Mass Casualty Decontamination for Chemical Incidents: Research Outcomes and Future Priorities
Abstract
1. Introduction
2. Key Findings from Mass Casualty Decontamination Research
2.1. Speed Is Critical
2.2. The Importance of Disrobing
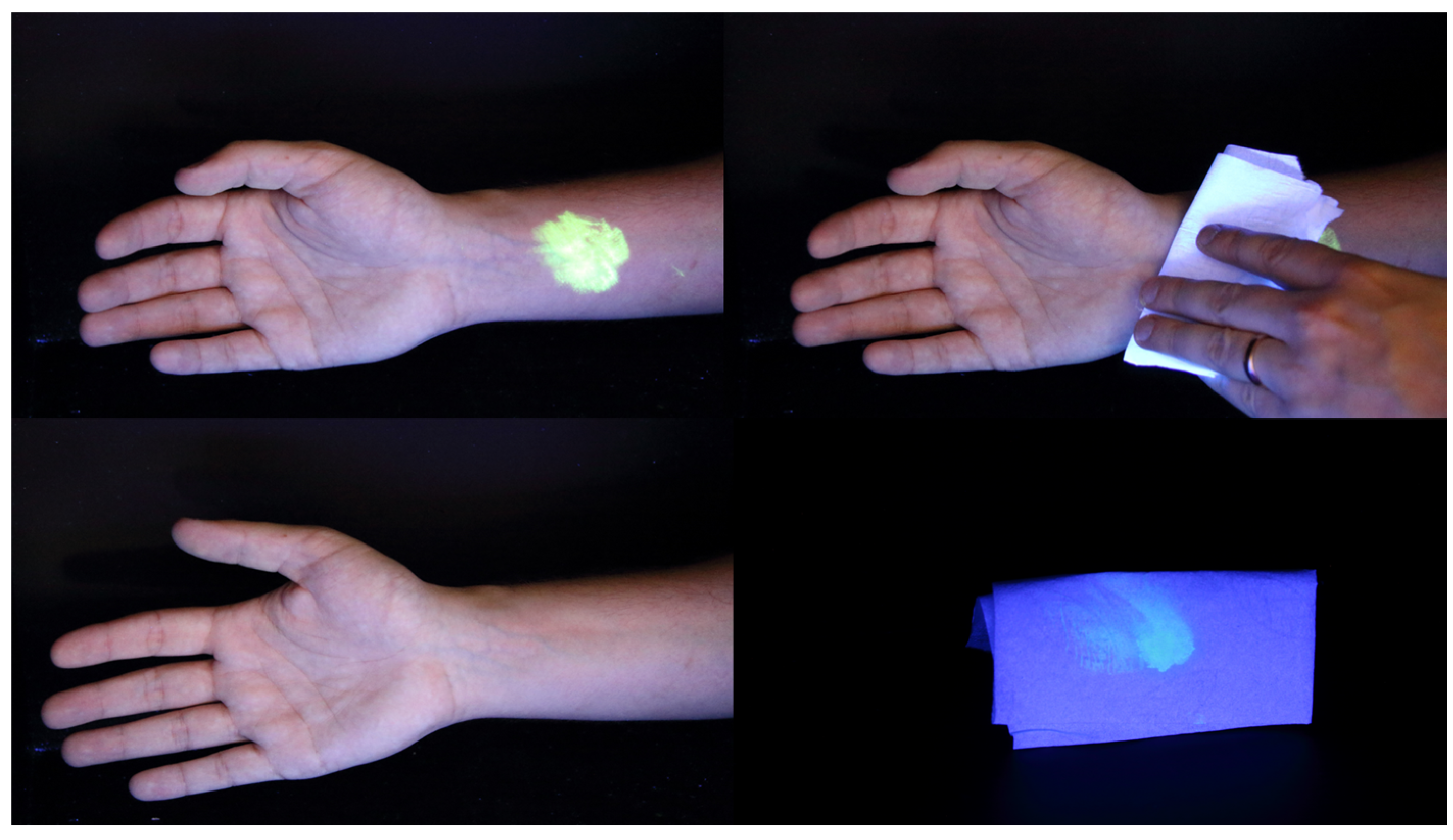
2.3. Dry Decontamination of Skin Is an Effective Intervention for Liquids When Initiated in a Timely Manner
2.4. There Are Optimised Parameters for Mass Decontamination Showering
2.5. Decontamination Methods Have Variable Efficacy for Liquid Contaminated Hair
2.6. Multiple Decontamination Interventions Performed in Sequence Are More Efficacious That Single Interventions Alone
2.7. Decontamination Must Be Casualty Focused to Facilitate Compliance
- (1)
- Communicate openly and honestly, providing regular updates about the nature of the incident and the actions that they are taking. Providing this information increases perceptions that responders are managing an incident in a fair and legitimate way and increases public willingness to comply with decontamination [42,63,65,66,68].
