Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis
Abstract
1. Introduction
2. Methods
2.1. Terminologies
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Selection and Extraction
2.5. Data Analysis and Synthesis
3. Results
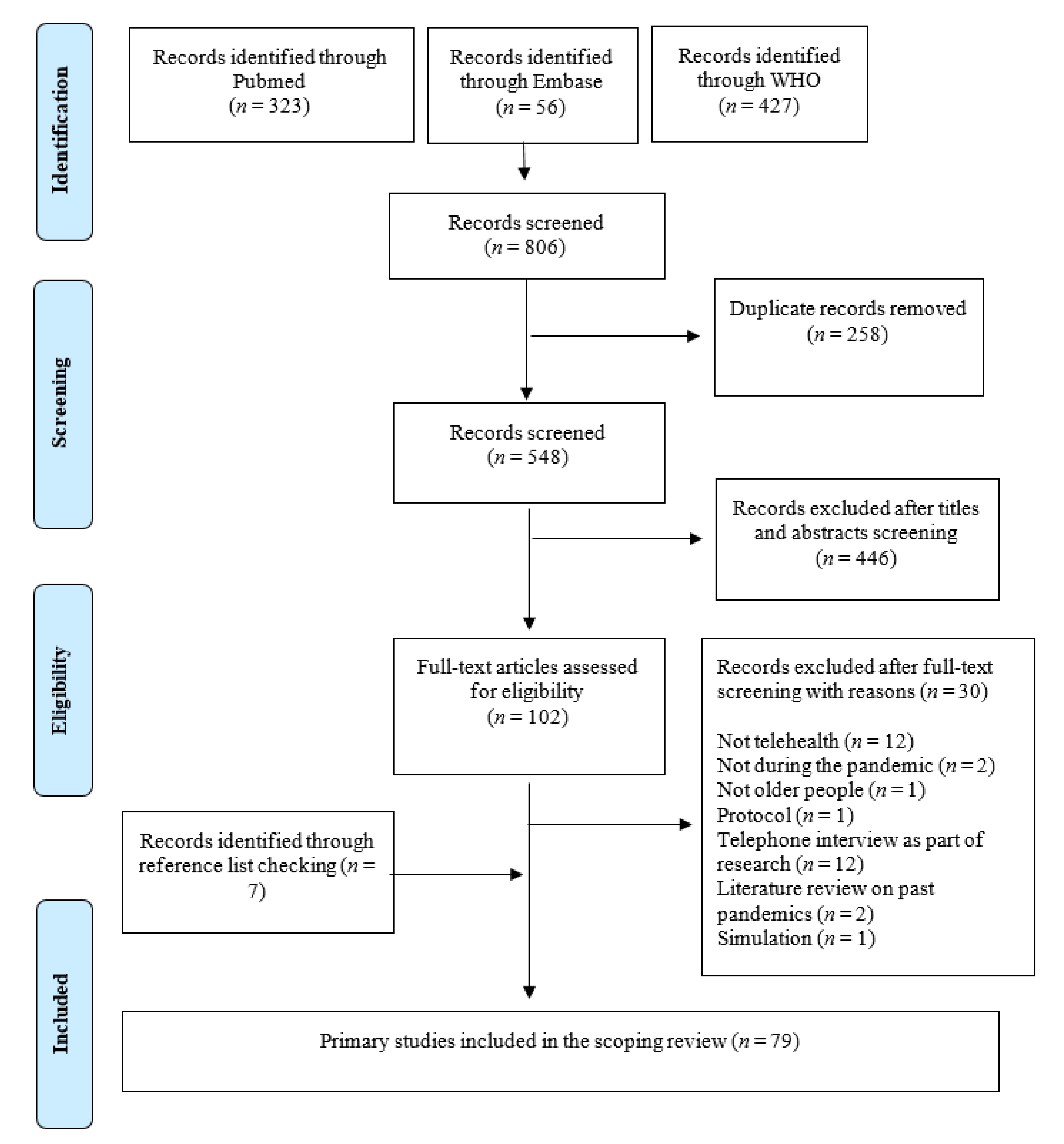
3.1. Selection of Articles
3.2. Characteristics of the Included Articles
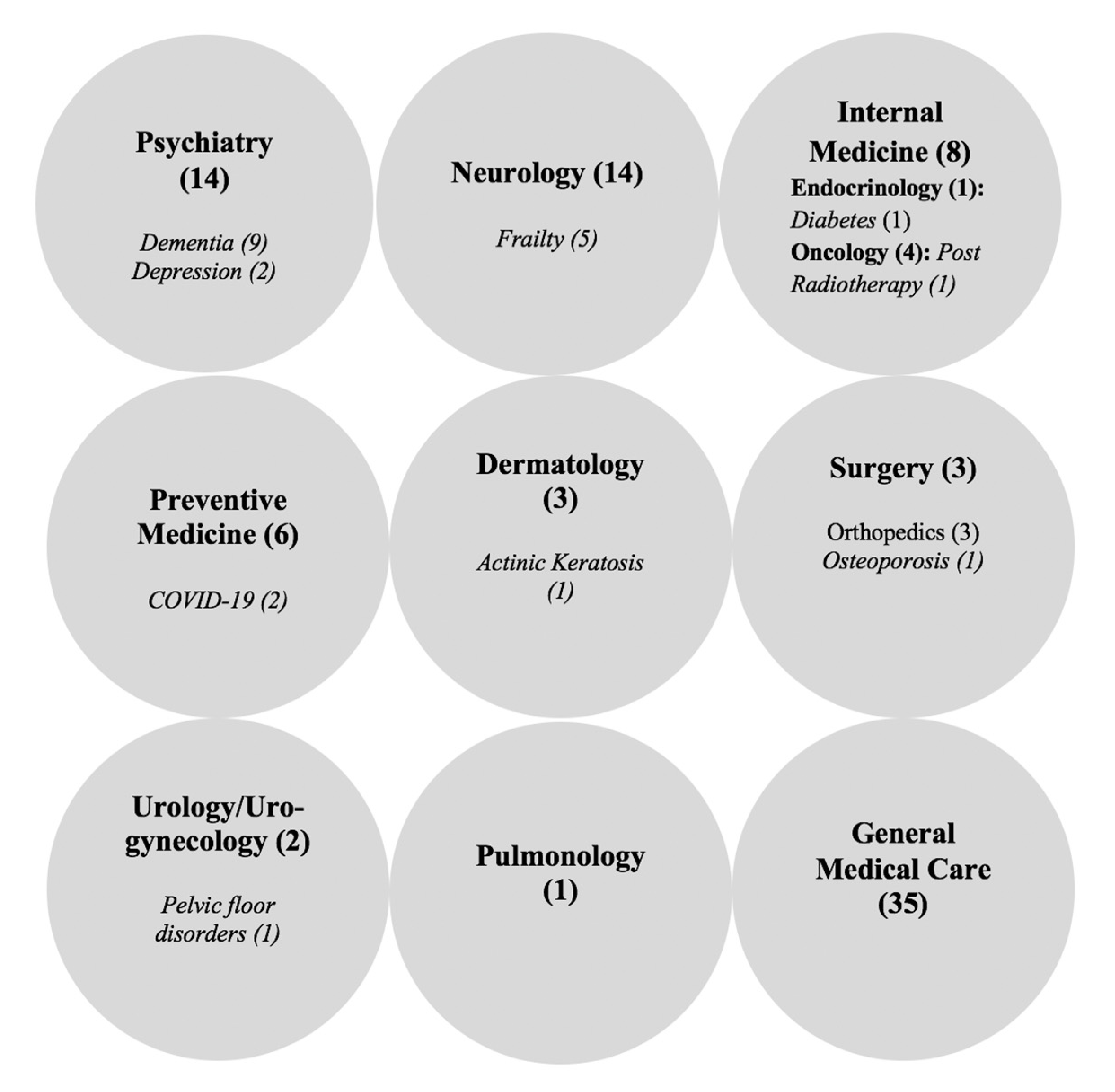
4. Discussion
4.1. Availability, Accessibility, Affordability, and Quality of Telehealth in Geriatric Care during the COVID-19 Pandemic
4.2. Strengths, Weakness, Opportunities, and Threats for Telehealth Use in Geriatric Care during the COVID-19 Pandemic
4.3. Implications for Practice and Research Gaps
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ioannidis, J.P.; Axfors, C.; Contopoulos-Ioannidis, D.G. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ. Res. 2020, 188, 109890. [Google Scholar] [CrossRef]
- Doraiswamy, S.; Mamtani, R.; Ameduri, M.; Abraham, A.; Cheema, S. Respiratory epidemics and older people. Age Ageing 2020, 49, 896–900. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Policy Brief: The Impact of COVID-19 on Older Persons; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Vergara, J.; Parish, A.; Smallheer, B. Telehealth: Opportunities in geriatric patient care during COVID-19. Geriatr. Nurs. 2020, 41, 657–658. [Google Scholar] [CrossRef] [PubMed]
