.L.; Elter, J.R.; Southerland, J.H.; Strauss, R.P. Knowledge of oral cancer risk factors and diagnostic concepts among North Carolina dentists. Implications for diagnosis and referral. J. Am. Dent. Assoc. 2005, 136, 602–682. [Google Scholar] [CrossRef] [PubMed]
- Cruz, G.D.; Ostroff, J.S.; Kumar, J.V.; Gajendra, S. Preventing and detecting oral cancer. Oral health care providers’ readiness to provide health behavior counseling and oral cancer examinations. J. Am. Dent. Assoc. 2005, 136, 594–682. [Google Scholar] [CrossRef]
- Alonge, O.K.; Narendran, S. Oral cancer knowledge and practices of dentists along the Texas-Mexico border. J. Cancer Educ. 2004, 19, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Clovis, J.B.; Horowitz, A.M.; Poel, D.H. Oral and pharyngeal cancer: Knowledge and opinions of dentists in British Columbia and Nova Scotia. J. Can. Dent. Assoc. 2002, 68, 415–420. [Google Scholar]
- Clovis, J.B.; Horowitz, A.M.; Poel, D.H. Oral and pharyngeal cancer: Practices and opinions of dentists in British Columbia and Nova Scotia. J. Can. Dent. Assoc. 2002, 68, 421–425. [Google Scholar]
- Canto, M.T.; Drury, T.F.; Horowitz, A.M. Maryland dentists’ knowledge of oral cancer risk factors and diagnostic procedures. Health Promot. Pract. 2001, 2, 255–262. [Google Scholar] [CrossRef]
- Yellowitz, J.A.; Horowitz, A.M.; Drury, T.F.; Goodman, H.S. Survey of U.S. dentists’ knowledge and opinions about oral pharyngeal cancer. J. Am. Dent. Assoc. 2000, 131, 653–661. [Google Scholar] [CrossRef]
- Horowitz, A.M.; Drury, T.F.; Goodman, H.S.; Yellowitz, J.A. Oral pharyngeal cancer prevention and early detection. Dentists’ opinions and practices. J. Am. Dent. Assoc. 2000, 131, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, A.M.; Drury, T.F.; Canto, M.T. Practices of Maryland dentists: Oral cancer prevention and early detection—Baseline data from 1995. Oral Dis. 2000, 6, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, K.A.; Johnson, N.W. Dentists and oral cancer prevention in the UK: Opinions, attitudes and practices to screening for mucosal lesions and to counselling patients on tobacco and alcohol use: Baseline data from 1991. Oral Dis. 1999, 5, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Yellowitz, J.; Horowitz, A.M.; Goodman, H.S.; Canto, M.T.; Farooq, N.S. Knowledge, opinions and practices of general dentists regarding oral cancer: A pilot survey. J. Am. Dent. Assoc. 1998, 129, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, D.; Healy, C.M. Oral Cancer Awareness of Non-Consultant Hospital Doctors in Irish Hospitals. Ir. Med. J. 2018, 111, 667. [Google Scholar]
- Shimpi, N.; Bharatkumar, A.; Jethwani, M.; Chyou, P.H.; Glurich, I.; Blamer, J.; Acharya, A. Knowledgeability, Attitude and Behavior of Primary Care Providers Towards Oral Cancer: A Pilot Study. J. Cancer Educ. 2018, 33, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Hertrampf, K.; Wenz, H.J.; Koller, M.; Ambrosch, P.; Arpe, N.; Wiltfang, J. Knowledge of diagnostic and risk factors in oral cancer: Results from a large-scale survey among non-dental healthcare providers in Northern Germany. J. Craniomaxillofac. Surg. 2014, 42, 1160–1165. [Google Scholar] [CrossRef]
- Tanriover, O.; Hidiroglu, S.; Save, D.; Akan, H.; Ay, P.; Karavus, M.; Hayran, O. Knowledge of oral cancer, preventive attitudes, and behaviors of primary care physicians in Turkey. Eur. J. Cancer Prev. 2014, 23, 464–468. [Google Scholar] [CrossRef]
- Ni Riordain, R.; McCreary, C. Oral cancer—Current knowledge, practices and implications for training among an Irish general medical practitioner cohort. Oral Oncol. 2009, 45, 958–962. [Google Scholar] [CrossRef]
- LeHew, C.W.; Epstein, J.B.; Koerber, A.; Kaste, L.M. Training in the primary prevention and early detection of oral cancer: Pilot study of its impact on clinicians’ perceptions and intentions. Ear Nose Throat J. 2009, 88, 748–753. [Google Scholar] [CrossRef]
- Nicotera, G.; Di Stasio, S.M.; Angelillo, I.F. Knowledge and behaviors of primary care physicians on oral cancer in Italy. Oral Oncol. 2004, 40, 490–495. [Google Scholar] [CrossRef]
- Canto, M.T.; Horowitz, A.M.; Drury, T.F.; Goodman, H.S. Maryland family physicians’ knowledge, opinions and practices about oral cancer. Oral Oncol. 2002, 38, 416–424. [Google Scholar] [CrossRef]
- Hassona, Y.; Sawair, F.; Baqain, Z.; Maayta, W.; Shahin, A.; Scully, C. Oral Cancer Early Detection—A Pressing Need for Continuing Education in Jordan. Asian Pac. J. Cancer Prev. 2015, 16, 7727–7730. [Google Scholar] [CrossRef] [PubMed]
- Alami, A.Y.; El Sabbagh, R.F.; Hamdan, A. Knowledge of oral cancer among recently graduated medical and dental professionals in Amman, Jordan. J. Dent. Educ. 2013, 77, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Borhan-Mojabi, K.; Moradi, A.; Yazdabadi, A. Evaluating the degree of knowledge on oral cancer among general practitioners and dentists in Qazvin. J. Eval. Clin. Pract. 2012, 18, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Reed, S.G.; Cartmell, K.B.; Duffy, N.G.; Wahlquist, A.E.; Sinha, D.; Hollinger, A.; Bode, A.; Alberg, A.J.; Day, T.A. Oral cancer preventive practices of South Carolina dentists and physicians. J. Cancer Educ. 2010, 25, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, E.; Ruhlen, T.N.; Kronenberg, F.R.; Hayes, C.; Peters, E.S. Oral cancer knowledge, attitudes and practices: A survey of dentists and primary care physicians in Massachusetts. J. Am. Dent. Assoc. 2009, 140, 461–467. [Google Scholar] [CrossRef]
- Macpherson, L.M.; McCann, M.F.; Gibson, J.; Binnie, V.I.; Stephen, K.W. The role of primary healthcare professionals in oral cancer prevention and detection. Br. Dent. J. 2003, 195, 277–281. [Google Scholar] [CrossRef]
- Greenwood, M.; Lowry, R.J. Primary care clinicians’ knowledge of oral cancer: A study of dentists and doctors in the North East of England. Br. Dent. J. 2001, 191, 510–512. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yellowitz, J.A.; Goodman, H.S. Assessing physicians’ and dentists’ oral cancer knowledge, opinions and practices. J. Am. Dent. Assoc. 1995, 126, 53–60. [Google Scholar] [CrossRef]
