Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
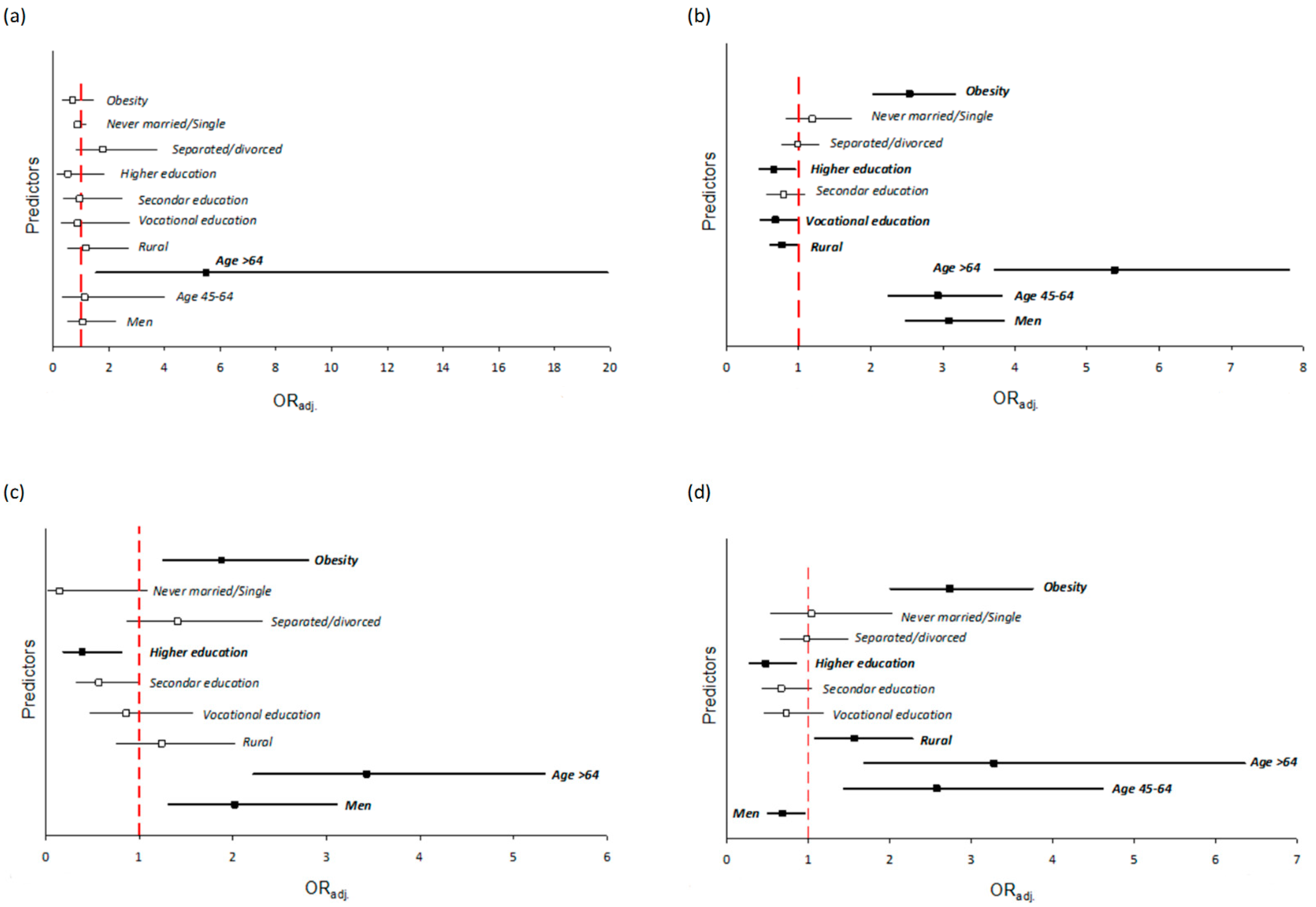
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight Factsheets. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 3 September 2020).
- NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef] [Green Version]
- Eurostat. Overweight and Obesity—BMI Statistics in European Union. Available online: https://ec.europa.eu/eurostat/statistics-explained/pdfscache/12376.pdf (accessed on 3 September 2020).