- (2)
- Communicate in a health-focused way about the need for decontamination. This includes explaining the nature of the threat (from contamination) and the efficacy of decontamination measures for reducing that threat [68]. This will ensure that members of the public understand the need for decontamination [61,63], and that they perceive the instruction to undertake decontamination as legitimate, thus increasing willingness to comply with decontamination instructions [42,62,66,67]. Specifically, responders should communicate: why decontamination is necessary, in terms of removing a contaminant from the skin and preventing any further risks to health; how decontamination will protect someone and their loved ones (e.g., reducing the risk of secondary contamination); and what decontamination will involve.
- (3)
- Casualties must also be able to effectively conduct decontamination. Evidence from decontamination exercises and field trials reveals that for both wet [62,63,66] and dry decontamination [18], provision of sufficient practical information is crucial for ensuring that casualties are able to effectively undertake decontamination, and that the process runs as smoothly and efficiently as possible.
- (4)
- To promote legitimacy of response, and hence increase casualties’ compliance, emergency responders must demonstrate respect for casualties’ needs. Demonstrating respect for casualties’ privacy and modesty will promote willingness to comply with decontamination [61,62,63,66]. While it may not always be possible to provide casualties with as much privacy as they would like, where this is not possible casualties’ concerns should be acknowledged, and the reasons for lack of privacy should be explained.
- (5)
- Respect members of vulnerable groups. There are four functional categories that may make someone more vulnerable during decontamination reduced ability to physically undertake decontamination; difficulty hearing or understanding decontamination instructions; social or cultural factors that make undergoing decontamination more difficult; existing health factors that may make them either more susceptible to the effects of the contaminant, or put them at increased risk while undergoing decontamination [69]. Responders must receive training and guidance for managing members of vulnerable groups and should put strategies in place to manage an incident involving these groups. As part of this process, responders should treat each individual as an expert in his or her own needs [69,70,71] demonstrating respect for casualties’ specific needs.
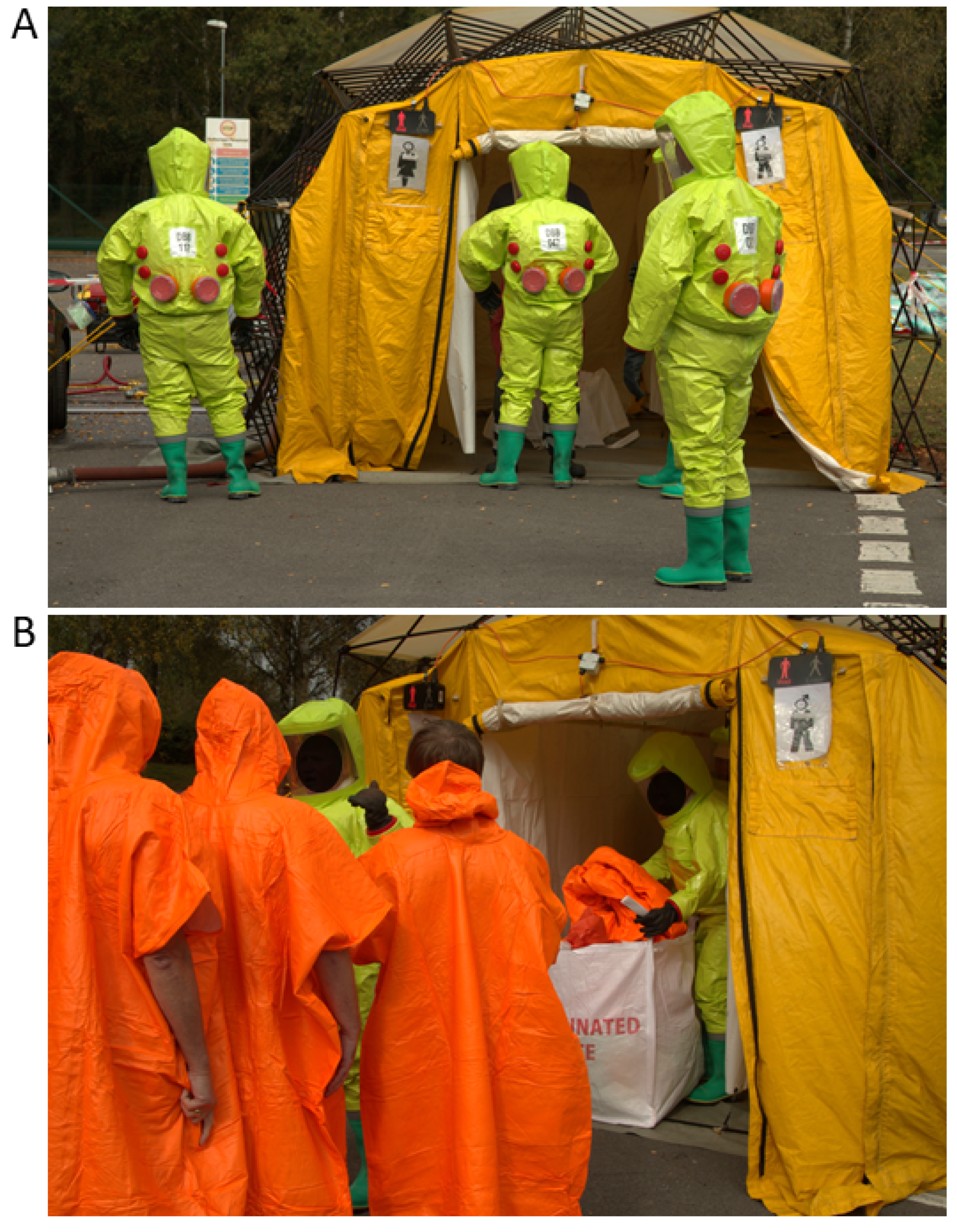
2.8. Decontamination Approaches Can Be Modified for Non-Ambulant Casualties and ‘Vulnerable Groups’
3. Future Research Priorities
3.1. The Risks from Chemical Vapours
3.2. The Choice of Chemical Simulant for Human Volunteer Studies
3.3. Accurately Assessing Systemic Exposure
3.4. The Significance of the ‘Wash-In’ Effect
3.5. Improved Communication Strategies
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- WHO. Manual for the Public Health Management of Chemical Incidents; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Wisner, B.; Adams, J. Environmental Health in Emergencies and Disasters: A Practical Guide; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Bos, P.; Ruijten, M.; Gundert-Remy, U.; Bull, S.; Nielsen, E.; Tissot, S.; Wood, M.; Cassel, G.; Russel, D.; Leffler, P.; et al. Human Risk Assessment of Single Exposure in Chemical Incidents: Present Situation and Emerging Chemical Incident Scenarios; RIVM: Bilthoven, The Netherlands, 2013. [Google Scholar]
- Genereux, M.; Petit, G.; Maltais, D.; Roy, M.; Simard, R.; Boivin, S.; Shultz, J.M.; Pinsonneault, L. The public health response during and after the Lac-Megantic train derailment tragedy: A case study. Disaster Health 2014, 2, 113–120. [Google Scholar] [CrossRef]
