Comparison of Depressive Symptoms and Its Influencing Factors among the Elderly in Urban and Rural Areas: Evidence from the China Health and Retirement Longitudinal Study (CHARLS)
Abstract
1. Introduction
2. Material and Methods
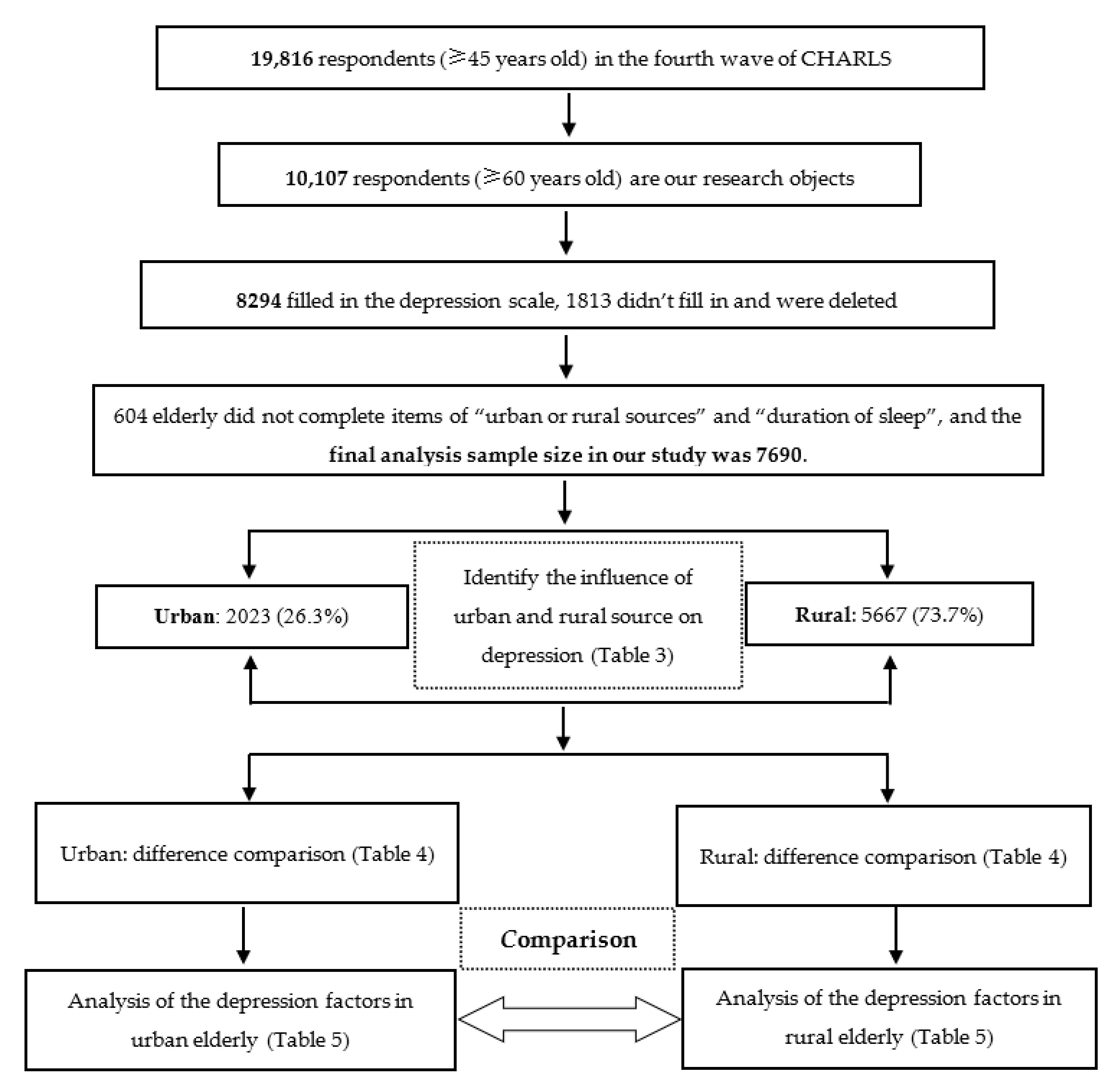
2.1. Participants and Design
2.2. Measurement
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Comparison of Depression in the Elderly between Urban and Rural Areas
3.3. Comparison of Influencing Factors of Depression between Urban and Rural Areas
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Industrial Research Center of China Health Care Industry Alliance. Available online: http://www.jkyl.org.cn/index.php?a=show&c=index&catid=9&id=9735&m=content.2020.02.10.22 (accessed on 28 December 2020).
- Giri, M.; Chen, T.; Yu, W.; Yu, W.H.; Lu, Y. Prevalence and correlates of cognitive impairment and depression among elderly people in the world’s fastest growing city, Chongqing, People’s Republic of China. Clin. Interv. Aging 2016, 11, 1091–1098. [Google Scholar] [CrossRef] [PubMed]
- Blazer, D.G. Depression in late life: Review and commentary. J. Gerontol. A Biol. 2003, 58, 249–265. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates.2017, 02. Available online: http://apps.who.int/iris/bitstream/10665/254610/1/WHO-MSD (accessed on 28 December 2020).