- Merrell, R.C. Geriatric Telemedicine: Background and Evidence for Telemedicine as a Way to Address the Challenges of Geriatrics. Healthc. Inform. Res. 2015, 21, 223–229. [Google Scholar] [CrossRef][Green Version]
- Lustig, T.A. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary; National Academies Press: Washington, DC, USA, 2012. [Google Scholar]
- Foster, M.V.; Sethares, K.A. Facilitators and barriers to the adoption of telehealth in older adults: An integrative review. Comput. Inform. Nurs. 2014, 32, 523–533. [Google Scholar] [CrossRef]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, S.; Abraham, A.; Mamtani, R.; Cheema, S. Use of Telehealth during the COVID-19 Pandemic: Scoping Review. J. Med. Internet Res. 2020, 22, e24087. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.F.; Teng, V.H.W.; Seetharaman, S.K.; Yip, A.W. Facilitating telehealth for older adults during the COVID-19 pandemic and beyond: Strategies from a Singapore geriatric center. Geriatr. Gerontol. Int. 2020, 20, 993–995. [Google Scholar] [CrossRef] [PubMed]
- Lam, K.; Lu, A.D.; Shi, Y.; Covinsky, K.E. Assessing Telemedicine Unreadiness Among Older Adults in the United States during the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 1389. [Google Scholar] [CrossRef]
- Mangoni, A.A. Geriatric medicine in an aging society: Up for a challenge? Front. Med. 2014, 1, 10. [Google Scholar] [CrossRef]