- Khankeh, H.; Ranjbar, M.; Khorasani-Zavareh, D.; Zargham-Boroujeni, A.; Johansson, E. Challenges in conducting qualitative research in health: A conceptual paper. Iran. J. Nurs. Midwifery Res. 2015, 20, 635–641. [Google Scholar]
- Fatima, N.; Mohiuddin, S.; Hosein, S.; Mervyn, M. Socio-Economic Implications Of A Younger Aged Female Predilection In Malignant Transformation Of Oral Sub Mucous Fibrosis. J. Ayub Med. Coll. Abbottabad 2019, 31, 16–20. [Google Scholar]
- Sarode, S.C.; Sarode, G.S.; Tupkari, J.V. Oral potentially malignant disorders: A proposal for terminology and definition with review of literature. J. Oral Maxillofac. Pathol. 2014, 18 (Suppl. S1), S77–S80. [Google Scholar] [CrossRef]
- Dhanuthai, K.; Rojanawatsirivej, S.; Thosaporn, W.; Kintarak, S.; Subarnbhesaj, A.; Darling, M.; Kryshtalskyj, E.; Chiang, C.P.; Shin, H.I.; Choi, S.Y.; et al. Oral cancer: A multicenter study. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e23–e29. [Google Scholar] [CrossRef]
- Speight, P.M.; Epstein, J.; Kujan, O.; Lingen, M.W.; Nagao, T.; Ranganathan, K.; Vargas, P. Screening for oral cancer-a perspective from the Global Oral Cancer Forum. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 680–687. [Google Scholar] [CrossRef] [PubMed]
- James, K.; Toner, M.; Stassen, L.F. Performing mucosal tissue biopsies in general dental practice. J. Ir. Dent. Assoc. 2011, 57, 203–208. [Google Scholar]
- Cornuz, J. Smoking cessation interventions in clinical practice. Eur. J. Vasc. Endovasc. Surg. 2007, 34, 397–404. [Google Scholar] [CrossRef]
- Grafton-Clarke, C.; Chen, K.W.; Wilcock, J. Diagnosis and referral delays in primary care for oral squamous cell cancer: A systematic review. Br. J. Gen. Pract. 2019, 69, e112–e126. [Google Scholar] [CrossRef] [PubMed]
- Leuci, S.; Amato, M.; Calabria, E.; Spagnuolo, G.; Masucci, M.; Davide, M.M. Screening Projects for Oral Carcinoma in Relation to Health Education and Patients’ Compliance: Study on 600 Participants. J. Int. Soc. Prev. Community Dent. 2017, 7, S163–S169. [Google Scholar] [CrossRef] [PubMed]
- Leuci, S.; Aria, M.; Nicolò, M.; Spagnuolo, G.; Warnakulasuriya, K.; Mignogna, M.D. Comparison of views on the need for continuing education on oral cancer between general dentists and oral medicine experts: A Delphi survey. J. Int. Soc. Prev. Community Dent. 2016, 6, 465–473. [Google Scholar] [CrossRef]


| Criteria | Inclusion | Exclusion | ||
|---|---|---|---|---|
| Language | Non-English | |||
| S | P | Sample | HCPs involved in OSCC/OPC management | Non-HCPs |
| PI | Phenomenon of interest | OSCC topics | Non-OSCC topics | |
| I | Intervention | Questionnaire-based survey and interview assessing knowledge OR/AND attitude OR/AND practice (See Table 2) | Non-questionnaire-based survey | |
| D | Design of study | Cross-sectional studies/comparative cross-sectional studies/RCTs, non-RCTs | Reviews, opinion-based studies, letter to editors, case reports, study protocols | |
| C | Comparison | Comparison of KAP among different HCPs when available | - | |
| E | O | Evaluation (E) (O) | HCPs’ knowledge status/skills/attitudes/perceptions/views/opinions/practices/behaviors | Unrelated with HCPs’ knowledge status/skills/attitudes/perceptions/views/opinions/practices/behaviors |
| R | Research type (R) | Qualitative studies, quantitative studies, and mixed-method studies | - | |
| Geographical area of interest | Worldwide | - | ||
| Study focus | Studies investigating the knowledge AND/OR attitudes AND/OR practices/behaviors of HCPs towards oral health topics Studies investigating almost two among knowledge, attitude, and practice Studies investigating the impact of OSCC/OPC educational interventions on HCPs’ knowledge AND/OR attitudes Studies focusing only on data about single categories of HCPs | Studies investigating the OC/OPC knowledge AND/OR attitudes AND/OR practices of medical/dental students Studies investigating the knowledge AND/OR attitudes AND/OR practices of HCPs towards other oral health related topics Studies with inadequate data Studies focusing on aggregated data per individual categories of HCPs |
| Knowledge |
| 1. Risk factors |
| Tobacco |
| Alcohol |
| Prior OSCC |
| Advanced age |
| HPV infection |
| Sun exposure |
| Diet |
| Betel quid chewing |
| Fungal infection |
| Immunosuppression |
| Radiotherapy |
| 2. Non-risk factors |
| Family history |
| Familiar clustering |
| Ill-fitting prothesis |
| Hot food and drink |
| Poor oral hygiene |
| Use of spicy food |
| Obesity |
| 3. OPMDs |
| Leukoplakia |
| Erythroplakia |
| Lichenoid lesions |
| Chronic hyperplastic candidiasis |
| Actinic cheilitis |
| Oral sub-mucous fibrosis |
| 4. Common sites of development |
| Lip |
| Tongue |
| Floor of the mouth |
| Buccal mucosa |
| Palate |
| Gum |
| 5. Clinical presentation |
| OSCC is the most common form of oral cancer |
| OSCC is asymptomatic at early stage |
| OSCC is diagnosticated more frequently at advanced stage |
| Lymph node characteristic of OSCC metastasis |
| Early OSCC lesions appear as small, painless red area |
| Ventral lateral border of the tongue most likely to develop OSCC |
| Submandibular lymph nodes are the first places of metastasis of OSCC |
| Lung is the most common site of distant metastasis of OSCC |
| Persistent ulcer, lump, non-healing socket, and/or bleeding gums could be signs of OSCC |
| Dysphagia |
| Limited tongue mobility |
| Attitude |
| Adequate/inadequate OSCC education received at medical/dental school |
| Quality of OSCC education |
| Up-to-date knowledge |
| Need to perform annual OSCC screening examinations for patients > 40 years old |
| Early detection improves 5-year survival rate |
| Training level in providing education on smoking cessation |
| Training level in OSCCC examination/screening |
| Believe/do not believe dentist/physician/dental hygienist is qualified to perform OSCC examination |
| Comfortable/uncomfortable during neck lymph nodes palpation |
| Comfortable/uncomfortable to refer suspicious oral lesions to specialists |
| Confident/non-confident in diagnosis of OSCC from clinical appearance |
| Patients’ knowledge level about risk factors |
| Should/should not inform patients about findings |
| Comfortable/uncomfortable to perform biopsy |