- Li, D.; Zhang, D.J.; Shao, J.J.; Shao, J.J.; Qi, X.D.; Tian, L. A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Arch. Gerontol. Geriatr. 2014, 58, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Andrade, G.E.; Martinez, G.D.; Rodriguez, A.F.; Garcia, E.E. Sedentary behaviors, physical activity, and changes in depression and psychological distress symptoms in older adults. Depress. Anxiety 2018, 35, 884–897. [Google Scholar] [CrossRef]
- Xu, Y.L.; Li, Z.H. The impact of economic welfare on depressive symptoms of the elderly in urban and rural areas of China. Res. Rep. 2018, 1, 17–24. [Google Scholar] [CrossRef]
- Pang, O.Y.; Sun, W. The association between depressive symptoms and fall accidents among middle-aged and elderly people in China. Environ. Health Prev. Med. 2018, 23, 42–49. [Google Scholar]
- Sutin, A.R.; Terracciano, A.; Milaneschi, Y.; An, Y.; Ferrucci, L.; Zonderman, A.B. The Trajectory of Depressive Symptoms across the Adult Life Span. JAMA Psychiatry 2013, 70, 803. [Google Scholar] [CrossRef]
- Wilkinson, P.; Ruane, C.; Tempest, K. Depression in older adults. BMJ 2018, 363, k4922. [Google Scholar] [CrossRef]
- Rodda, J.; Walker, Z.; Carter, J. Depression in older adults. BMJ 2011, 343, 5219. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health in China. Available online: https://www.who.int/china/health-topics/mental-health (accessed on 27 February 2020).
- Hu, Y.; Li, P.; Martikainen, P. Rural-urban disparities in age trajectories of depression caseness in later life: The China health and retirement longitudinal study. PLoS ONE 2019, 14, e0215907. [Google Scholar] [CrossRef]
- Aziz, R.; Steffens, D.C. What are the causes of late-life depression. Psychiatr Clin. N. Am. 2013, 36, 497–516. [Google Scholar] [CrossRef]
- Kaup, A.R.; Byers, A.L.; Falvey, C.; Simonsick, E.M.; Satterfield, S.; Ayonayon, H.N.; Smagula, S.F.; Rubin, S.M.; Yaffe, K. Trajectories of Depressive Symptoms in Older Adults and Risk of Dementia. JAMA Psychiatry 2016, 73, 525–531. [Google Scholar] [CrossRef]
- Musliner, K.L.; Munk Olsen, T.; Eaton, W.W.; Zandi, P.P. Heterogeneity in long-term trajectories of depressive symptoms: Patterns, predictors and outcomes. J. Affect. Disord. 2016, 192, 199–211. [Google Scholar] [CrossRef]
- Huang, L.Q.; Li, H.; Chen, H.Q.; Zhang, J.J.; Zhang, H.H.; Jiang, J.P. The locus of depressive symptoms of elders in China: Based on CHARLS. Zhejiang Med. Educ. 2019, 18, 38–40. [Google Scholar]
- Harithasan, D.; Mukari, Z.S.; Ishak, W.S.; Shahar, S.; Yeong, W.L. The impact sensory impairment on cognitive performance, quality of life, depression, and loneliness in older adults. Int. J. Geriatr. Psychiatry 2020, 35, 358–364. [Google Scholar] [CrossRef]
- Fleury, M.J.; Ngui, A.; Bamvita, J.M.; Grenier, G.; Caron, J. Predictors of Healthcare Service Utilization for Mental Health Reasons. Int. J. Environ. Res. Public Health 2014, 11, 10559–10586. [Google Scholar] [CrossRef]
- Jokela, M.; Batty, G.D.; Vahtera, J.; Elovainio, M.; Kivimaki, M. Socioeconomic inequalities in common mental disorders and psychotherapy treatment in the UK between 1991 and 2009. Br. J. Psychiatry 2013, 202, 115–120. [Google Scholar] [CrossRef]
- Gianluca, S.; Xenia, G.; Giovanna, C.; Pompili, M.; Rihmer, Z. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J. Affect. Disord. 2017, 210, 249–257. [Google Scholar] [CrossRef]
- Zhang, L. Study on Intergenerational Relations and Chinese Elderly Depression in the Perspectives of Gendered and Marital Status. Huazhong Keji Daxue Xuebao 2019, 33, 28–38. [Google Scholar]
- Li, J.S.; Ma, W.J. Prevalence and influencing factors of depression symptom among middle-aged and elderly people in China. Chin. J. Public Health 2017, 33, 177–181. [Google Scholar]
- Liu, L.; Zang, Z.Y.; Liu, J.T.; Zhang, F.Y.; Wu, S.; He, Y. Analysis of the Status Quo of ADL, Self-rated Health and Depression among Chinese Elderly. Med. Soc. 2020, 33, 90–94. [Google Scholar]
- Feng, Q.W.; Wang, Q.N.; Yang, L.S.; Liu, K.Y.; Cao, H.J.; Xie, S.Y.; Li, K.C.; Ma, L.G.; Chen, G.M.; Tao, F.B. The association between depressive symptoms and chronic diseases among elderly people in urban and rural communities of Lu’an City. Mod. Prev. Med. 2018, 45, 3731–3747. [Google Scholar]
