Influence of Resistance Training on Gait & Balance Parameters in Older Adults: A Systematic Review
Abstract
:1. Introduction
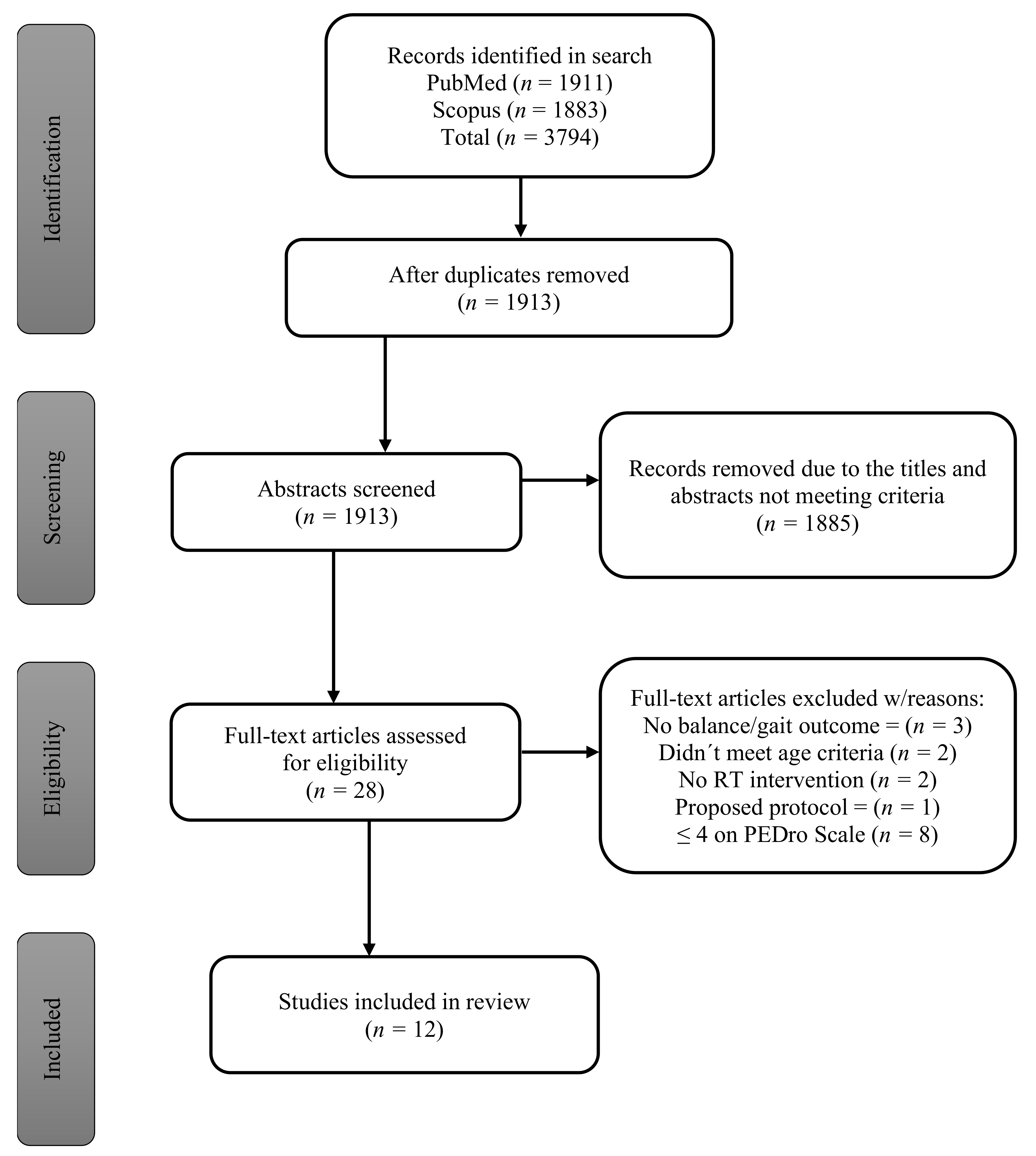
2. Methods
2.1. Study Selection—Inclusion Criteria
2.2. Study Selection—Exclusion Criteria
3. Results
Study Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Colombo, P.J.; Crawley, M.E.; East, B.S.; Hill, A.R. Aging and the Brain. Encycl. Hum. Behav. Second Ed. 2012, 53–59. [Google Scholar] [CrossRef]
- Kanasi, E.; Ayilavarapu, S.; Jones, J. The aging population: Demographics and the biology of aging. Periodontol. 2000 2016, 72, 13–18. [Google Scholar] [CrossRef]
- Álvarez-García, J.; Durán-Sánchez, A.; Río-Rama, D.; de la Cruz, M.; García-Vélez, D.F. Active ageing: Mapping of scientific coverage. Int. J. Environ. Res. Public Health 2018, 15, 2727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “active Aging. ” Gerontologist 2016, 56, S268–S280. [Google Scholar] [CrossRef] [PubMed]
- De Labra, C.; Guimaraes-Pinheiro, C.; Maseda, A.; Lorenzo, T.; Millán-Calenti, J.C. Effects of physical exercise interventions in frail older adults: A systematic review of randomized controlled trials Physical functioning, physical health and activity. BMC Geriatr. 2015, 15, 154. [Google Scholar] [CrossRef] [Green Version]
- Khanuja, K.; Joki, J.; Bachmann, G.; Cuccurullo, S. Gait and balance in the aging population: Fall prevention using innovation and technology. Maturitas 2018, 110, 51–56. [Google Scholar] [CrossRef]
- Wales, N.S.; Health, P. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing 2016, 38, 345–352. [Google Scholar] [CrossRef] [Green Version]
- Sherrington, C.; Fairhall, N.; Wallbank, G.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S. Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic Review. Br. J. Sports Med. 2020, 54, 885–891. [Google Scholar] [CrossRef]
- Papa, E.V.; Dong, X.; Hassan, M. Resistance training for activity limitations in older adults with skeletal muscle function deficits: A systematic review. Clin. Interv. Aging 2017, 12, 955–961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaap, L.A.; Van Schoor, N.M.; Lips, P.; Visser, M. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: The longitudinal aging study Amsterdam. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 1199–1204. [Google Scholar] [CrossRef]
- Clark, B.C.; Manini, T.M. What is dynapenia? Nutrition 2012, 28, 495–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sgaravatti, A.; Santos, D.; Bermúdez, G.; Barboza, A. Velocidad de marcha del adulto mayor funcionalmente saludable Gait Speed in Functionally and Healthy Elder People Velocidade da marcha do idoso funcionalmente saudável. In Anales de la Facultad de Medicina; Universidad de la República: Montevideo, Uruguay, 2018; Volume 5, pp. 93–101. [Google Scholar]
- Gomeñuka, N.A.; Oliveira, H.B.; Silva, E.S.; Costa, R.R.; Kanitz, A.C.; Liedtke, G.V.; Schuch, F.B.; Peyré-Tartaruga, L.A. Effects of Nordic walking training on quality of life, balance and functional mobility in elderly: A randomized clinical trial. PLoS ONE 2019, 14, e0211472. [Google Scholar] [CrossRef] [PubMed]
