Increased Risk of Traumatic Injuries among Parents of Children with Attention Deficit/Hyperactivity Disorder: A Nationwide Population-Based Study
Abstract
1. Introduction
1.1. Attention-Deficit/Hyperactivity Disorder and Risk for Injury
1.2. Do Parents of Children with ADHD Have a Higher Risk of Traumatic Injuries than Parents of Children without ADHD?
1.3. Aim of The Study
2. Methods
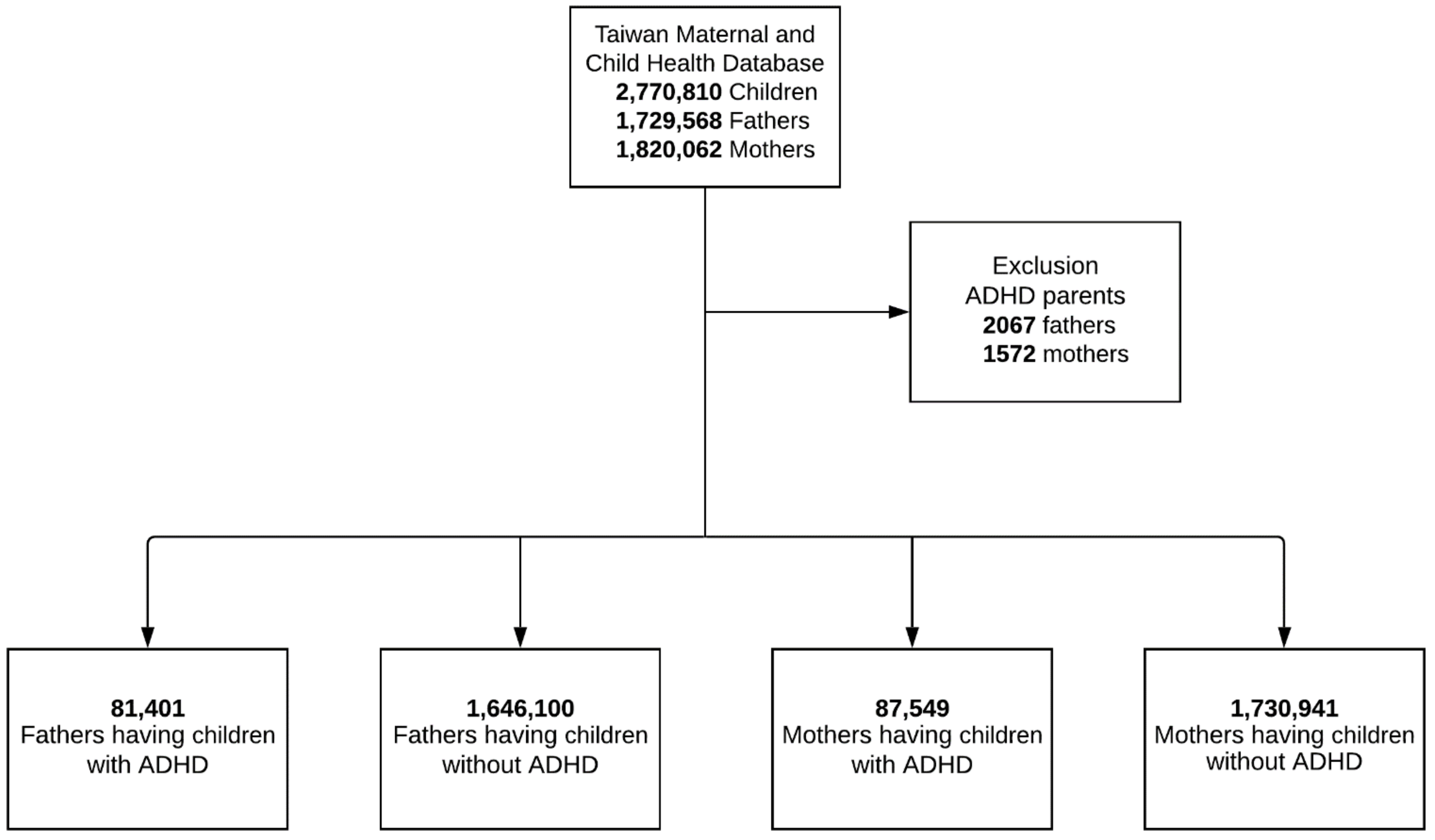
2.1. Population
2.2. Measure
2.2.1. Exposure
2.2.2. Outcome
2.2.3. Covariates
2.3. Statistical Analyses
3. Results
4. Discussion
4.1. Main Findings of the Current Study
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rappley, M.D. Clinical practice. Attention deficit-hyperactivity disorder. N. Engl. J. Med. 2005, 352, 165–173. [Google Scholar] [CrossRef]
- American Psychiatric Association. DSM-5 Task Force. In Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef]
- Thomas, R.; Sanders, S.; Doust, J.; Beller, E.; Glasziou, P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics 2015, 135, e994–e1001. [Google Scholar] [CrossRef]
- Simon, V.; Czobor, P.; Balint, S.; Meszaros, A.; Bitter, I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. Br. J. Psychiatry 2009, 194, 204–211. [Google Scholar] [CrossRef]
- Doshi, J.A.; Hodgkins, P.; Kahle, J.; Sikirica, V.; Cangelosi, M.J.; Setyawan, J.; Erder, M.H.; Neumann, P.J. Economic impact of childhood and adult attention-deficit/hyperactivity disorder in the United States. J. Am. Acad. Child. Adolesc. Psychiatry 2012, 51, 10–990. [Google Scholar] [CrossRef] [PubMed]
- Asherson, P.; Buitelaar, J.; Faraone, S.V.; Rohde, L.A. Adult attention-deficit hyperactivity disorder: Key conceptual issues. Lancet Psychiatry 2016, 3, 568–578. [Google Scholar] [CrossRef]
- Thapar, A.; Cooper, M. Attention deficit hyperactivity disorder. Lancet 2016, 387, 1240–1250. [Google Scholar] [CrossRef]
- Grygiel, P.; Humenny, G.; Rebisz, S.; Bajcar, E.; Switaj, P. Peer Rejection and Perceived Quality of Relations With Schoolmates Among Children With ADHD. J. Atten. Disord. 2018, 22, 738–751. [Google Scholar] [CrossRef] [PubMed]
- DuPaul, G.J.; McGoey, K.E.; Eckert, T.L.; VanBrakle, J. Preschool children with attention-deficit/hyperactivity disorder: Impairments in behavioral, social, and school functioning. J. Am. Acad. Child. Adolesc. Psychiatry 2001, 40, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Peasgood, T.; Bhardwaj, A.; Biggs, K.; Brazier, J.E.; Coghill, D.; Cooper, C.L.; Daley, D.; De Silva, C.; Harpin, V.; Hodgkins, P.; et al. The impact of ADHD on the health and well-being of ADHD children and their siblings. Eur. Child. Adolesc. Psychiatry 2016, 25, 1217–1231. [Google Scholar] [CrossRef]
- Galera, C.; Melchior, M.; Chastang, J.F.; Bouvard, M.P.; Fombonne, E. Childhood and adolescent hyperactivity-inattention symptoms and academic achievement 8 years later: The GAZEL Youth study. Psychol. Med. 2009, 39, 1895–1906. [Google Scholar] [CrossRef]