- Wu, S.; Zhang, F.Y.; Zang, Z.Y.; Liu, J.T.; He, Y. Analysis on depression and life satisfaction of the elderly in China and influencing factors. J. Zhengzhou Univ. (Med Sci.) 2019, 54, 88–92. [Google Scholar] [CrossRef]
- Li, Y.; Lu, J.H.; Cheng, Q.; Gu, D.N. Association between Social Participation and Depression among Older Adults in China. Popul. Develoment 2020, 26, 86–97. [Google Scholar]
- Wang, S.K. Social Ecology Exploration and Health Intervention Strategies Research of Regular Physical Activity for the Elderly in City Community. Ph.D. Thesis, Shandong University, Jinan, China, July 2012. [Google Scholar]
- Fried, E.I.; Nesse, R.M. Depression sum-scores don’t add up: Why analyzing specific depression symptoms is essential. BMC Med. 2015, 13, 72. [Google Scholar] [CrossRef]
- Li, T.; Chen, X.Z.; Yin, S.F.; Zhang, L.C. Influence of marital status on life satisfaction and depression of empty nest elderly. Chin. J. Gerontol. 2018, 38, 4058–4059. [Google Scholar]
- Zhou, J.; Liu, Y.; Yuan, H.; Jin, L.R.; Li, D.D.; Wang, Z.N. The Prevalence and influencing factors of depressive symptoms among the elderly in a rural community of Anhui province. J. Qiqihar Univ. Med. 2018, 39, 573–576. [Google Scholar]
- Pei, Q.Y. Analysis of Depressive Symptoms and Influencing Factors in Chinese Elderly. Ph.D. Thesis, Zhengzhou University, Zhengzhou, China, June 2019. [Google Scholar]
- Li, L. Social Medicine, 5th ed.; People’s Health Publishing House: Beijing, China, 2017; pp. 28–29. [Google Scholar]
- Wang, X.L.; Li, J.; Wei, L.L. Analysis of depressive symptoms of the elderly in China. Popul. J. 2010, 5, 43–47. [Google Scholar]
- Yang, Z.; Chen, R.; Hu, X.; Ren, X.H. Factors that related to the depressive symptoms among elderly in urban and rural areas of China. China J. Epidemiol. 2017, 38, 1088–1093. [Google Scholar]
- Zhang, L.; Xu, Y.; Nie, H.; Zhang, Y.D.; Wu, Y. The prevalence of depressive symptoms among the older in China: A meta-analysis: The prevalence of depressive symptoms. Int. J. Geriatr. Psychiatry 2012, 27, 900–906. [Google Scholar] [CrossRef]
- Hou, B.; Nazroo, J.; Banks, J.; Marshall, A. Are cities good for health? A study of the impacts of planned urbanization in China. Int. J. Epidemiol. 2019, 48, 1083–1090. [Google Scholar] [CrossRef]
- Gan, C.J.; Zhao, X. The disparity in depression status between the urban and rural elderly based on Fairlie decomposition method. Chin. J. Geiatr. 2020, 06706–06710. [Google Scholar] [CrossRef]
- He, S.; Song, D.; Jian, W.Y. The Association between Urbanization and Depression among the Middle-Aged and Elderly: A Longitudinal Study in China. J. Health Care Organ. Provis. Financ. 2020, 57, 1–9. [Google Scholar] [CrossRef]
- Ruan, Y.H.; Zhu, D.M. Association of Chinese drifting elderly’s intergenerational support satisfaction with expectation: A mixed method study in Shanghai. Int. J. Health Plann Manag. 2021, 36, 173–188. [Google Scholar] [CrossRef]
- Zhao, Y.H.; Hu, Y.S.; James, P.S.; John, S.; Yang, G.H. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef]
- James, P.S.; Tian, M.; Zhao, Y.H. Community Effects on Elderly Health: Evidence from CHARLS National Baseline. J. Econ. Ageing 2014, 1, 1–21. [Google Scholar]
- Zhao, Y.H.; John, S.; Yang, G.H.; John, G.; Hu, P.F.; Hu, Y.S.; Lei, X.Y.; Liu, M.; Park, A.; Smith, J.P.; et al. China Health and Retirement Longitudinal Study, Wave 4 User’s Guide; National School of Development, Peking University: Beijing, China, 2020. [Google Scholar]
- Chen, H.J.; Mui, A.C. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int. Psychogeriatr. 2014, 26, 49–57. [Google Scholar] [CrossRef]
- Qin, T.; Liu, W.; Yin, M.; Shu, C.; Yan, M.M.; Zhang, J.Y.; Yin, P. Body mass index moderates the relationship between C-reactive protein and depressive symptoms: Evidence from the CHARLS. Sci. Rep. 2017, 7, 39940. [Google Scholar] [CrossRef]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D(Center for Epidemiology Studies Depression Scale). Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Huang, O.B.; Wang, X.H.; Chen, G. Reliability and validity of 10 item CES—D among middle aged and older adults in China. Chin. J. Health Psychol. 2015, 23, 1036–1041. [Google Scholar]
- United Nations Department of Economic and Social Affairs. Population Division. World Urbanization Prospects: The 2018 Revision. Available online: https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf (accessed on 27 February 2020).