- Dotchin, C.L.; Akinyemi, R.O.; Gray, W.K.; Walker, R.W. Geriatric medicine: Services and training in Africa. Age Ageing 2012, 42, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Brubaker, J. (Ed.) The Birth of a New Specialty: Geriatrics. J. Lanc. Gen. Hosp. 2008, 3, 105–107. [Google Scholar]
- Cimperman, M.; Brenčič, M.M.; Trkman, P.; Stanonik Mde, L. Older adults’ perceptions of home telehealth services. Telemed. J. e-Health 2013, 19, 786–790. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.; Pearce, P.F.; Ferguson, L.A.; Langford, C.A. Understanding scoping reviews: Definition, purpose, and process. J. Am. Assoc. Nurse Pract. 2017, 29, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.; Allen, P.; Peckham, S.; Goodwin, N. Asking the right questions: Scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res. Policy Syst. 2008, 6, 7. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Peters, M.; Godfrey, C.; McInerney, P. Scoping Reviews, Joanna Briggs Institute Reviewer Manual [Internet]; The Joanna Briggs Institute: Adelaide, Australia, 2017; Chapter 11. [Google Scholar]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Collaboration, C. Guidance for producing a Campbell evidence and gap map. Campbell Syst. Rev. 2020, 16, e1125. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Open Science Framework (OSF). OSF Home. 2020. Available online: https://osf.io/dashboard (accessed on 20 October 2020).
