Social Contact with Family and Non-Family Members Differentially Affects Physical Activity: A Parallel Latent Growth Curve Modeling Approach
Abstract
1. Introduction
2. Materials and Methods
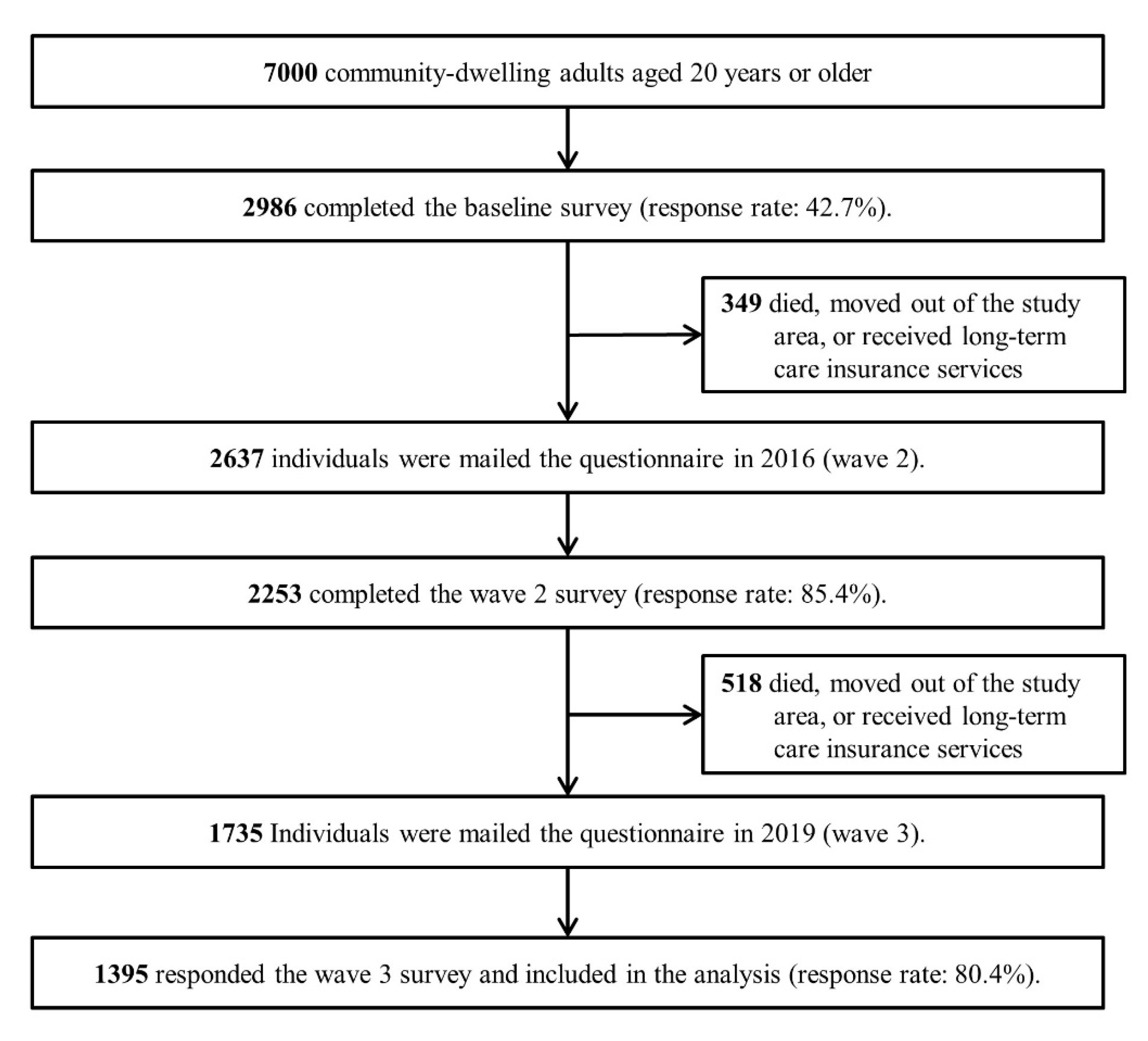
2.1. Study Design and Participants
2.2. Measurements
