Mother’s Own Milk Feeding in Preterm Newborns Admitted to the Neonatal Intensive Care Unit or Special-Care Nursery: Obstacles, Interventions, Risk Calculation
Abstract
1. Introduction
2. Modifiable Risk Factors for NMOM Feeding at Discharge
2.1. Skin-to-Skin Contact in the Delivery Room and the NICU
2.2. Strategies of Infant Feeding and Milk Expression
2.3. Mode of Delivery
3. Unmodifiable Risk Factors for NMOM Feeding at Discharge
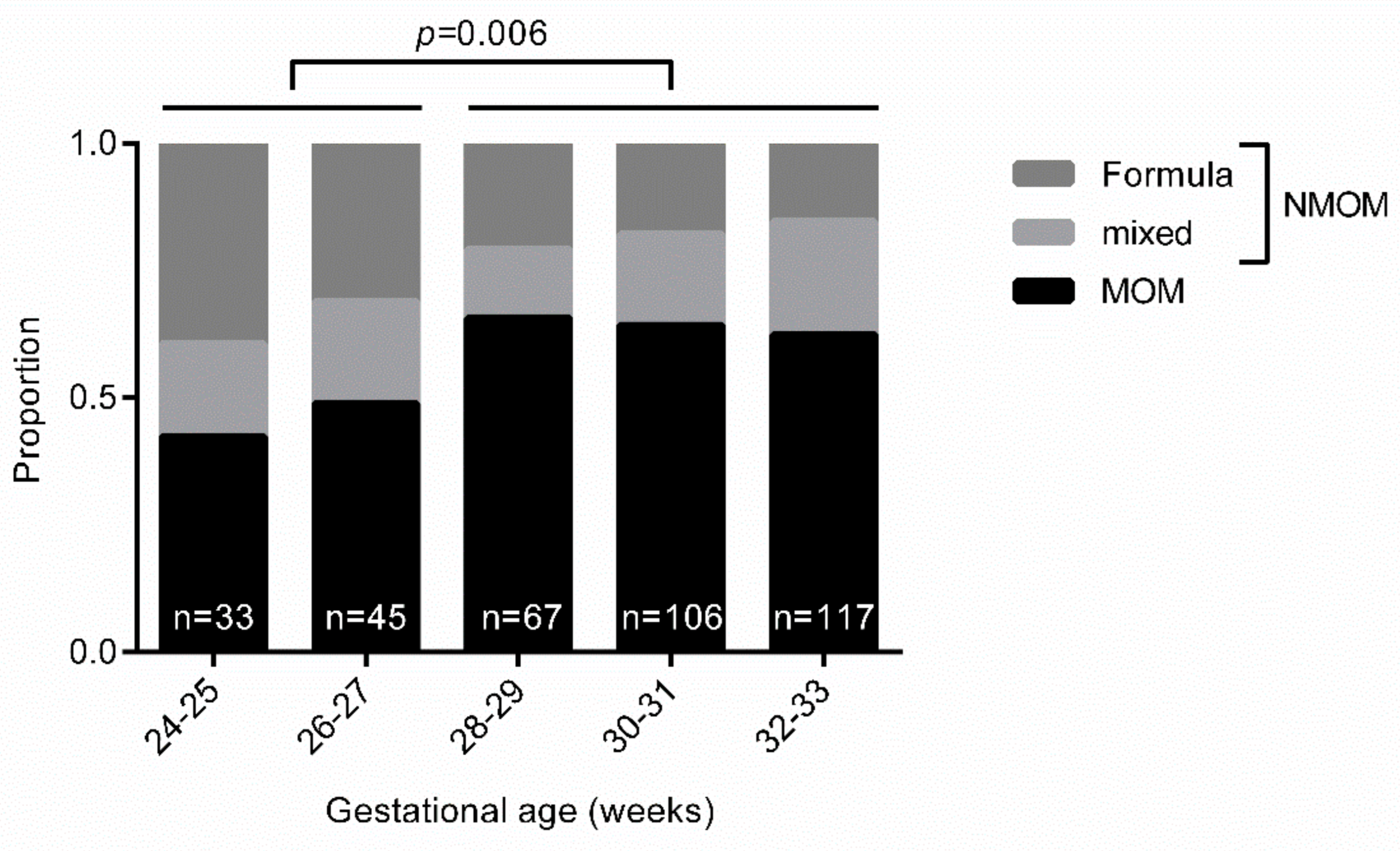
3.1. Demographical Risk Factors of the Infant
3.2. Demographical Risk Factors of the Mother
3.3. Health and Disease-Related Risk Factors of the Infant
3.4. Health and Disease-Related Risk Factors of the Mother
3.5. Maternal Experiences with Milk Expression
4. Identifying Mother–Baby Dyads at Risk of NMOM Feeding at Discharge
5. Checklist for Quality-Improvement Projects to Increase MOM Feeding at Discharge
- Is MOM feeding at discharge seen as an important outcome parameter?