- Bouaziz, W.; Vogel, T.; Schmitt, E.; Kaltenbach, G.; Geny, B.; Olivier, P. Health bene fi ts of aerobic training programs in adults aged 70 and over: A systematic review. Arch. Gerontol. Geriatr. 2017, 69, 110–127. [Google Scholar] [CrossRef] [PubMed]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance Training for Older Adults: Position Statement From the National Strength and Conditioning Association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef]
- Hassan, B.H.; Hewitt, J.; Keogh, J.W.L.; Bermeo, S.; Duque, G.; Henwood, T.R. Impact of resistance training on sarcopenia in nursing care facilities: A pilot study. Geriatr. Nurs. 2016, 37, 116–121. [Google Scholar] [CrossRef]
- Woolford, S.J.; Sohan, O.; Dennison, E.M.; Cooper, C.; Patel, H.P. Approaches to the diagnosis and prevention of frailty. Aging Clin. Exp. Res. 2020, 32, 1629–1637. [Google Scholar] [CrossRef]
- Jadczak, A.D.; Makwana, N.; Luscombe-Marsh, N.; Visvanathan, R.; Schultz, T.J. Effectiveness of exercise interventions on physical function in community-dwelling frail older people: An umbrella review of systematic reviews. JBI Evid. Synth. 2018, 16, 752–775. [Google Scholar] [CrossRef]
- Lopez, P.; Silveira, R.; Regis, P.; Rech, A.; Grazioli, R.; Izquierdo, M.; Cadore, E.L. Benefits of resistance training in physically frail elderly: A systematic review. Aging Clin. Exp. Res. 2018, 30, 889–899. [Google Scholar] [CrossRef]
- Latham, N.K.; Bennett, D.A.; Stretton, C.M.; Anderson, C.S. Systematic Review of Progressive Resistance Strength Training in Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2004, 59, 48–61. [Google Scholar] [CrossRef]
- Steib, S.; Schoene, D.; Pfeifer, K. Dose-response relationship of resistance training in older adults: A meta-analysis. Med. Sci. Sports Exerc. 2010, 42, 902–914. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 7, 889–896. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fahlman, M.M.; McNevin, N.; Boardley, D.; Morgan, A.; Topp, R. Effects of resistance training on functional ability in elderly individuals. Am. J. Heal. Promot. 2011, 25, 237–243. [Google Scholar] [CrossRef]
- Gonzalez, A.M.; Mangine, G.T.; Fragala, M.S.; Stout, J.R.; Beyer, K.S.; Bohner, J.D.; Emerson, N.S.; Hoffman, J.R. Resistance training improves single leg stance performance in older adults. Aging Clin. Exp. Res. 2014, 26, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Sparrow, D.; Gottlieb, D.J.; Demolles, D.; Fielding, R.A. Increases in muscle strength and balance using a resistance training program administered via a telecommunications system in older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66, 1251–1257. [Google Scholar] [CrossRef] [PubMed]
- Nicklas, B.J.; Chmelo, E.; Delbono, O.; Carr, J.J.; Lyles, M.F.; Marsh, A.P. Effects of resistance training with and without caloric restriction on physical function and mobility in overweight and obese older adults: A randomized controlled trial. Am. J. Clin. Nutr. 2015, 101, 991–999. [Google Scholar] [CrossRef]