| Advise/do not advise patients with suspicious oral lesions |
| Need of continuous education in the future |
| Adequate/inadequate preparation to explain the risks of tobacco/alcohol use |
| Practice |
| Extra/intraoral examination |
| Lymph nodes palpation |
| Biopsy |
| Use of blue toluidine/fluorescent light |
| Asking about current/previous use of tobacco |
| Asking about the type and amounts of tobacco products used |
| Asking about current/previous use of alcohol |
| Asking about the type and amounts of alcohol use |
| Asking about personal/family history of cancer |
| Asking about type of diet |
| Asking about sun exposure |
| Refer to a specialist (as oral and maxillofacial surgeons, oral medicine specialists, ENT, physicians, specialized hospital) |
| Knowledge | Attitude | Practice | |||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Participants | Quality Assessment | Risk Factors | Precancerous Lesions | Clinical Picture | Common Sites of Development | Opinion | History Taking | Physical Examination |
| Aldossri et al., 2020 [17] | 932 | >75% | Tobacco 99.5% Alcohol 97.2% Prior OSCC 98.6% HPV 88.2% Elderly 69.6% Diet 31.8% | N.A. | Ulcer 99.7% Red patch 98.6% White patch 98.6% Dysphagia 93.9% Paraesthesia 96% Airway obstruction 89.3% Oral bleeding 86.6% Pain 85.1% Trismus 65.5% Chronic earache 58.1% | N.A. | Visual examination is effective in early detection 97.9% Skills in neck examination 96.1% Up-to-date personal knowledge 92.4% Skills in auxiliary devices 83.2% Skills in RX 76.5% Smoking cessation is effective 39.6% Biopsy is mandatory 35.4% Advice HPV vaccine 29.5% Alcohol cessation is effective 22.3% | N.A. | N.A. |
| da Silva Leonel et al., 2019 [18] | 71 | <75% | Tobacco 100% Alcohol 98.6% Sun exposure 97.2% Family history 95.8% Elderly 93% Ill-fitting prothesis 88.7% Emotional stress 78.9% Poor oral hygiene 78.9% Presence of decay teeth 74.6% Diet 59.2% Oral sex 50.7% Hot food and drink 46.5% Drug abuse 21.1% | Leukoplakia 85.9% Candidiasis 5.6% Stomatitis 4.2% Blistering 1.4% | OSCC diagnosis (III/IV stage) 76.1% OSCC 66.2% | Tongue and floor of the mouth 71.9% Buccal mucosa 11.2% Palate 4.2% Gingival 2.8% | Key role of dentist 98.6% Need of CE 95.8% Lack of patients’ knowledge 84.5% Adequate knowledge 66.2% Previous CE courses 49.3% Undergraduate training was adequate 43.7% Diagnostic procedure experience 26.8% | N.A. | Intra- and extraoral 98.6% |
| Jboor et al., 2019 [19] | 177 | >75% | Tobacco 97.4% Prior OSCC 94.3% Alcohol 93.2% HPV 85.3% Betel quid chewing 74.5% Elderly 72.8% Sun exposure 63.3% Gutka use 49.1% Diet 28.2% | Erythroplakia & Leukoplakia 53.7% | OSCC 84.2% Positive lymph node 75.7% Red patch 66.7% Tongue high-risk area 46.3% OSCC diagnosis (III/IV stage) 39% OSCC time diagnosis > 60 years 31.6% Asymptomatic at early stage 21.5% | Tongue 77.9% Floor of the mouth 54.2% | Smoking cessation is effective 90% Up-to-date personal knowledge 66.7% Visual examination is effective in early detection 48.6% | Tobacco 92.6% Prior OSCC 86.8% Family history 80.6% Tobacco products 80% Alcohol products 46.8% Alcohol 66.3% | N.A. |
| Nazar et al., 2019 [20] | 289 | >75% | Tobacco 99.7% Alcohol 99.7% | Erythroplakia and Leukoplakia 97.9% | OSCC 80.6% Positive lymph node 74.3% Asymptomatic at early stage 31.3% | Tongue and Floor of the mouth 80.3% | Need of CE 92.4% Up-to-date personal knowledge 55% Visual examination is effective in early detection 38% | Tobacco 62% Alcohol 17% | Intra- and extraoral 50% |
| Khattab et al., 2018 [21] | 400 | <75% | N.A. | N.A. | N.A. | N.A. | N.A. | N.A. | Intra- and extraoral 37.5% Lymph nodes 26.5% Biopsy 27.5% |
| Pavão Spaulonci et al., 2018 [22] | Senior GDPs 105; junior GDPs 84 | >75% | Junior: Tobacco 100%/Alcohol 96.4%/Family history 95.2%/Sun exposure 90.5%/HPV 84.5% Other malignancies 83.3%/Ill-fitting prothesis 60.7%/Emotional stress 56%/Oral sex 51.2%/Presence of decay teeth 44%/Hot food and drink 40.5%/Poor oral hygiene 40.5%/Drug abuse 34.5%/Diet 31%/Spicy food 23.8%/Obesity 16.7% Senior: Tobacco 100%/Alcohol 100%/Family history 95.2%/Ill-fitting prothesis 93.3%/HPV 92.4%/Sun exposure 81.9% Other malignancies 79%/Presence of decay teeth 76.2%/Hot food and drink 74.3%/Emotional stress 67.6%/Poor oral hygiene 64.8%/Oral sex 59%/Diet 47.6%/Spicy food 34.3%/Drug abuse 28.6%/Obesity 16.2% | Junior: Leukoplakia 73.8% Senior: Leukoplakia 75.2% | Junior: Ulcer 85.7% Positive lymph node 69% OSCC 67.9% Junior: Ulcer 85.7% Positive lymph node 69.5% OSCC 64.8% | Junior Tongue 59.5% Senior Tongue 50.5% | Junior Previous CE courses 48.8% Undergraduate training was adequate 70.2% Up-to-date personal knowledge 54.8% Junior Previous CE courses 31.4% Undergraduate training was adequate 43.8% Up-to-date personal knowledge 51.4% | N.A. | Junior Intra- and extraoral examination at 1st visit 78.6% Senior Intra- and extraoral examination at 1st visit 85.7% |
| Hashim et al., 2018 [23] | 298 | >75% | Tobacco 99% Prior OSCC 92.3% Alcohol 87.30% HPV 76.6% Sun exposure 73.2% Elderly 60.9% Diet 43.8% | Leukoplakia 28.4% Candidiasis 19.1% Actinic cheilitis 18.6% Erythroplakia 7.7% OLP 5.7% | Ulcer 87.6% Positive lymph node 82.9% White patch 79.9% Dysphagia and limited tongue mobility 68.9% Lump 66.9% Red patch 63.2% Non-healing socket 35.1% | Tongue 30.1% Floor of the mouth 18.7% Palate 7% | Need of CE 84.9% Previous CE courses 48% Visual examination is effective in early detection 31.14% Biopsy is mandatory 9.9% | N.A. | Scalpel biopsy 40% Brush biopsy 20.4% Toluidine blue 6% Fluorescent imaging 5.7% Exfoliative cytology 5% |
| Kogi et al., 2018 [24] | 110 | Other malignancies 52.7% Tobacco 41.8% Elderly 21.8% HPV 18.2% Alcohol 13.6% Diet 10.9% | N.A. | N.A. | N.A. | Need of CE 86.4% Up-to-date personal knowledge 3.6% | N.A. | Intra- and extraoral examination at 1st visit 43.6%; at recall 32.7% | |
| Ahmed et al., 2017 [25] | 130 | >75% | Family history 64.6% Comorbidities 60% HPV 60% Elderly 58.4% Ill-fitting prothesis 41.6% Tobacco 38.9% Alcohol 38.9% Diet 29.2% | N.A. | OSCC 90% Ulcer 83.2% Red patch 80.5% White patch 80.5% Swelling 43.4% Pain 13% | Lips 22.1% Tongue 20.4% Floor of the mouth 19.5% | Need of CE 95.6% Need of referral guidelines 88.5% Visual examination is effective in early detection 46% Adequate knowledge 64.7% Undergraduate training was adequate 27.4% Up-to-date personal knowledge 26.7% | N.A. | Lymph nodes 57% Intraoral 51% Extraoral 40.8% Biopsy 26.5% RX 20.4% |