2.2.1. Physical Activity
2.2.2. Social Contact
2.3. Covariates
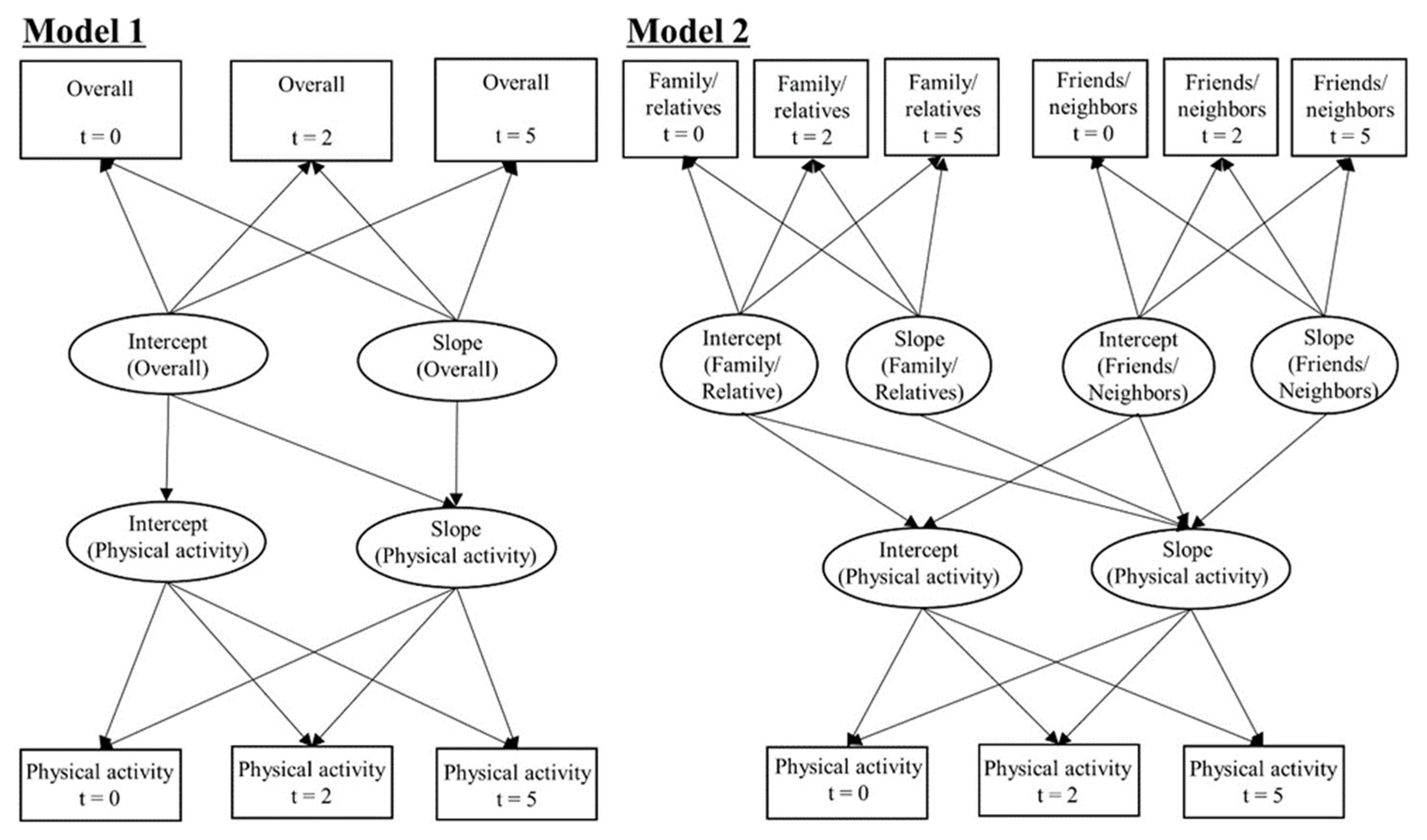
2.4. Statistical Analysis
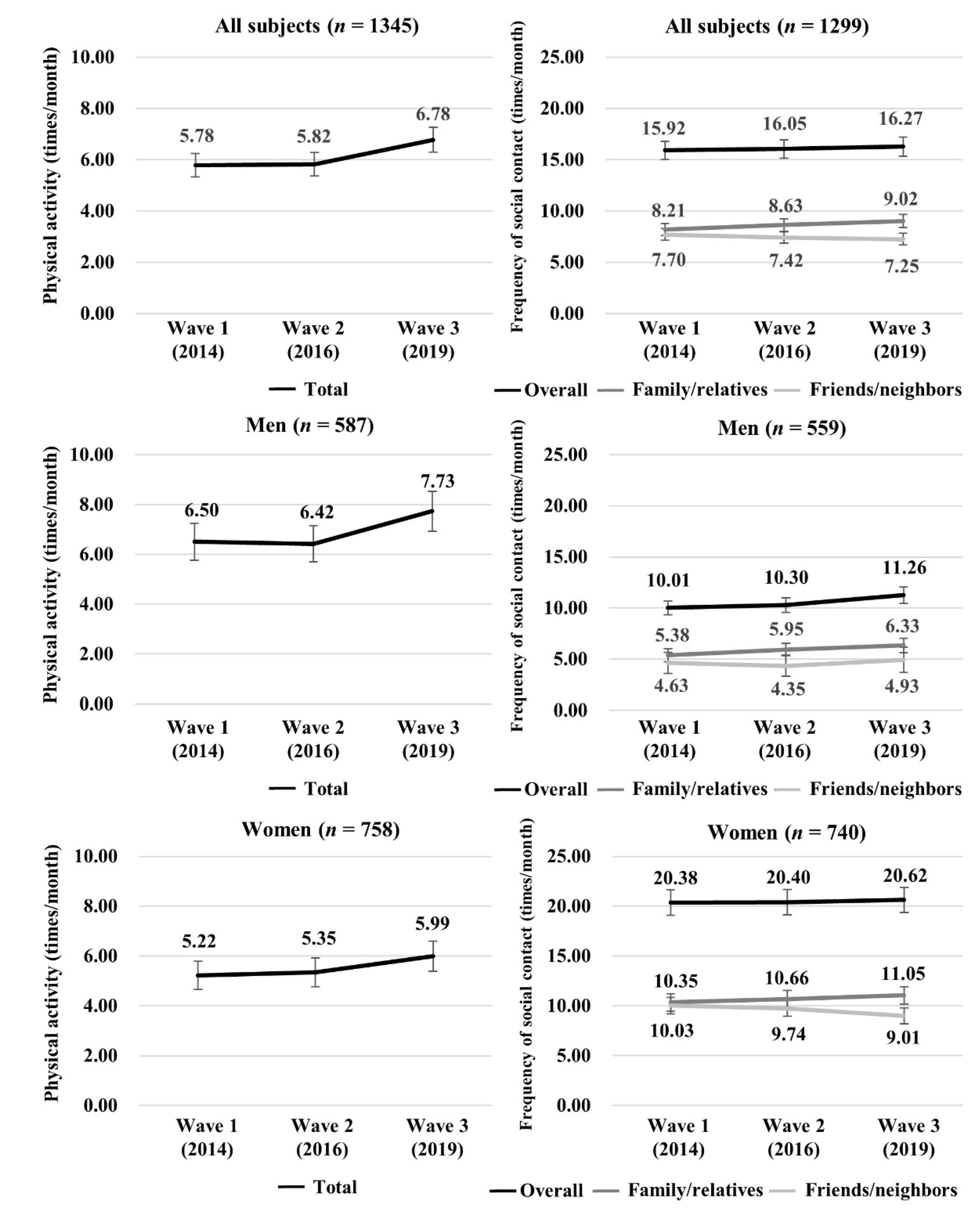
3. Results
4. Discussion
4.1. Trajectories of PA and Social Contact over Five Years
4.2. Longitudinal Association of Social Contact with PA
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “Active Aging”. Gerontologist 2016, 56 (Suppl. 2), S268–S280. [Google Scholar] [CrossRef]
- World Health Organization Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf?ua=1 (accessed on 6 August 2020).