- Is skin-to-skin care in the delivery room facilitated?
- Is skin-to-skin care in the NICU possible during the first days of life, especially in the first week of life?
- Is breast-milk expression started within 6 h after delivery?
- Do parents receive information on breastfeeding/breast-milk expression antenatally?
- Is the amount of pumped breast milk discussed at daily rounds?
- Are targeted interventions available for infants at risk, such as after abdominal surgery or below 28 weeks gestational age?
- Are targeted interventions available for mothers at risk, such as with nicotine use or gestational diabetes?
- Are targeted interventions available for mothers not achieving 500 mL per day of pumped breast milk at day 14 postpartum?
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Statistics
References
- Schanler, R.J.; Shulman, R.J.; Lau, C. Feeding strategies for premature infants: Beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics 1999, 103, 1150–1157. [Google Scholar] [CrossRef] [PubMed]
- Furman, L.; Taylor, G.; Minich, N.; Hack, M. The effect of maternal milk on neonatal morbidity of very low-birth-weight infants. Arch. Pediatr. Adolesc. Med. 2003, 157, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, P.; Stolfi, I.; Pedicino, R.; Vagnarelli, F.; Mosca, F.; Pugni, L.; Bollani, L.; Pozzi, M.; Gomez, K.; Tzialla, C.; et al. Human milk feeding prevents retinopathy of prematurity (ROP) in preterm VLBW neonates. Early Hum. Dev. 2013, 89, S64–S68. [Google Scholar] [CrossRef]
- Spiegler, J.; Preuß, M.; Gebauer, C.; Bendiks, M.; Herting, E.; Göpel, W.; Berghäuser, M.A.; Böckenholt, K.; Bohnhorst, B.; Böttger, R.; et al. Does Breastmilk Influence the Development of Bronchopulmonary Dysplasia? J. Pediatr. 2016, 169, 76–80.e4. [Google Scholar] [CrossRef]
- Schanler, R.J. Outcomes of Human Milk-Fed Premature Infants. Semin. Perinatol. 2011, 35, 29–33. [Google Scholar] [CrossRef]
- Rozé, J.C.; Darmaun, D.; Boquien, C.Y.; Flamant, C.; Picaud, J.C.; Savagner, C.; Claris, O.; Lapillonne, A.; Mitanchez, D.; Branger, B.; et al. The apparent breastfeeding paradox in very preterm infants: Relationship between breast feeding, early weight gain and neurodevelopment based on results from two cohorts, EPIPAGE and LIFT. BMJ Open 2012, 2. [Google Scholar] [CrossRef]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatr. Int. J. Paediatr. 2015, 104, 96–113. [Google Scholar] [CrossRef]
- Chua, S.; Arulkumaran, S.; Lim, I.; Selamat, N.; Ratnam, S.S. Influence of breastfeeding and nipple stimulation on postpartum uterine activity. BJOG An Int. J. Obstet. Gynaecol. 1994, 101, 804–805. [Google Scholar] [CrossRef]
- Johnson, T.J.; Patel, A.L.; Bigger, H.R.; Engstrom, J.L.; Meier, P.P. Economic Benefits and Costs of Human Milk Feedings: A Strategy to Reduce the Risk of Prematurity-Related Morbidities in Very-Low-Birth-Weight Infants. Adv. Nutr. 2014, 5, 207–212. [Google Scholar] [CrossRef]
- Eidelman, A.I.; Schanler, R.J. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar]
- Mitha, A.; Piedvache, A.; Glorieux, I.; Zeitlin, J.; Roué, J.M.; Blondel, B.; Durox, M.; Burguet, A.; Kaminski, M.; Ancel, P.Y.; et al. Unit policies and breast milk feeding at discharge of very preterm infants: The EPIPAGE-2 cohort study. Paediatr. Perinat. Epidemiol. 2019, 33, 59–69. [Google Scholar] [CrossRef]