- Wojtyła-Buciora, P.; Bołdowski, T.; Wojtyła, C.; Żukiewicz-Sobczak, W.; Juszczak, K.; Chęcińska-Maciejewska, Z.; Wojtyła, A.; Krauss, H. National survey of body mass and dietary behaviour for middle school, high school and university students. J. Health Inequal. 2017, 1, 64–69. [Google Scholar] [CrossRef] [Green Version]
- Harton, A.; Myszkowska-Ryciak, J.; Laskowski, W.; Gajewska, D. Prevalence of overweight and obesity among adolescents in Poland. J. Health Inequal. 2019, 5, 180–187. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization Regional Office for Europe. Overweight and Obesity in Europe: Factsheets. Available online: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics (accessed on 3 September 2020).
- Główny Urząd Statystyczny. Zdrowie i Zachowanie Zdrowotne Mieszkańców Polski w Świetle Europejskiego Ankietowego Badania Zdrowia (EHIS) 2014 r; Statistics Poland: Warsaw, Poland, 2015. [Google Scholar]
- Eurostat. European Health Interview Survey. Available online: https://ec.europa.eu/eurostat/web/microdata/european-health-interview-survey (accessed on 25 January 2021).
- Stepaniak, U.; Micek, A.; Waśkiewicz, A.; Bielecki, W.; Drygas, W.; Janion, M.; Kozakiewicz, K.; Niklas, A.; Puch-Walczak, A.; Pająk, A. Prevalence of general and abdominal obesity and overweight among adults in Poland Results of the WOBASZ II study (2013–2014) and comparison with the WOBASZ study (2003–2005). Polskie Archiwum Medycyny Wewnętrznej 2016, 126, 662–671. [Google Scholar] [CrossRef] [Green Version]
- Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet 2009, 373, 1083–1096. [Google Scholar] [CrossRef] [Green Version]
- Chow, W.H.; Dong, L.M.; Devesa, S.S. Epidemiology and risk factors for kidney cancer. Nat. Rev. Urol. 2010, 7, 245–257. [Google Scholar] [CrossRef]
- Knight, J.A. Diseases and Disorders Associated with Excess Body Weight. Ann. Clin. Lab. Sci 2011, 41, 107–121. Available online: http://www.annclinlabsci.org/content/41/2/107.long (accessed on 3 September 2020).
- World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective A Summary of the Third Expert Report. 2018. Available online: www.dietandcancerreport.org (accessed on 3 September 2020).
- Dragomir, M.; Mullie, P.; Bota, M.; Koechlin, A.; Macacu, A.; Pizot, C.; Boyle, P. Nutrition and prostate cancer: Review of the evidence. J. Health Inequal. 2019, 5, 155–173. [Google Scholar] [CrossRef]
- Zdrojewski, T. Completing the cardiovascular revolution: Smoking, alcohol, diet, and air pollution. J. Health Inequal. 2019, 5, 38. [Google Scholar] [CrossRef]
- Fontaine, K.R.; Redden, D.T.; Wang, C.; Westfall, A.O.; Allison, D.B. Years of life lost due to obesity. J. Am. Med. Assoc. 2003, 289, 187–193. [Google Scholar] [CrossRef]
- Tremmel, M.; Gerdtham, U.G.; Nilsson, P.M.; Saha, S. Economic burden of obesity: A systematic literature review. Int. J. Environ. Res. Public Health 2017, 14, 435. [Google Scholar] [CrossRef]
- Krzyżanowska-Świniarska, B. Otyłość Prosta. In Podręcznik Chorób Wewnętrznych; Andrzej, S., Ed.; Medycyna Praktyczna: Krakow, Poland, 2012; pp. 1369–1373. Available online: https://medbook.com.pl/ksiazka/pokaz/id/5172/tytul/choroby-wewnetrzne-tom-1-szczeklik-medycyna-praktyczna (accessed on 3 September 2020).
- Jarosz, M.; Respondek, W.; Rychlik, W. Economical and health-related consequences of overweight and obesity and other chronic non-communicable diseases. In Obesity, Nutrition, Physical Activity, Health of Poles. Diagnosis of nutritional Status, Physical Activity and Nutritional Risk Factors of Obesity and Chronic Non-Communicable Diseases in Poland; Jarosz, M., Ed.; Insytut Żywności i Żywienia: Warszawa, Poland, 2006; Available online: https://w.bibliotece.pl/2215960/Otyłość+żywienie+aktywność+fizyczna+zdrowie+Polaków (accessed on 3 September 2020).
