The Incidence and Nature of Claims against Dentists Related to Periodontal Treatment in Israel during the Years 2005–2019
Abstract
1. Introduction
2. Materials and Methods
- Claims related to diagnosis, management, and outcomes of periodontal disease according to the MCI registry.
- Files including full relevant data: gender and age of the patient, date of the complaint, treatment setting (private, public, or corporate clinic), a detailed description of the adverse event, nature of allegations, clinical outcome of injury, outcome of claim, and payment amounts.
- Demographics: data were compared between female and male patients and between age groups (≤/>35 years at presentation).
- The main reasons for the claims: this was further divided into subgroups:
- (a)
- The management of periodontal disease by periodontists: this included, injuries during periodontal therapy including neural damage, tooth/teeth loss, root resorption, patients’ disappointment of the esthetic outcomes (recession aggravation, enlargement of interdental embrasure), thermal hypersensitivity, increased tooth/teeth mobility, and needs for re-treatment.
- (b)
- Secondary periodontal complications occurring during non-periodontal treatment, such as prosthetic rehabilitation, implant therapy, tooth extraction, orthodontic, restorative, endodontic, pedodontic, or any other type of dental/oral treatment. This parameter was further classified according to the exact reason for the claim: delayed or false diagnosis, delay in treatment, needs for further treatment due to lack of disease, diagnosis and complications following the treatment (neural damage, esthetic damage, distress and pain, tooth/teeth loss and needs for additional treatment).
- (c)
- Documentation/information: lack of relevant information regarding the treatment performed and possible complications and lack of a detailed informed consent.
- The clinical setting where treatment was provided:
- (a)
- private dental practices (PDC)
- (b)
- public dental practices (PDP)
- (c)
- corporations (private dental clinics registered under one juristic entity).
- Litigation outcome:
- (a)
- compromise out of court between insurance company and claimant
- (b)
- mediation—in court compromise
- (c)
- rejection—rejection of the malpractice claim by the insurance company without any further litigation
- (d)
- cancellation—claim cancellation by the court
- (e)
- court adjudicated—in court verdict
- (f)
- insurance rejection—rejection of the claim as the treatment was not performed during insurance policy period
- (g)
- accepted arbitration at the Israeli Dental Association Court
- (h)
- file closed without compensation—the court litigation decision was that the claimant is not entitled to any compensation.
3. Statistics
4. Results
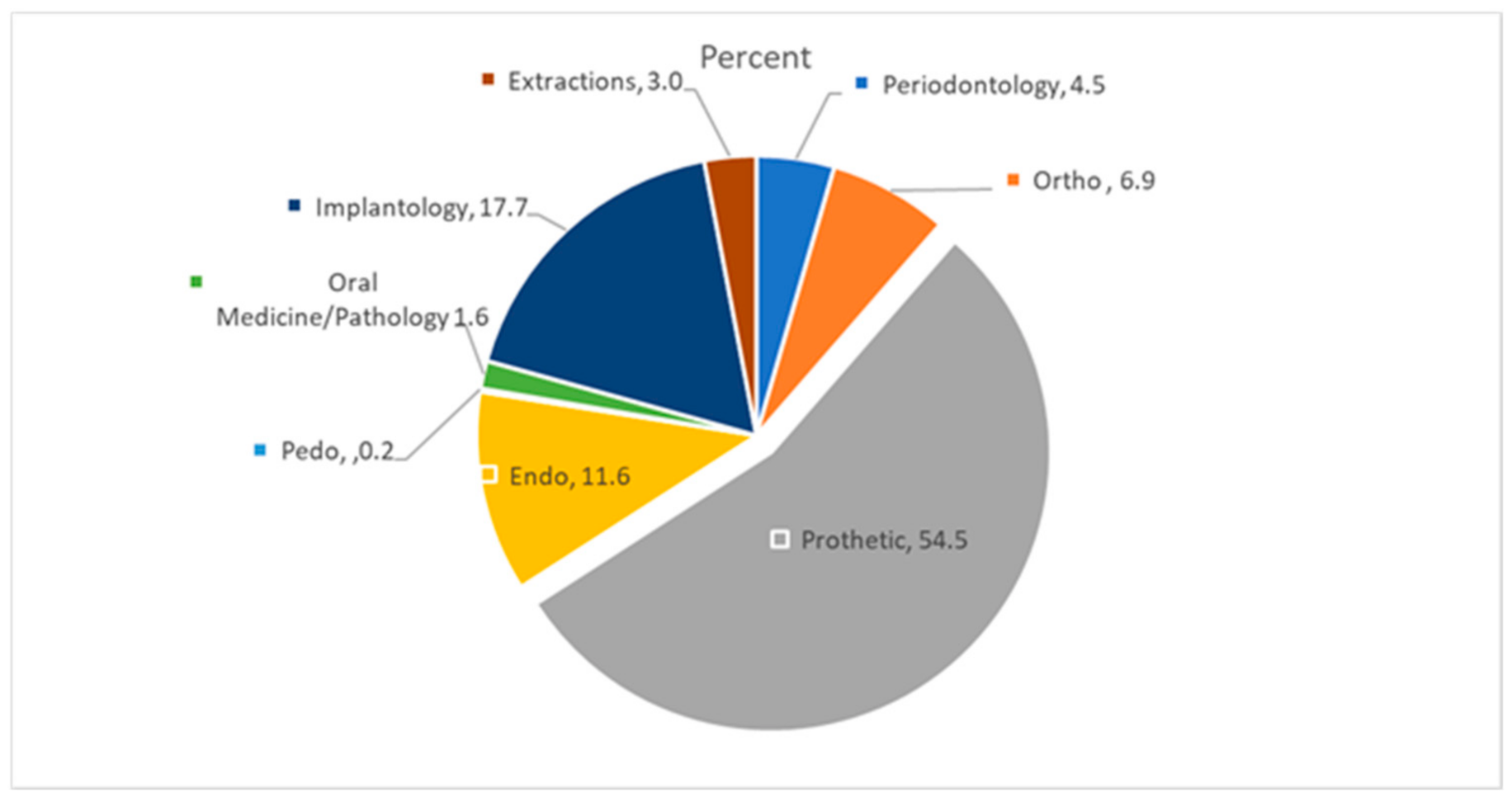
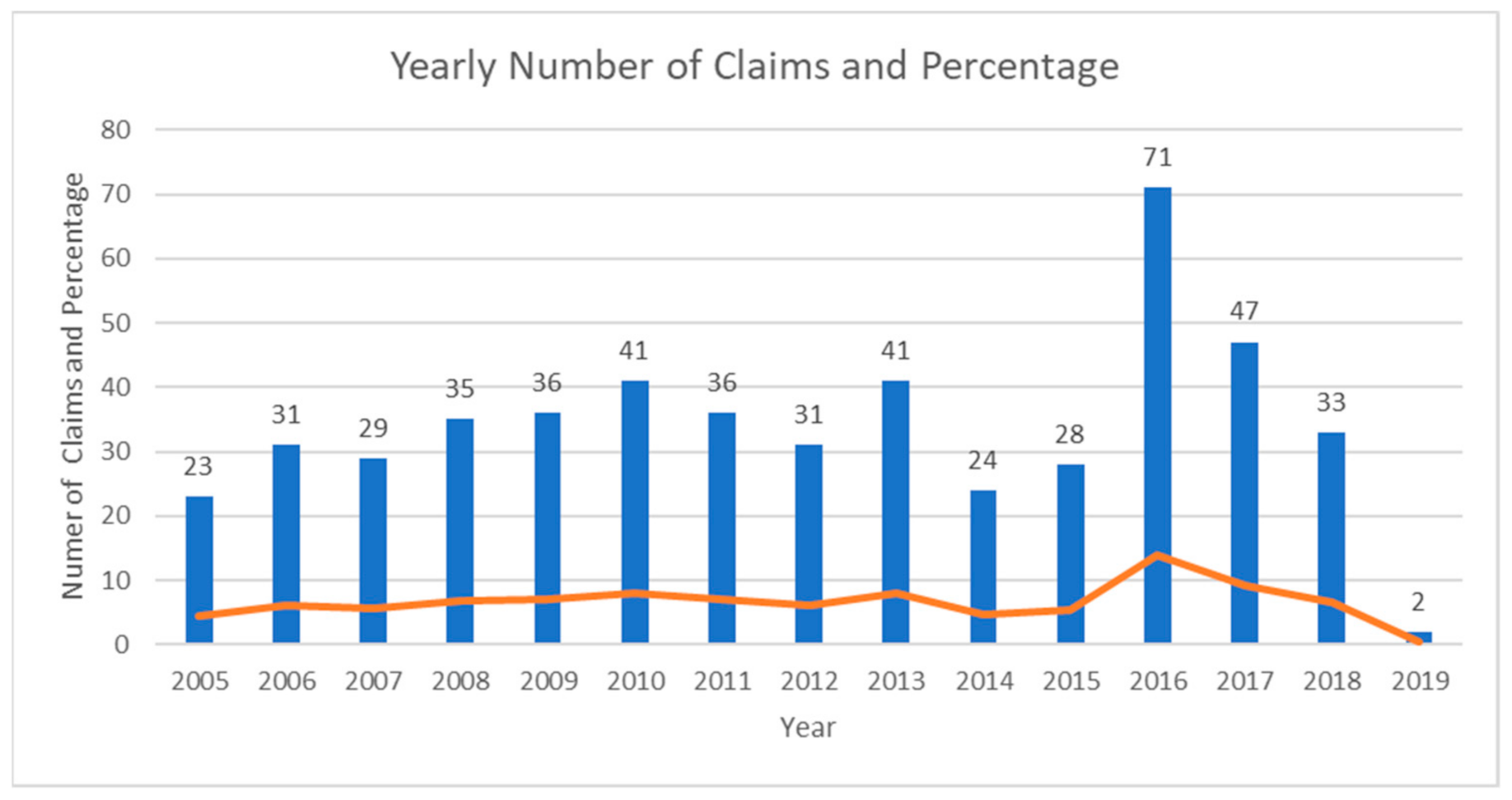
4.1. The Purpose of the Claim as a Function of the Primary Treatment Performed
4.2. Allegation Nature by General Category
4.3. Claims According to the Treatment Performed
5. Discussion
6. Conclusions
- Practitioners should dedicate a significant part of the total treatment time to preoperative diagnosis and planning. Treatment plans should be outlined in writing and be detailed. The dentist must inform the patient of the risks and benefits of the proposed treatment, the consequences of declining treatment, and the available treatment options. Alternative treatment plans should be discussed with the patient and documented. It is inevitable that, if a dentist carries out dental treatment without the consent of the patient, he/she will face the consequences.
- It is preferable to develop a full cause-related therapy and maintenance program. A skilled dentist is supposed to carry out an optimal treatment plan with minimal changes in most clinical situations (and potential changes must be acknowledged).
- All documents should be signed and retained, including treatment-specific informed consent (sinus augmentation, bone augmentation, immediate placement, etc.) and financial agreement to undergo the treatment plan.
- The main causes for lawsuits are actual body injury and major disappointment with the results of the therapy. The combination of proper operative skills and a good doctor–patient relationship will reduce the number of legal claims.