- Wilson, E.; Edstedt Bonamy, A.-K.; Bonet, M.; Toome, L.; Rodrigues, C.; Howell, E.A.; Cuttini, M.; Zeitlin, J. Room for improvement in breast milk feeding after very preterm birth in Europe: Results from the EPICE cohort. Matern. Child Nutr. 2018, 14, e12485. [Google Scholar] [CrossRef]
- Oras, P.; Thernström Blomqvist, Y.; Hedberg Nyqvist, K.; Gradin, M.; Rubertsson, C.; Hellström-Westas, L.; Funkquist, E.L. Skin-to-skin contact is associated with earlier breastfeeding attainment in preterm infants. Acta Paediatr. Int. J. Paediatr. 2016, 105, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Tully, K.P.; Holditch-Davis, D.; White-Traut, R.C.; David, R.; O’Shea, T.M.; Geraldo, V. A Test of Kangaroo Care on Preterm Infant Breastfeeding. J. Obstet. Gynecol. Neonatal Nurs. JOGNN 2016, 45, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, A.G.; Yehualashet, S.S.; Bayleyegn, A.D. The effects of kangaroo mother care on the time to breastfeeding initiation among preterm and LBW infants: A meta-analysis of published studies. Int. Breastfeed. J. 2019, 14. [Google Scholar] [CrossRef]
- Maastrup, R.; Hansen, B.M.; Kronborg, H.; Bojesen, S.N.; Hallum, K.; Frandsen, A.; Kyhnaeb, A.; Svarer, I.; Hallström, I. Factors associated with exclusive breastfeeding of preterm infants. Results from a prospective national cohort study. PLoS ONE 2014, 9, e89077. [Google Scholar] [CrossRef] [PubMed]
- Pierrat, V.; Coquelin, A.; Cuttini, M.; Khoshnood, B.; Glorieux, I.; Claris, O.; Durox, M.; Kaminski, M.; Ancel, P.-Y.; Arnaud, C. Translating Neurodevelopmental Care Policies into Practice. Pediatr. Crit. Care Med. 2016, 17, 957–967. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.S.; Chalmers, B.; Hodnett, E.D.; Sevkovskaya, Z.; Dzikovich, I.; Shapiro, S.; Collet, J.P.; Vanilovich, I.; Mezen, I.; Ducruet, T.; et al. Promotion of breastfeeding intervation trial (PROBIT): A randomized trial in the Republic of Belarus. J. Am. Med. Assoc. 2001, 285, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Maastrup, R.; Walloee, S.; Kronborg, H. Nipple shield use in preterm infants: Prevalence, motives for use and association with exclusive breastfeeding—Results from a national cohort study. PLoS ONE 2019, 14, e0222811. [Google Scholar] [CrossRef]
- Davanzo, R.; Monasta, L.; Ronfani, L.; Brovedani, P.; Demarini, S. Breastfeeding at NICU Discharge. J. Hum. Lact. 2013, 29, 374–380. [Google Scholar] [CrossRef]
- Pineda, R.G. Predictors of Breastfeeding and Breastmilk Feeding Among Very Low Birth Weight Infants. Breastfeed. Med. 2011, 6, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Zachariassen, G.; Faerk, J.; Grytter, C.; Esberg, B.; Juvonen, P.; Halken, S. Factors associated with successful establishment of breastfeeding in very preterm infants. Acta Paediatr. 2010, 99, 1000–1004. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, C.; Blondel, B.; Piedvache, A.; Wilson, E.; Bonamy, A.K.E.; Gortner, L.; Rodrigues, C.; van Heijst, A.; Draper, E.S.; Cuttini, M.; et al. Low breastfeeding continuation to 6 months for very preterm infants: A European multiregional cohort study. Matern. Child Nutr. 2019, 15, e12657. [Google Scholar] [CrossRef]