- Marques, E.A.; Wanderley, F.; Machado, L.; Sousa, F.; Viana, J.L.; Moreira-Gonçalves, D.; Moreira, P.; Mota, J.; Carvalho, J. Effects of resistance and aerobic exercise on physical function, bone mineral density, OPG and RANKL in older women. Exp. Gerontol. 2011, 46, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.; Coelho, E.; Silva, M.; Pindus, D.; Cumming, S.; Teixeira, A.; Veríssimo, M. Effects of strength and aerobic-based training on functional fitness, mood and the relationship between fatness and mood in older adults. J. Sports Med. Phys. Fitness 2011, 51, 489–496. [Google Scholar]
- Hewitt, J.; Goodall, S.; Clemson, L.; Henwood, T.; Refshauge, K. Progressive Resistance and Balance Training for Falls Prevention in Long-Term Residential Aged Care: A Cluster Randomized Trial of the Sunbeam Program. J. Am. Med. Dir. Assoc. 2018, 19, 361–369. [Google Scholar] [CrossRef]
- Alfieri, F.M.; Riberto, M.; Gatz, L.S.; Ribeiro, C.P.C.; Lopes, J.A.F.; Battistella, L.R. Comparison of multisensory and strength training for postural control in the elderly. Clin. Interv. Aging 2012, 7, 119–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramirez-Campillo, R.; Diaz, D.; Martinez-Salazar, C.; Valdés-Badilla, P.; Delgado-Floody, P.; Méndez-Rebolledo, G.; Cañas-Jamet, R.; Cristi-Montero, C.; García-Hermoso, A.; Celis-Morales, C.; et al. Effects of different doses of high-speed resistance training on physical performance and quality of life in older women: A randomized controlled trial. Clin. Interv. Aging 2016, 11, 1797–1804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiotsu, Y.; Yanagita, M. Comparisons of low-intensity versus moderate-intensity combined aerobic and resistance training on body composition, muscle strength, and functional performance in older women. Menopause 2018, 25, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Sylliaas, H.; Brovold, T.; Wyller, T.B.; Bergland, A. Progressive strength training in older patients after hip fracture: A randomised controlled trial. Age Ageing 2011, 40, 221–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cancela Carral, J.M.; Rodríguez, A.L.; Cardalda, I.M.; Gonçalves Bezerra, J.P.A. Muscle strength training program in nonagenarians—A randomized controlled trial. Rev. Assoc. Med. Bras. 2019, 65, 851–856. [Google Scholar] [CrossRef]
- Ribeiro, P.A.B.; Boidin, M.; Juneau, M.; Nigam, A.; Gayda, M. High-intensity interval training in patients with coronary heart disease: Prescription models and perspectives. Ann. Phys. Rehabil. Med. 2017, 60, 50–57. [Google Scholar] [CrossRef] [Green Version]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower extremity function and subsequent disability: Consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, 221–231. [Google Scholar] [CrossRef] [Green Version]
- Whittle, M.W. Chapter 5—Applications of gait analysis. In Gait Analysis, 4th ed.; Whittle, M.W., Ed.; Butterworth-Heinemann: Edinburgh, Scotland, 2007; pp. 177–193. ISBN 978-0-7506-8883-3. [Google Scholar]
