Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients
Abstract
1. Introduction
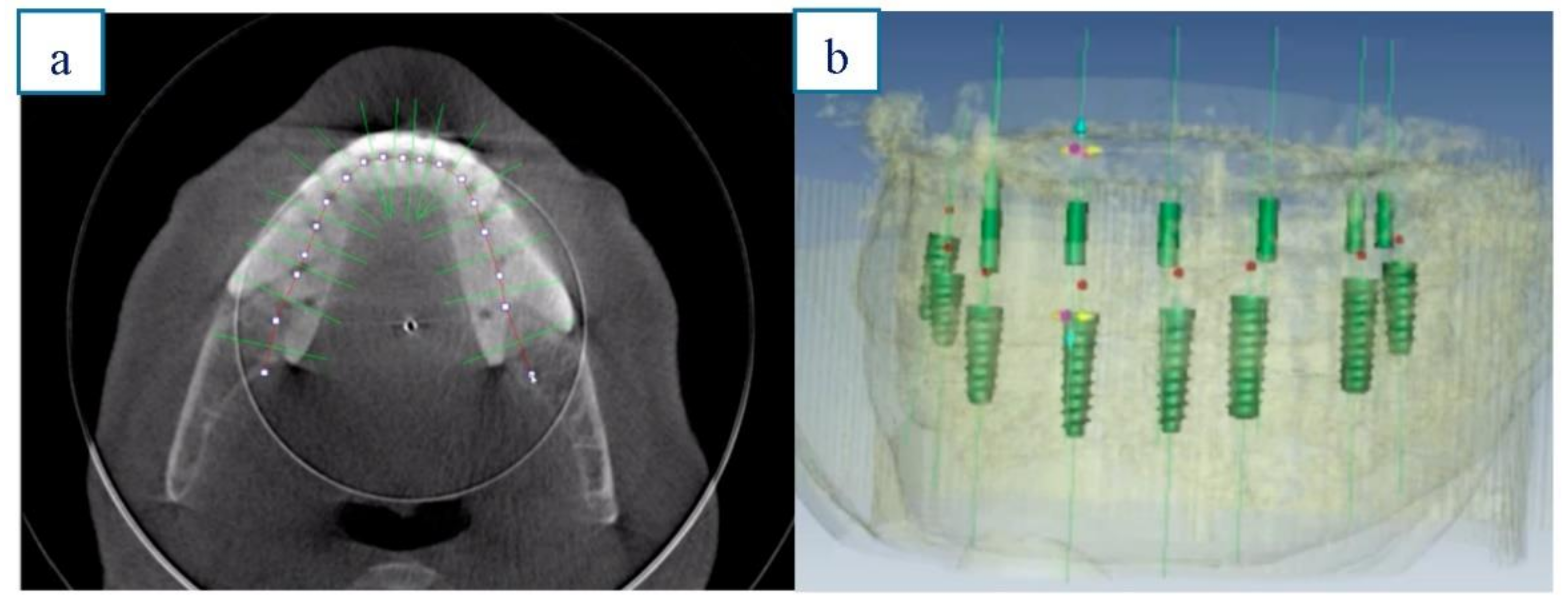
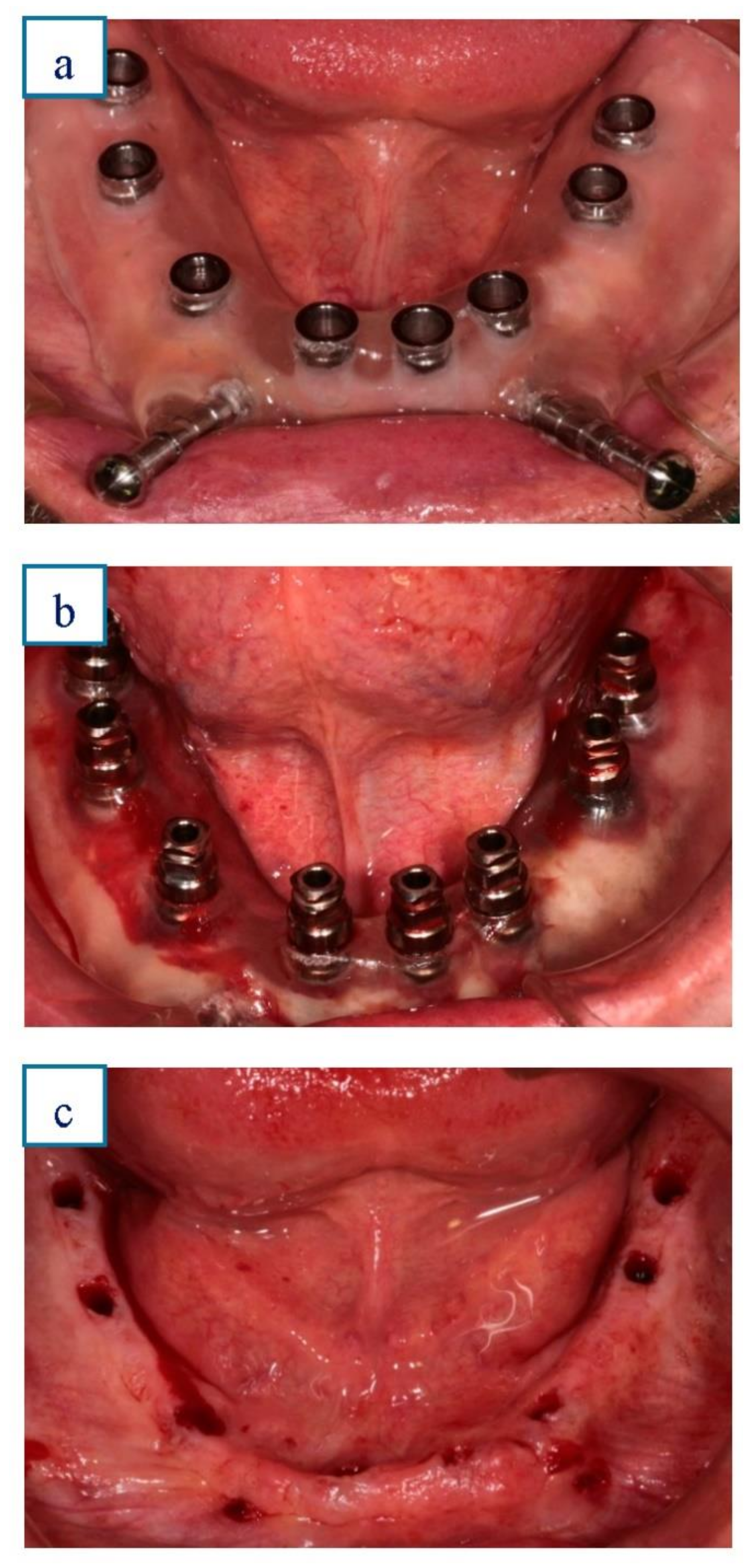
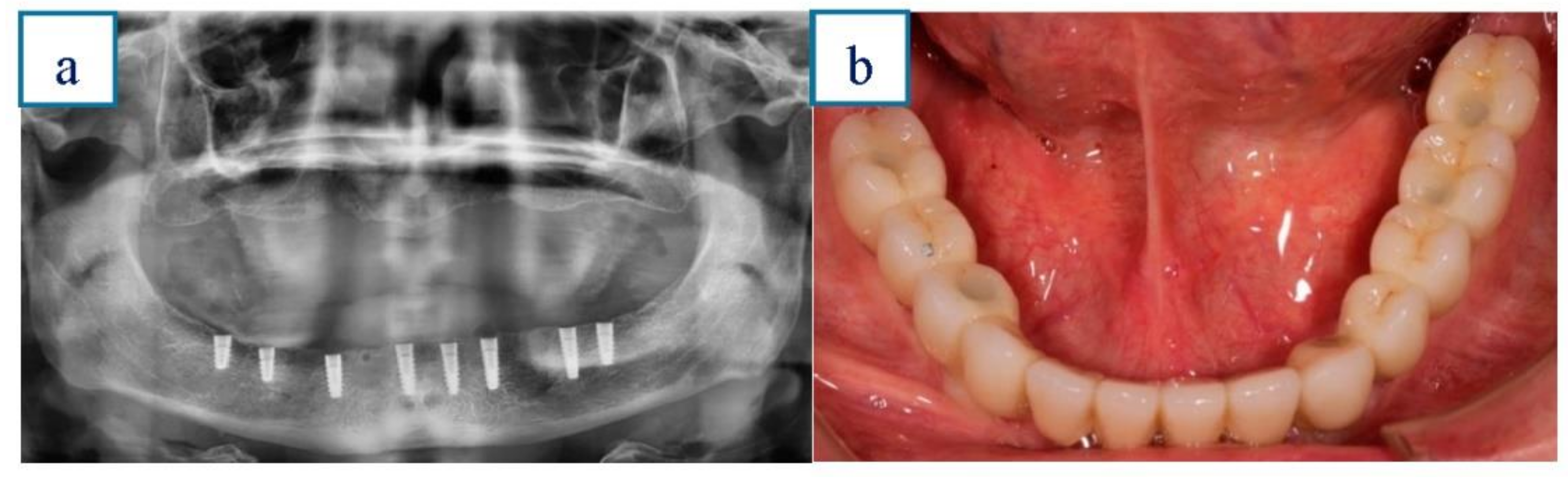
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; de Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontol 2000 2017, 73, 121–133. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Laleman, I.; Jacobs, R.; Quirynen, M. Computer-supported implant planning and guided surgery: A narrative review. Clin. Oral Implant. Res. 2015, 26 (Suppl. 1), 69–76. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 25–42. [Google Scholar] [CrossRef]
- Shelley, A.M.; Ferrero, A.; Brunton, P.; Goodwin, M.; Horner, K. The impact of CBCT imaging when placing dental implants in the anterior edentulous mandible: A before–after study. Br. Dent. J. 2018, 224, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Chen, H.-Y.; DoDo, H.; Yousef, H.; Firestone, A.R.; Chaudhry, J.; Johnston, W.M.; Lee, D.J.; Emam, H.A.; Kim, D.-G. Efficacy of cone-beam computed tomography in evaluating bone quality for optimum implant treatment planning. Implant Dent. 2017, 26, 405–411. [Google Scholar] [CrossRef]
- Pyo, S.W.; Lim, Y.J.; Koo, K.T.; Lee, J. Methods used to assess the 3D accuracy of dental implant positions in computer-guided implant placement: A review. J. Clin. Med. 2019, 8, 54. [Google Scholar] [CrossRef] [PubMed]
- Bernard, L.; Vercruyssen, M.; Duyck, J.; Jacobs, R.; Teughels, W.; Quirynen, M. A randomized controlled clinical trial comparing guided with nonguided implant placement: A 3-year follow-up of implant-centered outcomes. J. Prosthet. Dent. 2019, 121, 904–910. [Google Scholar] [CrossRef]
- Pozzi, A.; Tallarico, M.; Marchetti, M.; Scarfò, B.; Esposito, M. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur. J. Oral Implant. 2014, 7, 229–242. [Google Scholar]
- Stefanelli, L.V.; Mandelaris, G.A.; Franchina, A.; Pranno, N.; Pagliarulo, M.; Cera, F.; Maltese., F.; Angelis, F.; Carlo, S.D. Accuracy of dynamic navigation system workflow for implant supported full arch prosthesis: A case series. Int. J. Environ. Res. Public Health 2020, 17, 5038. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Liu, Z.; Song, L.; Kuo, C.L.; Shafer, D.M. Clinical factors affecting the accuracy of guided implant surgery- a systematic review and meta-analysis. J. Evid. Base Dent. Pract. 2018, 18, 28–40. [Google Scholar] [CrossRef]