- Zatońska, K.; Zatoński, W.A.; Szuba, A. Prospective urban and rural epidemiology Poland—Study design. J. Health Inequal. 2016, 2, 136–141. [Google Scholar] [CrossRef]
- Teo, K.; Chow, C.K.; Vaz, M.; Rangarajan, S.; Yusuf, S. The Prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am. Heart J. 2009, 158, 1–7.e1. [Google Scholar] [CrossRef]
- Polskie Towarzystwo Diabetologiczne. Zalecenia Kliniczne Dotyczące Postępowania u Chorych na Cukrzycę 2019. Diabetologia Praktyczna 2019, 5, 100. [Google Scholar]
- Szuba, A.; Martynowicz, H.; Zatońska, K.; Ilow, R.; Regulska-Ilow, B.; Różańska, D.; Wołyniec, M.; Połtyn-Zaradna, K.; Zatoński, W. Prevalence of hypertension in Polish population of PURE Poland study. J. Health Inequal. 2017, 2, 157–162. [Google Scholar] [CrossRef] [Green Version]
- Biela, U.; Pajak, A.; Kaczmarczyk-Chałas, K.; Głuszek, J.; Tendera, M.; Waśkiewicz, A.; Kurjata, P.; Wyrzykowski, B. Incidence of overweight and obesity in women and men between the ages of 20–74. Results of the WOBASZ program. Kardiologia Polska 2005, 63, 632–635. Available online: https://pubmed.ncbi.nlm.nih.gov/20527435/ (accessed on 3 September 2020).
- Matyjaszczyk, P.; Hoffmann, K.; Bryl, W. Epidemiology of chosen risk factors of cardiovascular diseases. Przegląd Kardiodiabetologiczny 2011, 6, 255–262. Available online: https://www.termedia.pl/Artykul-pogladowy-Epidemiologia-wybranych-czynnikow-ryzyka-chorob-ukladu-krazenia,47.18065.0.0.html (accessed on 3 September 2020).
- Zatonska, K.; Janik-Koncewicz, K.; Ilow, R.; Regulska-Ilow, B.; Rozanska, D.; Szuba, A.; Einhorn, J.; Vatten, L.; Xiao-Mei, M.; Janszky, I.; et al. Prevalence of obesity—Baseline assessment in the prospective cohort ‘PONS’ study. Ann. Agric. Environ. Med. 2011, 18, 246–250. Available online: http://www.aaem.pl/Prevalence-of-obesity-baseline-assessment-in-the-prospective-cohort-PONS-study.71691.0.2.html (accessed on 3 September 2020).
- Vainio, H.; Kaaks, R.; Bianchini, F. Weight control and physical activity in cancer prevention: International evaluation of the evidence. Eur. J. Cancer Prev. 2002, 11, 94–100. Available online: https://pubmed.ncbi.nlm.nih.gov/12570341/ (accessed on 3 September 2020).
- Jarosz, M.; Rychlik, E. Overweight and obesity among adults in Poland, 1983–2005. Adv. Med. Sci. 2008, 53, 158–166. [Google Scholar] [CrossRef] [Green Version]
- Ogden, C.L.; Carrol, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012, 82, 1–8. Available online: https://pubmed.ncbi.nlm.nih.gov/22617494/ (accessed on 3 September 2020).