- Latorre Román, P.Á.; Muñoz Jiménez, M.; Salas Sánchez, J.; Consuegra González, P.; Moreno Del Castillo, R.; Herrador Sánchez, J.A.; López Ivanco, M.D.A.; Linares Jiménez, C.; Navas Morales, J.F.; Párraga Montilla, J.A. Complex gait is related to cognitive functioning in older people: A cross-sectional study providing an innovative test. Gerontology 2020, 66, 401–408. [Google Scholar] [CrossRef]
- Bird, S.P.; Tarpenning, K.M.; Marino, F.E. Designing resistance training programmes to enhance muscular fitness: A review of the acute programme variables. Sport Med. 2005, 35, 841–851. [Google Scholar] [CrossRef]
- Kraemer, W.J.; Ratamess, N.A. Fundamentals of Resistance Training: Progression and Exercise Prescription. Med. Sci. Sports Exerc. 2004, 36, 674–688. [Google Scholar] [CrossRef]
- Schwenk, M.; Jordan, E.D.H.; Honarvararaghi, B.; Mohler, J.; Armstrong, D.G.; Najafi, B. Effectiveness of foot and ankle exercise programs on reducing the risk of falling in older adults: A systematic review and meta-analysis of randomized controlled trials. J. Am. Podiatr. Med. Assoc. 2013, 103, 534–547. [Google Scholar] [CrossRef] [Green Version]
- Simek, E.M.; McPhate, L.; Haines, T.P. Adherence to and efficacy of home exercise programs to prevent falls: A systematic review and meta-analysis of the impact of exercise program characteristics. Prev. Med. 2012, 55, 262–275. [Google Scholar] [CrossRef]
- Kraemer, W.J.; Adams, K.; Cafarelli, E.; Dudley, G.A.; Dooly, C.; Feigenbaum, M.S.; Fleck, S.J.; Franklin, B.; Fry, A.C.; Hoffman, J.R.; et al. Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. 2002, 34, 364–380. [Google Scholar] [CrossRef]
- González-Badillo, J.J.; Marques, M.C.; Sánchez-Medina, L. The Importance of Movement Velocity as a Measure to Control Resistance Training Intensity. J. Hum. Kinet. Spec. Issue 2011, 29, 15–19. [Google Scholar] [CrossRef]
- Knutzen, K.M.; Brilla, L.R.; Caine, D. Validity of 1RM Prediction Equations for Older Adults. J. Strength Cond. Res. 1999, 13, 242–246. [Google Scholar] [CrossRef]
- Willardson, J.M. A brief review: How much rest between sets? Strength Cond. J. 2008, 30, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Borde, R.; Hortobágyi, T.; Granacher, U. Dose–Response Relationships of Resistance Training in Healthy Old Adults: A Systematic Review and Meta-Analysis. Sport Med. 2015, 45, 1693–1720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villanueva, M.G.; Lane, C.J.; Schroeder, E.T. Short rest interval lengths between sets optimally enhance body composition and performance with 8 weeks of strength resistance training in older men. Eur. J. Appl. Physiol. 2015, 115, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, A.; Hortobágyi, T.; Beurskens, R.; Granacher, U. Effects of Supervised vs. Unsupervised Training Programs on Balance and Muscle Strength in Older Adults: A Systematic Review and Meta-Analysis. Sport Med. 2017, 47, 2341–2361. [Google Scholar] [CrossRef] [PubMed]
- Haraldstad, K.; Rohde, G.; Stea, T.H.; Lohne-Seiler, H.; Hetlelid, K.; Paulsen, G.; Berntsen, S. Changes in health-related quality of life in elderly men after 12 weeks of strength training. Eur. Rev. Aging Phys. Act. 2017, 14, 10–15. [Google Scholar] [CrossRef] [Green Version]