| Mariño et al., 2017 [26] | 241 | >75% | Tobacco 99.4% Betel quid chewing 98.2% Prior OSCC 97% Alcohol 94.6% | N.A. | N.A. | N.A. | Visual examination is effective in early detection 95.2% | N.A. | Intraoral 99.7% Oropharynx 92.3% Extraoral 83.8% Lymph nodes 80.7% |
| Kebabcıoğlu et al., 2017 [27] | 170 | >75% | Tobacco 98.8% Prior OSCC 95.3% Alcohol 91.2% HPV 90% Sun exposure 86.5% Betel quid chewing 80.6% Elderly 56.5% Diet 52.4% | Erythroplakia and leukoplakia 64.1% | OSCC 64.7% White patch 35.9% Red patch 26.5% OSCC time diagnosis >60 yrs 12.9% | Tongue and floor of the mouth 37.1% Palate and floor of mouth 11.2% Palate 2.4% | Lack of patients’ knowledge 85.9% Skills in neck examination 70% Visual examination is effective in early detection 53% | N.A. | N.A. |
| Haresaku et al., 2016 [28] | Japanese 137; Australian 259 | >75% | Japanese: Tobacco 90% Family history 74% Alcohol 52% HPV 38% Betel quid chewing 25% Caffeine 15% Australian: Betel quid chewing 98% Tobacco 98% Alcohol 94% HPV 93% Family history 75% Caffeine 5% | N.A. | N.A. | N.A. | Japanese Need of CE > 90% Visual examination is effective in early detection 76.8 % | N.A. | Japanese Intraoral 89.3% Extraoral 35.7% Lymph nodes 10.7% Oropharynx 10.7% Australian Intraoral 98.4% Extraoral 80.5% Lymph nodes 50.8% Oropharynx 23.8% |
| Navabi et al., 2016 [29] | 313 | >75% | Alcohol 26.3% Tobacco 26.3% | N.A. | OSCC 66.7% OSCC time diagnosis >60 yrs 66.7% Positive lymph node 48.6% | Tongue and lips 26.7% | Ease for referral 92.7% Undergraduate training was adequate 41.3% Visual examination is effective in early detection 28% Smoking cessation is effective 27.9% Up-to-date personal knowledge 26.7% Dentist skills in visual inspection 20.2% Physician skills in visual inspection 13.4% | Tobacco 87.2% Tobacco products 76.5% Alcohol 76.5% Prior OSCC 75.9% Family history 75.2% | N.A. |
| Akbari et al., 2015 [30] | GDPs 55; specialists 18 | <75% | GDPs Tobacco 92.7% Specialists Tobacco 88.9% | GDPs Leukoplakia 58.2% Specialists Leukoplakia 66.7% | GDPs Submandibular lymph nodes as first place of metastasis 89.1%/OSCC 87.2%/Lung as first place of distant metastasis 67.3%/Two weeks is minimum time to differentiate cancer from inflammation 63.6%/Lower lip is related with better prognosis of oral cancer 49.1%/Minor salivary tumor commonly placed in lateral posterior palate 47.3% Specialists Submandibular lymph nodes as first place of metastasis 100%/OSCC 100%/Lung as first place of distant metastasis 88.9%/Two weeks is minimum time to differentiate cancer from inflammation 94.4%/Lower lip is related with better prognosis of oral cancer 77.8%/Minor salivary tumor common placed in lateral posterior palate 61.1% | GDPs Tongue 70.9% Floor of the mouth 56.4% Specialists Tongue 88.9% Floor of the mouth 88.9% | N.A. | N.A. | N.A. |
| Hassona et al., 2015 [74] | 165 | >75% | Tobacco 97.6% Prior OSCC 75.2% Alcohol 64.2% OPMDs 60.6% Betel quid chewing 53.9% Comorbidities 43% HPV 36.4 % Sun exposure 30.3% Elderly 26.7% Diet 21.8% | Leukoplakia 71.5% Erythroplakia 53.3% Candidiasis 42.4% OSMF 33.3% OLP 28.5% Actinic cheilitis 21.8% | OSCC time diagnosis >60 yrs 81.8% Positive lymph node 71.5% Ulcer 68.5% White patches 62.4% Dysphagia and limited tongue mobility 60.6% Red patch 59.4% Lump 58.8% Non-healing socket 38.2% | N.A. | N.A. | N.A. | Scalpel biopsy 84.8% Fluorescent imaging 68.5% Exfoliative cytology 46.7% Brush biopsy 28.5% Toluidine biopsy 24.2% |
| Allen et al., 2015 [31] | 640 | <75% | N.A. | N.A. | N.A. | N.A. | Visual examination is effective in early detection 98.9% Key role of dentist 90.9% Key role of dental hygienist 69% Key role of physician 48.2% | N.A. | Intra- and extraoral examination at 1st visit 94.5%; at recall 85.7% |
| Anandani et al., 2015 [32] | 83 | >75% | Betel quid chewing 34.1% Tobacco 27.7% Alcohol 14.1% Chronic disease 14.3% Family history 6.1% | N.A. | N.A. | Labial mucosa 26.2% Tongue 19.7% Floor of the mouth 8.2% Palate 6.6% | N.A. | N.A. | N.A. |
| Alaizari et al., 2014 [33] | 800 | >75% | Tobacco 96.4% Shammah usage 91.9% Betel chewing 79.2% Prior OSCC 76.9% Alcohol 73.3% Ill-fitting prothesis 70.1% Comorbidities 65.2% HPV 66.1% Elderly 48% Diet 41.6% Sun exposure 67% Obesity 24% | N.A. | OSCC 82.81% | Tongue and floor of the mouth 45.7% | Ease for referral 94.1% OSCC early diagnosis improves the survival rate 87.3% Need of CE 86% Biopsy is mandatory 75.1% Visual examination is effective in early detection 72.4% Smoking cessation is effective 72% Skills in neck examination 68.3% Up-to-date personal knowledge 47.1% | Tobacco 79.6% | Biopsy 75.1% Intra- and extraoral 68.3% Lymph nodes 68.3% |
| Mehdizadeh et al., 2014 [34] | 124 | >75% | N.A. | N.A. | OSCC 81.2% | Tongue 59.6% Floor of the mouth 58.8% | Need of CE 94% Delay in OSCC diagnosis 74.8% Key role of dentist 60.4% ENT has a key role in OSCC diagnosis 37.2% ENT has a key role in OSCC treatment 27.4% Undergraduate training was adequate 20.4% | Clinical chart 90.4% Recommendations in elderly 70% Addiction 67.6% Family history 52% Biopsy 37% | Intra- and extraoral 84.8% Lymph nodes 74.2% |
| Saleh et al., 2014 [35] | 362 | <75% | Tobacco 99.4% Betel quid chewing 99.2% Alcohol 88.9% HPV 67.2% | N.A. | Ulcer 97% White patch 93.1% Red patch 93.1% Gingival bleeding 67.1% | N.A. | N.A. | N.A. | Intra- and extraoral 84.8% |
| Ramaswamy et al., 2014 [36] | 450 | >75% | Tobacco 94% | N.A. | Ulcer 50% Red patch 50% | N.A. | N.A. | N.A. | Intra- and extraoral 90% |
| Razavi et al., 2013 [37] | 139 | >75% | Tobacco 97% Alcohol 78% Sun exposure 72% Iron deficiency 62% Ill-fitting prothesis 22% Poor oral hygiene 17% Diet 6% | Erythroplakia and leukoplakia 50% | Positive lymph node 67% Asymptomatic at early stage 45% Red patch 33% OSCC time diagnosis >60 yrs 33% | Tongue and floor of the mouth 51% | Key role of dentist 71% Undergraduate training was adequate 36% Adequate post graduate training 16% | N.A. | Intra- and extraoral 11% Lymph nodes 23% Biopsy 6% |