- Fatehi, F.; Wootton, R. Telemedicine, telehealth or e-health? A bibliometric analysis of the trends in the use of these terms. J. Telemed. Telecare 2012, 18, 460–464. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development; World Health Organisation: Geneva, Switzerland, 1997. [Google Scholar]
- Peña-López, I. Guide to Measuring Information and Communication Technologies (ICT) in Education; UNESCO Institute for Statistics: Montreal, QC, Canada, 2009. [Google Scholar]
- World Health Organization. Telemedicine: Opportunities and Developments in Member States; Report on the Second Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Arai, H.; Ouchi, Y.; Yokode, M.; Ito, H.; Uematsu, H.; Eto, F.; Oshima, S.; Ota, K.; Saito, Y.; Sasaki, H.; et al. Toward the realization of a better aged society: Messages from gerontology and geriatrics. Geriatr. Gerontol. Int. 2011, 12, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Georgia Uo. What Is Gerontology. 2021. Available online: https://iog.publichealth.uga.edu/what-is-gerontology/ (accessed on 30 January 2021).
- WHO. Novel Coronavirus—China; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Bain, P. Research Guides: Systematic Reviews and Meta Analysis: Databases and Sources; Harvard Library: Boston, MA, USA, 2021; Available online: https://guides.library.harvard.edu/meta-analysis (accessed on 7 January 2021).
- Halladay, C.W.; Trikalinos, T.A.; Schmid, I.T.; Schmid, C.H.; Dahabreh, I.J. Using data sources beyond PubMed has a modest impact on the results of systematic reviews of therapeutic interventions. J. Clin. Epidemiol. 2015, 68, 1076–1084. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 Global Literature on Coronavirus Disease. 2021. Available online: https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/ (accessed on 20 August 2020).
- Association, M.L. MLA: COVID-19 Literature Searching. 2020. Available online: https://www.mlanet.org/page/covid-19-literature-searching (accessed on 1 January 2021).
- Lipscomb, C.E. Medical Subject Headings (MeSH). Bull. Med. Libr. Assoc. 2000, 88, 265–266. [Google Scholar] [PubMed]
- Knight, S.R.; Pengel, L.H.M.; Morris, P.J. Evidence in Transplantation. In Kidney Transplantation—Principles and Practice, 7th ed.; Morris, P.J., Knechtle, S.J., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2014; Chapter 42; pp. 729–736. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hupe, M. EndNote X9. J. Electron. Resour. Med. Libr. 2019, 16, 117–119. [Google Scholar] [CrossRef]
- Schmucker, C.; Motschall, E.; Antes, G.; Meerpohl, J.J. Methods of evidence mapping. A systematic review. Bundesgesundh. Gesundh. Gesundh. 2013, 56, 1390–1397. [Google Scholar] [CrossRef]
- Jasiulewicz-Kaczmarek, M. SWOT analysis for Planned Maintenance strategy—A case study. IFAC-PapersOnLine 2016, 49, 674–679. [Google Scholar] [CrossRef]
- World Bank. World Bank Country and Lending Groups. 2020. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 24 August 2020).
- World Health Organization. Regional Offices. 2020. Available online: https://www.who.int/about/who-we-are/regional-offices (accessed on 24 August 2020).
- Chen, K. Use of Gerontechnology to Assist Older Adults to Cope with the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 983–984. [Google Scholar] [CrossRef]
- Charness, N.; Jastrzembski, T.S. Gerontechnology. In Future Interaction Design II; Isomäki, H., Saariluoma, P., Eds.; Springer: London, UK, 2009; pp. 1–29. [Google Scholar]
