Workplace Healthy Lifestyle Determinants and Wellbeing Needs across the Preconception and Pregnancy Periods: A Qualitative Study Informed by the COM-B Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Participants
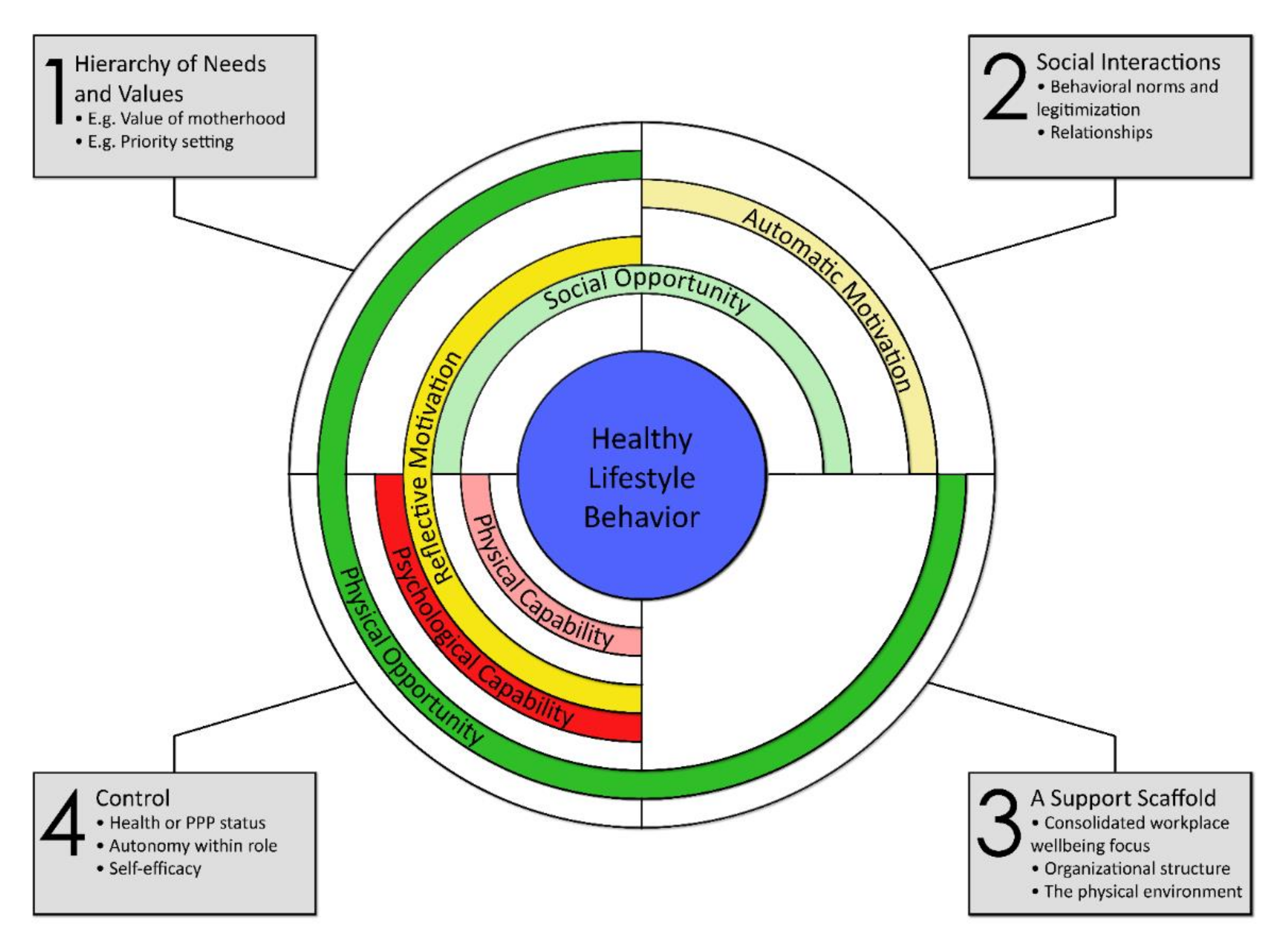
3.2. Themes
3.2.1. Theme 1: Hierarchy of Needs and Values
There is the time problem… sometimes, depending on the time of the year, if I have deadlines, I don’t have time to go to the gym.(FG5)
I totally get the message that health is also not optional, but the reality is if there’s ten things on the list, and I can only get through seven of them, I have to…prioritize these other things.(FG5)
It made it even worse because I was, like, so upset and I got told ‘be strong for your team’. It’s like, what? So, I’m not allowed to be upset? And that was pretty much the message I got was ‘be really strong’.(FG2)
I think that with students you visually see them… like those two women who can have their babies at University and still study, like that is a fantastic thing visually, but I don’t think I could, if I had a baby, I couldn’t bring my baby to work.(FG1)
Also, in your job… like I love doing my job well, but… my current contract’s over in six months and I can already feel myself going, ‘I don’t give a shit about that anymore’, whatever it is, because I’m not going to be there, you know, pushing it anymore… But I don’t know why the university don’t value, you know, staff like myself a little bit more.(FG2)
When they come back from maternity leave…they consequently lose their office and they go to a shared environment, where previously they had their own office with their own things. So, there’s a disadvantage there in even having a baby, because you are coming back with less than what you started with…it’s just what it says…(FG5)
I’ve worked in many different workplaces, like a lot of male-dominated workplaces, and the comments, not necessarily directed at me, but directed at maternity leave in general here have been, like I was so shocked about just the comments, like there was an academic that basically said he would not employ… a woman of child-bearing age.(FG1)
You do get the sense that women carry that unfair burden of the leave stigma, I mean there’s also a man at work somewhere who’s a father to a baby, who’s part of that conception, part of that gestation process and that birth process, whose career is not touched, you know, and it’s not fair is it?(FG1)
3.2.2. Theme 2: Social Interactions
Relationships
Members of the team go out… They were walking three to four times a week, even [if] it’s just, like, 45 min to an hour, particularly if the weather was good…(FG2)
They really understand connectivity… like every month they celebrate somebody’s birthday. They’ll celebrate…they’ll connect, they come out and have lunch together…those kinds of things.(FG4)
It was really tricky early on…to find somewhere to, to breastfeed on this campus, and my success in continuing to breastfeed was because I had a boss who…as we got to know each other a bit better… She had a tiny office, and we would sit back-to-back, while I was doing it.(FG3)
I think there’s an incredible variety of experiences of this here, there’s such a vast organization and there are so many decision makers and so much depends on your immediate supervisor. And I hear stories that are really positive, and you just think, ‘that’s fantastic’, and then you hear other stories and you just think, ‘What decade are we in?’(FG5)
