Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Types of Participants
2.3. Type of Exposure and Interventions
2.4. Types of Outcomes
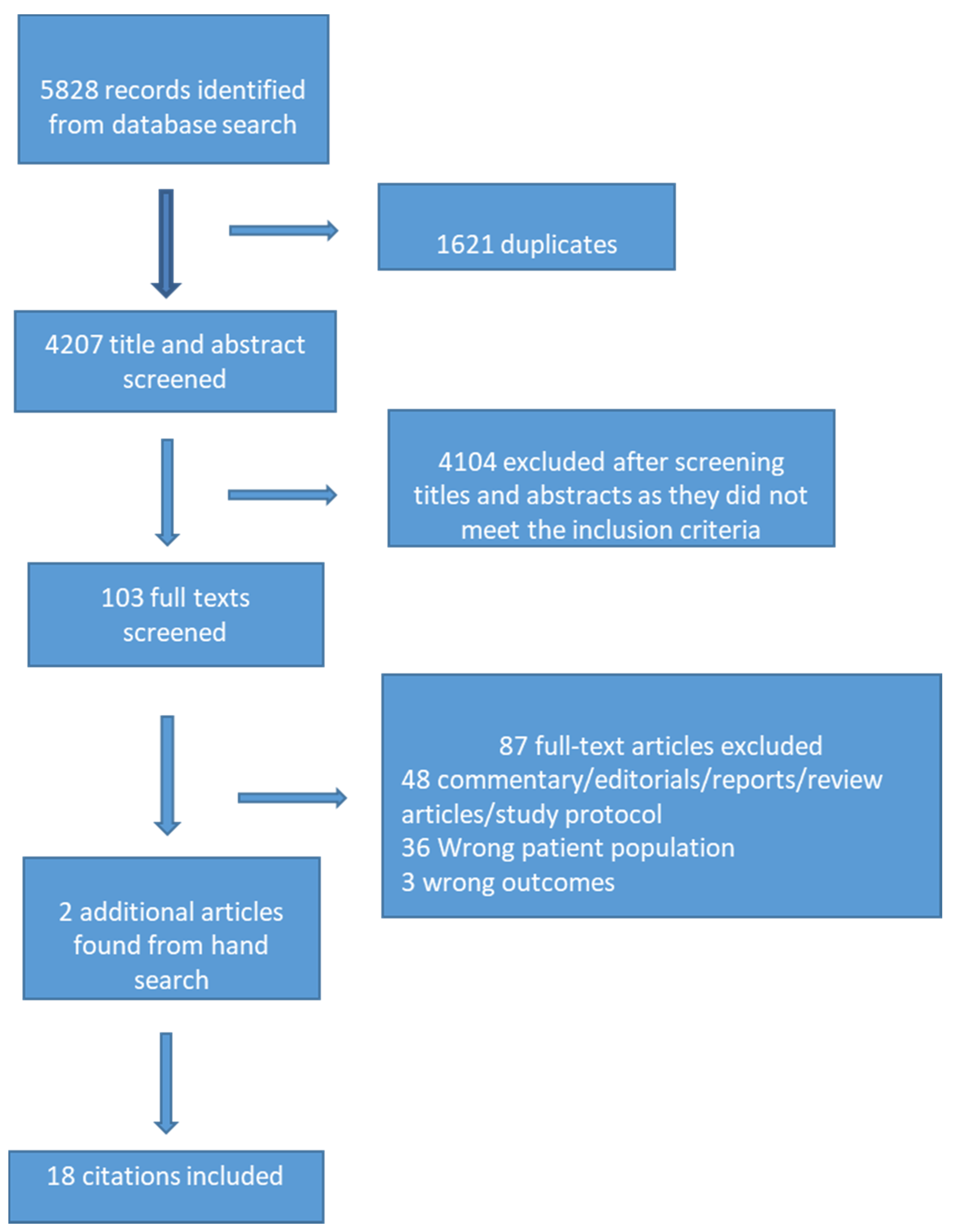
2.5. Study Selection
2.6. Data Extraction
2.7. Quality Assessment
2.8. Data Analysis/Synthesis
3. Results
3.1. Study Characteristics
3.2. Methodological Quality
4. Study Findings
4.1. Impact of the Pandemic on Children’s and Adolescents’ Mental Health
4.2. Impact of Control Measures to Contain the Effect on Children’s and Adolescents’ Mental Health
4.3. Impact of Pandemic/Epidemic Related Stigma on Mental Health
4.4. Interventions Employed during the Previous and Current Pandemic to Promote Children’s and Adolescents’ Mental Health
5. Discussion
Limitations and Future Directions
6. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brooks, S.K.; Smith, L.E.; Webster, R.K.; Weston, D.; Woodland, L.; Hall, I.; Rubin, G.J. The impact of unplanned school closure on children’s social contact: Rapid evidence review. Eurosurveillance 2020, 25, 2000188. [Google Scholar] [CrossRef]
- Lee, J. Mental health effects of school closures during COVID-19. Lancet Child. Adolesc. Health 2020, 4, 421. Available online: https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(20)30109-7/abstract (accessed on 14 March 2021). [CrossRef]
- Smetana, J.G.; Campione-Barr, N.; Metzger, A. Adolescent development in interpersonal and societal contexts. Annu. Rev. Psychol. 2006, 57, 255–284. [Google Scholar] [CrossRef] [PubMed]
- CDC. Helping Children Cope with Emergencies|CDC. 2020. Available online: https://www.cdc.gov/childrenindisasters/helping-children-cope.html (accessed on 14 March 2021).