- Zhao, B. Facts and lessons related to the explosion accident in Tianjin Port, China. Nat. Hazards 2016, 84, 707–713. [Google Scholar] [CrossRef]
- Yap, C.K.; Peng, S.H.T.; Leow, C.S. Contamination in Pasir Gudang Area, Peninsular Malaysia: What can we learn from Kim Kim River chemical waste contamination? J. Humanit. Educ. Dev. 2019, 1, 84–87. [Google Scholar] [CrossRef]
- Ahmed, F.; Maroof, H.; Ahmed, N.; Sheridan, R. Acid attacks: A new public health pandemic in the west? Int. J. Surg. 2017, 48, 32–33. [Google Scholar] [CrossRef]
- United Nations. United Nations Mission to Investigate Allegations of the Use of Chemical Weapons in the Syrian Arab Republic; Final Report; United Nations: New York, NY, USA, 2013. [Google Scholar]
- OPCW. Report on the Use of a Chemical Weapon in the Death of a DPRK National; OPCW: The Hague, The Netherlands, 2017. [Google Scholar]
- Vale, J.A.; Marrs, T.O.; Maynard, R.C. Novichok: A murderous nerve agent attack in the UK. Clin. Toxicol. 2018, 56, 1093–1097. [Google Scholar] [CrossRef]
- Bongers, S.; Janssen, N.A.; Reiss, B.; Grievink, L.; Lebret, E.; Kromhout, H. Challenges of exposure assessment for health studies in the aftermath of chemical incidents and disasters. J. Expo Sci. Environ. Epidemiol. 2008, 18, 341–359. [Google Scholar] [CrossRef]
- Baker, D. The problem of secondary contamination following chemical agent release. Crit. Care 2005, 9, 323–324. [Google Scholar] [CrossRef] [PubMed]
- NHS England Emergency Preparedness, Resilience and Response. Concept of Operations for Managing Mass Casualties; NHS England: London, UK, 2017. [Google Scholar]
- Kirk, M.A.; Deaton, M.L. Bringing order out of chaos: Effective strategies for medical response to mass chemical exposure. Emerg. Med. Clin. N. Am. 2007, 25, 527–548. [Google Scholar] [CrossRef] [PubMed]
- Scanlon, J. Chemically contaminated casualties: Different problems and possible solutions. Am. J. Disaster Med. 2010, 5, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Leary, A.D.; Schwartz, M.D.; Kirk, M.A.; Ignacio, J.S.; Wencil, E.B.; Cibulsky, S.M. Evidence-based patient decontamination: An integral component of mass exposure chemical incident planning and response. Disaster Med. Public Health Prep. 2014, 8, 260–266. [Google Scholar] [CrossRef]
- Okumura, T.; Hisaoka, T.; Yamada, A.; Naito, T.; Isonuma, H.; Okumura, S.; Miura, K.; Sakurada, M.; Maekawa, H.; Ishimatsu, S.; et al. The Tokyo subway sarin attack—Lessons learned. Toxicol. Appl. Pharmacol. 2005, 207, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Amlôt, R.; Carter, H.; Riddle, L.; Larner, J.; Chilcott, R.P. Volunteer trials of a novel improvised dry decontamination protocol for use during mass casualty incidents as part of the UK’S Initial Operational Response (IOR). PLoS ONE 2017, 12, e0179309. [Google Scholar] [CrossRef]
- Amlot, R.; Larner, J.; Matar, H.; Jones, D.R.; Carter, H.; Turner, E.A.; Price, S.C.; Chilcott, R.P. Comparative analysis of showering protocols for mass-casualty decontamination. Prehosp. Disaster Med. 2010, 25, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Egan, J.R.; Amlôt, R. Modelling mass casualty decontamination systems informed by field exercise data. Int. J. Environ. Res. Public Health 2012, 9, 3685–3710. [Google Scholar] [CrossRef] [PubMed]
- Kassouf, N.; Syed, S.; Larner, J.; Amlôt, R.; Chilcott, R.P. Evaluation of absorbent materials for use as ad hoc dry decontaminants during mass casualty incidents as part of the UK’s Initial Operational Response (IOR). PLoS ONE 2017, 12, e0170966. [Google Scholar] [CrossRef]
- Optimisation through Research of Chemical Incident Decontamination Systems. Available online: http://www.orchidsproject.eu/project.html (accessed on 1 March 2021).