Behavioral Norms and Legitimization of Health Behaviors
I do have a boss and the next boss up as well who are very, like, big on lunch breaks and will… be seen even when they’re busy going and taking a lunch break and they will encourage you to take a lunch break.(FG3)
I’m in a middle management position and I would say that I’m a really bad example to my staff… like most people definitely get a lunch, a lot of people are able to go for walks and things like that. So, I would encourage and support that… But yeah, I work all day, I go home and…still work and I work on the weekends to do…my job. But that’s life.(FG2)
[It] can be a very flexible working environment as well, like working around your children and there’s a lot of people where I work, there’s hardly anyone that actually works nine to five, five days a week. They’re all starting early, finishing early or staying late, or just not working that day or doing all sorts of hours or working from home and school pickups and it’s… really supportive.(FG2)
There was one girl who was pregnant a few years ago. I don’t really know… Probably not anyone who’s in a management role like me, rather [those who] already have had children or a lot of them are males to be honest.(FG3)
We had probably a higher number of women and young women, so it was always a bit of a running…you know, oh gosh, trying to replace the person that’s having the baby, so rather than see that as a problem because they’re like, oh my God, like now you know, who’s going to do that job?(FG2)
3.2.3. Theme 3: A Support Scaffold
Consolidated Workplace Wellbeing Focus
[The workplace] does a lot of ‘ad-hockery’, so you have things that [are] offered and it’s someone who’s got passionate and made it happen. And you don’t know if it’s going to carry on, it’s just…you don’t know if it’s consistent.(FG5)
Yeah, so I think it’s probably something that needs to be broadcast a bit more and there’s a lot of things, like, that I think on this campus that are just not well organized and communicated.(FG4)
It comes down to the… whose responsibility is it though? Like we don’t have a health and wellbeing full-time staff member that runs all these things…(FG4)
We are working in a culture, in an environment that hasn’t been people-centered for a long time and stress is just considered a normal part of doing business, and people’s stress levels… there’s a reason they stopped doing the staff surveys. They don’t want to know…(FG5)
If you are seeing pregnancy or parenting as a challenging situation to manage at work, then that says something about the place that you’re working in. If you are having to figure out how I can make this incredible life event have the minimal impact on my workplace and my career, the way I do my job…(FG5)
Organizational Structure
Yeah, having facilities and feeling like you can use them away from your desk because… I’m not a part of the school, I’m employed centrally and sometimes when you look into the team and you, you get funny looks…(FG1)
The Physical Environment
I think the food offerings on this campus are abysmal, have been for many years, getting worse and they don’t support healthy eating. They make it very hard to eat… Especially if you are just pushed for time and you just need a quick something, it’s very hard to choose healthy if you are grabbing something and going back to your desk. They need to make it much easier.(FG5)