- Colombo, M.; Mangano, C.; Mijiritsky, E.; Krebs, M.; Hauschild, U.; Fortin, T. Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health 2017, 17, 150. [Google Scholar] [CrossRef]
- Amorfini, L.; Migliorati, M.; Drago, S.; Silvestrini-Biavati, A. Immediately loaded implants in rehabilitation of the maxilla: A two-year randomized clinical trial of guided surgery versus standard procedure. Clin. Implant Dent. Relat. Res. 2017, 19, 280–295. [Google Scholar] [CrossRef] [PubMed]
- Ciabattoni, G.; Acocella, A.; Sacco, R. Immediately restored full arch-fixed prosthesis on implants placed in both healed and fresh extraction sockets after computer-planned flapless guided surgery. A 3-year follow-up study. Clin. Implant Dent. Relat. Res. 2017, 19, 997–1008. [Google Scholar] [CrossRef] [PubMed]
- Marra, R.; Acocella, A.; Rispoli, A.; Sacco, R.; Ganz, S.D.; Blasi, A. Full-mouth rehabilitation with immediate loading of implants inserted with computer-guided flapless surgery: A 3-year multicenter clinical evaluation with oral health impact profile. Implant Dent. 2013, 22, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Venezia, P.; Torsello, F.; Santomauro, V.; Dibello, V.; Cavalcanti, R. Full digital workflow for the treatment of an edentulous patient with guided surgery, immediate loading and 3D-printed hybrid prosthesis: The BARI technique 2.0. A case report. Int. J. Environ. Res. Public Health 2019, 16, 5160. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Hauschild, U.; Sader, R.; Ghanaati, S. Complete-arch fixed reconstruction by means of guided surgery and immediate loading: A retrospective clinical study on 12 patients with 1 year of follow-up. BMC Oral Health 2020, 20, 15. [Google Scholar] [CrossRef]
- Gallardo, Y.N.R.; da Silva-Olivio, I.R.; Gonzaga, L.; Sesma, N.; Martin, W. A systematic review of clinical outcomes on patients rehabilitated with complete-arch fixed implant-supported prostheses according to the time of loading. J. Prosthodont. 2019, 2, 958–968. [Google Scholar] [CrossRef]
- Kauffmann, P.; Rau, A.; Engelke, W.; Troeltzsch, M.; Brockmeyer, P.; Dagmar, L.S. Cordesmeyer R. Accuracy of Navigation-Guided Dental Implant Placement with Screw Versus Hand Template Fixation in the Edentulous Mandible. Int. J. Oral Maxillofac. Implant. 2018, 33, 383–388. [Google Scholar] [CrossRef]