- Home Office. Initial Operational Response to a CBRN Incident. 2015. Available online: https://www.jesip.org.uk/uploads/media/pdf/CBRN%20JOPs/IOR_Guidance_V2_July_2015.pdf (accessed on 4 September 2020).
- Programme, J.E.S.I. Responding to a CBRN(e) Event: Joint Operating Principles for the Emergency Services. 2016. Available online: https://www.jesip.org.uk/uploads/media/pdf/CBRN%20JOPs/JESIP_CBRN_E_JOPS_Document_On.pdf (accessed on 4 September 2020).
- Chilcott, R.P.; Amlôt, R. (Eds.) Primary Response Incident Scene Management (PRISM) Guidance for Chemical Incidents; Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority: Washington, DC, USA, 2015.
- Chilcott, R.; Larner, J.; Matar, H. Primary Response Incident Scene Management: PRISM Guidance, 2nd ed.; Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority: Washington, DC, USA, 2018; Volume 1.
- Orchids Project. Available online: http://www.orchidsproject.eu (accessed on 17 June 2019).
- Chilcott, R.P.; Larner, J.; Durrant, A.; Hughes, P.; Mahalingam, D.; Rivers, S.; Thomas, E.; Amer, N.; Barrett, M.; Matar, H.; et al. Evaluation of US Federal Guidelines (Primary Response Incident Scene Management [PRISM]) for Mass Decontamination of Casualties During the Initial Operational Response to a Chemical Incident. Ann. Emerg. Med. 2018, 73, 671–684. [Google Scholar] [CrossRef]
- Chilcott, R.P. Managing mass casualties and decontamination. Environ. Int. 2014, 72, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Feldman, R.J. Chemical agent simulant release from clothing following vapor exposure. Acad. Emerg. Med. 2010, 17, 221–224. [Google Scholar] [CrossRef]
- Matar, H.; Price, S.C.; Chilcott, R.P. Temporal effects of disrobing on the skin absorption of chemical warfare agents and CW agent simulants. Toxicology 2010, 278, 344–345. [Google Scholar] [CrossRef]
- Gaskin, S.; Pisaniello, D.; Edwards, J.W.; Bromwich, D.; Reed, S.; Logan, M.; Baxter, C. Chlorine and hydrogen cyanide gas interactions with human skin: In vitro studies to inform skin permeation and decontamination in HAZMAT incidents. J. Hazard. Mater. 2013, 262, 759–765. [Google Scholar] [CrossRef]
- Power, S.; Symons, C.; Carter, H.; Jones, E.; Amlot, R.; Larner, J.; Matar, H.; Chilcott, R.P. Mass Casualty Decontamination in the United States: An Online Survey of Current Practice. Health Secur. 2016, 14, 226–236. [Google Scholar] [CrossRef]
- Chilcott, R.P.; Mitchell, H.; Matar, H. Optimization of Nonambulant Mass Casualty Decontamination Protocols as Part of an Initial or Specialist Operational Response to Chemical Incidents. Prehosp. Emerg. Care 2018, 23, 32–43. [Google Scholar] [CrossRef]
- Chilcott, R.P.; Wyke, S.M. CBRN Incidents. In Health Emergency Preparedness and Response; Sellwood, C., Wapling, A., Eds.; CABI: Wallingford, UK, 2016; pp. 167–180. [Google Scholar]
- Chilcott, R.P. Dermal aspects of chemical warface agents. In Chemical Warfare Agents: Toxicology and Treatment, 2nd ed.; Marrs, T., Maynard, R., Sidell, F., Eds.; John Wiley and Sons: Hoboken, NJ, USA, 2007; pp. 409–422. [Google Scholar]
- Butler, D. UK rolls out terror-attack plan. Nature 2014, 506, 139–140. [Google Scholar] [CrossRef]
- Taysse, L.; Daulon, S.; Delamanche, S.; Bellier, B.; Breton, P. Skin decontamination of mustards and organophosphates: Comparative efficiency of RSDL and Fuller’s earth in domestic swine. Hum. Exp. Toxicol. 2007, 26, 135–141. [Google Scholar] [CrossRef]
- Lademann, J.; Patzelt, A.; Schanzer, S.; Richter, H.; Gross, I.; Menting, K.H.; Frazier, L.; Sterry, W.; Antoniou, C. Decontamination of the skin with absorbing materials. Skin Pharmacol. Physiol. 2011, 24, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Matar, H.; Guerreiro, A.; Piletsky, S.A.; Price, S.C.; Chilcott, R.P. Preliminary evaluation of military, commercial and novel skin decontamination products against a chemical warfare agent simulant (methyl salicylate). Cutan. Ocul. Toxicol. 2016, 35, 137–144. [Google Scholar] [CrossRef]