These little bar fridges, everyone brings their lunch and they’re packed in there, and it’s not really accommodated in some areas for people to all bring their lunch and have a fridge.(FG4)
I have to move around a bit as my stakeholders are located in many places and this campus being on a hill, I get to walk up that hill quite a lot and stairs, three flights.(FG1)
There’s nothing available, you have to physically talk to someone. And sometimes you won’t want to talk to your supervisor to say, ‘hey, I’m thinking about becoming pregnant. Is there somewhere that I shouldn’t be going in the lab?’(FG2)
3.2.4. Theme 4: Control
Health or Preconception, Pregnancy, or Postpartum (PPP) Status
I had a dodgy ankle and I tend to like food for comfort, and I wasn’t able to do as much exercise. Um, so you know, put a bit of weight on and formed lots of bad habits like eating chocolate after meals and eating chocolate all day long really.(FG2)
For some people, if it is hard to get pregnant, the main thing you worry about is whether it works or not… But yeah, the idea of waiting until you are healthier, I hadn’t been in a position to think of that and I think it’s great that you can.(FG3)
Autonomy Within Work Role
So many times, you can be doing two-hour practical tutorials in the… lab, four of them in a row, back-to-back…You’re supposed to have 10 min, but of course all the students were desperate to talk to you.(FG4)
But someone who I know does work kind of reduced hours and is in a position which is kind of a similar level to mine. And she kind of leaves early, which is a bad way of phrasing it, but… I feel like you’d just end up doing the same amount of work anyway.(FG3)
So, all our committee meetings are on a Friday and I’m not working on a Friday at the moment, so I’m on committees, but it’s meaningless because I can’t come the meetings… You’re an apology, but I actually feel like I’m apologizing for not being there. I feel bad. I’m letting them down, how can I be on a committee and not turn up? And I’m not paid to be there.(FG3)
In a way I already feel so compromised working part time and not just working part time but consistently working just slightly shorter hours on every day than I really should or would like to… It feels like I can’t ask anything more of [my workplace] like that, like I’m squeezing from them as much as I can simply by coming back part time and working those shorter hours. So, the idea for example, of going to the gym at lunch time… It’s almost incomprehensible to me because I work through lunch because I’m going to be leaving at quarter to four to pick up the kids and I might spend 10 min eating a sandwich…(FG3)
There are people, like, who are in relatively low, like, frontline roles like call centers or reception type roles where if they go out for the day, like kid gets sick you have to go pick them up, it actually does cause a challenge. It’s a management challenge…(FG5)
But it’s more than food for me, it’s also the sedentary nature of my job, it’s extremely sedentary and more so every year as we become more efficient and the job requires more just sitting at your desk and powering through the work, less opportunity to move during the day. That’s a really a big thing for me, is that the work itself is unhealthy.(FG5)