- Amorfini, L.; Storelli, S.; Romeo, E. Rehabilitation of a dentate mandible requiring a full arch rehabilitation. immediate loading of a fixed complete denture on 8 implants placed with a bone-supported surgical computer planned guide: A case report. J. Oral Implant. 2011, 37, 106–113. [Google Scholar] [CrossRef]
- Spielau, T.; Hauschild, U.; Katsoulis, J. Computer-assisted, template-guided immediate implant placement and loading in the mandible: A case report. BMC Oral Health 2019, 19, 55. [Google Scholar] [CrossRef]
- Verhamme, L.M.; Meijer, G.J.; Boumans, T.; de Haan, A.F.J.; Bergé, S.J.; Maal, T.J.J. A clinically relevant accuracy study of computer-planned implant placement in the edentulous maxilla using mucosa-supported surgical templates. Clin. Implant Dent. Relat. Res. 2015, 17, 343–352. [Google Scholar] [CrossRef]
- Pettersson, A.; Komiyama, A.; Hultin, M.; Nasstrom, K.; Klinge, B. Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin. Implant Dent. Relat. Res. 2013, 14, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Gillot, L.; Noharet, R.; Cannas, B. Guided surgery and presurgical prosthesis: Preliminary results of 33 fully edentulous maxillae treated in accordance with the NobelGuide protocol. Clin. Implant Dent. Relat. Res. 2010, 12 (Suppl. 1), 104–113. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; De Riu, G.; Pisano, M.; Cattina, G.; Tullio, A. Implant treatment software planning and guided flapless surgery with immediate provisional prosthesis delivery in the fully edentulous maxilla. A retrospective analysis of 15 consecutively treated patients. Eur. J. Oral Implantol. 2010, 3, 245–251. [Google Scholar] [PubMed]
- Hultin, M.; Svensson, K.G.; Trulsson, M. Clinical advantages of computer-guided implant placement: A systematic review. Clin. Oral Implant. Res. 2012, 23 (Suppl. 6), 124–135. [Google Scholar] [CrossRef] [PubMed]
- Magrin, G.L.; Rafael, S.N.F.; Passoni, B.B.; Magini, R.S.; Benfatti, C.A.M.; Gruber, R.; Peruzzo, D.C. Clinical and tomographic comparison of dental implants placed by guided virtual surgery versus conventional technique: A split-mouth randomized clinical trial. J. Clin. Periodontol. 2020, 47, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Yogui, F.C.; Verri, F.R.; Gomes, J.M.L.; Lemos, C.A.A.; Cruz, R.S.; Pellizzer, E.P. Comparison between computer-guided and freehand dental implant placement surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2020, 10. [Google Scholar] [CrossRef]