- Canevelli, M.; Bruno, G.; Cesari, M. Providing Simultaneous COVID-19—Sensitive and Dementia-Sensitive Care as We Transition from Crisis Care to Ongoing Care. J. Am. Med. Dir. Assoc. 2020, 21, 968–969. [Google Scholar] [CrossRef]
- Ishikawa, R.Z. I may never see the ocean again: Loss and grief among older adults during the COVID-19 pandemic. Psychol. Trauma 2020, 12, S85–S86. [Google Scholar] [CrossRef] [PubMed]
- Lai, F.H.-Y.; Yan, E.W.-H.; Chan, D.T.-H. The Protective Impact of Telemedicine on Persons with Dementia and their Caregivers during the COVID-19 Pandemic. Am. J. Geriatr. Psychiatry 2020, 28, 1175. [Google Scholar] [CrossRef]
- Battisti, N.M.L.; Mislang, A.R.; Cooper, L.; O’Donovan, A.; Audisio, R.A.; Cheung, K.-L.; Sarrió, R.G.; Stauder, R.; Soto-Perez-De-Celis, E.; Jaklitsch, M.; et al. Adapting care for older cancer patients during the COVID-19 pandemic: Recommendations from the International Society of Geriatric Oncology (SIOG) COVID-19 Working Group. J. Geriatr. Oncol. 2020, 11, 1190–1198. [Google Scholar] [CrossRef]
- Escura Sancho, S.; Ros Cerro, C.; Angles-Acedo, S.; Bataller Sanchez, E.; Espuna-Pons, M. How did COVID-19 pandemic change the way we attend the patients in an urogynaecological unit. Clin. Investig. Ginecol. Obstet. 2020, 47, 111–117. [Google Scholar]
- McLellan, L.J.; Morelli, M.; Simeone, E.; Khazova, M.; Ibbotson, S.H.; Eadie, E. SmartPDT®: Smartphone enabled real-time dosimetry via satellite observation for daylight photodynamic therapy. Photodiagn. Photodyn. Ther. 2020, 31, 101914. [Google Scholar] [CrossRef] [PubMed]
- Cuffaro, L.; Di Lorenzo, F.; Bonavita, S.; Tedeschi, G.; Leocani, L.; Lavorgna, L. Dementia care and COVID-19 pandemic: A necessary digital revolution. Neurol. Sci. 2020, 41, 1977–1979. [Google Scholar] [CrossRef] [PubMed]
- Fatyga, E.; Dziegielewska-Gesiak, S.; Wierzgon, A.; Stoltny, D.; Muc-Wierzgon, M. The coronavirus disease 2019 pandemic: Telemedicine in elderly patients with type 2 diabetes. Pol. Arch. Intern. Med. 2020, 130, 452–454. [Google Scholar]
- Hau, Y.S.; Kim, J.K.; Hur, J.; Chang, M.C. How about actively using telemedicine during the COVID-19 pandemic? J. Med. Syst. 2020, 44, 108. [Google Scholar] [CrossRef]
- Cormi, C.; Chrusciel, J.; Laplanche, D.; Dramé, M.; Sanchez, S. Telemedicine in nursing homes during the COVID-19 outbreak: A star is born (again). Geriatr. Gerontol. Int. 2020, 20, 646–647. [Google Scholar] [CrossRef]
- Cheung, G.; Peri, K. Challenges to Dementia Care during COVID-19: Innovations in Remote Delivery of Group Cognitive Stimulation Therapy; Taylor & Francis: Abingdon-on-Thames, UK, 2020. [Google Scholar]
- Longpré-Poirier, C.; Desbeaumes Jodoin, V.; Miron, J.-P.; Lespérance, P. Remote Monitoring of Intranasal Ketamine Self-Administration as Maintenance Therapy in Treatment-Resistant Depression (TRD): A Novel Strategy for Vulnerable and At-Risk Populations to COVID-19? Am. J. Geriatr. Psychiatry 2020, 28, 892–893. [Google Scholar]
- Carr, D.; Boerner, K.; Moorman, S. Bereavement in the Time of Coronavirus: Unprecedented Challenges Demand Novel Interventions. J. Aging Soc. Policy 2020, 32, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, P.; Yatnatti, S.K. Intergenerational Digital Engagement: A Way to Prevent Social Isolation during the COVID-19 Crisis. J. Am. Geriatr. Soc. 2020, 68, 1394–1395. [Google Scholar] [CrossRef]