- Chen, V.C.; Chan, H.L.; Wu, S.I.; Lee, M.; Lu, M.L.; Liang, H.Y.; Dewey, M.E.; Stewart, R.; Lee, C.T. Attention-Deficit/Hyperactivity Disorder and Mortality Risk in Taiwan. JAMA Netw. Open 2019, 2, e198714. [Google Scholar] [CrossRef] [PubMed]
- Dalsgaard, S.; Leckman, J.F.; Mortensen, P.B.; Nielsen, H.S.; Simonsen, M. Effect of drugs on the risk of injuries in children with attention deficit hyperactivity disorder: A prospective cohort study. Lancet Psychiatry 2015, 2, 702–709. [Google Scholar] [CrossRef]
- Herguner, A.; Erdur, A.E.; Basciftci, F.A.; Herguner, S. Attention-deficit/hyperactivity disorder symptoms in children with traumatic dental injuries. Dent. Traumatol. 2015, 31, 140–143. [Google Scholar] [CrossRef]
- Dalsgaard, S.; Ostergaard, S.D.; Leckman, J.F.; Mortensen, P.B.; Pedersen, M.G. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet 2015, 385, 2190–2196. [Google Scholar] [CrossRef]
- Perera, H.; Fernando, S.M.; Yasawardena, A.D.; Karunaratne, I. Prevalence of attention deficit hyperactivity disorder (ADHD) in children presenting with self-inserted nasal and aural foreign bodies. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1362–1364. [Google Scholar] [CrossRef]
- Wei, H.T.; Pan, T.L.; Hsu, J.W.; Huang, K.L.; Bai, Y.M.; Ko, N.Y.; Su, T.P.; Li, C.T.; Tsai, S.J.; Lin, W.C.; et al. Risks of bipolar disorder, depressive disorder, and traumatic brain injury among siblings of patients with attention-deficit hyperactivity disorder. J. Affect. Disord. 2019, 245, 335–339. [Google Scholar] [CrossRef]
- Oerlemans, A.M.; Hartman, C.A.; de Bruijn, Y.G.; Franke, B.; Buitelaar, J.K.; Rommelse, N.N. Cognitive impairments are different in single-incidence and multi-incidence ADHD families. J. Child. Psychol. Psychiatry 2015, 56, 782–791. [Google Scholar] [CrossRef] [PubMed]
- Van Dongen, E.V.; von Rhein, D.; O’Dwyer, L.; Franke, B.; Hartman, C.A.; Heslenfeld, D.J.; Hoekstra, P.J.; Oosterlaan, J.; Rommelse, N.; Buitelaar, J. Distinct effects of ASD and ADHD symptoms on reward anticipation in participants with ADHD, their unaffected siblings and healthy controls: A cross-sectional study. Mol. Autism 2015, 6, 48. [Google Scholar] [CrossRef] [PubMed]
- Chen, V.C.; Yang, Y.H.; Yu Kuo, T.; Lu, M.L.; Tseng, W.T.; Hou, T.Y.; Yeh, J.Y.; Lee, C.T.; Chen, Y.L.; Lee, M.J.; et al. Methylphenidate and the risk of burn injury among children with attention-deficit/hyperactivity disorder. Epidemiol. Psychiatr. Sci. 2020, 29, e146. [Google Scholar] [CrossRef] [PubMed]
- Kendrick, D.; Barlow, J.; Hampshire, A.; Polnay, L.; Stewart-Brown, S. Parenting interventions for the prevention of unintentional injuries in childhood. Cochrane Database Syst. Rev. 2007, CD006020. [Google Scholar] [CrossRef]