She said, ‘the reason I quit [was] because they used to message me every single night asking me to look at things at nine, ten o’clock at night’. And she goes, ‘I wanted to be at home with my kids’ or just, ‘that was my downtime’.(FG2)
Self-Efficacy
I definitely think sometimes, as someone who would’ve liked to have kids at some point, I do feel like a real pressure around the fact…I’ve probably got more time to do things in my life right now… I feel quite busy as it is… I have recently gotten more back into exercising and I do it before work because I find I don’t have time during the day and I can just talk myself out of it if I have the whole day. It’s, like, five reasons by the end of the day why I shouldn’t go, and it just makes sense to go straight home and sit on the couch.(FG1)
I brought my gym to my office because I have room, my office just has three desks and I’m in the corner and I put everything over there for my exercise so that bench is not huge… And I just make myself go there every two hours and do exercise.”(FG2)
4. Discussion
4.1. Capability
4.2. Opportunity
4.3. Motivation
4.4. Strengths and Limitations
4.5. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L.; et al. Association of gestational weight gain with maternal and infant outcomes: A systematic review and meta-analysis. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Insufficient Physical Activity; Australian Government: Canberra, Australia, 2020. Available online: https://www.aihw.gov.au/reports/risk-factors/insufficient-physical-activity/contents/insufficient-physical-activity (accessed on 10 February 2021).
- Slater, K.; Rollo, M.E.; Szewczyk, Z.; Ashton, L.; Schumacher, T.; Collins, C. Do the dietary intakes of pregnant women attending public hospital antenatal clinics align with Australian guide to healthy eating recommendations? Nutrients 2020, 12, 2438. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.P.; Street, S.J.; Soan, E.J.; Mokhtar, N.; Byrne, N.M. Physical activity and development and obesity. Curr. Obes. Rep. 2013, 2, 261–266. [Google Scholar] [CrossRef]
- Harrison, C.L.; Skouteris, H.; Boyle, J.; Teede, H.J. Preventing obesity across the preconception, pregnancy and postpartum cycle: Implementing research into practice. Midwifery 2017, 52, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; Hall, J.; Skouteris, H.; Currie, S. Defining preconception: Exploring the concept of a preconception population. BMC Pregnancy Childbirth 2020, 20, 280. [Google Scholar] [CrossRef]
- Khan, N.N.; Boyle, J.A.; Lang, A.Y.; Harrison, C.L. Preconception health attitudes and behaviours of women: A qualitative investigation. Nutrients 2019, 11, 1490. [Google Scholar] [CrossRef]
- Madden, S.K.; Skouteris, H.; Bailey, C.; Hills, A.P.; Ahuja, K.D.K.; Hill, B. Women in the workplace: Promoting healthy lifestyles and mitigating weight gain during the preconception, pregnancy, and postpartum periods. Int. J. Environ. Res. Public Health 2020, 17, 3. [Google Scholar] [CrossRef]
- Dodge, R.; Daly, A.P.; Huyton, J.; Sanders, L.D. The challenge of defining wellbeing. Int. J. Wellbeing 2012, 2, 3. [Google Scholar] [CrossRef]
- Conesa Carpintero, E.; González Ramos, A.M. Accelerated researchers: Psychosocial risks in gendered institutions in academia. Front. Psychol. 2018, 9, 1077. [Google Scholar] [CrossRef]