- Pun, V.C.; Manjourides, J.; Suh, H.H. Close proximity to roadway and urbanicity associated with mental ill-health in older adults. Sci. Total Environ. 2019, 658, 854–860. [Google Scholar] [CrossRef] [PubMed]
- Bezold, C.P.; Banay, R.F.; Coull, B.A.; Hart, J.E.; James, P.; Kubzansky, L.D.; Missmer, S.A.; Laden, F. The relationship between surrounding greenness in childhood and adolescence and depressive symptoms in adolescence and early adulthood. Ann. Epidemiol. 2018, 28, 213–219. [Google Scholar] [CrossRef]
- Generaal, E.; Timmermans, E.J.; Dekkers, J.E.C.; Smit, J.H.; Penninx, B.W. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychol. Med. 2019, 49, 149–161. [Google Scholar] [CrossRef]
- Generaal, E.; Hoogendijk, E.O.; Stam, M.; Henke, C.; Rutters, F.; Oosterman, M.; Huisman, M.; Kramer, S.E.; Elders, P.M.; Timmermans, E.J.; et al. Neighbourhood characteristics and prevalence and severity of depression: Pooled analysis of eight Dutch cohort studies. Br. J. Psychiatry 2019, 215, 468–475. [Google Scholar] [CrossRef]
- Bui, Q.T.; Vu, L.T.; Tran, D.M. Trajectories of depression in adolescents and young adults in Vietnam during rapid urbanisation: Evidence from a longitudinal study. J. Child. Adolesc. Ment. Health 2018, 30, 51–59. [Google Scholar] [CrossRef]
- Arvind, B.A.; Gururaj, G.; Loganathan, S.; Amudhan, S.; Varghese, M.; Benegal, V.; Rao, G.N.; Kokane, A.M.; Chavan, B.S.; Dalal, P.K.; et al. Prevalence and socioeconomic impact of depressive disorders in India: Multisite population-based cross-sectional study. BMJ Open 2019, 9, e027250. [Google Scholar] [CrossRef]
- Galea, S.; Freudenberg, N.; Vlahov, D. Cities and population health. Soc. Sci. Med. 2005, 60, 1017–1033. [Google Scholar] [CrossRef]
- Galea, S.; Bresnahan, M.; Susser, E. Mental health in the city. In Cities and the Health of the Public, 1st ed.; Freudenberg, N., Galea, S., Vlahov, D., Eds.; Vanderbilt University Press: Nashville, TN, USA, 2006; pp. 247–273. [Google Scholar]
- Jiang, C.H.; Zhu, F.; Qin, T.T. Relationships between Chronic Diseases and Depression among Middle aged and Elderly People in China: A Prospective Study from CHARLS. Curr. Med. Sci. 2020, 40, 858–870. [Google Scholar] [CrossRef]
- He, X.Y.; Liu, Z.; Liu, M.Y.; Lu, Z.W.; Yin, P. Related factors of depression symptoms comorbid of physical pain in elderly. Chin. Ment. Health J. 2017, 31, 714–717. [Google Scholar]
- Chen, H. A Research on Health Level of the Elderly and Its Influencing Factors. Ph.D. Thesis, Hebei University, Baoding, China, May 2017. [Google Scholar]
- Zhang, J.; Zhang, Y.Y.; Luan, Z.G.; Zhang, X.J.; Jiang, H.R.; Wang, A.P. A study on depression of the elderly with different sleep quality in pension institutions in Northeastern China. BMC Geriatr. 2020, 20, 374. [Google Scholar] [CrossRef]
- Kim, A.E.; Jang, M.H.; Park, K.H.; Min, J.Y. Effects of Self-Efficacy, Depression, and Anger on Health-Promoting Behaviors of Korean Elderly Women with Hypertension. Int. J. Environ. Res. Public Health 2020, 17, 6296. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.N.; Wang, Z.J.; Zheng, X.Y. Association between the change of daily living activities and symptoms of depression in Chinese middle-aged and elderly people. Chin. J. Epidemiol. 2017, 38, 1055–1059. [Google Scholar]
| Type of Variables | Name and Definition of Variables | Variable Assignment |
|---|---|---|
| Demographic variables | Urban and rural areas (their Hukou status, which is a population registration system used in China that indicate individual’s rural or urban residency status. Specifically, agricultural hukou was classified as rural hukou, while non-agricultural hukou and unified residence hukou were classified as urban hukou. Hukou is a population registration system that has long been used in China. Every Chinese citizen is required to legally register in the system, as either agricultural or non-agricultural residency (normally referred to as rural vs. urban) | Urban = 1 |