- Casey, L.; Fucile, S.; Dow, K.E. Determinants of Successful Direct Breastfeeding at Hospital Discharge in High-Risk Premature Infants. Breastfeed. Med. 2018, 13, 346–351. [Google Scholar] [CrossRef]
- Bonet, M.; Blondel, B.; Agostino, R.; Combier, E.; Maier, R.F.; Cuttini, M.; Khoshnood, B.; Zeitlin, J. Variations in breastfeeding rates for very preterm infants between regions and neonatal units in Europe: Results from the MOSAIC cohort. Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F450–F452. [Google Scholar] [CrossRef] [PubMed]
- Darfour-Oduro, S.A.; Kim, J. WIC Mothers’ Social Environment and Postpartum Health on Breastfeeding Initiation and Duration. Breastfeed. Med. 2014, 9, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Lussier, M.M.; Tosi, L.; Brownell, E.A. Predictors of Mother’s Own Milk Feeding at Discharge in Preterm Infants. Adv. Neonatal Care 2019, 19, 468–473. [Google Scholar] [CrossRef]
- Flacking, R.; Nyqvist, K.H.; Ewald, U. Effects of socioeconomic status on breastfeeding duration in mothers of preterm and term infants. Eur. J. Public Health 2007, 17, 579–584. [Google Scholar] [CrossRef]
- Kirchner, L.; Jeitler, V.; Waldhör, T.; Pollak, A.; Wald, M. Long hospitalization is the most important risk factor for early weaning from breast milk in premature babies. Acta Paediatr. 2009, 98, 981–984. [Google Scholar] [CrossRef]
- Ratner, P.A.; Johnson, J.L.; Bottorff, J.L. Smoking Relapse and Early Weaning Among Postpartum Women: Is There an Association? Birth 1999, 26, 76–82. [Google Scholar] [CrossRef]
- Haile, Z.T.; Oza-Frank, R.; Azulay Chertok, I.R.; Passen, N. Association between History of Gestational Diabetes and Exclusive Breastfeeding at Hospital Discharge. J. Hum. Lact. 2016, 32, NP36–NP43. [Google Scholar] [CrossRef] [PubMed]
- Hauff, L.E.; Demerath, E.W. Body image concerns and reduced breastfeeding duration in primiparous overweight and obese women. Am. J. Hum. Biol. 2012, 24, 339–349. [Google Scholar] [CrossRef]
- Gianni, M.L.; Bezze, E.N.; Sannino, P.; Baro, M.; Roggero, P.; Muscolo, S.; Plevani, L.; Mosca, F. Maternal views on facilitators of and barriers to breastfeeding preterm infants. BMC Pediatr. 2018, 18, 283. [Google Scholar] [CrossRef]
- Hoban, R.; Bigger, H.; Schoeny, M.; Engstrom, J.; Meier, P.; Patel, A.L. Milk Volume at 2 Weeks Predicts Mother’s Own Milk Feeding at Neonatal Intensive Care Unit Discharge for Very Low Birthweight Infants. Breastfeed. Med. 2018, 13, 135–141. [Google Scholar] [CrossRef] [PubMed]
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| SSC in the delivery room | |||
| No | 267 | 160 (60.0) | 1.00 (Reference) |
| Yes | 54 | 38 (70.4) | 1.59 (0.84–2.99) |
| SSC in the first week of life | |||
| No | 169 | 90 (53.3) | 1.00 (Reference) |
| Yes | 199 | 133 (65.8) | 1.69 (1.11–2.58) |
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| Breastfeeding at least once during hospital stay | |||
| No | 92 | 26 (28.3) | 1.00 (Reference) |
| Yes | 275 | 195 (70.9) | 6.19 (3.67–10.44) |
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| Mode of delivery | |||
| Vaginal delivery | 56 | 40 (71.4) | 1.00 (Reference) |
| C-section | 312 | 181 (58.0) | 0.55 (0.30–1.03) |