- Periodontal consultation before dental treatment may reduce malpractice risks, adverse events, and un-necessary changes of the treatment plan. The most common issues of claims were related to primary “non-periodontal patients” meaning that dental treatment was supplied while ignoring the under/delayed treating of the periodontal disease. Once established, it should be clearly presented to the patient, including the risks and benefits, alternative treatment options, and possible complications.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Givol, N.; Frenkel, T.; Tickotsky, N.; Moskovitz, M. The incidence and nature of complaints against dentists for the treatment of children in Israel from 1992–2011. Community Dent. Health 2015, 32, 56–59. [Google Scholar] [CrossRef] [PubMed]
- Thomas, L.A.; Tibble, H.; Too, L.S.; Hopcraft, M.S.; Bismark, M.M. Complaints about dental practitioners: An analysis of 6 years of complaints about dentists, dental prosthetists, oral health therapists, dental therapists and dental hygienists in Australia. Aust. Dent. J. 2018, 63, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Karhunen, S.; Virtanena, J.I. Dental treatment injuries in the Finnish Patient Insurance Centre in 2000–2011. Acta Odontol. Scand. 2016, 74, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Givol, N.; Taicher, S.; Halamish-Shani, T.; Chaushu, G. Risk management aspects of implant dentistry. Int. J. Oral Maxillofac. Implant. 2002, 17, 258–262. [Google Scholar]
- Kiani, M.; Sheikhazadi, A. A five-year survey for dental malpractice claims in Tehran, Iran. J. Forensic Leg. Med. 2010, 16, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Pinchi, V.; Varvara, G.; Pradella, F.; Focardi, M.; Domati, M.D.; Norelli, G. Analysis of professional malpractice claims in implant dentistry in Italy from insurance company technical reports, 2006 to 2010. Int. J. Oral Maxillofac. Implant. 2014, 29, 1177–1184. [Google Scholar] [CrossRef][Green Version]
- Pinchi, V.; Pradella, F.; Gasparetto, L.; Norelli, G.A. Trends in endodontic claims in Italy. Int. Dent. J. 2013, 63, 43–48. [Google Scholar] [CrossRef]
- Eke, P.I.; Borgnakke, W.S.; Genco, R.J. Recent epidemiologic trends in periodontitis in the USA. Periodontology 2000 2020, 82, 257–267. [Google Scholar] [CrossRef]
- Lindhe, J.; Lang, N.P.; Karring, T. Clinical Periodontology and Implant Dentistry, 6th ed.; Blackwell Munksgaard: Oxford, UK, 2008. [Google Scholar]
- Hapcook, C.P. Dental malpractice claims: Percentages and procedures. J. Am. Dent. Assoc. 2006, 137, 1444–1445. [Google Scholar] [CrossRef]
- Mann, J. Dental and Oral Health in Israel Objectives 2020- Report of the Israeli Ministry of Health- Heb. Available online: https://www.health.gov.il/publicationsfiles/2020_18052016.pdf (accessed on 1 June 2016).
- Sgan-Cohen, H.D.; Donchin, M.; Goultschin, J.; Soskolne, A.; Brayer, L. Periodontal treatment needs, by CPITN, among employees of a Jerusalem hospital. Int. Dent. J. 1992, 42, 92–96. [Google Scholar]