| Rural = 2 | ||
| Gender | Male = 1 | |
| Female = 2 | ||
| Age (the real age = the respondent’s birth year and month minus the interview year and month.) | 60–64 = 1 | |
| 65–74 = 2 | ||
| ≥75 = 3 | ||
| Marital status | Married and live with spouse = 1 | |
| Married but not live with spouse = 2 | ||
| Divorced = 3 | ||
| Widower = 4 | ||
| Never married = 5 | ||
| Education level (the highest level of education that the respondent attained was self-reported in CHARLS) | Illiterate = 1 | |
| Elementary school and below = 2 | ||
| Middle school = 3 | ||
| High\vocational school and above = 4 | ||
| Minorities (there are 56 ethnic groups in China, all of which are called ethnic minorities except the Han nationality) | Han = 1 | |
| Ethnic minorities = 2 | ||
| Religious belief | No = 0 | |
| Yes = 1 | ||
| Having income or not (did you receive any wage and bonus income [except pension] in the past year?) | No = 0 | |
| Yes = 1 | ||
| Health related variables | Self-reported health (would you say your health is very good, good, fair, poor or very poor?) | Very good = 1 |
| Good = 2 | ||
| Fair = 3 | ||
| Poor = 4 | ||
| Very poor = 5 | ||
| Duration of sleep (during the past month, how many hours of actual sleep did you get at night? (average hours for one night)) | ≤5 h = 1 | |
| 6–9 h = 2 | ||
| ≥10 h = 3 | ||
| Life satisfaction (How satisfied are you with your life overall? Are you completely satisfied, very satisfied, somewhat satisfied, not very satisfied, or not satisfied at all?) | Completely satisfied = 1 | |
| Very satisfied = 2 | ||
| Somewhat satisfied = 3 | ||
| Not very satisfied = 4 | ||
| Not satisfied at all =5 | ||
| Chronic disease (including hypertension, diabetes or high blood sugar, cancer or a malignant tumor, chronic lung disease such as chronic bronchitis or emphysema, heart diseases, stroke, emotional, nervous, or psychiatric problems, arthritis, dyslipidemia, liver disease, kidney disease, stomach or other digestive disease, asthma.) | Having none of these chronic disease = 0 | |
| Having one of these chronic disease = 1 | ||
| Social activities (whether they participated in the following social activities in the past month: “interacted with friend”, “played Ma-jong, chess, cards, or went to a community club”, “sent to a sporting event, participated in a social group, or participated in some other sort of club”, “took part in a community-related organization”, “took part in voluntary or charity work”, “attended an educational or training course”.) | Having none of these social activities = 0 | |
| Having one of these social activities = 1 | ||
| Dependent variable | Depressive symptoms (recoded from continuous variable [1–30 scores], and transformed into binary variable, ≤10: negative; >10: positive) | ≤10 = 0 |
| >10 = 1 |
| Variables | Urban | Rural | Total |
|---|---|---|---|
| Gender | |||
| Male | 987 (48.8) | 2962 (52.3) | 3949 (51.4) |
| Female | 1036 (52.30) | 2705 (47.7) | 3741 (48.6) |
| Age | |||
| 60–64 | 712 (35.2) | 2091 (36.9) | 2803 (36.4) |
| 65–74 | 958 (47.4) | 2803 (49.5) | 3761 (48.9) |
| ≥75 | 353 (17.4) | 773 (13.6) | 1126 (14.6) |
| Marital status | |||
| Married and live with spouse | 1574 (77.8) | 4405 (77.7) | 5979 (77.8) |
| Married but not live with spouse | 68 (3.4) | 201 (3.5) | 269 (3.5) |
| Divorced | 35 (1.7) | 38 (0.7) | 73 (0.9) |
| Widowed | 346 (17.1) | 1023 (18.1) | 1323 (17.2) |
| Never married | 6 (0.3) | 40 (0.7) | 46 (0.6) |