- Krist, L.; Dimeo, F.; Keil, T. Can progressive resistance training twice a week improve mobility, muscle strength, and quality of life in very elderly nursing-home residents with impaired mobility? A pilot study. Clin. Interv. Aging 2013, 8, 443–448. [Google Scholar] [CrossRef] [Green Version]
| Authors | 1 * | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alfieri et al., (2012) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Cancela Carral et al., (2019) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| De Sousa et al., (2013) ▪ | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Fahlman et al., (2011) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Forte et al., (2013) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Gonzalez et al., (2014) ▪ | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Hewitt et al., 2018 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Iuliano et al., (2015) | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Marques et al., (2011) | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Martins R, et al. (2011) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Nicholson et al., (2015) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Nicklas et al., (2016) ▪ | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Pamukoff et al., 2014 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Ramirez-Campillo, Rodrigo, et al. (2016) | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Roma et al., (2013) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Sahin et al., (2018) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Shiotsu & Yanagita, (2018) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Sparrow et al., (2011) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Sylliaas et al., (2011) | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yoon et al., (2018) | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Authors | Population | Population (Cont.) | Age | n = | Male | Female |
|---|---|---|---|---|---|---|
| Alfieri et al., (2012) | Community-dwelling | 70.18 ± 4.8 | 23 | 1 | 22 | |
| Cancela Carral et al., (2019) | Residential care | Frail | 90.8 ± 4.02 | 13 | 0 | 13 |
| Fahlman et al., (2011) | Community-dwelling | 74.8 ± 1 | 46 | NR | NR | |
| Gonzalez et al., (2014) | Community-dwelling | 71.1 ± 6.1 | 23 | 12 | 11 | |
| Hewitt et al., 2018 | Residential care | 86 ± 7 | 113 | 42 | 71 | |
| Marques et al., (2011) | Community-dwelling | 67.3 ± 5.2 | 23 | 0 | 23 | |
| Martins et al. (2011) | Residential care | 73.4 ± 6.4 | 23 | 10 | 13 | |
| Nicklas et al., (2016) | Community-dwelling | Overweight/Obese | 69.4 ± 3.6 | 63 | 34 | 29 |
| Ramirez-Campillo et al., (2016) | Community-dwelling | 70 ± 6.9 | 8 | 0 | 8 | |
| Shiotsu & Yanagita, (2018) | Community-dwelling | 69.0 ± 4.1 | 12 | 0 | 12 | |
| Sparrow et al., (2011) | Community-dwelling | Vets & Spouses * | 70.3 ± 7.5 | 52 | 35 | 17 |
| Sylliaas et al., (2011) | Community-dwelling | Hip Fracture | 82.1 ± 6.5 | 100 | 15 | 85 |