- Siette, J.; Wuthrich, V.; Low, L.-F. Social Preparedness in Response to Spatial Distancing Measures for Aged Care during COVID-19. J. Am. Med. Dir. Assoc. 2020, 21, 985–986. [Google Scholar] [CrossRef]
- Lipner, S.R.; Ouchida, K. Novel Solutions for Dermatologic Care of Geriatric Patients and the Role of the Dermatology House Call. J. Am. Acad. Dermatol. 2020, 83, e419. [Google Scholar] [CrossRef] [PubMed]
- Korczyn, A.D. Dementia in the COVID-19 Period. J. Alzheimer’s Dis. 2020, 75, 1071–1072. [Google Scholar] [CrossRef]
- Sano, M.; Lapid, M.I.; Ikeda, M.; Mateos, R.; Wang, H.; Reichman, W.E. Psychogeriatrics in a world with COVID-19. Int. Psychogeriatr. 2020, 32, 1101–1105. [Google Scholar] [CrossRef] [PubMed]
- Simpson, C.L.; Kovarik, C.L. Effectively engaging geriatric patients via teledermatology. J. Am. Acad. Dermatol. 2020, 83, e417–e418. [Google Scholar] [CrossRef]
- Fisk, M.; Livingstone, A.; Pit, S.W. Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 2020, 22, e19264. [Google Scholar] [CrossRef]
- DiGiovanni, G.; Mousaw, K.; Lloyd, T.; Dukelow, N.; Fitzgerald, B.; D’Aurizio, H.; Loh, K.P.; Mohile, S.; Ramsdale, E.; Maggiore, R.; et al. Development of a telehealth geriatric assessment model in response to the COVID-19 pandemic. J. Geriatr. Oncol. 2020, 11, 761–763. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Gannon, A.; Dolan, C.; McCarthy, G. Telehealth in Psychiatry of Old Age: Ordinary Care in Extraordinary Times in Rural North-West Ireland. Am. J. Geriatr. Psychiatry 2020, 28, 1009–1011. [Google Scholar] [CrossRef] [PubMed]
- Dewar, S.; Lee, P.G.; Suh, T.T.; Min, L. Uptake of Virtual Visits in A Geriatric Primary Care Clinic During the COVID-19 Pandemic. J. Am. Geriatr. Soc. 2020, 68, 1392–1394. [Google Scholar] [CrossRef]
- Kasle, D.A.; Torabi, S.J.; Savoca, E.L.; Judson, B.L.; Manes, R.P. Outpatient Otolaryngology in the Era of COVID-19: A Data-Driven Analysis of Practice Patterns. Otolaryngol. Head Neck Surg. 2020, 163, 138–144. [Google Scholar] [CrossRef]
- Sorinmade, O.A.; Kossoff, L.; Peisah, C. COVID-19 and Telehealth in Older Adult Psychiatry-opportunities for now and the Future. Int. J. Geriatr. Psychiatry 2020, 35, 1427–1430. [Google Scholar] [CrossRef]
- Tousi, B. Dementia Care in the Time of COVID-19 Pandemic. J. Alzheimer’s Dis. 2020, 76, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Marra, D.E.; Hamlet, K.M.; Bauer, R.M.; Bowers, D. Validity of teleneuropsychology for older adults in response to COVID-19: A systematic and critical review. Clin. Neuropsychol. 2020, 34, 1411–1452. [Google Scholar] [CrossRef] [PubMed]
- Banskota, S.; Healy, M.; Goldberg, E.M. 15 Smartphone Apps for Older Adults to Use While in Isolation during the COVID-19 Pandemic. West. J. Emerg. Med. 2020, 21, 514–525. [Google Scholar] [CrossRef]
- Morrow-Howell, N.; Galucia, N.; Swinford, E. Recovering from the COVID-19 Pandemic: A Focus on Older Adults. J. Aging Soc. Policy 2020, 32, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Goulabch, R.; Bocle, H.; Vignet, R.; Sotto, A.; Loubet, P. Digital tablets to improve quality of life of COVID-19 older inpatients during lockdown. Eur. Geriatr. Med. 2020, 11, 705–706. [Google Scholar] [CrossRef]
- Goodman-Casanova, J.M.; Dura-Perez, E.; Guzman-Parra, J.; Cuesta-Vargas, A.; Mayoral-Cleries, F. Telehealth Home Support During COVID-19 Confinement for Community-Dwelling Older Adults With Mild Cognitive Impairment or Mild Dementia: Survey Study. J. Med. Internet Res. 2020, 22, e19434. [Google Scholar] [CrossRef] [PubMed]