- Faraone, S.V.; Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol. Psychiatry 2019, 24, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.N.; Conners, C.K.; Erhardt, D.; Arnold, L.E.; Hechtman, L.; Hinshaw, S.P.; Hoza, B.; Newcorn, J.H.; Swanson, J.M.; Vitiello, B. Familial aggregation of ADHD characteristics. J. Abnorm. Child. Psychol. 2000, 28, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Starck, M.; Grunwald, J.; Schlarb, A.A. Occurrence of ADHD in parents of ADHD children in a clinical sample. Neuropsychiatr. Dis. Treat. 2016, 12, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, Y.; Quintero, J.; Anand, E.; Casillas, M.; Upadhyaya, H.P. Underdiagnosis of attention-deficit/hyperactivity disorder in adult patients: A review of the literature. Prim. Care Companion CNS Disord. 2014, 16. [Google Scholar] [CrossRef]
- Boxhoorn, S.; Lopez, E.; Schmidt, C.; Schulze, D.; Hanig, S.; Cholemkery, H.; Freitag, C.M. Attention as neurocognitive endophenotype of ADHD across the life span: A family study. Eur. Arch. Psychiatry Clin. Neurosci. 2019, 269, 627–644. [Google Scholar] [CrossRef]
- Thissen, A.J.; Rommelse, N.N.; Hoekstra, P.J.; Hartman, C.; Heslenfeld, D.; Luman, M.; van Lieshout, M.; Franke, B.; Oosterlaan, J.; Buitelaar, J.K. Attention deficit hyperactivity disorder (ADHD) and executive functioning in affected and unaffected adolescents and their parents: Challenging the endophenotype construct. Psychol. Med. 2014, 44, 881–892. [Google Scholar] [CrossRef]
- Rogers, M.A.; Wiener, J.; Marton, I.; Tannock, R. Parental involvement in children’s learning: Comparing parents of children with and without Attention-Deficit/Hyperactivity Disorder (ADHD). J. Sch. Psychol. 2009, 47, 167–185. [Google Scholar] [CrossRef] [PubMed]
- Wehmeier, P.M.; Schacht, A.; Barkley, R.A. Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. J. Adolesc. Health 2010, 46, 209–217. [Google Scholar] [CrossRef]
- Fridman, M.; Banaschewski, T.; Sikirica, V.; Quintero, J.; Erder, M.H.; Chen, K.S. Factors associated with caregiver burden among pharmacotherapy-treated children/adolescents with ADHD in the Caregiver Perspective on Pediatric ADHD survey in Europe. Neuropsychiatr. Dis. Treat. 2017, 13, 373–386. [Google Scholar] [CrossRef]
- Li, C.-Y.; Chen, L.-H.; Chiou, M.-J.; Liang, F.-W.; Lu, T.-H. Set-up and future applications of the Taiwan Maternal and Child Health Database (TMCHD). Taiwan J. Public Health 2016, 35, 209–220. [Google Scholar]
- Liu, C.; Hung, Y.; Chuang, Y.; Chen, Y.; Weng, W.; Liu, J.; Liang, K. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar]
- Allison, P.D. Comparing logit and probit coefficients across groups. Sociol. Methods Res. 1999, 28, 186–208. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Su, C.C.; Shao, S.C.; Sung, S.F.; Lin, S.J.; Kao Yang, Y.H.; Lai, E.C. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 2019, 11, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Thapar, A.; Cooper, M.; Eyre, O.; Langley, K. What have we learnt about the causes of ADHD? J. Child. Psychol. Psychiatry 2013, 54, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Babinski, D.E.; Waxmonsky, J.G.; Waschbusch, D.A.; Pelham, W.E., Jr. Behavioral Observations of Parents With ADHD During Parent Training. J. Atten. Disord. 2018, 22, 1289–1296. [Google Scholar] [CrossRef]