| Pentenero et al., 2013 [38] | 450 | >75% | Prior OSCC 51.1% | Leukoplakia 79.6% Erythroplakia 57.1% | N.A. | Tongue 74.4% Floor of the mouth 72.9% Palate 18.7% | Up-to-date personal knowledge 83.1% Need of CE 31.8% | N.A. | Intraoral 84% |
| Rocha–Boulevas et al., 2012 [39] | 93 | <75% | Prior OSCC 78.4% Tobacco 78.4% Alcohol 56.9% Elderly 44.1% Diet 17.2% | Erythroplakia and leukoplakia 51.61% | OSCC 52.6% Red patch 51.6% OSCC time diagnosis >60 yrs 47.3% | Tongue and floor of the mouth 18.2% | Smoking cessation is effective 74.19% Alcohol cessation is effective 67.74% Skills in neck examination 66.67% Lack of patients’ knowledge 47.3% Visual examination is effective in early detection 39.78% | Alcohol products 88.1% Alcohol 82.2% Prior OSCC 59.14% Tobacco products 50.54% Tobacco 49.4% Family history 22.58% | N.A. |
| Joseph et al., 2012 [40] | 153 | >75% | Tobacco 100% Prior OSCC 97.3% Betel quid chewing 89% Alcohol 88.8% Sun exposure 82.7% HPV 71.2% Elderly 60.3% Diet 52.7% | Erythroplakia and leukoplakia 93.2% | Asymptomatic at early stage 90.7% OSCC diagnosis (III/IV stage) 75% Positive lymph node 70.1% Visual inspection is the most effective screening method 50.4% | Tongue and floor of the mouth 85% | OSCCC early diagnosis improves survival rate 98% Ease for referral 89.5% Skills in neck examination 72.5% Up-to-date personal knowledge 51.6% Smoking cessation is effective 38.6% Visual examination is effective in early detection 38.6% Previous CE courses 30.1% Alcohol cessation is effective 20.3% | Tobacco 65% Alcohol 21.6% | Intraoral 86.3% Biopsy 62.9% |
| Vijay Kumar et al., 2012 [41] | 240 | <75% | Alcohol 99% Tobacco 78.3% Ill-fitting prothesis 53.7% Sun exposure 45% Elderly 31.2% | Blistering 3% | OSCC 96% White patch 82% OSCC time diagnosis >60 yrs 59% Red erosion 9% | Buccal mucosa 83% | Ease for referral 98.7% Annual visual inspection for patients over 40 is mandatory 67.9% Visual examination is effective in early detection 68.3% Skills in neck examination 50.4% Up-to-date personal knowledge 39.1% | Tobacco 68% Alcohol 68% | Intra- and extraoral 37% Lymph nodes 37% Biopsy 24% |
| Seoane et al., 2012 [42] | 791 | >75% | N.A. | N.A. | N.A. | N.A. | N.A. | N.A. | Intraoral 90.3% Biopsy 28.7% |
| Maybury et al., 2012 [43] | 463 | >75% | Tobacco 98% Prior OSCC 97% Alcohol 95% HPV 88% Elderly 71% Sun exposure 64% Diet 35% | Erythroplakia and leukoplakia 42% | OSCC 83% Asymptomatic at early stage 80% Red patch 81% Positive lymph node 77% Tongue high-risk area 72% OSCC time diagnosis >60 yrs 30% OSCC diagnosis (III/IV stage) 28% | Tongue 59% | Up-to-date personal knowledge 81% Visual examination is effective in early detection 94% Skills in neck examination 79% Smoking cessation is effective 32% Alcohol cessation is effective 15% | N.A. | N.A. |
| Alami et al., 2012 [75] | 55 | >75% | Tobacco 92% Alcohol 83% Sun exposure 67% Elderly 62% HPV 47% Diet 33% | Erythroplakia 47.3% Leukoplakia 40% OLP 14.5% Nicotinic stomatitis 14.5% | OSCC 98.2% Red or white patch 94.5% Asymptomatic at early stage 90.9% Positive lymph node 80% OSCC diagnosis (III/IV stage) 75.9% | Floor of the mouth 45.5% Tongue 29.1% Lips 29.1% | N.A. | N.A. | N.A. |
| Borhan–Mojabi et al., 2011 [76] | 86 | >75% | Tobacco 78.3% Alcohol 34.9% | N.A. | N.A. | Tongue 80.9% Lips 28.3% Floor of the mouth 25.7% | Lack of patients’ knowledge 40.7% | N.A. | Intraoral 79.15% |
| Hertrampf et al., 2011 [44] | 306 | >75% | Tobacco 99% Prior OSCC 95.1% Alcohol 92.8% Sun exposure 68% Elderly 60.5% HPV 57.8% Diet 19% | Erythroplakia and leukoplakia 67.6% | OSCC 86.9% Need of three negative follow-ups 84.6% OSCC diagnosis (III/IV stage) 81% Tongue high-risk area 67.6% Red patch 59.5% OSCC time diagnosis >60 yrs 47.7% Asymptomatic in the early stages 47.1% | Floor of the mouth 76.1% Tongue 70.3% | OSCC early diagnosis improves the survival rate 98.4% | N.A. | Intraoral 84.3% |
| Decuseara et al., 2011 [45] | 254 | >75% | Alcohol 98% Tobacco 98% Prior OSCC 83% Sun exposure 79% HPV 60% Elderly 53% Radiotherapy 39% Spicy food 33% Diet 28% Hot food and drink 9% | Leukoplakia 87% Erythroplakia 82% Erythroplakia and leukoplakia 80% | Asymptomatic at early stage 95% Tongue high-risk area 87% OSCC diagnosis (III/IV stage) 86% OSCC time diagnosis >60 yrs 42% | Floor of the mouth 86% Tongue 70% | OSCC early diagnosis improves the survival rate 95% Visual examination is effective in early detection 73% Skills in neck examination 55% Smoking cessation is effective 33% Alcohol cessation is effective 13% | Tobacco 75% Prior OSCC 70% Alcohol 45% | Intra- and extraoral 97% |
| Hertrampf et al., 2010 [46] | 306 | >75% | Tobacco 99% Alcohol 93% Prior OSCC 95% Sun exposure 68% Elderly 61% HPV infection 58% Diet 19% | Erythroplakia and leukoplakia 67% | OSCC 87% Need of three negative follow-ups 85% OSCC diagnosis (III/IV stage) 81% Positive lymph node 71% Tongue high-risk area 68% Red patch 60% Asymptomatic at early stage 47% OSCC time diagnosis >60 yrs 46% | Floor of the mouth 76% Tongue 70% | OSCC early diagnosis improves the survival rate 90% | N.A. | Intraoral 70% |
| Reed et al., 2010 [77] | 288 | <75% | Tobacco 90% Betel quid chewing 88% Alcohol 45% HPV 26% Diet 6% | N.A. | N.A. | N.A. | N.A. | Tobacco 70% | Intraoral 81% |
| Klosa et al., 2010 [47] | 306 | >75% | N.A. | N.A. | N.A. | N.A. | Annual visual inspection for patients over 40 is mandatory 84% Dentists are qualified to perform OSCC examination 71% Visual examination is effective in early detection 63% | Tobacco 65% Prior OSCC 65% Tobacco products 45 Family history 40% Alcohol 35% Alcohol products 25% | Intra- and extraoral 28% |
| López–Jornet et al., 2010 [48] | 340 | >75% | Tobacco 100% Alcohol 96.4% Prior OSCC 95.5% Ill-fitting prothesis 95.5% Family history 87.1% Poor oral hygiene 77.6% Elderly 69.4% Diet 52.6% Spicy foods 40.8% Obesity 14.4% | Erythroplakia and leukoplakia 95% | Tongue high-risk area 96.8% Asymptomatic at early stage 95.6% OSCC diagnosis (III/IV stage) 94.7% OSCC 90.6% Positive lymph node 86.2% Red/white patch 89.7% OSCC time diagnosis >60 yrs 72.6% | Tongue and floor of the mouth 89.1% | Dentists are qualified to perform OSCC examination 94.7% Ease for referral 90.9% Annual visual inspection for patients over 40 is mandatory 89.7% Skills in neck examination 52.6% Up-to-date personal knowledge 49.7% Physicians are qualified to perform OC examination 41.8% Smoking cessation is effective 41.5% Alcohol cessation is effective 27.6% Dental hygienists are qualified to perform OC examination 13.8% | N.A. | N.A. |