- Befort, C.A.; Nazir, N.; Perri, M.G. Prevalence of Obesity Among Adults from Rural and Urban Areas of the United States: Findings from NHANES (2005–2008). J. Rural Health 2012, 28, 392–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, K.A.; Gall, S.L.; Venn, A.J.; Otahal, P.; Blizzard, L.; Dwyer, T.; Cleland, V.J. Accumulated exposure to rural areas of residence over the life course is associated with overweight and obesity in adulthood: A 25-year prospective cohort study. Ann. Epidemiol. 2017, 27, 169–175.e2. [Google Scholar] [CrossRef]
- Jokela, M.; Kivimäki, M.; Elovainio, M.; Viikari, J.; Raitakari, O.T.; Keltikangas-Järvinen, L. Urban/rural differences in body weight: Evidence for social selection and causation hypotheses in Finland. Soc. Sci. Med. 2009, 68, 867–875. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Boyle, P.; Anderson, B.O.; Andersson, L.C.; Ariyaratne, Y.; Auleley, G.R.; Barbacid, M.; Bartelink, H.; Baselga, J.; Behbehani, K.; Belardelli, F.; et al. Need for global action for cancer control. Ann. Oncol. 2008, 19, 1519–1521. [Google Scholar] [CrossRef]
- Mongraw-Chaffin, M.L.; Peters, S.A.; Huxley, R.R.; Woodward, M. The sex-specific association between BMI and coronary heart disease: A systematic review and meta-analysis of 95 cohorts with 1·2 million participants. Lancet Diabetes Endocrinol. 2015, 3, 437–449. [Google Scholar] [CrossRef] [Green Version]
- Field, A.E.; Coakley, E.H.; Must, A.; Spadano, J.L.; Laird, N.; Dietz, W.H.; Rimm, E.; Colditz, G.A. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch. Intern. Med. 2001, 161, 1581–1586. [Google Scholar] [CrossRef]
- Rutkowski, M.; Bandosz, P.; Czupryniak, L.; Gaciong, Z.; Solnica, B.; Jasiel-Wojculewicz, H.; Wyrzykowski, B.; Pencina, M.J.; Zdrojewski, T. Prevalence of diabetes and impaired fasting glucose in Poland-the NATPOL 2011 Study. Diabet. Med. 2014, 31, 1568–1571. [Google Scholar] [CrossRef]
- Jarosz, M.; Rychlik, E. Obesity—Health and Global Challenge. 2011. Available online: http://www.pnmedycznych.pl/wp-content/uploads/2014/09/pnm_2011_712_717.pdf (accessed on 3 September 2020).
- Artham, S.M.; Lavie, C.J.; Milani, R.V.; Ventura, H.O. Obesity and hypertension, heart failure, and coronary heart disease - Risk factor, paradox, and recommendations for weight loss. Ochsner J. 2009, 9, 124–132. [Google Scholar]
| Variables | N | BMI (kg/m2) | p-Value * | |||
|---|---|---|---|---|---|---|
| <18.5 N = 15 | 18.5–24.9 N = 571 | 25.0–29.9 N = 817 | ≥30.0 N = 632 | |||
| Total | 2035 | 0.7% (15) | 28.1% (571) | 40.1% (817) | 31.1% (632) | |
| Sex: | <0.001 | |||||
| Men | 754 | 0.4% (3) | 20.8% (157) | 47.8% (360) | 31.0% (234) | |
| Women | 1281 | 0.9% (12) | 32.3% (414) | 35.7% (457) | 31.1% (398) | |
| Place of residence: | <0.001 | |||||
| Urban | 1210 | 0.7% (9) | 30.2% (365) | 43.1% (522) | 26.0% (314) | |
| Rural | 825 | 0.7% (6) | 25.0% (206) | 35.8% (295) | 38.5% (318) | |
| Age, years: | <0.001 | |||||
| 30–44 | 358 | 1.4% (5) | 43.6% (156) | 35.2% (126) | 19.8% (71) | |
| 45–64 | 1350 | 0.6% (8) | 25.9% (350) | 40.8% (551) | 32.7% (441) | |
| >64 | 327 | 0.6% (2) | 19.9% (65) | 42.8% (140) | 36.7% (120) | |
| Level of education: | <0.001 | |||||
| Primary | 301 | 0.7% (2) | 18.2% (55) | 35.9% (108) | 45.2% (136) | |