| Authors | Exercise Modality | Days/Week | Weeks | Sets | Reps | Rest-time | Load | Total Time |
|---|---|---|---|---|---|---|---|---|
| Alfieri et al., (2012) | Machines | 2 | 12 | 3 | 12,10,8 | NR | 50%, 75%, MTL | 60 |
| Cancela Carral et al., (2019) | Elastic Bands | 2 | 12 | varied | varied | 30–60 sec | progressive | 60 |
| Fahlman et al., (2011) | Elastic Bands | 3 | 16 | 2 | 12 | NR | progressive | NR |
| Gonzalez et al., (2014) | Body Weight/Machines | 2 | 6 | 3 | 8 to 15 | NR | NR | NR |
| Hewitt et al., 2018 | Pneumatic/Balance | 2 | 25 | 2 to 3 | 10 to 15 | NR | Moderate (CR10) | 60 |
| Marques et al., (2011) | Machines | 3 | 32 | 2 | 6 to 8 | ≥2 min | 75–85% 1RM | 60 |
| Martins et al. (2011) | Calesthetics/Elastic Bands | 3 | 16 | varied | varied | 3 min | progressive | 45 |
| Nicklas et al., (2016) | Machines | 3 | 20 | 3 | 10 | ±1 min | 70% 1RM | NR |
| Ramirez-Campillo et al., (2016) | High-speed RT | 2 | 12 | 3 | varied | ±1 min | 75% 1RM | 50 to 70 |
| Shiotsu & Yanagita, (2018) | Machines | 2 | 10 | 3 | 8 to 12 | NR | 60–70% 1RM | NR |
| Sparrow et al., (2011) | Body Weight/Free Weights | 3 | 26 | 2 | 12 | NR | varied | 60 |
| Sylliaas et al., (2011) | Body Weight/Machines | 3 | 12 | 3 | 8 to 12 | NR | 80% 1RM | 45 to 60 |
| Authors | Drop-outs | Explanation | Adverse Events | Explanation |
|---|---|---|---|---|
| Alfieri et al., (2012) | 5 | 1 ankle fracture, 1 rib fracture, 1 uncontrolled HF, 1 knee pain, 1 gave up | NR | |
| Cancela Carral et al., (2019) | 2 | death | NR | |
| Fahlman et al., (2011) | 4 | NR | NR | |
| Gonzalez et al., (2014) | 0 | 0 | ||
| Hewitt et al., 2018 | 16 | 15 deceased, 1 moved away | 4 | 3 musculoskeletal aches/pains, 1 noninjurious fall. |
| Marques et al., (2011) | 8 | Medical issues unrelated (n = 3) Disinterest (n = 3) Personal reasons (n = 2) | 0 | |
| Martins et al. (2011) | 0 | NR | ||
| Nicklas et al., (2016) | 7 | 3 personal health issues, 2 caretaking, 1 changed mind, 1 lost to follow-up | 2 | 2 musculoskeletal complaints |
| Ramirez-Campillo et al., (2016) | 0 | 0 | ||
| Shiotsu & Yanagita, (2018) | 3 | 3 private reasons | NR | |
| Sparrow et al., (2011) | 3 | NR | 8 | 8 musculoskeletal |
| Sylliaas et al., (2011) | 5 | 1 nursing home, 1 died, 3 illness | NR |
| Authors | Variable | Tools | Conclusion |
|---|---|---|---|
| Alfieri et al., (2012) | Balance | Timed Up and Go (TUG); Berg; Oscillation of the body’s center of pressure | Both multisensory and RT interventions improved static and dynamic mobility in healthy elderly subjects. |
| Cancela Carral et al., (2019) | Balance | TUG | Muscle strength intervention programs may help promote healthy lifestyles by maintaining autonomy, improving function, and balance. |
| Fahlman et al., (2011) | Gait | Velocity (m/min), step time (seconds), step length (cm): GAITRite mat | Eight weeks of RT increased the parameters of velocity and step length. Additional emphasis on gait training could improve gains even further. |