- Abu Wasel, M.; Tagger Green, N.; Saminsky, M.; Barnea, E.; Mijiritsky, M.; Kolerman, R. The incidence and nature of claims against dentists for dental implant treatment in Israel during the years 2005–2015. Int. J. Oral Implantol. 2021, 14, 57–66. [Google Scholar]
- Manca, R.; Bruti, V.; Napoletano, S.; Marinelli, E. A 15 years survey for dental malpractice claims in Rome, Italy. Forensic Leg. Med. 2018, 58, 74–77. [Google Scholar] [CrossRef]
- Perea-Pérez, B.; Labajo-González, E.; Santiago-Sáez, A.; Albarrán-Juan, E.; Villa-Vigil, A. Analysis of 415 adverse events in dental practice in Spain from 2000 to 2010. Med. Oral Patol. Oral y Cir. Bucal 2014, 19, e500-5. [Google Scholar] [CrossRef]
- Zanin, A.A.; Herrera, L.M.; Melani, R.F. Civil liability: Characterization of the demand for lawsuits against dentists. Braz. Oral Res. 2016, 30, e91. [Google Scholar] [CrossRef]
- Bjørndal, L.; Reit, C. Endodontic malpractice claims in Denmark 1995–2004. Int. Endod. J. 2008, 41, 1059–1065. [Google Scholar] [CrossRef]
- Gulati, A.; Herd, M.K.; Nimako, M.; Anand, R.; Brennan, P.A. Litigation in National Health Service oral and maxillofacial surgery: Review of the last 15 years. Br. J. Oral Maxillofac. Surg. 2012, 50, 385–388. [Google Scholar] [CrossRef]
- Figgener, L.; Kleinheinz, J. Implant dentistry at the focus of liability lawsuits. Int. J. Oral Maxillofac. Implant. 2004, 19, 382–387. [Google Scholar] [CrossRef]
- Pukk, K.; Lundberg, J.; Penaloza-Pesantes, R.V.; Brommels, M.; Gaffney, F.A. Do women simply complain more? National patient injury claims data show gender and age differences. Qual. Manag. Health Care 2003, 12, 225–231. [Google Scholar] [CrossRef]
- Givol, N.; Taicher, S.; Halamish-Shani, T.; Chaushu, G. Medicolegal aspects of altered sensation following implant placement in the mandible. Int. J. Oral Maxillofac. Implant. 2002, 17, 413–415. [Google Scholar]
- Castro, A.C.C.; Franco, A.; Silva, R.F.; Portilho, C.D.M.; Oliveira, H.C.M. Prevalence and content of legal suits founded on dental malpractice in the courts of Midwest Brazil. Rev. Bras. Odontol. Leg. 2015, 2, 46–52. [Google Scholar] [CrossRef][Green Version]
- Ji, Y.D.; Peacock, Z.S.; Resnick, C.M. Characteristics of National Malpractice Claims in Oral and Maxillofacial Surgery. J. Oral Maxillofac. Surg. 2020, 78, 1314–1318. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lyons, K.M. Interdisciplinary interface between fixed prosthodontics and periodontics. Periodontology 2000 2017, 74, 40–62. [Google Scholar] [CrossRef] [PubMed]
- Nassani, M.Z. Aspects of Malpractice in Prosthodontics. J. Prosthodont. 2017, 26, 672–681. [Google Scholar] [CrossRef]
- Smith, M.M.; Knight, E.T.; Al-Harthi, L.; Leichter, J.W. Chronic periodontitis and implant dentistry. Periodontology 2000 2017, 74, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Rotstein, I. Interaction between endodontics and periodontics. Periodontology 2000 2017, 74, 11–39. [Google Scholar] [CrossRef]
- Givol, N.; Rosen, E.; Taicher, S.; Tsesis, I. Risk management in endodontics. J. Endod. 2010, 36, 982–984. [Google Scholar] [CrossRef]