- Wang, L.J.; Lee, S.Y.; Yuan, S.S.; Yang, C.J.; Yang, K.C.; Huang, T.S.; Chou, W.J.; Chou, M.C.; Lee, M.J.; Lee, T.L.; et al. Prevalence rates of youths diagnosed with and medicated for ADHD in a nationwide survey in Taiwan from 2000 to 2011. Epidemiol. Psychiatr. Sci. 2017, 26, 624–634. [Google Scholar] [CrossRef]
- Van Emmerik-van Oortmerssen, K.; van de Glind, G.; van den Brink, W.; Smit, F.; Crunelle, C.L.; Swets, M.; Schoevers, R.A. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: A meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012, 122, 11–19. [Google Scholar] [CrossRef]
- Frias, A.; Palma, C.; Farriols, N. Comorbidity in pediatric bipolar disorder: Prevalence, clinical impact, etiology and treatment. J. Affect. Disord. 2015, 174, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Massetti, G.M.; Ouyang, L.; Grosse, S.D.; Mercy, J.A. Attention-deficit/hyperactivity disorder, conduct disorder, and young adult intimate partner violence. Arch. Gen. Psychiatry 2010, 67, 1179–1186. [Google Scholar] [CrossRef]
- Wymbs, B.; Molina, B.; Pelham, W.; Cheong, J.; Gnagy, E.; Belendiuk, K.; Walther, C.; Babinski, D.; Waschbusch, D. Risk of intimate partner violence among young adult males with childhood ADHD. J. Atten. Disord. 2012, 16, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, R.A.; Kallis, C.; Coid, J.W. Adult attention deficit hyperactivity disorder and violence in the population of England: Does comorbidity matter? PLoS ONE 2013, 8, e75575. [Google Scholar] [CrossRef] [PubMed]
- Margari, F.; Craig, F.; Petruzzelli, M.G.; Lamanna, A.; Matera, E.; Margari, L. Parents psychopathology of children with Attention Deficit Hyperactivity Disorder. Res. Dev. Disabil. 2013, 34, 1036–1043. [Google Scholar] [CrossRef]
- Steinhausen, H.C.; Gollner, J.; Brandeis, D.; Muller, U.C.; Valko, L.; Drechsler, R. Psychopathology and personality in parents of children with ADHD. J. Atten. Disord. 2013, 17, 38–46. [Google Scholar] [CrossRef]
- Rice, F.; Riglin, L.; Lomax, T.; Souter, E.; Potter, R.; Smith, D.J.; Thapar, A.K.; Thapar, A. Adolescent and adult differences in major depression symptom profiles. J. Affect. Disord. 2019, 243, 175–181. [Google Scholar] [CrossRef]
- Wundersitz, L. Driver distraction and inattention in fatal and injury crashes: Findings from in-depth road crash data. Traffic Inj. Prev. 2019, 20, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Javalkar, K.; Rak, E.; Phillips, A.; Haberman, C.; Ferris, M.; Van Tilburg, M. Predictors of Caregiver Burden among Mothers of Children with Chronic Conditions. Children (Basel) 2017, 4, 39. [Google Scholar] [CrossRef]
| Variable | Fathers of Children with ADHD | Fathers of Children without ADHD | Mothers of Children with ADHD | Mothers of Children without ADHD |