- León, S.; Giacaman, R. COVID-19 and Inequities in Oral Health Care for Older People: An Opportunity for Emerging Paradigms. JDR Clin. Transl. Res. 2020, 5, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Upadhyaya, G.K.; Iyengar, K.; Jain, V.K.; Vaishya, R. Challenges and strategies in management of osteoporosis and fragility fracture care during COVID-19 pandemic. J. Orthop. 2020, 21, 287–290. [Google Scholar] [CrossRef]
- Yu, E.W.; Tsourdi, E.; Clarke, B.L.; Bauer, D.C.; Drake, M.T. Osteoporosis Management in the Era of COVID-19. J. Bone Miner. Res. 2020, 35, 1009–1013. [Google Scholar] [CrossRef]
- Edelman, L.S.; McConnell, E.S.; Kennerly, S.M.; Alderden, J.; Horn, S.D.; Yap, T.L. Mitigating the Effects of a Pandemic: Facilitating Improved Nursing Home Care Delivery Through Technology. JMIR Aging 2020, 3, e20110. [Google Scholar] [CrossRef]
- Echeverría, P.; Bergas, M.A.M.; Puig, J.; Isnard, M.; Massot, M.; Vedia, M.-C.; Peiró, R.; Ordorica, Y.; Pablo, S.; Ulldemolins, M.; et al. COVIDApp as an Innovative Strategy for the Management and Follow-Up of COVID-19 Cases in Long-Term Care Facilities in Catalonia: Implementation Study. JMIR Public Health Surveill. 2020, 6, e21163. [Google Scholar]
- Danilewitz, M.; Ainsworth, N.J.; Bahji, A.; Chan, P.; Rabheru, K. Virtual psychiatric care for older adults in the age of COVID-19: Challenges & opportunities. Int. J. Geriatr. Psychiatry 2020, 35, 1468–1469. [Google Scholar]
- Naarding, P.; Voshaar, R.O.; Marijnissen, R. COVID-19: Clinical Challenges in Dutch Geriatric Psychiatry. Am. J. Geriatr. Psychiatry 2020, 28, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Archbald-Pannone, L.R.; Harris, D.A.; Albero, K.; Steele, R.L.; Pannone, A.F.; Mutter, J.B. COVID-19 Collaborative Model for an Academic Hospital and Long-Term Care Facilities. J. Am. Med. Dir. Assoc. 2020, 21, 939–942. [Google Scholar] [CrossRef] [PubMed]
- Gould, C.E.; Hantke, N.C. Promoting Technology and Virtual Visits to Improve Older Adult Mental Health in the Face of COVID-19. Am. J. Geriatr. Psychiatry 2020, 28, 889–890. [Google Scholar] [CrossRef]
- Benaque, A.; Gurruchaga, M.J.; Abdelnour, C.; Hernández, I.; Cañabate, P.; Alegret, M.; Rodríguez, I.; Rosende-Roca, M.; Tartari, J.P.; Esteban, E.; et al. Dementia Care in Times of COVID-19: Experience at Fundació ACE in Barcelona, Spain. J. Alzheimer’s Dis. 2020, 76, 33–40. [Google Scholar] [CrossRef]
- Chen, A.T.; Ge, S.; Cho, S.; Teng, A.K.; Chu, F.; Demiris, G.; Zaslavsky, O. Reactions to COVID-19, Information and Technology Use, and Social Connectedness among Older Adults with Pre-Frailty and Frailty. Geriatr. Nurs. 2020. [Google Scholar] [CrossRef]
- Seifert, A. The Digital Exclusion of Older Adults during the COVID-19 Pandemic. J. Gerontol. Soc. Work 2020, 63, 674–676. [Google Scholar] [CrossRef]
- Elbeddini, A.; Prabaharan, T.; Almasalkhi, S.; Tran, C.; Zhou, Y. Barriers to conducting deprescribing in the elderly population amid the COVID-19 pandemic. Res. Soc. Adm. Pharm. 2021, 17, 1942–1945. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.; Bardach, S.H.; Pope, N.D. COVID-19 and the Digital Divide: Will Social Workers Help Bridge the Gap? J. Gerontol. Soc. Work 2020, 63, 671–673. [Google Scholar] [CrossRef] [PubMed]
- Hartt, M. COVID-19: A lonely pandemic. Cities Health 2020, 1–3. [Google Scholar] [CrossRef]