| Vocational | 324 | 1.2% (4) | 25.9% (84) | 37.1% (120) | 35.8% (116) | |
| Secondary | 796 | 0.6% (5) | 28.6% (228) | 40.5% (322) | 30.3% (241) | |
| Higher | 603 | 0.7% (4) | 33.7% (203) | 42.9% (259) | 22.7% (137) | |
| Lack of information | 11 | 0.0% (0) | 9.1% (1) | 72.7% (8) | 18.2% (2) | |
| Marital status: | 0.016 | |||||
| Married/living together | 1508 | 0.7% (10) | 27.6% (417) | 41.2% (621) | 30.5% (460) | |
| Separated/divorced | 375 | 0.3% (1) | 28.5% (107) | 36.0% (135) | 35.2% (132) | |
| Never married/single | 146 | 2.7% (4) | 32.2% (47) | 38.4% (56) | 26.7% (39) | |
| Lack of information | 6 | 0.0% (0) | 0.0% (0) | 83.3% (5) | 16.6% (1) | |
| Stroke | 38 | 0.0% (0) | 23.7% (9) | 47.4% (18) | 28.9% (11) | 0.767 |
| CHD | 112 | 0.0% (0) | 16.1% (18) | 34.8% (39) | 49.1% (55) | <0.001 |
| Hypertension | 1217 | 0.5% (6) | 19.2% (234) | 41.7% (507) | 38.6% (470) | <0.001 |
| Diabetes | 200 | 0.0% (0) | 12.5% (25) | 30.0% (60) | 57.5% (115) | <0.001 |
| Variable | Obesity | p-Value | ORadj. (95% CI) | |||
|---|---|---|---|---|---|---|
| Yes N = 632 | No N = 1403 | |||||
| n | % | n | % | |||
| Sex: | 0.974 | |||||
| Women | 398 | 63.0 | 883 | 62.9 | 1.00 (ref.) | |
| Men | 234 | 37.0 | 520 | 37.1 | 0.99 (0.81–1.20) a | |
| Age group: | <0.001 | |||||
| 30–44 | 71 | 11.2 | 287 | 20.5 | 1.00 (ref.) | |
| 45–64 | 441 | 69.8 | 909 | 64.8 | 1.76 (1.42–2.17) b | |
| >64 | 120 | 19.0 | 207 | 14.8 | 1.91 (1.36–2.70) b | |
| Place of residence: | <0.001 | |||||
| Urban | 314 | 49.7 | 896 | 63.9 | 1.00 (ref.) | |
| Rural | 318 | 50.3 | 507 | 36.1 | 1.79 (1.48–2.16) c | |
| Level of education: | <0.001 | |||||
| Primary | 136 | 21.6 | 165 | 11.8 | 1.00 (ref.) | |
| Vocational | 116 | 18.4 | 208 | 14.9 | 0.84 (0.75–0.93) c | |
| Secondary | 241 | 38.3 | 555 | 39.8 | 0.69 (0.66–0.95) c | |
| Higher | 137 | 21.7 | 466 | 33.4 | 0.42 (0.34–0.56) c | |
| Marital status: | 0.105 | |||||
| Living together | 460 | 72.9 | 1048 | 75.0 | 1.00 (ref.) | |
| Separated | 132 | 20.9 | 243 | 17.4 | 0.84 (0.75–1.23) c | |
| Single | 39 | 6.2 | 107 | 7.7 | 0.88 (0.79–1.19) c | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zatońska, K.; Psikus, P.; Basiak-Rasała, A.; Stępnicka, Z.; Gaweł-Dąbrowska, D.; Wołyniec, M.; Gibka, J.; Szuba, A.; Połtyn-Zaradna, K. Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 2701. https://doi.org/10.3390/ijerph18052701
Zatońska K, Psikus P, Basiak-Rasała A, Stępnicka Z, Gaweł-Dąbrowska D, Wołyniec M, Gibka J, Szuba A, Połtyn-Zaradna K. Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(5):2701. https://doi.org/10.3390/ijerph18052701
Chicago/Turabian StyleZatońska, Katarzyna, Piotr Psikus, Alicja Basiak-Rasała, Zuzanna Stępnicka, Dagmara Gaweł-Dąbrowska, Maria Wołyniec, Julia Gibka, Andrzej Szuba, and Katarzyna Połtyn-Zaradna. 2021. "Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study" International Journal of Environmental Research and Public Health 18, no. 5: 2701. https://doi.org/10.3390/ijerph18052701
APA StyleZatońska, K., Psikus, P., Basiak-Rasała, A., Stępnicka, Z., Gaweł-Dąbrowska, D., Wołyniec, M., Gibka, J., Szuba, A., & Połtyn-Zaradna, K. (2021). Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. International Journal of Environmental Research and Public Health, 18(5), 2701. https://doi.org/10.3390/ijerph18052701