- Ravidà, A.; Barootchi, S.; Tattan, M.; Saleh, M.H.A.; Gargallo-Albiol, J.; Wang, H.L. Clinical outcomes and cost effectiveness of computer guided versus conventional implant-retained hybrid prostheses: A long-term retrospective analysis of treatment protocols. J. Periodontol. 2018, 89, 1015–1024. [Google Scholar] [CrossRef]
- Orenticher, G.; Horowitz, A.; Goldsmith, D.; Delgado-Ruiz, R.; Abboud, M. Cumulative survival rate of implants placed fully guided using CT-guided surgery: A 7-year retrospective study. Compendium 2014, 35, 590–598. [Google Scholar]
- Jané-Salas, E.; Roselló-Llabrés, X.; Jané-Pallí, E.; Mishra, S.; Ayuso-Montero, R.; López-López, J. Open flap versus flapless placement of dental implants. A randomized controlled pilot trial. Odontology 2018, 106, 340–348. [Google Scholar] [CrossRef]
- Limongelli, L.; Tempesta, A.; Crincoli, V.; Favia, G. Massive Lingual and Sublingual Haematoma following Postextractive Flapless Implant Placement in the Anterior Mandible. Case Rep. Dent. 2015, 2015, 839098. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Velloso, G.; Luz, D.; Porto Barboza, E. Implant survival rates, marginal bone level changes, and complications in full-mouth rehabilitation with flapless computer-guided surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2015, 44, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Komiyama, A.; Klinge, B.; Hultin, M. Treatment outcome of immediately loaded implants installed in edentulous jaws following computer-assisted virtual treatment planning and flapless surgery. Clin. Oral Implant. Res. 2008, 19, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Sanna, A.M.; Molly, L.; van Steenberghe, D. Immediately loaded CAD-CAM manufactured fixed complete dentures using flapless implant placement procedures: A cohort study of consecutive patients. J. Prosthet. Dent. 2007, 97, 331–339. [Google Scholar] [CrossRef]