- Dalton, L.; Rapa, E.; Stein, A. Protecting the psychological health of children through effective communication about COVID-19. Lancet Child. Adolesc. Health 2020, 4, 346–347. Available online: https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(20)30097-3/abstract (accessed on 14 March 2021). [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. Available online: https://www.sciencedirect.com/science/article/pii/S0165178120318382 (accessed on 14 March 2021). [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266.e1. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7127630/ (accessed on 14 March 2021). [CrossRef] [PubMed]
- Elliott, D.S.; Huizinga, D.; Menard, S. Multiple Problem Youth: Delinquency, Substance Use, and Mental Health Problems; Springer: New York, NY, USA, 2012; Available online: https://www.springer.com/gp/book/9780387969251 (accessed on 14 March 2021).
- Hawkins, E.H. A tale of two systems: Co-occurring mental health and substance abuse disorders treatment for adolescents. Annu. Rev. Psychol. 2009, 60, 197–227. [Google Scholar] [CrossRef] [PubMed]
- World Economic Forum. COVID-19 is Hurting Children’s Mental Health. Here’s How to Help|World Economic. 2020. Available online: https://www.weforum.org/agenda/2020/05/covid-19-is-hurting-childrens-mental-health/ (accessed on 16 March 2021).
- WHO. Helping Children Cope with Stress. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/helping-children-cope-with-stress-print.pdf (accessed on 14 March 2021).
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J. Clin. Epidemiol. 2021, 130, 13–22. [Google Scholar] [CrossRef]
- WHO. WHO|Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide. World Health Organization: Geneva, Switzerland, 2017. Available online: http://www.who.int/alliance-hpsr/resources/publications/rapid-review-guide/en/ (accessed on 14 March 2021).
- MedRxiv. medRxiv.org—COVID-19 SARS-CoV-2 Preprints from MedRxiv and BioRxiv. Available online: https://www.medrxiv.org/ (accessed on 14 March 2021).
- ChinaXiv. ChinaXiv.org. Pre-Release Platform for Scientific and Technological Papers of the Chinese Academy of Sciences. 2020. Available online: http://chinaxiv.org/home.htm?locale=en (accessed on 14 March 2021).
- Covidence. Covidence—Better Systematic Review Management. 2019. Available online: https://www.covidence.org/ (accessed on 14 March 2021).
- Decosimo, C.A.; Hanson, J.; Quinn, M.; Badu, P.; Smith, E.G. Playing to live: Outcome evaluation of a community-based psychosocial expressive arts program for children during the Liberian Ebola epidemic. Glob. Ment. Health Camb. Engl. 2019, 6, e3. [Google Scholar] [CrossRef] [PubMed]
- Denis-Ramirez, E.; Sørensen, K.H.; Skovdal, M. In the midst of a ‘perfect storm’: Unpacking the causes and consequences of Ebola-related stigma for children orphaned by Ebola in Sierra Leone. Child. Youth Serv. Rev. 2017, 73, 445–453. Available online: https://www.infona.pl//resource/bwmeta1.element.elsevier-5f7b5e4a-8251-33c0-ac6c-5084d47c6a4a (accessed on 14 March 2021). [CrossRef]
- Kamara, S.; Walder, A.; Duncan, J.; Kabbedijk, A.; Hughes, P.; Muana, A. Mental health care during the Ebola virus disease outbreak in Sierra Leone. Bull. World Health Organ. 2017, 95, 842–847. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5710077/ (accessed on 14 March 2021). [CrossRef] [PubMed]
- Taylor, M.R.; Agho, K.E.; Stevens, G.J.; Raphael, B. Factors influencing psychological distress during a disease epidemic: Data from Australia’s first outbreak of equine influenza. BMC Public Health 2008, 8, 347. [Google Scholar] [CrossRef] [PubMed]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Buzzi, C.; Tucci, M.; Ciprandi, R.; Brambilla, I.; Caimmi, S.; Ciprandi, G.; Marseglia, G.L. The psycho-social effects of COVID-19 on Italian adolescents’ attitudes and behaviors. Ital. J. Pediatr. 2020, 46, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Zheng, D.; Liu, J.; Gong, Y.; Guan, Z.; Lou, D. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav. Immun. 2020, 88, 36–38. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7247496/ (accessed on 14 March 2021). [CrossRef]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7329661/ (accessed on 14 March 2021). [CrossRef]
- Ellis, W.E.; Dumas, T.M.; Forbes, L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. Rev. Can. Sci. Comport. 2020, 52, 177–187. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 841–852. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7173777/ (accessed on 14 March 2021). [CrossRef]