| Seoane–Leston et al., 2010 [49] | 440 | >75% | Diet 18.6% | Leukoplakia 78% OLP 72% | N.A. | N.A. | N.A. | N.A. | N.A. |
| Applebaum et al., 2009 [78] | 274 | >75% | N.A. | Erythroplakia and leukoplakia 34% | N.A. | N.A. | Dentists are qualified to perform OSCC examination 96% Visual examination is effective in early detection 85% Lack of patients’ knowledge 79.5% Skills in neck examination 66.67% Up-to-date personal knowledge 50% Physicians are qualified to perform OC examination 45% Smoking cessation is effective 24% Alcohol cessation is effective 12% | Tobacco 85.5% Prior OSCC 85% Family history 56% Alcohol 51% Tobacco products 34% Alcohol products 34% | N.A. |
| Mahalaha et al., 2009 [50] | 34 | >75% | N.A. | N.A. | OSCC 79.4% Red patch 76.5% Tongue high-risk area 70% Asymptomatic at early stage 67.6% Positive lymph node 56.3% OSCC time diagnosis >60 yrs 30.3% Persistent ulcer 26.5% Need of three negative follow-ups 6.2% Bleeding area 2.9% Pain 2.9% Swelling 2.9% | Tongue and floor of the mouth 62% | Annual visual inspection for patients over 40 is mandatory 100% Ease for referral 96.9% Dentists are qualified to perform OSCC examination 96.9% Visual examination is effective in early detection 84.4% Skills in neck examination 71.9% Up-to-date personal knowledge 70% Undergraduate training was adequate 65.7% | N.A. | Intra- and extraoral examination at 1st visit 83% at recall 73% Lymph nodes 57% |
| Colella et al., 2007 [12] | 457 | >75% | Tobacco 94.1% Prior OSCC 89.5% Alcohol 79.2% Elderly 47.9% Diet 25.8% | Erythroplakia and leukoplakia 53.8% | N.A. | Tongue and floor of the mouth 32% | Smoking cessation is effective 80.9% Alcohol cessation is effective 76.5% Visual examination 53.8% Skills in neck examination 66.8% Lack of patients’ knowledge 39.6% | Tobacco 81.8% Prior OSCC 78.6% Alcohol 71.9% Alcohol products 59.9% Tobacco products 55.6% Family history 47.9% | Intra- and extraoral examination at 1st visit 52.3% |
| LeHew et al., 2007 [51] | 518 | >75% | Elderly 47.9% Family history 31.3% Alcohol 8.1% Tobacco 1.2% | Leukoplakia 83.6% Erythroplakia 72% | OSCC 74.7% Positive lymph node 64.3% White patch 53.9% OSCC time diagnosis >60 yrs 20.1% Red patch 31.5% | Tongue 77.4% Floor of the mouth 72% Buccal mucosa 26.3% | Need of CE 74.5% | Tobacco 76.1% Tobacco products 63.5% Alcohol 47.4% Alcohol products 28.8% | Intra- and extraoral 92.3% Lymph nodes 71.5% |
| Gajendra et al., 2006 [52] | 499 | >75% | Tobacco 90% Alcohol 80% Sun exposure 60% Elderly 55% Betel quid chewing 52% Diet 25% Gutka consumption 16% | N.A. | OSCC time diagnosis >60 yrs 33% | N.A. | Visual examination is effective in early detection 82% Previous CE courses 80% Skills in neck examination 75% Up-to-date personal knowledge 72% Lack of patient’s knowledge 65% Dentist skills in visual inspection 53% Dental hygienist skills in visual inspection 38% Smoking cessation is effective 20% Alcohol cessation is effective 15% | Prior OSCC 79% Tobacco 70% Tobacco products 58% Family history 57% Alcohol 45% Alcohol products 31% | Intra- and extraoral 85% |
| Kujan et al., 2006 [53] | 143 | <75% | N.A. | N.A. | N.A. | N.A. | Undergraduate training was adequate 51% | Prior OSCC 74.2% Tobacco 67.1% Tobacco products 55.2% Alcohol 41.3% Betel quid chewing 39.8% Alcohol products 32.8% Family history 21% Diet 25.3% Sun exposure 10.5% | Intra- and extraoral 92% |
| Seoane et al., 2006 [54] | 32 | <75% | N.A. | N.A. | N.A. | N.A. | N.A. | N.A. | Scalpel biopsy 96.9% Intraoral examination 87.5% Toluidine blue 9.4% |
| Patton et al., 2005 [55] | 584 | >75% | Tobacco 100% Prior OSCC 99% Alcohol 95% Elderly 76% Sun exposure 74% HPV 60% Diet 39% | Erythroplakia and leukoplakia 73% | Need of three negative follow-ups 98% OSCC 84% Red patch 82% Asymptomatic at early stage 79% Positive lymph node 70% Tongue high-risk area 77% OSCC diagnosis (III/IV stage) 53% OSCC time diagnosis >60 yrs 29% | Floor of the mouth 79% Tongue 78% | OSCC early diagnosis improves survival rate 99% | N.A. | Intraoral 83% |
| Cruz et al., 2005 [56] | 904 | <75% | N.A. | N.A. | N.A. | N.A. | N.A. | Tobacco 77% Tobacco products 66% Alcohol 54.5% Alcohol products 36% | Intra- and extraoral examination at 1st visit 86%; at recall 80% |
| Alonge et al., 2004 [57] | 158 | >75% | Tobacco 98% Alcohol 98% Prior OSCC 93% Hot food and drink 75% Elderly 74% Spicy food 73% Family history of cancer 70% Obesity 63% Poor oral hygiene 42% Diet 37% Ill-fitting prothesis 33% | Erythroplakia and leukoplakia 31% | OSCC 84% Positive lymph node 79% Red patch 76% Asymptomatic at early stage 76% Tongue high-risk area 68% Lip cancer related to the sun 76% OSCC diagnosis (III/IV stage) 53% OSCC time diagnosis >60 yrs 39% | Tongue and floor of the mouth 51% | Need of CE 81% Undergraduate training was adequate 75% Previous CE courses 64% | N.A. | Intra- and extraoral examination at 1st visit 67% Recall visit 54% Lymph nodes 36% |
| Macpherson et al., 2003 [79] | 225 | >75% | Tobacco 94% Alcohol 90% HPV 35% Fungal infections 33% | Leukoplakia 79% Erythroplakia 67% | N.A. | N.A. | N.A. | N.A. | N.A. |
| Clovis et al., 2002 [58] | British Columbia 401 Nova Scotia 269 | <75% | Tobacco 99.4% Prior OSCC 96.6% Alcohol 90.4% Elderly 78.7% Sun exposure 70.1% HPV 53.1% Diet 34% | Erythroplakia and leukoplakia 76% | Need of three negative follow-ups 92.4% OSCC 83.4% Asymptomatic at early stage 78.4% Red patch 77.3% Tongue high-risk area 75.7% Positive lymph node 68.1% OSCC diagnosis (III/IV stage) 54.4% OSCC time diagnosis >60 yrs 45.7% | Tongue 78.7% Floor of the mouth 66.6% | OSCC early diagnosis improves the survival rate 97.8% Up-to-date personal knowledge 56.8% | N.A. | Intraoral 80.6% |