- Tallarico, M.; Meloni, S.M. Retrospective analysis on survival rate, template-related complications, and prevalence of peri-implantitis of 694 anodized implants placed using computer-guided surgery: Results between 1 and 10 years of follow-up. Int. J. Oral Maxillofac. Implant. 2017, 32, 1162–1171. [Google Scholar] [CrossRef]
| n | % | |
|---|---|---|
| Males | 10 | 45.4 |
| Females | 12 | 54.5 |
| History of periodontitis | 11 | 50 |
| Smokers | 6 | 27.3 |
| History of periodontitis and smokers | 5 | 22.7 |
| n | % | |
|---|---|---|
| 3.5 mm implant diameter | 87 | 43.9 |
| 4 mm implant diameter | 111 | 56.1 |
| 10 mm implant length | 132 | 66.7 |
| 12 mm implant length | 66 | 33.3 |
| Implant loss | 5 | 2.5 |
| n | % | n Total | % Total | ||
|---|---|---|---|---|---|
| Implant loss | 5 | 22.7 | 5 | 22.7 | |
| Peri-implantitis | History of periodontitis | 7 | 63.6 | 10 | 45.4 |
| Smoking | 4 | 66.6 * | |||
| Technical complications | Provisional prosthesis | 2 | 9.1 | 6 | 27.3 |
| Definitive prosthesis | 4 | 18.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velasco-Ortega, E.; Jiménez-Guerra, A.; Ortiz-Garcia, I.; Moreno-Muñoz, J.; Núñez-Márquez, E.; Cabanillas-Balsera, D.; López-López, J.; Monsalve-Guil, L. Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients. Int. J. Environ. Res. Public Health 2021, 18, 4125. https://doi.org/10.3390/ijerph18084125
Velasco-Ortega E, Jiménez-Guerra A, Ortiz-Garcia I, Moreno-Muñoz J, Núñez-Márquez E, Cabanillas-Balsera D, López-López J, Monsalve-Guil L. Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients. International Journal of Environmental Research and Public Health. 2021; 18(8):4125. https://doi.org/10.3390/ijerph18084125
Chicago/Turabian StyleVelasco-Ortega, Eugenio, Alvaro Jiménez-Guerra, Ivan Ortiz-Garcia, Jesús Moreno-Muñoz, Enrique Núñez-Márquez, Daniel Cabanillas-Balsera, José López-López, and Loreto Monsalve-Guil. 2021. "Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients" International Journal of Environmental Research and Public Health 18, no. 8: 4125. https://doi.org/10.3390/ijerph18084125
APA StyleVelasco-Ortega, E., Jiménez-Guerra, A., Ortiz-Garcia, I., Moreno-Muñoz, J., Núñez-Márquez, E., Cabanillas-Balsera, D., López-López, J., & Monsalve-Guil, L. (2021). Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients. International Journal of Environmental Research and Public Health, 18(8), 4125. https://doi.org/10.3390/ijerph18084125