| Education level | |||
| Illiterate | 225 (11.1) | 1761 (31.1) | 1986 (25.8) |
| Elementary school and below | 760 (37.6) | 2858 (50.4) | 3618 (47.0) |
| Middle school | 547 (27.0) | 758 (13.4) | 1305 (17.0) |
| High\vocational school and above | 491 (24.3) | 290 (5.1) | 781 (10.1) |
| Minorities | |||
| Han | 1885 (93.2) | 5288 (93.3) | 7173 (92.8) |
| Ethnic minorities | 138 (6.8) | 397 (6.7) | 517 (7.2) |
| Religious beliefs | |||
| No | 1815 (89.7) | 5051 (89.1) | 6866 (89.3) |
| Yes | 208 (10.3) | 616 (10.9) | 824 (10.7) |
| Self-reported health | |||
| Very good | 212 (10.5) | 592 (10.4) | 804 (10.5) |
| Good | 278 (13.7) | 586 (10.3) | 864 (11.2) |
| Fair | 1072 (53.0) | 2710 (47.8) | 3782 (49.2) |
| Poor | 351 (17.4) | 1368 (24.1) | 1719 (22.4) |
| Very poor | 110 (5.4) | 408 (7.2) | 518 (6.7) |
| Duration of sleep | |||
| ≤5 h | 676 (33.4) | 2059 (36.3) | 2735 (35.6) |
| 6–9 h | 1254 (62.0) | 2955 (52.1) | 4209 (54.7) |
| ≥10 h | 93 (4.6) | 653 (11.5) | 746 (9.7) |
| Life satisfaction | |||
| Completely satisfied | 107 (5.3) | 277 (4.9) | 384 (5.0) |
| Very satisfied | 605 (29.9) | 1873 (33.1) | 2478 (32.2) |
| Somewhat satisfied | 1174 (58.0) | 2915 (51.3) | 4089 (53.2) |
| Not very satisfied | 99 (4.9) | 446 (7.9) | 545 (7.1) |
| Not at all satisfied | 38 (1.9) | 156 (2.8) | 194 (2.5) |
| Chronic diseases | |||
| No | 977 (48.3) | 3098 (54.7) | 4075 (53.0) |
| Yes | 1046 (51.7) | 2569 (45.3) | 3615 (47.01) |
| Social activities | |||
| No | 732 (36.2) | 3093 (54.6) | 3825 (49.7) |
| Yes | 1291 (63.8) | 2574 (45.4) | 3865 (50.3) |
| Having income or not | |||
| No | 1583 (78.3) | 4493 (79.3) | 6076 (79.0) |
| Yes | 440 (21.7) | 1174 (20.7) | 1614 (21.0) |
| Variables | Unadjusted Model OR-unadjusted (95% CI) | Fully Adjusted Model OR-adjusted (95% CI) |
|---|---|---|
| Urban and rural source | ||
| Urban | 1 | 1 |
| Rural | 1.88 (1.67, 2.12) | 1.52 (1.32, 1.76) |
| Gender | ||
| Male | 1 | 1 |
| Female | 1.95 (1.76, 2.15) | 1.62 (1.43, 1.84) |
| Age | ||
| 60–64 | 1 | 1 |
| 65–74 | 1.04 (0.94, 1.16) | 0.98 (0.86, 1.11) |
| ≥75 | 1.02 (0.88, 1.19) | 0.94 (0.79, 1.13) |
| Marital status | ||
| Married and live with spouse | 1 | 1 |
| Married but not live with spouse | 1.04 (0.80, 1.37) | 0.98 (0.72, 1.33) |
| Divorced | 1.29 (0.79, 2.09) | 1.24 (0.69, 2.22) |
| Widower | 1.60 (1.41, 1.81) | 1.22 (1.05, 1.42) |
| Never married | 1.32 (0.72, 2.42) | 1.33 (0.66, 2.68) |
| Education level | ||
| Illiterate | 1 | 1 |
| Elementary school and below | 0.73 (0.65, 0.81) | 0.93 (0.81, 1.07) |
| Middle school | 0.43 (0.36, 0.50) | 0.68 (0.56, 0.83) |
| High\vocational school and above | 0.27 (0.22, 0.34) | 0.47 (0.37, 0.61) |
| Minorities | ||
| Han | 1 | 1 |
| Ethnic minorities | 1.35 (1.12, 1.62) | 1.31 (1.06, 1.62) |
| Religious beliefs | ||
| No | 1 | 1 |
| Yes | 1.06 (0.91, 1.24) | 1.12 (0.94, 1.35) |
| Self-reported health | ||
| Very good | 1 | 1 |
| Good | 0.27 (0.02, 2.98) | 0.41 (0.03, 5.34) |
| Fair | 0.40 (0.04, 4.44) | 0.56 (0.04, 7.19) |
| Poor | 0.66 (0.06, 7.23) | 0.75 (0.06, 9.56) |
| Very poor | 2.02 (0.18, 22.28) | 1.74 (0.14, 22.35) |
| Duration of sleep | ||
| ≤5 h | 1 | 1 |
| 6–9 h | 0.35 (0.31, 0.38) | 0.48 (0.43, 0.54) |
| ≥10 h | 0.46 (0.38, 0.55) | 0.53 (0.44, 0.65) |
| Life satisfaction | ||
| Completely satisfied | 1 | 1 |
| Very satisfied | 1.06 (0.80, 1.40) | 1.09 (0.81, 1.46) |
| Somewhat satisfied | 1.98 (1.51, 2.58) | 1.98 (1.48, 2.64) |
| Not very satisfied | 9.98 (7.27, 13.68) | 7.39 (5.25, 10.39) |
| Not satisfied at all | 29.80 (18.27, 48.78) | 17.11 (10.11, 28.97) |
| Chronic disease | ||
| No | 1 | 1 |
| Yes | 1.63 (1.48, 1.79) | 1.22 (1.09, 1.37) |
| Social activities | ||
| No | 1 | 1 |
| Yes | 0.73 (0.66, 0.80) | 0.87 (0.77, 0.97) |