- Liu, S.; Liu, Y.; Liu, Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020, 289, 113070. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7227526/ (accessed on 14 March 2021). [CrossRef]
- Liu, X.; Luo, W.-T.; Li, Y.; Li, C.-N.; Hong, Z.-S.; Chen, H.-L.; Xiao, F.; Xia, J.-Y. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 2020, 9, 58. [Google Scholar] [CrossRef]
- Oosterhoff, B.; Palmer, C.A.; Wilson, J.; Shook, N. Adolescents’ Motivations to Engage in Social Distancing During the COVID-19 Pandemic: Associations with Mental and Social Health. J. Adolesc. Health 2020, 67, 179–185. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7205689/ (accessed on 14 March 2021). [CrossRef]
- Saurabh, K.; Ranjan, S. Compliance and Psychological Impact of Quarantine in Children and Adolescents due to Covid-19 Pandemic. Indian J. Pediatr. 2020, 87, 532–536. [Google Scholar] [CrossRef]
- Tian, F.; Li, H.; Tian, S.; Yang, J.; Shao, J.; Tian, C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020, 288, 112992. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151383/ (accessed on 14 March 2021). [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7084952/ (accessed on 14 March 2021). [CrossRef]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child. Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr. 2020, e201619. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7182958/ (accessed on 14 March 2021).
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. Mixed Methods Appraisal Tool (Mmat) Version 2018 User Guide. 2018. Available online: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2 (accessed on 14 March 2021).
- Kahraman, Ö.; Demirci, E.Ö. Internet addiction and attention-deficit-hyperactivity disorder: Effects of anxiety, depression and self-esteem. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2018, 60, 529–534. [Google Scholar] [CrossRef]
- Soni, R.; Upadhyay, R.; Jain, M. Prevalence of smart phone addiction, sleep quality and associated behaviour problems in adolescents. Int. J. Res. Med. Sci. 2017, 5, 515–519. Available online: https://www.msjonline.org/index.php/ijrms/article/view/2258 (accessed on 14 March 2021). [CrossRef]
- Elledge, C.; Avworo, A.; Cochetti, J.; Carvalho, C.; Grota, P. Characteristics of facilitators in knowledge translation: An integrative review. Collegian 2019, 26, 171–182. Available online: https://www.sciencedirect.com/science/article/pii/S1322769617301920 (accessed on 14 March 2021). [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Types of studies: Quantitative, qualitative, mixed methods studies, experimental (randomized (individually or cluster) and non-randomized controlled trials), observational studies with an internal comparison group (cohort-prospective and retrospective and case-control studies), Human studies Types of participants: studies that are conducted on school age children and adolescents (5 to 19 years), living in low-, middle- or high-income countries without any prior mental health disorder. Type of exposure: Recent COVID-19 or past pandemics (such as SARS-CoV-1, H1N1 influenza, equine influenza, Ebola, MERS-CoV etc.). Interventions delivered to school age children, adolescents and their families to improve mental health and decrease inclination towards substance abuse. Types of outcomes: Primary outcomes: rates of anxiety and depression and use of substance abuse. Secondary outcomes: fear of infection, frustration and boredom, fear of pandemic related uncertainty, fear of running out of basic supplies, and finances. | Not in English Studies that only included adults 18 years old or older Studies that did not report age Studies that included participants with prior mental health problems, those diagnosed with mental health disease, those who are homeless, and those with substance abuse issues. |
| S # | Author and Year | Country | Study Design | Target Population | Total Participants | Exposure | Intervention | Outcomes |
|---|---|---|---|---|---|---|---|---|
| 1 | Decosimo et al., 2019 [17] | Liberia, West Africa | Pre and Post design | 3–18 years | Treatment Group 1 (TG1), (N = 533) Treatment Group 2 (TG2), (N = 337) Total: 870 children | Ebola epidemic | Playing to live intervention including art therapy, play therapy, yoga therapy, support services, trained community facility, and cultural adaptation and community engagement program. TG1 received five months of the program. TG2 received three months of program | Statistically significant decrease in psychological stress symptoms over time before and after receiving the intervention in both treatment groups pre- to post-intervention and a significant difference in total symptoms over time. |