- Southworth, F.; James, T.; Davidson, L.; Williams, N.; Finnie, T.; Marczylo, T.; Collins, S.; Amlot, R. A controlled cross-over study to evaluate the efficacy of improvised dry and wet emergency decontamination protocols for chemical incidents. PLoS ONE 2020, 15, e0239845. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.; Weston, D.; Betts, N.; Wilkinson, S.; Amlôt, R. Public perceptions of emergency decontamination: Effects of intervention type and responder management strategy during a focus group study. PLoS ONE 2018, 13, e0195922. [Google Scholar] [CrossRef] [PubMed]
- Evaluation, Optimisation, Trialling and Modelling Procedures for Mass Patient Decontamination [ORCHIDS] [200723]—Project 2011. Available online: https://webgate.ec.europa.eu/chafea_pdb/health/projects/2007203/outputs (accessed on 4 September 2020).
- Amlot, R.; Riddle, L.; Chilcott, R.P. Minimum Practical Showering Duration for Mass Patient Decontamination; Chemical Toxicology Report No. 23; Health Protection Agency: Porton Down, UK, 2011. [Google Scholar]
- Moody, R.P.; Maibach, H.I. Skin decontamination: Importance of the wash-in effect. Food Chem. Toxicol. 2006, 44, 1783–1788. [Google Scholar] [CrossRef]
- Joseph, R.E.; Tsai, W.-J.; Tsao, L.-I.; Su, T.-P.; Cone, E.J. In Vitro Characterization of Cocaine Binding Sites in Human Hair. J. Pharmacol. Exp. Ther. 1997, 282, 1228–1241. [Google Scholar]
- Oxley, J.C.; Smith, J.L.; Kirschenbaum, L.J.; Shinde, K.P.; Marimganti, S. Accumulation of explosives in hair. J. Forensic. Sci. 2005, 50, 826–831. [Google Scholar] [CrossRef]
- Rolland, P.; Bolzinger, M.A.; Cruz, C.; Josse, D.; Briançon, S. Hairy skin exposure to VX in vitro: Effectiveness of delayed decontamination. Toxicol. In Vitro 2013, 27, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Matar, H.; Amer, N.; Kansagra, S.; Pinhal, A.; Thomas, E.; Townend, S.; Larner, J.; Chilcott, R.P. Hybrid in vitro diffusion cell for simultaneous evaluation of hair and skin decontamination: Temporal distribution of chemical contaminants. Sci. Rep. 2018, 8, 16906. [Google Scholar] [CrossRef] [PubMed]
- Grams, Y.Y.; Whitehead, L.; Lamers, G.; Sturmann, N.; Bouwstra, J.A. On-line diffusion profile of a lipophilic model dye in different depths of a hair follicle in human scalp skin. J. Invest. Dermatol. 2005, 125, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Rolland, P.; Bolzinger, M.A.; Cruz, C.; Briancon, S.; Josse, D. Human scalp permeability to the chemical warfare agent VX. Toxicol. In Vitro 2011, 25, 1974–1980. [Google Scholar] [CrossRef] [PubMed]
- Josse, D.; Wartelle, J.; Cruz, C. Showering effectiveness for human hair decontamination of the nerve agent VX. Chem. Biol. Interact. 2015, 232, 94–100. [Google Scholar] [CrossRef]
- Spiandore, M.; Piram, A.; Lacoste, A.; Prevost, P.; Maloni, P.; Torre, F.; Asia, L.; Josse, D.; Doumenq, P. Efficacy of scalp hair decontamination following exposure to vapours of sulphur mustard simulants 2-chloroethyl ethyl sulphide and methyl salicylate. Chem. Biol. Interact. 2017, 267, 74–79. [Google Scholar] [CrossRef]
- Spiandore, M.; Souilah-Edib, M.; Piram, A.; Lacoste, A.; Josse, D.; Doumenq, P. Desorption of sulphur mustard simulants methyl salicylate and 2-chloroethyl ethyl sulphide from contaminated scalp hair after vapour exposure. Chemosphere 2018, 191, 721–728. [Google Scholar] [CrossRef]
- Collins, S.; James, T.; Southworth, F.; Davidson, L.; Williams, N.; Orchard, E.; Marczylo, T.; Amlot, R. Human volunteer study of the decontamination of chemically contaminated hair and the consequences for systemic exposure. Sci. Rep. 2020, 10, 20822. [Google Scholar] [CrossRef]
- James, T.; Collins, S.; Amlôt, R.; Marczylo, T. GC–MS/MS quantification of benzyl salicylate on skin and hair: A novel chemical simulant for human decontamination studies. J. Chromatogr. B 2019, 1129, 121818. [Google Scholar] [CrossRef]