| Having income or not | ||
| No | 1 | 1 |
| Yes | 0.77 (0.69, 0.87) | 0.80 (0.70, 0.92) |
| Variables | Urban (N = 2023, N (%)) | Rural (N = 5667, N (%)) | ||||
|---|---|---|---|---|---|---|
| Depression | Normal | χ2-Value | Depression | Normal | χ2-Value | |
| Gender | ||||||
| Male | 171 (17.3) | 816 (83.7) | 19.93 ** | 773 (26.1) | 2189 (73.9) | 173.60 ** |
| Female | 264 (25.5) | 772 (74.5) | 1155 (42.7) | 1550 (57.3) | ||
| Age | ||||||
| 60–64 | 155 (21.8) | 557 (78.2) | 3.70 | 692 (33.1) | 1399 (66.9) | 1.89 |
| 65–74 | 192 (20.0) | 766 (80.0) | 978 (34.9) | 1825 (65.1) | ||
| ≥75 | 88 (24.9) | 265 (75.1) | 258 (33.4) | 515 (66.6) | ||
| Marital status | ||||||
| Married and live with spouse | 315 (20.0) | 1259 (80.0) | 13.67 * | 1408 (32.0) | 2997 (68.0) | 49.78 ** |
| Married but not live with spouse | 17 (25.0) | 51 (75.0) | 63 (31.3) | 138 (68.7) | ||
| Divorced | 5 (14.3) | 30 (85.7) | 20 (52.6) | 18 (47.4) | ||
| Widower | 97 (28.5) | 243 (71.5) | 422 (42.9) | 561 (57.1) | ||
| Never married | 1 (16.7) | 5 (83.3) | 15 (37.5) | 25 (62.5) | ||
| Education level | ||||||
| Illiterate | 69 (30.7) | 156 (69.3) | 35.45 ** | 720 (40.9) | 1041 (59.1) | 109.96 ** |
| Elementary school and below | 194 (25.5) | 566 (74.5) | 967 (34.1) | 1882 (65.9) | ||
| Middle school | 10 0 (18.3) | 447 (81.7) | 186 (24.5) | 572 (75.5) | ||
| High \vocational school and above | 72 (14.66) | 41 9(85.34) | 46 (15.9) | 244 (84.1) | ||
| Minorities | ||||||
| Han | 403 (21.4) | 1482 (78.6) | 0.25 | 1769 (33.5) | 3519 (66.5) | 11.38 ** |
| Ethnic minorities | 32 (23.3) | 106 (76.8) | 159 (42.0) | 220 (58.0) | ||
| Religious beliefs | 393 (21.7) | 1422 (78.3) | ||||
| No | 0.24 | 1708 (33.8) | 3343 (66.2) | 0.88 | ||
| Yes | 42 (20.2) | 166 (79.8) | 220 (35.7) | 396 (64.3) | ||
| Self-reported health | ||||||
| Very good | 11 (5.2) | 201 (94.8) | 230.04 ** | 96 (11.9) | 711 (88.1) | 585.92 ** |
| Good | 25 (9.0) | 253 (91.0) | 144 (16.7) | 720 (83.3) | ||
| Fair | 192 (17.9) | 880 (82.1) | 933 (24.7) | 2849 (75.3) | ||
| Poor | 144 (41.0) | 207 (59.0) | 863 (50.2) | 856 (49.8) | ||
| Very poor | 63 (57.3) | 4 7(42.7) | 327 (63.1) | 191 (36.9) | ||
| Duration of sleep | ||||||
| ≤5 h | 240(35.5) | 436(64.5) | 121.78** | 991(48.1) | 1068(51.9) | 288.07*** |
| 6–9 h | 174(13.9) | 1080(86.1) | 755(25.5) | 2200(74.5) | ||
| ≥10 h | 21(22.6) | 72(77.4) | 182(27.9) | 471(72.1) | ||
| Life satisfaction | ||||||
| Completely satisfied | 17 (15.9) | 90 (84.1) | 246.16 ** | 54 (19.5) | 223 (80.5) | 605.07 ** |
| Very satisfied | 62 (10.2) | 543 (89.8) | 418 (22.3) | 1455 (77.7) | ||
| Somewhat satisfied | 261 (22.2) | 913 (77.8) | 1004 (34.4) | 1911 (65.6) | ||
| Not very satisfied | 61 (61.6) | 38 (38.4) | 317 (71.1) | 129 (28.9) | ||
| Not satisfied at all | 34 (89.5) | 4 (10.5) | 135 (86.5) | 21 (13.5) | ||
| Chronic disease | ||||||
| No | 153 (15.7) | 824 (84.3) | 38.21 ** | 901 (29.1%) | 2197 (70.9) | 74.24 ** |
| Yes | 282 (27.0) | 763 (73.0) | 1027 (40.0%) | 1542 (60.0) | ||
| Social activities | ||||||
| No | 211 (28.8) | 521 (71.2) | 36.44 ** | 1093 (35.3) | 2000 (64.7) | 5.26 * |
| Yes | 224 (17.4) | 1067 (82.6) | 835 (32.4) | 1739 (67.6) | ||
| Having income or not | ||||||
| No | 353 (22.3) | 1229 (77.7) | 3.03 | 1582 (35.2) | 2911 (64.8) | 13.66 ** |
| Yes | 82 (18.6) | 359 (81.4) | 346 (29.5) | 828 (70.5) | ||
| Variables | Urban | Rural | Significance of Difference (Coefficient) | ||
|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||
| Gender | |||||
| Male | 1 | - | 1 | - | |
| Female | 1.46 * | 1.09, 1.96 | 1.68 ** | 1.46, 1.93 | 0.128 |
| Age | |||||
| 60–64 | 1 | - | 1 | - | |
| 65–74 | 0.81 | 0.59, 1.10 | 1.01 | 0.88, 1.16 | 0.191 |