- Lobelo, F.; Rohm Young, D.; Sallis, R.; Garber, M.D.; Billinger, S.A.; Duperly, J.; Hutber, A.; Pate, R.R.; Thomas, R.J.; Widlansky, M.E.; et al. Routine Assessment and Promotion of Physical Activity in Healthcare Settings: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e495–e522. [Google Scholar] [CrossRef]
- Warburton, D.E.; Charlesworth, S.; Ivey, A.; Nettlefold, L.; Bredin, S.S. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 39. [Google Scholar] [CrossRef]
- Guthold, R.; Ono, T.; Strong, K.L.; Chatterji, S.; Morabia, A. Worldwide variability in physical inactivity a 51-country survey. Am. J. Prev. Med. 2008, 34, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Labour and Welfare National Health and Nutrition Survey Japan. 2018. Available online: https://www.mhlw.go.jp/content/10900000/000635990.pdf (accessed on 6 August 2020).
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Berkman, L. Social Cohesion, Social Capital, and Health. In Social Epidemiology; Berkman, L., Kawachi, I., Eds.; Oxford University Press: Oxford, UK, 2000; pp. 174–190. [Google Scholar]
- Samuel, L.J.; Commodore-Mensah, Y.; Himmelfarb, C.R. Developing Behavioral Theory with the Systematic Integration of Community Social Capital Concepts. Health Educ Behav 2014, 41, 359–375. [Google Scholar] [CrossRef] [PubMed]
- Seino, S.; Kitamura, A.; Nishi, M.; Tomine, Y.; Tanaka, I.; Taniguchi, Y.; Yokoyama, Y.; Amano, H.; Narita, M.; Ikeuchi, T.; et al. Individual- and community-level neighbor relationships and physical activity among older Japanese adults living in a metropolitan area: A cross-sectional multilevel analysis. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 46. [Google Scholar] [CrossRef]
- Kepper, M.M.; Myers, C.A.; Denstel, K.D.; Hunter, R.F.; Guan, W.; Broyles, S.T. The neighborhood social environment and physical activity: A systematic scoping review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 124. [Google Scholar] [CrossRef]
- McNeill, L.H.; Kreuter, M.W.; Subramanian, S.V. Social environment and physical activity: A review of concepts and evidence. Soc. Sci. Med. 2006, 63, 1011–1022. [Google Scholar] [CrossRef]
- Bohm, A.W.; Mielke, G.I.; da Cruz, M.F.; Ramirez, V.V.; Wehrmesister, F.C. Social Support and Leisure-Time Physical Activity Among the Elderly: A Population-Based Study. J. Phys. Act. Health 2016, 13, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef]
- Cable, N.; Bartley, M.; Chandola, T.; Sacker, A. Friends are equally important to men and women, but family matters more for men’s well-being. J. Epidemiol. Community Health 2013, 67, 166–171. [Google Scholar] [CrossRef]
- Cable, N.; Chandola, T.; Lallukka, T.; Sekine, M.; Lahelma, E.; Tatsuse, T.; Marmot, M.G. Country specific associations between social contact and mental health: Evidence from civil servant studies across Great Britain, Japan and Finland. Public Health 2016, 137, 139–146. [Google Scholar] [CrossRef]
- Ding, D.; Ramirez Varela, A.; Bauman, A.E.; Ekelund, U.; Lee, I.M.; Heath, G.; Katzmarzyk, P.T.; Reis, R.; Pratt, M. Towards better evidence-informed global action: Lessons learnt from the Lancet series and recent developments in physical activity and public health. Br. J. Sports Med. 2020, 54, 462–468. [Google Scholar] [CrossRef]