- Antoun, J.S.; Mei, L.; Gibbs, K.; Farella, M. Effect of orthodontic treatment on the periodontal tissues. Periodontology 2000 2017, 74, 140–157. [Google Scholar] [CrossRef]
- Rich, A.M.; Seo, B.; Parachuru, V.; Hussaini, H.M. The nexus between periodontics and oral pathology. Periodontology 2000 2017, 74, 176–181. [Google Scholar] [CrossRef]
- Abu Ell Naaj, I.; Trost, O.; Tagger Green, N.; Trouilloud, P.; Robe, N.; Malka, G.; Peled, M. Peri-Implantitis or Squamous Cell Carcinoma. Rev. Stomatol. Chir. Maxillofac. 2007, 108, 458–460. [Google Scholar]
- Vasak, C.; Fiederer, R.; Watzek, G. Current state of training for implant dentistry in Europe: A questionnaire-based survey. Clin. Oral Implant. Res. 2007, 18, 18–20. [Google Scholar] [CrossRef]
- Wiebe, C.B.; Putnins, E.E. The periodontal disease classification system of the American Academy of Periodontology—An update. J. Can. Dent. Assoc. 2000, 66, 594–597. [Google Scholar]
- Lyons, K.M.; Darby, I. Interdisciplinary periodontics: The multidisciplinary approach to the planning and treatment of complex cases. Periodontology 2000 2017, 74, 7–10. [Google Scholar] [CrossRef]
| Variable | n | % | |
|---|---|---|---|
| Gender | Male | 186 | 36.6% |
| Female | 322 | 63.4% | |
| Age | >35 | 362 | 71.3% |
| ≤35 | 146 | 28.7% | |
| Sector | Private | 276 | 54.3% |
| Public | 198 | 39.0% | |
| Corporates | 34 | 6.7% | |
| Litigation status | Compensation by compromise | 421 | 82.8% |
| Compensation by court mediation | 37 | 7.3% | |
| Court adjudicated compensation | 5 | 1.0% | |
| Rejection | 17 | 3.4% | |
| Cancellation | 27 | 5.3% | |
| No compensation | 1 | 0.2% | |
| Total | 508 |
| Non-Periodontal Treatment | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n, (% of Total) | Gender, n (%) | Age (Years), n (%) | Treatment Settings, n (%) | Year of Claim, n (%) | ||||||||
| F | M | ρ | ≤35 | >35 | ρ | Private | Public | ρ | ≤2011 | >2011 | p | |
| Periodontal deterioration in another treatment 485 (95.5) | 307 (95.3) | 178 (95.7) | 1.000 | 138 (94.5) | 347 (95.9) | 0.488 | 265 (96.0) | 220 (94.8) | 0.530 | 221 (95.7) | 264 (95.3) | 0.879 |
| Aggravation of periodontitis 423 (83.3) | 148 (79.6) | 275 (85.4) | 0.09 | 109 (74.7) | 314 (86.7) | 0.002 | 240 (87.0) | 183 (78.9) | 0.017 | 187 (81.0) | 236 (85.2) | 0.233 |
| Over-treatment 90 (15.1) | 35 (18.8) | 55 (17.1) | 0.621 | 17 (11.6) | 73 (20.2) | 0.028 | 46 (16.7) | 44 (19) | 0.56 | 32 (13.9) | 58 (20.9) | 0.005 |
| Delay of Treatment 106 (11.2) | 62 (19.3) | 44 (23.7) | 0.240 | 43 (28.5) | 63 (17.4) | 0.004 | 51 (18.5) | 55 (23.7) | 0.149 | 42 (18.2) | 64 (23.1) | 0.189 |
| Delay of Diagnosis 60 (8) | 43 (13.4) | 17 (9.1) | 0.156 | 40 (27.4) | 20 (5.5) | <0.001 | 23 (8.3) | 37 (15.9) | 0.009 | 25 (10.8) | 35 (12.6) | 0.528 |
| False Diagnosis 27 (5.3) | 18 (5.6) | 9 (4.8) | 0.716 | 16 (5.1%) | 11 (5.6%) | 0.490 | 9 (3.3) | 18 (7.8) | 0.029 | 14 (6.1) | 13 (4.7) | 0.054 |
| Periodontal treatment by periodontists | ||||||||||||