- Franca, T.C.C.; Kitagawa, D.A.S.; Cavalcante, S.F.d.A.; da Silva, J.A.V.; Nepovimova, E.; Kuca, K. Novichoks: The Dangerous Fourth Generation of Chemical Weapons. Int. J. Mol. Sci. 2019, 20, 1222. [Google Scholar] [CrossRef] [PubMed]
- Davidson, L.; Southworth, F.; Collins, S.; Williams, N.; James, T.; Orchard, E.; Marczylo, T.; Amlôt, R. Improved mass casualty decontamination following a chemical incident: A combination of improvised and interim protocols in a controlled cross-over volunteer study. PLoS ONE 2021. Submitted. [Google Scholar]
- Collins, S.; Williams, N.; Southworth, F.; James, T.; Davidson, L.; Orchard, E.; Marczylo, T.; Amlot, R. Evaluating the impact of decontamination interventions performed in sequence for mass casualty chemical incidents. Emerg. Med. J. 2021. Submitted. [Google Scholar]
- Larner, J.; Durrant, A.; Hughes, P.; Mahalingam, D.; Rivers, S.; Matar, H.; Thomas, E.; Barrett, M.; Pinhal, A.; Amer, N.; et al. Efficacy of Different Hair and Skin Decontamination Strategies with Identification of Associated Hazards to First Responders. Prehosp. Emerg. Care 2019, 24, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.; Drury, J.; Rubin, G.J.; Williams, R.; Amlot, R. Public experiences of mass casualty decontamination. Biosecur. Bioterror. 2012, 10, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.; Drury, J.; Amlot, R.; Rubin, G.; Williams, R. Perceived responder legitimacy and group identification predict cooperation and compliance in a mass decontamination field exercise. Basic Appl. Soc. Psychol. 2013, 35, 575–585. [Google Scholar] [CrossRef]
- Carter, H.; Drury, J.; Rubin, G.J.; Williams, R.; Amlôt, R. The effect of communication during mass decontamination. Disaster Prev. Manag. Int. J. 2013, 22, 132–147. [Google Scholar] [CrossRef]
- Carter, H.; Amlôt, R. Mass Casualty Decontamination Guidance and Psychosocial Aspects of CBRN Incident Management: A Review and Synthesis. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carter, H.; Drury, J.; Amlot, R.; Rubin, G.; Williams, R. Effective responder communication, perceived responder legitimacy, and group identification predict public cooperation and compliance in a mass decontamination visualization experiment. J. Appl. Soc. Psychol. 2015, 45, 173–189. [Google Scholar] [CrossRef]
- Carter, H.; Drury, J.; Amlot, R.; Rubin, G.J.; Williams, R. Effective responder communication improves efficiency and psychological outcomes in a mass decontamination field experiment: Implications for public behaviour in the event of a chemical incident. PLoS ONE 2014, 9, e89846. [Google Scholar] [CrossRef]
- Carter, H.; Drury, J.; Rubin, G.J.; Williams, R.; Amlot, R. Applying crowd psychology to develop recommendations for the management of mass decontamination. Health Secur. 2015, 13, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Symons, C.; Amlot, R.; Carter, H.; Rubin, G.J. Effects of threat and efficacy messages on expected adherence to decontamination protocols in an immersive simulated chemical incident: A randomized controlled experiment. J. Contingencies Crisis Manag. 2021, 29, 54–76. [Google Scholar] [CrossRef]
- Carter, H.; Amlôt, R.; Williams, R.; Rubin, G.J.; Drury, J. Mass Casualty Decontamination in a Chemical or Radiological/Nuclear Incident: Further Guiding Principles. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef]
- Taylor, K.; Balfanz-Vertiz, K.; Humrickhouse, R.; Truitt, A. Decontamination of people with spinal cord injury: Best practices and lessons learned. SCI Psychosoc. Process 2008, 21, 15–25. [Google Scholar]
- Taylor, K.; Balfanz-Vertiz, K.; Humrickhouse, R.; Jurik, C. Decontamination with at-risk populations: Lessons learned. Internet J. Rescue Disaster Med. 2008, 9, 1–18. Available online: https://pdfs.semanticscholar.org/b9b9/c243fec92beab3f4586ee8cac36b7cae7b67.pdf (accessed on 4 September 2020).