- Larsen, B.A.; Strong, D.; Linke, S.E. The association between family and friend integration and physical activity: Results from the NHIS. Int. J. Behav. Med. 2014, 21, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, J.M.; Kim, J.; Dhurandhar, E.; Soliman, G.; Wehbi, N.K.; Canedy, J. Longitudinal associations between body mass index, physical activity, and healthy dietary behaviors in adults: A parallel latent growth curve modeling approach. PLoS ONE 2017, 12, e0173986. [Google Scholar] [CrossRef] [PubMed]
- Lightner, J.; Irwin, B.C.; Chrisman, M. Changes in Social Integration Predict Changes in Physical Activity: A 25-Year Prospective Study. J. Phys. Act. Health 2018, 15, 531–536. [Google Scholar] [CrossRef]
- Naseri, P.; Amiri, P.; Momenyan, S.; Zayeri, F.; Karimi, M.; Azizi, F. Longitudinal association between body mass index and physical activity among adolescents with different parental risk: A parallel latent growth curve modeling approach. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 59. [Google Scholar] [CrossRef]
- Brown, W.J.; Heesch, K.C.; Miller, Y.D. Life events and changing physical activity patterns in women at different life stages. Ann. Behav. Med. 2009, 37, 294–305. [Google Scholar] [CrossRef]
- Sander, J.; Schupp, J.; Richter, D. Getting together: Social contact frequency across the life span. Dev. Psychol. 2017, 53, 1571–1588. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Milton, K.; Bull, F.C.; Bauman, A. Reliability and validity testing of a single-item physical activity measure. Br. J. Sports Med. 2011, 45, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Kondo, K.; Ojima, T.; Hirai, H. Criteria for social isolation based on associations with health indicators among older people. A 10-year follow-up of the Aichi Gerontological Evaluation Study. Nihon Koshu Eisei Zasshi 2015, 62, 95–105. [Google Scholar] [PubMed]
- Koeneman, M.A.; Verheijden, M.W.; Chinapaw, M.J.; Hopman-Rock, M. Determinants of physical activity and exercise in healthy older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 142. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; York Cornwell, E.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef]
- Morris, L.J.; D’Este, C.; Sargent-Cox, K.; Anstey, K.J. Concurrent lifestyle risk factors: Clusters and determinants in an Australian sample. Prev. Med. 2016, 84, 1–5. [Google Scholar] [CrossRef]
- Rigg, J.; Sefton, T.O.M. Income Dynamics and the Life Cycle. J. Soc. Policy 2006, 35, 411–435. [Google Scholar] [CrossRef]
- Inagaki, H.; Ito, K.; Sakuma, N.; Sugiyama, M.; Okamura, T.; Awata, S. [Reliability and validity of the simplified Japanese version of the WHO-Five Well-being Index (S-WHO-5-J)]. Nihon Koshu Eisei Zasshi 2013, 60, 294–301. [Google Scholar]
- Hu, L.t.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Shaw, B.A.; Liang, J.; Krause, N.; Gallant, M.; McGeever, K. Age differences and social stratification in the long-term trajectories of leisure-time physical activity. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010, 65, 756–766. [Google Scholar] [CrossRef]
- Murayama, H.; Liang, J.; Shaw, B.A.; Botoseneanu, A.; Kobayashi, E.; Fukaya, T.; Shinkai, S. Changes in health behaviors and the trajectory of body mass index among older Japanese: A 19-year longitudinal study. Geriatr. Gerontol. Int. 2017, 17, 2008–2016. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef]