| 2 | Denis-Ramirez et al., 2017 [18] | Sierra Leone, West Africa | Qualitative study—Draw-and-write method | 8–14 years | 24 children | Ebola virus | N/A | Fear, Stigma |
| 3 | Kamara et al., 2017 [19] | Sierra Leone, West Africa | Prospective | 0–17 years | 27 children | Ebola virus | A nurse-led mental health and psychosocial support service via provision of psychotropic medication, psychological intervention, and social intervention | Depression Anxiety Grief Social problems. A nurse-led approach within a non-specialist setting was a successful model for delivering mental health and psychosocial support services during the Ebola outbreak in Sierra Leone. |
| Taylor et al., 2008 [20] | Australia | Cross sectional—online survey | Under 16 years: 36 children 16–24 years: 224 participants | 260 participants | Equine influenza | N/A | Psychological distress | |
| 5 | Sprang et al., 2013 [21] | United States, Canada | Mixed-method approach survey, focus groups, and interviews | Children | 586 Participants | H1N1 | N/A | PTSD |
| 6 | Buzzi et al., 2020 [22] | Italy | Cross sectional—Online survey | 13–19 years girls and boys | 2064 adolescents | COVID-19 | N/A | Consequences on psycho-social well-being |
| 7 | Chen et al., 2020 [23] | Guiyang, China | Cross sectional—Online survey | 6–15 years | 1036 Children Male 531 Female 505 | COVID-19 | N/A | Depression, Anxiety |
| 8 | Duan et al., 2020 [24] | China | Cross-sectional online survey design | 7 to 18 year | 3613 students 1812 males 1801 females | COVID-19 | N/A | Anxiety Symptoms, Depressive symptoms, Coping mechanisms |
| 9 | Ellis et al., 2020 [25] | Ontario, Canada | Cross-sectional online survey design | 14–18 years | 1054 Participants | COVID-19 | N/A | Stress, Loneliness, Depression |
| 10 | Liang et al., 2020 [26] | China | Cross-Sectional online survey | 14–20 years | 130 youths | COVID-19 | N/A | PTSD, Coping styles, Mental health |
| 11 | Liu et al., 2020a [27] | Sichuan, China | Cross-sectional online survey | 10–12 years 5–6 grade | 209 primary school students Girls 93 Boys 116 | COVID-19 | N/A | Psychosomatic symptoms, Psychological distress |
| 12 | X. Liu et al., 2020b [28] | China | Cross-sectional online survey design | Below 18 years | 34 participants | COVID-19 | N/A | Anxiety, Depression, Psychological abnormalities |
| 13 | Oosterhoff et l., 2020 [29] | United States | Cross sectional—Online survey | 13–18 years | 683 adolescents | COVID-19 | N/A | Anxiety symptoms. Depressive symptoms burdensomeness, belongingness |
| 14 | Saurabh et al., 2020 [30] | India | Cross sectional—survey questionnaire | 9–18 years | 252 children and adolescents | COVID-19 | N/A | Worry, Helplessness, Fear |
| 15 | Tian et al., 2020 [31] | China | Cross-sectional online survey | Children under 18 years | 22 participants | COVID-19 | N/A | Psychological symptoms |
| 16 | Wang et al., 2020 [32] | China | Cross-sectional online survey design | 12–21.4 years | 344 participants | COVID-19 | N/A | Stress, Anxiety, Depression |
| 17 | Zhou et al., 2020 [33] | China | Cross-sectional—online survey | 12–18 years | 8079 participants | COVID-19 | N/A | Depression, Anxiety |
| 18 | Xie et al., 2020 [34] | Hubei, China | Cross-sectional online survey design | Children grade 2–6 | 1784 Students | COVID-19 | N/A | Anxiety Symptoms, Depressive symptoms |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meherali, S.; Punjani, N.; Louie-Poon, S.; Abdul Rahim, K.; Das, J.K.; Salam, R.A.; Lassi, Z.S. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3432. https://doi.org/10.3390/ijerph18073432
Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, Lassi ZS. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(7):3432. https://doi.org/10.3390/ijerph18073432
Chicago/Turabian StyleMeherali, Salima, Neelam Punjani, Samantha Louie-Poon, Komal Abdul Rahim, Jai K. Das, Rehana A. Salam, and Zohra S. Lassi. 2021. "Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review" International Journal of Environmental Research and Public Health 18, no. 7: 3432. https://doi.org/10.3390/ijerph18073432
APA StyleMeherali, S., Punjani, N., Louie-Poon, S., Abdul Rahim, K., Das, J. K., Salam, R. A., & Lassi, Z. S. (2021). Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. International Journal of Environmental Research and Public Health, 18(7), 3432. https://doi.org/10.3390/ijerph18073432