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| Gestational age at birth | |||
| ≥28 weeks | 290 | 185 (63.8) | 1.00 (Reference) |
| <28 weeks | 78 | 36 (46.2) | 0.49 (0.29–0.81) |
| Multiples | |||
| No | 253 | 150 (59.3) | 1.00 (Reference) |
| Yes | 115 | 71 (61.7) | 1.11 (0.71–1.74) |
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| Maternal age | |||
| ≥25 years | 333 | 205 (61.6) | 1.00 (Reference) |
| <25 years | 35 | 16 (45.7) | 0.53 (0.26–1.06) |
| Professional education | |||
| No academic degree | 263 | 159 (60.5) | 1.00 (Reference) |
| Academic degree | 51 | 36 (70.6) | 1.57 (0.82–3.01) |
| Parity | |||
| Primipara | 222 | 135 (60.8) | 1.00 (Reference) |
| Multipara | 146 | 86 (58.9) | 0.92 (0.60–1.41) |
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| Intraventricular hemorrhage, grade 2 or higher | |||
| No | 345 | 211 (61.2) | 1.00 (Reference) |
| Yes | 22 | 9 (40.9) | 0.44 (0.18–1.06) |
| Posthemorrhagic ventricular dilatation | |||
| No | 354 | 214 (60.5) | 1.00 (Reference) |
| Yes | 14 | 7 (50.0%) | 0.65 (0.22–1.91) |
| Abdominal surgery | |||
| No | 349 | 214 (61.3) | 1.00 (Reference) |
| Yes | 19 | 7 (36.8%) | 0.37 (0.14–0.96) |
| Modifying Factor | MOM Feeding at Discharge | ||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| Nicotine or recreational drug use | |||
| No | 332 | 214 (64.4) | 1.00 (Reference) |
| Yes | 36 | 7 (19.4) | 0.13 (0.06–0.31) |
| Gestational diabetes | |||
| No | 331 | 205 (61.9) | 1.00 (Reference) |
| Yes | 37 | 16 (43.2) | 0.47 (0.24–0.93) |
| MOM Feeding at Discharge | |||
|---|---|---|---|
| Total | N (%) | OR (95% CI) | |
| MOM feeding risk score | |||
| 0 | 175 | 121 (69.1) | 1.00 (Reference) |
| 1 | 111 | 68 (61.3) | 0.71 (0.43–1.16) |
| 2 | 74 | 31 (41.9) | 0.32 (0.18–0.57) |
| 3 | 8 | 1 (12.5) | 0.06 (0.01–0.53) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heller, N.; Rüdiger, M.; Hoffmeister, V.; Mense, L. Mother’s Own Milk Feeding in Preterm Newborns Admitted to the Neonatal Intensive Care Unit or Special-Care Nursery: Obstacles, Interventions, Risk Calculation. Int. J. Environ. Res. Public Health 2021, 18, 4140. https://doi.org/10.3390/ijerph18084140
Heller N, Rüdiger M, Hoffmeister V, Mense L. Mother’s Own Milk Feeding in Preterm Newborns Admitted to the Neonatal Intensive Care Unit or Special-Care Nursery: Obstacles, Interventions, Risk Calculation. International Journal of Environmental Research and Public Health. 2021; 18(8):4140. https://doi.org/10.3390/ijerph18084140
Chicago/Turabian StyleHeller, Nadja, Mario Rüdiger, Vanessa Hoffmeister, and Lars Mense. 2021. "Mother’s Own Milk Feeding in Preterm Newborns Admitted to the Neonatal Intensive Care Unit or Special-Care Nursery: Obstacles, Interventions, Risk Calculation" International Journal of Environmental Research and Public Health 18, no. 8: 4140. https://doi.org/10.3390/ijerph18084140
APA StyleHeller, N., Rüdiger, M., Hoffmeister, V., & Mense, L. (2021). Mother’s Own Milk Feeding in Preterm Newborns Admitted to the Neonatal Intensive Care Unit or Special-Care Nursery: Obstacles, Interventions, Risk Calculation. International Journal of Environmental Research and Public Health, 18(8), 4140. https://doi.org/10.3390/ijerph18084140