- Sakurai, R.; Kawai, H.; Suzuki, H.; Kim, H.; Watanabe, Y.; Hirano, H.; Ihara, K.; Obuchi, S.; Fujiwara, Y. Poor Social Network, Not Living Alone, Is Associated With Incidence of Adverse Health Outcomes in Older Adults. J. Am. Med. Dir. Assoc. 2019, 20, 1438–1443. [Google Scholar] [CrossRef]
- Rostila, M. The Facets of Social Capital. J. Theory Soc. Behav. 2011, 41, 308–326. [Google Scholar] [CrossRef]
- Cotter, K.A.; Lachman, M.E. No strain, no gain: Psychosocial predictors of physical activity across the adult lifespan. J. Phys. Act. Health 2010, 7, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Abdin, E.; Chong, S.A.; Peh, C.X.; Vaingankar, J.A.; Chua, B.Y.; Verma, S.; Jeyagurunathan, A.; Shafie, S.; Subramaniam, M. The mediational role of physical activity, social contact and stroke on the association between age, education, employment and dementia in an Asian older adult population. BMC Psychiatry 2017, 17, 98. [Google Scholar] [CrossRef]
- Webel, A.R.; Okonsky, J.; Trompeta, J.; Holzemer, W.L. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am. J. Public Health 2010, 100, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Jonas, A.B.; Young, A.M.; Oser, C.B.; Leukefeld, C.G.; Havens, J.R. OxyContin(R) as currency: OxyContin(R) use and increased social capital among rural Appalachian drug users. Soc. Sci. Med. 2012, 74, 1602–1609. [Google Scholar] [CrossRef] [PubMed]
| Variables | All (n = 1395) | Men (n = 606) | Women (n = 789) | ||||
|---|---|---|---|---|---|---|---|
| Age—mean, SD | 51.1 | 14.5 | 52.1 | 14.3 | 50.4 | 14.6 | |
| Age group—n, % | |||||||
| Young (20–39 years) | 347 | 24.9 | 133 | 21.9 | 214 | 27.1 | |
| Middle-aged (40–64 years) | 777 | 55.7 | 347 | 57.3 | 430 | 54.5 | |
| Older adults (≥65 years) | 271 | 19.4 | 126 | 20.8 | 145 | 18.4 | |
| Years of education—n, % | |||||||
| <13 years | 454 | 32.5 | 189 | 31.2 | 265 | 33.6 | |
| ≥13 years | 875 | 62.7 | 385 | 63.5 | 490 | 62.1 | |
| Missing | 66 | 4.7 | 32 | 5.3 | 34 | 4.3 | |
| Subjective economic status—n, % | |||||||
| High | 392 | 28.1 | 161 | 26.6 | 231 | 29.3 | |
| Medium | 545 | 39.1 | 232 | 38.3 | 313 | 39.7 | |
| Low | 429 | 30.8 | 202 | 33.3 | 227 | 28.8 | |
| Missing | 29 | 2.1 | 11 | 1.8 | 18 | 2.3 | |
| Marital status—n, % | |||||||
| Married | 1087 | 77.9 | 481 | 79.4 | 606 | 76.8 | |
| Divorced/widowed/single | 278 | 19.9 | 113 | 18.6 | 165 | 20.9 | |
| Missing | 30 | 2.2 | 12 | 2.0 | 18 | 2.3 | |
| Employment status—n, % | |||||||
| Paid worker | 994 | 71.3 | 503 | 83.0 | 491 | 62.2 | |
| Not in the labor force | 372 | 26.7 | 89 | 14.7 | 283 | 35.9 | |
| Missing | 29 | 2.1 | 14 | 2.3 | 15 | 1.9 | |
| Self-rated health—n, % | |||||||
| Good | 1240 | 88.9 | 514 | 84.8 | 726 | 92.0 | |
| Poor | 148 | 10.6 | 89 | 14.7 | 59 | 7.5 | |
| Missing | 7 | 0.5 | 3 | 0.5 | 4 | 0.5 | |
| Mental health—mean, SD | 8.2 | 2.9 | 7.8 | 2.9 | 8.5 | 2.9 | |
| Medical history—n, % | |||||||
| Diabetes mellitus | 69 | 4.9 | 47 | 7.8 | 22 | 2.8 | |
| Hypertension | 212 | 15.2 | 111 | 18.3 | 101 | 12.8 | |
| Alcohol consumption—n, % | |||||||
| ≥1 day/week | 663 | 47.5 | 376 | 62.0 | 287 | 36.4 | |
| <1 day/week | 358 | 25.7 | 132 | 21.8 | 226 | 28.6 | |