| ≥75 | 0.99 | 0.66, 1.49 | 0.90 | 0.73, 1.11 | −0.139 |
| Marital status | |||||
| Married and live with spouse | 1 | - | 1 | - | |
| Married but not live with spouse | 1.22 | 0.57, 2.59 | 0.94 | 0.66, 1.33 | −0.150 |
| Divorced | 0.58 | 0.18, 1.85 | 2.15 * | 1.01, 4.58 | 1.567 * |
| Widower | 1.18 | 0.82, 1.72 | 1.24* | 1.05, 1.47 | 0.106 |
| Never married | 0.48 | 0.04, 6.62 | 1.48 | 0.71, 3.07 | 1.086 |
| Education level | |||||
| Illiterate | 1 | - | 1 | - | |
| Elementary school and below | 0.82 | 0.54, 1.24 | 0.95 | 0.82, 1.10 | 0.097 |
| Middle school | 0.55 * | 0.34, 0.88 | 0.71 * | 0.56, 0.89 | 0.095 |
| High\vocational school and above | 0.40 ** | 0.24, 0.65 | 0.42 ** | 0.29, 0.61 | −0.151 |
| Minorities | |||||
| Han | 1 | - | 1 | - | |
| Ethnic minorities | 1.11 | 0.67, 1.85 | 1.37 * | 1.08, 1.74 | 0.200 |
| Religious beliefs | |||||
| No | 1 | 0 | 1 | - | |
| Yes | 1.10 | 0.90, 1.35 | 1.12 | 0.94, 1.34 | −0.069 |
| Self-reported health | |||||
| Very good | 1 | - | 1 | - | −0.179 |
| Good | 1.74 | 0.76, 4.00 | 1.35 | 0.97, 1.86 | −0.298 |
| Fair | 2.50 * | 1.22, 5.14 | 1.68 ** | 1.29, 2.19 | −0.637 |
| Poor | 5.98 ** | 2.84, 12.59 | 3.92 ** | 2.98, 5.18 | −0.625 |
| Very poor | 12.74 ** | 5.51, 29.46 | 5.71 ** | 4.08, 7.99 | −0.849 |
| Duration of sleep | |||||
| ≤5 h | 1 | - | 1 | - | |
| 6–9 h | 0.42 | 0.33, 0.54 | 0.50 ** | 0.44, 0.58 | 0.181 |
| ≥10 h | 0.66 | 0.37, 1.18 | 0.52 ** | 0.42, 0.65 | −0.239 |
| Life satisfaction | |||||
| Completely satisfied | 1 | - | 1 | - | |
| Very satisfied | 0.69 | 0.34, 1.42 | 1.24 | 0.89, 1.74 | 0.707 |
| Somewhat satisfied | 1.55 | 0.79, 3.03 | 2.14 ** | 1.54, 2.98 | 0.357 |
| Not very satisfied | 6.57 ** | 2.90, 14.86 | 7.68 ** | 5.23, 11.29 | 0.118 |
| Not satisfied at all | 54.74 ** | 10.36, 289.30 | 15.34 ** | 8.61, 27.33 | −0.650 |
| Chronic disease | |||||
| No | 1 | - | 1 | - | |
| Yes | 1.68 ** | 1.27, 2.23 | 1.17 * | 1.03, 1.33 | −0.243 |
| Social activities | |||||
| No | 1 | - | 1 | - | |
| Yes | 0.68 * | 0.51, 0.90 | 0.93 | 0.82, 1.06 | 0.340 * |
| Having income or not | |||||
| No | 1 | - | 1 | - | |
| Yes | 0.84 | 0.61,1.16 | 0.79 * | 0.68, 0.93 | −0.036 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.; Fan, X.; Luo, H.; Zhou, Z.; Shen, C.; Hu, N.; Zhai, X. Comparison of Depressive Symptoms and Its Influencing Factors among the Elderly in Urban and Rural Areas: Evidence from the China Health and Retirement Longitudinal Study (CHARLS). Int. J. Environ. Res. Public Health 2021, 18, 3886. https://doi.org/10.3390/ijerph18083886
Liu H, Fan X, Luo H, Zhou Z, Shen C, Hu N, Zhai X. Comparison of Depressive Symptoms and Its Influencing Factors among the Elderly in Urban and Rural Areas: Evidence from the China Health and Retirement Longitudinal Study (CHARLS). International Journal of Environmental Research and Public Health. 2021; 18(8):3886. https://doi.org/10.3390/ijerph18083886
Chicago/Turabian StyleLiu, Haixia, Xiaojing Fan, Huanyuan Luo, Zhongliang Zhou, Chi Shen, Naibao Hu, and Xiangming Zhai. 2021. "Comparison of Depressive Symptoms and Its Influencing Factors among the Elderly in Urban and Rural Areas: Evidence from the China Health and Retirement Longitudinal Study (CHARLS)" International Journal of Environmental Research and Public Health 18, no. 8: 3886. https://doi.org/10.3390/ijerph18083886
APA StyleLiu, H., Fan, X., Luo, H., Zhou, Z., Shen, C., Hu, N., & Zhai, X. (2021). Comparison of Depressive Symptoms and Its Influencing Factors among the Elderly in Urban and Rural Areas: Evidence from the China Health and Retirement Longitudinal Study (CHARLS). International Journal of Environmental Research and Public Health, 18(8), 3886. https://doi.org/10.3390/ijerph18083886