- Monteith, R. Validation of a Hazmat/CBRN Decontamination Protocol within a Canadian Context. Master’s Thesis, Royal Roads University, Victoria, BC, Canada, 2013. [Google Scholar]
- Turner, L.; Jewkes, F.; Amlôt, R.; Simpson, J. Exercise Young Neptune: Mass Decontamination of Children Field Exercise; Health Protection Agency: London, UK, 2007. [Google Scholar]
- Carter, H.; Drury, J.; Amlôt, R. Social Identity and Intergroup Relationships in the Management of Crowds during Mass Emergencies and Disasters: Recommendations for Emergency Planners and Responders. Polic. J. Policy Pract. 2018, 14, 931–944. [Google Scholar] [CrossRef]
- Drury, J.; Novelli, D.; Stott, C. Representing crowd behaviour in emergency planning guidance: ‘mass panic’ or collective resilience? Resilience 2013, 1, 18–37. [Google Scholar] [CrossRef]
- Bakker, M.H.; Kerstholt, J.H.; Giebels, E. Deciding to Help: Effects of Risk and Crisis Communication. J. Contingencies Crisis Manag. 2018, 26, 113–126. [Google Scholar] [CrossRef]
- Stubbé, H.E.; van Emmerik, M.L.; Kerstholt, J.H. Helping behavior in a virtual crisis situation: Effects of safety awareness and crisis communication. J. Risk Res. 2017, 20, 433–444. [Google Scholar] [CrossRef]
- Ribordy, P.; Rocksen, D.; Dellgar, U.; Persson, S.A.; Arnoldsson, K.; Ekasen, H.; Haggbom, S.; Nerf, O.; Ljungqvist, A.; Gryth, D.; et al. Mobile decontamination units-room for improvement? Prehosp. Disaster Med. 2012, 27, 425–431. [Google Scholar] [CrossRef]
- Moffett, P.M.; Baker, B.L.; Kang, C.S.; Johnson, M.S. Evaluation of time required for water-only decontamination of an oil-based agent. Mil. Med. 2010, 175, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Matar, H.; Atkinson, K.L.; Kansagra, S.; Larner, J.; Amlôt, R.; Chilcott, R.P. Advanced Studies of Mass Decontamination Milestone M4: Effects of Hydrodynamics, Detergents and Delays on the Effectiveness of the Ladder Pipe Decontamination System—Studies with Methyl Salicylate and Curcumin-Methyl Salicylate Mixture; Report No: TDDT-14-07A; University of Hertfordshire: Hatfield, UK, 2014. [Google Scholar]
- Amlôt, R.; Symons, C.; Jones, E.; Bredbere, S.; Cavell, B.; Carter, H.; Larner, J.; Viegas, V.A.; Shetage, S.S.; Chilcott, R.P. Advanced Studies of Mass Decontamination Milestone M5: Effects of Hydrodynamics and Disrobing on the Effectiveness of the Ladder Pipe Decontamination System. Human Volunteer Studies with a CW Agent Simulant; Report No: TDDT-15-08A; University of Hertfordshire: Hatfield, UK, 2015. [Google Scholar]
- Symons, C.; Jones, E.; Bredbere, S.; Amlôt, R.; Larner, J.; Shetage, S.S.; Viegas, V.A.; Chilcott, R.P. Advanced Studies of Mass Decontamination Milestone M6: Effects of Delays on the Effectiveness of the Ladder Pipe Decontamination System. Human Volunteer Studies with a CW Agent Simulant; Report No: TDDT-15-07A; University of Hertfordshire: Hatfield, UK, 2015. [Google Scholar]
- Symons, C.; Jones, E.; Bredbere, S.; Cavell, B.; Amlôt, R.; Larner, J.; Shetage, S.S.; Viegas, V.A.; Chilcott, R.P. Advanced Studies of Mass Decontamination Milestone M8: Effects of Detergents on the Effectiveness of the Ladder Pipe Decontamination System. Human Volunteer Studies with a CW Agent Simulant; University of Hertfordshire: Hatfield, UK, 2015. [Google Scholar]
- James, T.; Wyke, S.; Marczylo, T.; Collins, S.; Gaulton, T.; Foxall, K.; Amlot, R.; Duarte-Davidson, R. Chemical warfare agent simulants for human volunteer trials of emergency decontamination: A systematic review. J. Appl. Toxicol. 2018, 38, 113–121. [Google Scholar] [CrossRef] [PubMed]
- James, T.; Collins, S.; Amlot, R.; Marczylo, T. Analysis of Chemical Simulants in Urine: A Useful Tool for Assessing Emergency Decontamination Efficacy in Human Volunteer Studies. Prehosp. Disaster Med. 2020, 35, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Moody, R.P.; Nadeau, B. In vitro dermal absorption of two commercial formulations of 2,4-dichlorophenoxyacetic acid dimethylamine (2,4-D amine) in rat, guinea pig and human skin. Toxicol. In Vitro 1997, 11, 251–262. [Google Scholar] [CrossRef]
- Moody, R.P.; Nadeau, B.; Chu, I. In vitro dermal absorption of N,N-Diethyl-m-toluamide (DEET) in rat, guinea pig, and human skin. Vitro Toxicol. 1995, 8, 263–275. [Google Scholar]