- Madden, S.K.; Cordon, E.L.; Bailey, C.; Skouteris, H.; Ahuja, K.D.K.; Hills, A.P.; Hill, B. The effect of workplace lifestyle programmes on diet, physical activity, and weight-related outcomes for working women: A systematic review using the TIDieR checklist. Obes. Rev. 2020, 21, e13027. [Google Scholar] [CrossRef]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Richards, K.A.R.; Hemphill, M. A Practical Guide to Collaborative Qualitative Data Analysis. J. Teach. Phys. Educ. 2017, 37, 1–20. [Google Scholar] [CrossRef]
- QSR International. NVivo Qualitative Data Analysis Software X9; QSR International: Melbourne, Australia, 2010. [Google Scholar]
- Benton, M.R.; Tape, N.; Deussen, A.R.; Turnbull, D.; Dodd, J.M. Barriers to and facilitators for addressing overweight and obesity before conception: A qualitative study. Women Birth 2020. [Google Scholar] [CrossRef] [PubMed]
- Flannery, C.; McHugh, S.; Anaba, A.E.; Clifford, E.; O’Riordan, M.; Kenny, L.C.; McAuliffe, F.M.; Kearney, P.M.; Byrne, M. Enablers and barriers to physical activity in overweight and obese pregnant women: An analysis informed by the theoretical domains framework and COM-B model. BMC Pregnancy Childbirth 2018, 18, 178. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Moholdt, T.; Hawley, J.A. Maternal lifestyle interventions: Targeting preconception health. Trends Endocrinol. Metab. 2020, 31, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Townsend, N.; Wickramasinghe, K.; Williams, J.; Bhatnagar, P.; Rayney, M. Physical Activity Statistics; British Heart Foundation: London, UK, 2015; pp. 16–19. Available online: https://www.bhf.org.uk/-/media/files/publications/research/bhf_physical-activity-statistics-2015feb.pdf (accessed on 11 February 2021).
- Jenkins, K.R.; Fakhoury, N.; Marzec, M.L.; Harlow-Rosentraub, K.S. Perceptions of a culture of health: Implications for communications and programming. Health Promot. Pract. 2015, 16, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Seward, M.W.; Goldman, R.E.; Linakis, S.K.; Werth, P.; Roberto, C.A.; Block, J.P. Showers, culture, and conflict resolution: A qualitative study of employees’ perceptions of workplace wellness opportunities. J. Occup. Environ. Med. 2019, 61, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; McPhie, S.; Fuller-Tyszkiewicz, M.; Gillman, M.W.; Skouteris, H. Psychological health and lifestyle management preconception and in pregnancy. Semin. Reprod. Med. 2016, 34, 121–128. [Google Scholar] [CrossRef]
- Auspurg, K.; Hinz, T.; Sauer, C. Why should women get less? Evidence on the gender pay gap from multifactorial survey experiments. Am. Sociol. Rev. 2017, 82, 179–210. [Google Scholar] [CrossRef]
- Cole, J.A.; Tully, M.A.; Cupples, M.E. “They should stay at their desk until the work’s done”: A qualitative study examining perceptions of sedentary behaviour in a desk-based occupational setting. BMC Res. Notes 2015, 8, 683. [Google Scholar] [CrossRef]
- Gatrell, C. Putting pregnancy in its place: Conceiving pregnancy as carework in the workplace. Health Place 2011, 17, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; Skouteris, H.; Fuller-Tyszkiewicz, M. Interventions designed to limit gestational weight gain: A systematic review of theory and meta-analysis of intervention components. Obes. Rev. 2013, 14, 435–450. [Google Scholar] [CrossRef] [PubMed]