| Former-drinker | 82 | 5.9 | 29 | 4.8 | 53 | 6.7 | |
| Non-drinker | 289 | 20.7 | 69 | 11.4 | 220 | 27.9 | |
| Missing | 3 | 0.2 | 0 | 0.0 | 3 | 0.4 | |
| Smoking status—n, % | |||||||
| Smoker | 233 | 16.7 | 170 | 28.1 | 63 | 8.0 | |
| Former-smoker | 424 | 30.4 | 277 | 45.7 | 147 | 18.6 | |
| Non-smoker | 734 | 52.6 | 159 | 26.2 | 575 | 72.9 | |
| Missing | 4 | 0.3 | 0 | 0.0 | 4 | 0.5 | |
| Frequency of well-balanced meals—n, % | |||||||
| ≥5 days/week | 1030 | 73.8 | 427 | 70.5 | 603 | 76.4 | |
| 1–4 days/week | 306 | 21.9 | 148 | 24.4 | 158 | 20.0 | |
| <1 day/week | 58 | 4.2 | 31 | 5.1 | 27 | 3.4 | |
| Missing | 1 | 0.1 | 0 | 0.0 | 1 | 0.1 | |
| Parameter | All (n = 1395) | |||
|---|---|---|---|---|
| β | SE | p-Value | ||
| PA (Intercept) | ||||
| Overall social contact (Intercept) | 0.029 | 0.018 | 0.113 | |
| PA (Slope) | ||||
| Overall social contact (Intercept) | 0.009 | 0.005 | 0.044 | |
| Overall social contact (Slope) | 0.169 | 0.071 | 0.017 | |
| CFI | 0.995 | |||
| TLI | 0.989 | |||
| RMSEA (90% CI) | 0.014 (0.003, 0.021) | |||
| Parameter | All (n = 1395) | |||
|---|---|---|---|---|
| β | SE | p-Value | ||
| PA (Intercept) | ||||
| Frequency of contacting family/relatives (Intercept) | −0.022 | 0.025 | 0.386 | |
| Frequency of contacting friends/neighbors (Intercept) | 0.104 | 0.034 | 0.002 | |
| PA (Slope) | ||||
| Frequency of contacting family/relatives (Intercept) | 0.016 | 0.006 | 0.008 | |
| Frequency of contacting friends/neighbors (Intercept) | 0.002 | 0.008 | 0.783 | |
| Frequency of contacting family/relatives (Slope) | 0.139 | 0.065 | 0.033 | |
| Frequency of contacting friends/neighbors (Slope) | 0.154 | 0.113 | 0.174 | |
| CFI | 0.970 | |||
| TLI | 0.950 | |||
| RMSEA (90% CI) | 0.029 (0.025, 0.033) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemoto, Y.; Sakurai, R.; Matsunaga, H.; Murayama, Y.; Hasebe, M.; Nishi, M.; Narita, M.; Fujiwara, Y. Social Contact with Family and Non-Family Members Differentially Affects Physical Activity: A Parallel Latent Growth Curve Modeling Approach. Int. J. Environ. Res. Public Health 2021, 18, 2313. https://doi.org/10.3390/ijerph18052313
Nemoto Y, Sakurai R, Matsunaga H, Murayama Y, Hasebe M, Nishi M, Narita M, Fujiwara Y. Social Contact with Family and Non-Family Members Differentially Affects Physical Activity: A Parallel Latent Growth Curve Modeling Approach. International Journal of Environmental Research and Public Health. 2021; 18(5):2313. https://doi.org/10.3390/ijerph18052313
Chicago/Turabian StyleNemoto, Yuta, Ryota Sakurai, Hiroko Matsunaga, Yoh Murayama, Masami Hasebe, Mariko Nishi, Miki Narita, and Yoshinori Fujiwara. 2021. "Social Contact with Family and Non-Family Members Differentially Affects Physical Activity: A Parallel Latent Growth Curve Modeling Approach" International Journal of Environmental Research and Public Health 18, no. 5: 2313. https://doi.org/10.3390/ijerph18052313
APA StyleNemoto, Y., Sakurai, R., Matsunaga, H., Murayama, Y., Hasebe, M., Nishi, M., Narita, M., & Fujiwara, Y. (2021). Social Contact with Family and Non-Family Members Differentially Affects Physical Activity: A Parallel Latent Growth Curve Modeling Approach. International Journal of Environmental Research and Public Health, 18(5), 2313. https://doi.org/10.3390/ijerph18052313