| Gonzalez et al., (2014) | Balance | Single leg balance | These findings support the use of progressive resistance training for untrained older adults to improve balance. |
| Hewitt et al., 2018 | Gait & Balance | Short Physical Performance Battery (SPPB) | Moderate-intensity PRT and high-level balance exercise significantly reduced falls and improved SPPB performance. |
| Marques et al., (2011) | Balance | 8-foot Up and Go (8-ft UG) | 8-month RT, but not AT, can induce significant bone adaptation in older women and both regimens elicited significant gains in balance. |
| Martins et al., (2011) | Balance | 8-ft UG | Both AT and RT interventions improved functional fitness. |
| Nicklas et al., (2016) | Gait & Balance | gait speed; SPPB; chair rise | Both RT and RT + Calorie Restriction groups increased in gait speed, SPPB score, and chair rise time. |
| Ramirez-Campillo et al., (2016) | Balance | 8-ft UG; Bilateral balance w/Bertec BP5050 balance plate platform | 2 or 3 training sessions/week of RT (equated for volume and intensity) are equally effective for improving physical performance and quality of life of older women. |
| Shiotsu & Yanagita, (2018) | Gait & Balance | 10-m walk speed; TUG; single-leg balance with eyes open; Functional Reach Test (FRT) | 10-m walk speed significantly increased in all training groups; Combined AT & moderate-intensity RT resulted in significant improvements in dynamic balance capacity. |
| Sparrow et al., (2011) | Balance | Single leg balance (eyes open) and Tandem stance | A home-based RT program for older adults resulted in significant improvements in muscular strength and balance. |
| Sylliaas et al., (2011) | Gait & Balance | Berg; TUG; 10-m walk speed | Significant improvements in BBS, sit-to-stand, TUG, and 10 m walk speed. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keating, C.J.; Cabrera-Linares, J.C.; Párraga-Montilla, J.A.; Latorre-Román, P.A.; del Castillo, R.M.; García-Pinillos, F. Influence of Resistance Training on Gait & Balance Parameters in Older Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1759. https://doi.org/10.3390/ijerph18041759
Keating CJ, Cabrera-Linares JC, Párraga-Montilla JA, Latorre-Román PA, del Castillo RM, García-Pinillos F. Influence of Resistance Training on Gait & Balance Parameters in Older Adults: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(4):1759. https://doi.org/10.3390/ijerph18041759
Chicago/Turabian StyleKeating, Christopher J., José Carlos Cabrera-Linares, Juan A. Párraga-Montilla, Pedro A. Latorre-Román, Rafael Moreno del Castillo, and Felipe García-Pinillos. 2021. "Influence of Resistance Training on Gait & Balance Parameters in Older Adults: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 4: 1759. https://doi.org/10.3390/ijerph18041759
APA StyleKeating, C. J., Cabrera-Linares, J. C., Párraga-Montilla, J. A., Latorre-Román, P. A., del Castillo, R. M., & García-Pinillos, F. (2021). Influence of Resistance Training on Gait & Balance Parameters in Older Adults: A Systematic Review. International Journal of Environmental Research and Public Health, 18(4), 1759. https://doi.org/10.3390/ijerph18041759