| Clovis et al., 2002 [59] | British Columbia 401; Nova Scotia 269 | <75% | N.A. | N.A. | N.A. | N.A. | British Columbia Visual examination is effective in early detection 83.1% Skills in neck examination 74.8% Undergraduate training was adequate 68.5% Smoking cessation is effective 11.4% Alcohol cessation is effective 5.3% Nova Scotia Visual examination is effective in early detection 79.5% Skills in neck examination 69.4% Undergraduate training was adequate 68.3% Smoking cessation is effective 7.8% Alcohol cessation is effective 5.3% | British Columbia Prior OSCC 93.1% Tobacco 76.8% Family history 69.6% Tobacco products 62.4% Alcohol 35.65 Alcohol products 17.7% Nova Scotia Tobacco 82% Prior OSCC 87.4% Family history 64.5% Tobacco products 60.1% Alcohol 39.3% Alcohol products 23.4% | British Columbia Intra- and extraoral examination at 1st visit 71.2%; at recall 54.5% Lymph nodes 27.4% Nova Scotia Intra- and extraoral examination at 1st visit 69.9%; at recall 45.7% Lymph nodes 26.2% |
| Canto et al., 2001 [60] | 508 | >75% | Tobacco 100% Prior OSCC 97% Alcohol 95% Elderly 68% Sun exposure 62% Diet 30% | Erythroplakia and leukoplakia 32% | OSCC 82% Red patch 81% Asymptomatic at early stage 76% Positive lymph node 76% Tongue high-risk area 71% OSCC diagnosis (III/IV stage) 50% OSCC time diagnosis >60 yrs 35% | Tongue and floor of the mouth 62% | N.A. | N.A. | N.A. |
| Greenwood et al., 2001 [80] | 143 | >75% | Tobacco 90.7% Betel quid chewing 60.8% Alcohol 45.7% | N.A. | N.A. | N.A. | N.A. | N.A. | Intra- and extraoral 68.2% |
| Yellowitz et al., 2000 [61] | 3200 | >75% | Tobacco 99.7% Alcohol 92.7% Prior OSCC 96.4% Elderly 70% Sun exposure 64% Diet 33% | Erythroplakia and leukoplakia 37% | OSCC 83% Red patch 80% Asymptomatic at early stage 76% Tongue high-risk area 71% Positive lymph node 69% OC diagnosis (III/IV stage) 51% OSCC time diagnosis >60 yrs 33% | Tongue and floor of the mouth 54% | Need of CE 84% Up-to-date personal knowledge 68% | N.A. | Intraoral 81% |
| Horowitz et al., 2000 [62] | 3200 | >75% | N.A. | N.A. | N.A. | N.A. | Visual examination is effective in early detection 88% Undergraduate training was adequate 78% Skills in neck examination 72% Smoking cessation is effective 28% Alcohol cessation is effective 11% | Prior OSCC 91% Tobacco 83.5% Tobacco products 72% Family history 65% Alcohol 55% Alcohol products 33% | Intra- and extraoral examination at 1st visit 81% at recall 68% Lymph nodes 30% |
| Horowitz et al., 2000 [63] | 243 | >75% | N.A. | N.A. | N.A. | N.A. | Visual examination is effective in early detection 92.6% Skills in neck examination 76.5% Undergraduate training was adequate 74% Smoking cessation is effective 25% Alcohol cessation is effective 11.5% | Prior OSCC 92.1% Tobacco 84.2% Tobacco products 70.2% Family history 69.2% Alcohol 60.9% Alcohol products 35.8% | Intra- and extraoral examination at 1st visit 83.7% at recall 78.3% Lymph nodes 34.3% |
| Warnakulasuriya et al., 1999 [64] | 2519 | <75% | N.A. | N.A. | N.A. | N.A. | N.A. | Tobacco 50.2% Alcohol 19.3% | Intra- and extraoral 84% Biopsy 21% |
| Yellowitz et al., 1998 [65] | 243 | <75% | Tobacco 99.6% Sun exposure 97.9% Prior OSCC 95.7% Alcohol 90.8% Elderly 68.9% Ill-fitting prothesis 64.6% Poor oral hygiene 47.2% Diet 33.6% | Erythroplakia and leukoplakia 36% | OSCC 83% OSCC time diagnosis >60 yrs 30% Asymptomatic at early stage 27% | Tongue 74% Floor of the mouth 68% Tongue and floor of the mouth 46% Buccal mucosa 30% Palate 14% | Annual visual inspection for patients over 40 is mandatory 97.6% OSCC early diagnosis improves survival rate 96.4% Visual examination is effective in early detection 88% Up-to-date personal knowledge 83.7% Skills in neck examination 77.2% Lack of patients’ knowledge 67% | Tobacco 78.5% Tobacco products 65% Alcohol 40.5% Alcohol products 20% | Intra- and extraoral examination at 1st visit 33% Lymph nodes 33% |
| Yellowitz et al., 1995 [81] | 57 | >75% | N.A. | N.A. | OSCC time diagnosis >60 yrs 89% Pain 37.5% | N.A. | Annual visual inspection for patients over 40 is mandatory 92.5% Ease to referral 88.2% Up-to-date personal knowledge 73.1% OSCC early diagnosis improves the survival rate 65.5% | N.A. | N.A. |
| Knowledge | Attitude | Practice | |||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Participants | Quality Assessment | Risk Factors | Precancerous Lesions | Clinical Picture | Common Sites of Development | Opinion | History Taking | Physical Examination |
| Shanahan et al., 2018 [66] | 221 | >75% | Tobacco 93.7% OPMDs 69.1% Alcohol 63.3% HPV 29% Comorbidities 8.6% Betel quid chewing 5.9% Sun exposure 3.2% Diet 2.3% | Leukoplakia 34.5% Erythroplakia 14.5% Erythroleukoplakia 1.4% | Ulcer 67.3% Exophytes 31.4% Bleeding 15.5% Positive lymph node 3.2% Necrosis 1.4% Fixation 0.9% Induration 0.5% | N.A. | Visual examination is effective in early detection 14% | N.A. | N.A. |
| Shimpi et al., 2016 [67] | 121 | >75% | N.A. | Leukoplakia 65.3% | Abnormal growth 100% Ulcer 100% | N.A. | Smoking cessation is effective 100% Skills in neck examination 100% Ease for referral 56% Annual visual inspection for patient over 40 is mandatory 53% Undergraduate training was adequate 44% | N.A. | Intra- and extraoral 53% |
| Hassona et al., 2015 [74] | 165 | >75% | Tobacco 95.8% Prior OSCC 72.1% OPMDs 69.1% Comorbidities 57.6% Betel quid chewing 53.9% Alcohol 50.3% HPV 50.3% Elderly 47.9% Diet 31.5% Sun exposure 18.2% | Leukoplakia 61.2% OSMF 37.6% Candidiasis 37% Erythroplakia 35.2% OLP 27.9% Actinic cheilitis 13.9% | OSCC time diagnosis > 60 yrs 78.8% Dysphagia and limited tongue mobility 73.9% Positive lymph nodes 72.1% Lump 67.9% Ulcer 66.7% White patch 49.1% Non-healing socket 47.9% Red patch 44.2% | N.A. | N.A. | N.A. | Fluorescent imaging 77.6% Scalpel biopsy 73.3% Exfoliative cytology 56.4% Brush biopsy 43% Toluidine biopsy 17.6% |