- Thangaratinam, S.; Rogozińska, E.; Jolly, K.; Glinkowski, S.; Duda, W.; Borowiack, E.; Roseboom, T.; Tomlinson, J.; Walczak, J.; Kunz, R.; et al. Interventions to reduce or prevent obesity in pregnant women: A systematic review. Health Technol. Assess. 2012, 16, 1–191. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; McPhie, S.; Moran, L.J.; Harrison, P.; Huang, T.T.; Teede, H.; Skouteris, H. Lifestyle intervention to prevent obesity during pregnancy: Implications and recommendations for research and implementation. Midwifery 2017, 49, 13–18. [Google Scholar] [CrossRef]
- Hill, B.; Ling, M.; Mishra, G.; Moran, L.J.; Teede, H.J.; Bruce, L.; Skouteris, H. Lifestyle and psychological factors associated with pregnancy intentions: Findings from a longitudinal cohort study of Australian women. Int. J. Environ. Res. Public Health 2019, 16, 24. [Google Scholar] [CrossRef]
- Nkrumah, I.; North, M.; Kothe, E.; Chai, T.L.; Pirotta, S.; Lim, S.; Hill, B. The relationship between pregnancy intentions and diet or physical activity behaviors in the preconception and antenatal periods: A systematic review and meta-analysis. J. Midwifery Womens Health 2020, 65, 660–680. [Google Scholar] [CrossRef]

| Variable | Participants |
|---|---|
| Age, mean (range), years | 44.1 (27–62) |
| Children, n (%) | |
| Yes | 16 (64) |
| No | 9 (36) |
| Number of children | |
| Mean (range) | 1.3 (0–4) |
| Median | 2 |
| Workplace role, n (%) | |
| Professional * | 14 (56) |
| Academic | 9 (36) |
| Other | 2 (8) |
| Employment fraction, n (%) | |
| Full time | 16 (64) |
| Part time | 9 (36) |
| Employment status, n (%) | |
| Continuing † | 11 (44) |
| Fixed term ‡ | 5 (20) |
| Casual § | 2 (8) |
| Not stated | 7 (28) |
| Work Location, n (%) | |
| Hobart Area (Focus Groups 1–3) | 13 (52) |
| Launceston Area (Focus Groups 4–5) | 12 (48) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madden, S.K.; Blewitt, C.A.; Ahuja, K.D.K.; Skouteris, H.; Bailey, C.M.; Hills, A.P.; Hill, B. Workplace Healthy Lifestyle Determinants and Wellbeing Needs across the Preconception and Pregnancy Periods: A Qualitative Study Informed by the COM-B Model. Int. J. Environ. Res. Public Health 2021, 18, 4154. https://doi.org/10.3390/ijerph18084154
Madden SK, Blewitt CA, Ahuja KDK, Skouteris H, Bailey CM, Hills AP, Hill B. Workplace Healthy Lifestyle Determinants and Wellbeing Needs across the Preconception and Pregnancy Periods: A Qualitative Study Informed by the COM-B Model. International Journal of Environmental Research and Public Health. 2021; 18(8):4154. https://doi.org/10.3390/ijerph18084154
Chicago/Turabian StyleMadden, Seonad K., Claire A. Blewitt, Kiran D. K. Ahuja, Helen Skouteris, Cate M. Bailey, Andrew P. Hills, and Briony Hill. 2021. "Workplace Healthy Lifestyle Determinants and Wellbeing Needs across the Preconception and Pregnancy Periods: A Qualitative Study Informed by the COM-B Model" International Journal of Environmental Research and Public Health 18, no. 8: 4154. https://doi.org/10.3390/ijerph18084154
APA StyleMadden, S. K., Blewitt, C. A., Ahuja, K. D. K., Skouteris, H., Bailey, C. M., Hills, A. P., & Hill, B. (2021). Workplace Healthy Lifestyle Determinants and Wellbeing Needs across the Preconception and Pregnancy Periods: A Qualitative Study Informed by the COM-B Model. International Journal of Environmental Research and Public Health, 18(8), 4154. https://doi.org/10.3390/ijerph18084154