- Moody, R.P.; Nadeau, B.; Chu, I. In vitro dermal absorption of pesticides: VI. In vivo and in vitro comparison of the organochlorine insecticide DDT in rat, guinea pig, pig, human and tissue-cultured skin. Toxicol. In Vitro 1994, 8, 1225–1232. [Google Scholar] [CrossRef]
- Misik, J.; Pavlikova, R.; Josse, D.; Cabal, J.; Kuca, K. In vitro skin permeation and decontamination of the organophosphorus pesticide paraoxon under various physical conditions—Evidence for a wash-in effect. Toxicol. Mech. Methods 2012, 22, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Filon, F.L.; Boeniger, M.; Maina, G.; Adami, G.; Spinelli, P.; Damian, A. Skin absorption of inorganic lead (PbO) and the effect of skin cleansers. J. Occup. Environ. Med. 2006, 48, 692–699. [Google Scholar] [CrossRef]
- Loke, W.K.; Soo-Hway, U.; Lau, S.K.; Lim, J.S.; Tay, G.S.; Koh, C.H. Wet decontamination-induced stratum corneum hydration--effects on the skin barrier function to diethylmalonate. J. Appl. Toxicol. 1999, 19, 285–290. [Google Scholar] [CrossRef]
- Moody, R.P.; Nadeau, B. An automated in vitro dermal absorption procedure: III. In vivo and in vitro comparison with the insect repellent N,N-diethyl-m-toluamide in mouse, rat, guinea pig, pig, human and tissue-cultured skin. Toxicol. In Vitro 1993, 7, 167–176. [Google Scholar] [CrossRef]
- Misik, J.; Pavlik, M.; Novotny, L.; Pavlikova, R.; Chilcott, R.P.; Cabal, J.; Kuca, K. In vivo decontamination of the nerve agent VX using the domestic swine model. Clin. Toxicol. 2012, 50, 807–811. [Google Scholar] [CrossRef] [PubMed]
- Thors, L.; Koch, M.; Wigenstam, E.; Koch, B.; Hagglund, L.; Bucht, A. Comparison of skin decontamination efficacy of commercial decontamination products following exposure to VX on human skin. Chem. Biol. Interact. 2017, 273, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Bjarnason, S.; Mikler, J.; Hill, I.; Tenn, C.; Garrett, M.; Caddy, N.; Sawyer, T.W. Comparison of selected skin decontaminant products and regimens against VX in domestic swine. Hum. Exp. Toxicol. 2008, 27, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.; Drury, J.; Amlôt, R. Understanding the Impact of Responder Management Strategies on Public Experiences and Behaviour during Mass Casualty Decontamination. In Skin Decontamination: A Comprehensive Clinical Research Guide; Zhu, H., Maibach, H.I., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 199–210. [Google Scholar] [CrossRef]
- Carter, H.E.; Gauntlett, L.; Amlot, R. Public Perceptions of the “Remove, Remove, Remove” Information Campaign Before and During a Hazardous Materials Incident: A Survey. Health Secur. 2021, 19, 100–107. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Conditions |
|---|---|
| Temperature | 35 °C |
| Duration | 90 s |
| Active washing | Provision of cotton wash cloths |
| Detergent | 0.5% detergent solution |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collins, S.; James, T.; Carter, H.; Symons, C.; Southworth, F.; Foxall, K.; Marczylo, T.; Amlôt, R. Mass Casualty Decontamination for Chemical Incidents: Research Outcomes and Future Priorities. Int. J. Environ. Res. Public Health 2021, 18, 3079. https://doi.org/10.3390/ijerph18063079
Collins S, James T, Carter H, Symons C, Southworth F, Foxall K, Marczylo T, Amlôt R. Mass Casualty Decontamination for Chemical Incidents: Research Outcomes and Future Priorities. International Journal of Environmental Research and Public Health. 2021; 18(6):3079. https://doi.org/10.3390/ijerph18063079
Chicago/Turabian StyleCollins, Samuel, Thomas James, Holly Carter, Charles Symons, Felicity Southworth, Kerry Foxall, Tim Marczylo, and Richard Amlôt. 2021. "Mass Casualty Decontamination for Chemical Incidents: Research Outcomes and Future Priorities" International Journal of Environmental Research and Public Health 18, no. 6: 3079. https://doi.org/10.3390/ijerph18063079
APA StyleCollins, S., James, T., Carter, H., Symons, C., Southworth, F., Foxall, K., Marczylo, T., & Amlôt, R. (2021). Mass Casualty Decontamination for Chemical Incidents: Research Outcomes and Future Priorities. International Journal of Environmental Research and Public Health, 18(6), 3079. https://doi.org/10.3390/ijerph18063079