| Hertrampf et al., 2014 [68] | 192 GMPs 135 INTs 33 ENTs 28 DERMs | >75% | ENTS Tobacco 100%/Alcohol 100%/Prior OSCC 100%/Elderly 73% /HPV 70% /Sun exposure 64%/Diet 24% GMPs Tobacco 99%/Prior OSCC 94%/Alcohol 91%/Elderly 78%/HPV 54%/Sun exposure 46%/Diet 34% INTs: Tobacco 94.5%/Prior OSCC 92.5%/Alcohol 88.5%/Elderly 70.5% /HPV 50.5%/Sun exposure 48% /Diet 40% DERMs Sun exposure 96%/Prior OSCC 93%/Tobacco 93%/HPV 82%/Alcohol 79%/Elderly 75%/Diet 18% | ENTs Erythroplakia and leukoplakia 91% GMPs Erythroplakia and leukoplakia 85% INTs Erythroplakia and leukoplakia DERMs Erythroplakia and leukoplakia 82% | ENTs Positive lymph node 94% OSCC 91% OSCC diagnosis (III/IV stage) 85% Asymptomatic at early stage 27% GMPs OSCC diagnosis (III/IV stage) 85% Positive lymph node 82% OSCC 75% Asymptomatic at early stage 51% INTs OSCC diagnosis (III/IV stage) 85.5% Positive lymph node 85% OSCC 83.5% Asymptomatic at early stage 55% DERMs OSCC 93% OSCC diagnosis (III/IV stage) 82% Asymptomatic at early stage 82% Positive lymph node 79% | ENTs Floor of the mouth 67% Tongue 67% GMPs Floor of the mouth 71% Tongue 52% INTs Floor of the mouth 71% Tongue 60% DERMs Floor of the mouth 75% Tongue 61% | N.A. | N.A. | ENTs Intraoral 100% GMPs Intraoral 84% INTs Intraoral 78.5% DERMs Intraoral 89% |
| Tanriover et al., 2014 [69] | 164 | >75% | Tobacco 98.8% Prior OSCC 93.9% Poor oral hygiene 93.3% Alcohol 89% Family history 90.2% Elderly 87.8% Spicy foods 84.8% Sun exposure 73.2% Diet 68.9% | Erythroplakia and leukoplakia 84.1% | OSCC 75.6% | Floor of the mouth 51.8% Tongue 48.8 % | OSCC early diagnosis improves survival rate 87.8% | Tobacco 78.5% Tobacco products 70.1% Alcohol 56.7% Alcohol products 43.3% | Intra- and extraoral 65.2% |
| Alami et al., 2012 [75] | 57 | >75% | Tobacco 91% Alcohol 61% Elderly 48% Diet 25% HPV 22% Sun exposure 15% | Leukoplakia 64.9% Erythroplakia 17.5% OLP 12.3% Nicotinic stomatitis 12.3% | Positive lymph node 92.9% OSCC 89.3% Red or white patch 89.1% Asymptomatic at early stage 78.6% OSCC diagnosis (III/IV stage) 50% | Lips 42.1% Floor of the mouth 33.3% Tongue 22.8% | N.A. | N.A. | N.A. |
| Borhan–Mojabi et al., 2011 [76] | 66 | >75% | Tobacco 78.3% Alcohol 34.9% | N.A. | N.A. | Tongue 80.9% Lips 28.3% Floor of the mouth 25.7% | Adequate knowledge 51.5% | N.A. | Intraoral 39.4% |
| Reed et al., 2010 [77] | 221 | >75% | Betel quid chewing 98% Tobacco 90% Alcohol 37% HPV 18% Diet 4% | N.A. | N.A. | N.A. | N.A. | Alcohol 100% Prior OSCC 100% Tobacco 100% Alcohol products 97% Family history 97% Tobacco products 97% | N.A. |
| Applebaum et al., 2009 [78] | 118 | >75% | N.A. | Erythroplakia and leukoplakia 10% | N.A. | N.A. | Dentists are qualified to perform OSCC examination 91% Smoking cessation is effective 85% Alcohol cessation is effective 75% Physicians are qualified to perform OSCC examination 67% Visual examination is effective in early detection 46% Adequate knowledge 5% | Alcohol 100% Prior OSCC 100% Tobacco 100% Alcohol products 97% Family history 97% Tobacco products 97% | N.A. |
| Riordain et al., 2009 [70] | 236 | >75% | Tobacco 98.7% Alcohol 50.8% Poor oral hygiene 20.7% Elderly 5% Comorbidities 2.5% Ill-fitting prothesis 2.5% Spicy food 2.5% Dental caries 1.7% Male gender 1.2% Betel quid chewing 0.8% Gastric reflux 0.8% | Leukoplakia 12.7% OLP 1.2% Erythroplakia 0.4% | Ulcer 67.4% Pain 30.9% Swelling 21.6% Positive lymph node 16.5% Dysphagia 16.5% Bleeding 12.7% Lump 12.7% Halitosis 1.2% Hemoptysis 1.2% Burning sensation 0.8% Cough 0.8% Drooling 0.4% Hoarseness 0.4% | N.A. | Need of CE 99.6% Previous CE courses 3.39% | N.A. | N.A. |
| LeHew et al., 2009 [71] | 8 | <75% | Tobacco 87% Alcohol 62% | Leukoplakia 75% Erythroplakia 62% | N.A. | N.A. | N.A. | N.A. | N.A. |
| Nicotera et al., 2004 [72] | 198 | >75% | Tobacco 87.6% Alcohol 64% Prior OSCC 31.5% Elderly 2.8% | Leukoplakia 91.5% Erythroplakia 41.7% | OSCC 60.9% Red patch 17.6% | Tongue 68.8% Floor of the mouth 37.1% | Need of CE 84.9% | Tobacco 85.1% Alcohol 82.5% Prior OSCC 52.9% Family history 48.1% | Intra- and extraoral 63.8% |
| Macpherson et al., 2003 [79] | 198 | >75% | Tobacco 97% Alcohol 79% Elderly 76% HPV 23% Fungal infections 20% | Erythroplakia 22% Leukoplakia 72% | N.A. | N.A. | N.A. | N.A. | N.A. |
| Canto et al., 2002 [73] | 240 | >75% | Tobacco 100% Prior OSCC 99.2% Alcohol 89.3% Sun exposure 55.5% Elderly 42% Diet 29.5% | Erythroplakia and leukoplakia 10.4% | Positive lymph node 86.1% OSCC 80.2% Asymptomatic at early stage 71.3% OSCC diagnosis (III/IV stage) 60.1% Red patch 57% OSCC time diagnosis >60 yrs 42% Tongue high-risk area 34.5% | Tongue and floor of the mouth 25.4% | Skills in neck examination 98.8% Smoking cessation is effective 88.2% Alcohol cessation is effective 76% Visual examination is effective in early detection 61.8% Undergraduate training was adequate 53.8% | Alcohol 77% Alcohol products 77% Family history 77% Prior OSCC 77% Tobacco 77% Tobacco products 77% | Intraoral 90.7% |
| Greenwood et al., 2001 [80] | 151 | >75% | Tobacco 90.7% Betel quid chewing 50.3% Alcohol 45.7% | N.A. | N.A. | N.A. | N.A. | N.A. | Intra- and extraoral 68.2% |
| Yellowitz et al., 1995 [81] | 93 | <75% | N.A. | N.A. | OSCC time diagnosis > 60 yrs 92.6% Pain 50.7% | N.A. | Annual visual inspection for patients over 40 is mandatory 84.1% OSCC early diagnosis improves the survival rate 63.3% Ease for referral 51.3% Up-to-date personal knowledge 32.6% | N.A. | N.A. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coppola, N.; Mignogna, M.D.; Rivieccio, I.; Blasi, A.; Bizzoca, M.E.; Sorrentino, R.; Lo Muzio, L.; Spagnuolo, G.; Leuci, S. Current Knowledge, Attitudes, and Practice among Health Care Providers in OSCC Awareness: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4506. https://doi.org/10.3390/ijerph18094506
Coppola N, Mignogna MD, Rivieccio I, Blasi A, Bizzoca ME, Sorrentino R, Lo Muzio L, Spagnuolo G, Leuci S. Current Knowledge, Attitudes, and Practice among Health Care Providers in OSCC Awareness: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(9):4506. https://doi.org/10.3390/ijerph18094506
Chicago/Turabian StyleCoppola, Noemi, Michele Davide Mignogna, Immacolata Rivieccio, Andrea Blasi, Maria Eleonora Bizzoca, Roberto Sorrentino, Lorenzo Lo Muzio, Gianrico Spagnuolo, and Stefania Leuci. 2021. "Current Knowledge, Attitudes, and Practice among Health Care Providers in OSCC Awareness: Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 9: 4506. https://doi.org/10.3390/ijerph18094506
APA StyleCoppola, N., Mignogna, M. D., Rivieccio, I., Blasi, A., Bizzoca, M. E., Sorrentino, R., Lo Muzio, L., Spagnuolo, G., & Leuci, S. (2021). Current Knowledge, Attitudes, and Practice among Health Care Providers in OSCC Awareness: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(9), 4506. https://doi.org/10.3390/ijerph18094506