|---|---|---|---|---|
| N = 81,401 | N = 1,646,100 | N = 87,549 | N = 1,730,941 | |
| Age, Mean (SD) | 42.9 (6.1) | 40.4 (6.9) | 38.9 (5.1) | 37.5 (5.7) |
| Urbanicity, n (%) | ||||
| Urban | 66,073 (81.2) | 1,276,763.0 (77.6) | 70,979 (81.1) | 1,346,539 (77.8) |
| Rural | 15,328 (18.8) | 369,337.0 (22.4) | 16,570 (18.9) | 384,402 (22.2) |
| Low-income, n (%) | 4222 (5.2) | 51,671.0 (3.1) | 4182 (4.8) | 48,560 (2.8) |
| Traumatic injuries, n (%) | ||||
| Burn injury | 3189 (3.9) | 57,694 (3.5) | 4004 (4.6) | 60,365 (3.5) |
| Fracture | 13,451 (16.5) | 247,982 (15.1) | 8047 (9.2) | 129,281 (7.5) |
| Traumatic brain injury | 4721 (5.8) | 88,873 (5.4) | 4396 (5.0) | 68,146 (3.9) |
| Traumatic Injuries | Fathers of Children with ADHD vs. Fathers of Children without ADHD | Mothers of Children with ADHD vs. Mothers of Children without ADHD | Parents of Children with ADHD vs. Parents of Children without ADHD | |||
|---|---|---|---|---|---|---|
| Crude HR (95% CI) | Adjusted HR (95% CI) a | Crude H (95% CI) | Adjusted HR (95% CI) a | Crude HR (95% CI) | Adjusted HR (95% CI) b | |
| Burn injury | 1.19 (1.45–1.23) | 1.23 (1.19–1.27) | 1.33 (1.30–1.36) | 1.35 (1.32–1.38) | 1.24 (1.22–1.26) | 1.30 (1.27–1.32) |
| Fracture | 1.11 (1.09–1.13) | 1.16 (1.14–1.18) | 1.26 (1.24–1.29) | 1.30 (1.28–1.32) | 1.14 (1.13–1.15) | 1.20 (1.22–1.21) |
| Traumatic brain injury | 1.08 (1.05–1.11) | 1.21 (1.17–1.24) | 1.33 (1.30–1.36) | 1.45 (1.42–1.48) | 1.15 (1.13–1.17) | 1.27 (1.25–1.29) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, D.-J.; Chen, Y.-L.; Chen, Y.-Y.; Hsiao, R.C.; Lu, W.-H.; Yen, C.-F. Increased Risk of Traumatic Injuries among Parents of Children with Attention Deficit/Hyperactivity Disorder: A Nationwide Population-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 3586. https://doi.org/10.3390/ijerph18073586
Li D-J, Chen Y-L, Chen Y-Y, Hsiao RC, Lu W-H, Yen C-F. Increased Risk of Traumatic Injuries among Parents of Children with Attention Deficit/Hyperactivity Disorder: A Nationwide Population-Based Study. International Journal of Environmental Research and Public Health. 2021; 18(7):3586. https://doi.org/10.3390/ijerph18073586
Chicago/Turabian StyleLi, Dian-Jeng, Yi-Lung Chen, Ying-Yeh Chen, Ray C. Hsiao, Wei-Hsin Lu, and Cheng-Fang Yen. 2021. "Increased Risk of Traumatic Injuries among Parents of Children with Attention Deficit/Hyperactivity Disorder: A Nationwide Population-Based Study" International Journal of Environmental Research and Public Health 18, no. 7: 3586. https://doi.org/10.3390/ijerph18073586
APA StyleLi, D.-J., Chen, Y.-L., Chen, Y.-Y., Hsiao, R. C., Lu, W.-H., & Yen, C.-F. (2021). Increased Risk of Traumatic Injuries among Parents of Children with Attention Deficit/Hyperactivity Disorder: A Nationwide Population-Based Study. International Journal of Environmental Research and Public Health, 18(7), 3586. https://doi.org/10.3390/ijerph18073586