| Periodontal surgery results 23 (4.5) | 16 (5) | 7 (3.8) | 0.529 | 3 (2.1) | 20 (5.5) | 0.102 | 13 (4.7) | 10 (4.3) | 1.000 | 7 (3.0) | 16 (5.8) | 0.198 |
| documentation/information | ||||||||||||
| Violation of autonomy 239 (47.0) | 87 (46.8) | 152 (47.2) | 0.925 | 57 (39) | 182 (50.3) | 0.024 | 142 (51.4) | 97 (41.8) | 0.032 | 52 (22.5) | 187 (67.5) | 0.005 |
| Change in Treatment plan 12 (1.8) | 6 (1.9) | 6 (3.2) | 0.330 | 0 (0) | 12 (3.3) | 0.023 | 6 (2.2) | 6 (2.6) | 0.778 | 4 (1.7) | 8 (2.9) | 0.560 |
| Clinical Outcomes of Allegations n (%) | Gender, n (%) | Age (Years), n (%) | Treatment Settings, n (%) | Year of Claim, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | ρ | ≤35 | >35 | ρ | Private | Public | ρ | ≤2011 | >2011 | ρ | |
| Distress and pain 431 (84.8%) | 158 (84.9%) | 273 (84.8%) | 0.96 | 117 (80.1%) | 314 (100%) | 0.075 | 256 (92.8%) | 175 (75.4%) | <0.001 | 186 (80.5%) | 245 (88.4) | 0.018 |
| Tooth damage or loss 397 (78.1%) | 154 (82.85) | 243 (75.5%) | 0.054 | 107 (73.35%) | 290 (80.1%) | 0.098 | 212 (76.8%) | 185 (79.7%) | 0.452 | 186 (80.5%) | 211 (76.2%) | 0.218 |
| Re-Surgery 145 (28.5%) | 61 (32.8%) | 84 (26.1%) | 0.107 | 39 (26.7%) | 106 (29.3%) | 0.589 | 84 (30.4%) | 61 (26.3%) | 0.325 | 64 (27.7%) | 81 (29.2%) | 0.767 |
| Disappointment of the esthetic outcomes 114 (22.4%) | 30 (16.1%) | 84 (26.2%) | 0.009 | 37 (25.5%) | 77 (21.3%) | 0.346 | 67 (24.4%) | 47 (20.3%) | 0.287 | 49 (21.3%) | 65 (23.5%) | 0.594 |
| Neural Damage 21 (4.1%) | 8 (4.3%) | 13 (4%) | 0.886 | 3 (2.1%) | 18 (5%) | 0.216 | 18 (6.5%) | 3 (1.3%) | 0.003 | 2 (0.9%) | 19 (6.9%) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nassar, D.; Tagger-Green, N.; Tal, H.; Nemcovsky, C.; Mijiritsky, E.; Beitlitum, I.; Barnea, E.; Kolerman, R. The Incidence and Nature of Claims against Dentists Related to Periodontal Treatment in Israel during the Years 2005–2019. Int. J. Environ. Res. Public Health 2021, 18, 4153. https://doi.org/10.3390/ijerph18084153
Nassar D, Tagger-Green N, Tal H, Nemcovsky C, Mijiritsky E, Beitlitum I, Barnea E, Kolerman R. The Incidence and Nature of Claims against Dentists Related to Periodontal Treatment in Israel during the Years 2005–2019. International Journal of Environmental Research and Public Health. 2021; 18(8):4153. https://doi.org/10.3390/ijerph18084153
Chicago/Turabian StyleNassar, Dima, Nirit Tagger-Green, Haim Tal, Carlos Nemcovsky, Eitan Mijiritsky, Ilan Beitlitum, Eitan Barnea, and Roni Kolerman. 2021. "The Incidence and Nature of Claims against Dentists Related to Periodontal Treatment in Israel during the Years 2005–2019" International Journal of Environmental Research and Public Health 18, no. 8: 4153. https://doi.org/10.3390/ijerph18084153
APA StyleNassar, D., Tagger-Green, N., Tal, H., Nemcovsky, C., Mijiritsky, E., Beitlitum, I., Barnea, E., & Kolerman, R. (2021). The Incidence and Nature of Claims against Dentists Related to Periodontal Treatment in Israel during the Years 2005–2019. International Journal of Environmental Research and Public Health, 18(8), 4153. https://doi.org/10.3390/ijerph18084153