- Hoffman, G.J.; Webster, N.J.; Bynum, J.P.W. A Framework for Aging-Friendly Services and Supports in the Age of COVID-19. J. Aging Soc. Policy 2020, 32, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Joy, M.; McGagh, D.; Jones, N.; Liyanage, H.; Sherlock, J.; Parimalanathan, V.; Akinyemi, O.; Van Vlymen, J.; Howsam, G.; Marshall, M.; et al. Reorganisation of primary care for older adults during COVID-19: A cross-sectional database study in the UK. Br. J. Gen. Pract. 2020, 70, e540–e547. [Google Scholar] [CrossRef] [PubMed]
- Seifert, A.; Cotten, S.R.; Xie, B. A Double Burden of Exclusion?Digital and Social Exclusion of Older Adults in Times of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020. [Google Scholar] [CrossRef] [PubMed]
- Eghtesadi, M. Breaking Social Isolation Amidst COVID-19: A Viewpoint on Improving Access to Technology in Long-Term Care Facilities. J. Am. Geriatr. Soc. 2020, 68, 949–950. [Google Scholar] [CrossRef] [PubMed]
- Phillips, N.A.; Chertkow, H.; Pichora-Fuller, M.K.; Wittich, W. Special Issues on Using the Montreal Cognitive Assessment for telemedicine Assessment During COVID-19. J. Am. Geriatr. Soc. 2020, 68, 942–944. [Google Scholar] [CrossRef]
- Frost, R.; Nimmons, D.; Davies, N. Using Remote Interventions in Promoting the Health of Frail Older Persons Following the COVID-19 Lockdown: Challenges and Solutions. J. Am. Med. Dir. Assoc. 2020, 21, 992–993. [Google Scholar] [CrossRef]
- Luciani, L.G.; Mattevi, D.; Cai, T.; Giusti, G.; Proietti, S.; Malossini, G. Teleurology in the Time of Covid-19 Pandemic: Here to Stay? Urology 2020, 140, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Xie, B.; Charness, N.; Fingerman, K.; Kaye, J.; Kim, M.T.; Khurshid, A. When Going Digital Becomes a Necessity: Ensuring Older Adults’ Needs for Information, Services, and Social Inclusion during COVID-19. J. Aging Soc. Policy 2020, 32, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Cooper-Brown, L.; Ivensky, V.; Launay, C.P. Telemedicine for housebound older persons during the Covid-19 pandemic. Maturitas 2020, 142, 8–10. [Google Scholar] [CrossRef] [PubMed]
- Lester, P.E.; Holahan, T.; Siskind, D.; Healy, E. Policy Recommendations Regarding Skilled Nursing Facility Management of Coronavirus 19 (COVID-19): Lessons from New York State. J. Am. Med. Dir. Assoc. 2020, 21, 888–892. [Google Scholar] [CrossRef]
- D’Adamo, H.; Yoshikawa, T.; Ouslander, J.G. Coronavirus disease 2019 in geriatrics and long-term care: The ABCDs of COVID-19. J. Am. Geriatr. Soc. 2020, 68, 912–917. [Google Scholar] [CrossRef]
- Medina-Walpole, A.; Trucil, D.E. In COVID-19 response to Congress & Administration, AGS calls for access to medical supplies, telehealth, among other needs. Geriatr. Nurs. 2020, 41, 347–348. [Google Scholar]
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef]
- Bujnowska-Fedak, M.; Grata-Borkowska, U. Use of telemedicine-based care for the aging and elderly: Promises and pitfalls. Smart Homecare Technol. TeleHealth 2015, 2015, 91–105. [Google Scholar] [CrossRef]
- Horbach, S.P.J.M. Pandemic publishing: Medical journals strongly speed up their publication process for COVID-19. Quant. Sci. Stud. 2020, 1, 1056–1067. [Google Scholar] [CrossRef]
- Palayew, A.; Norgaard, O.; Safreed-Harmon, K.; Andersen, T.H.; Rasmussen, L.N.; Lazarus, J.V. Pandemic publishing poses a new COVID-19 challenge. Nat. Hum. Behav. 2020, 4, 666–669. [Google Scholar] [CrossRef]
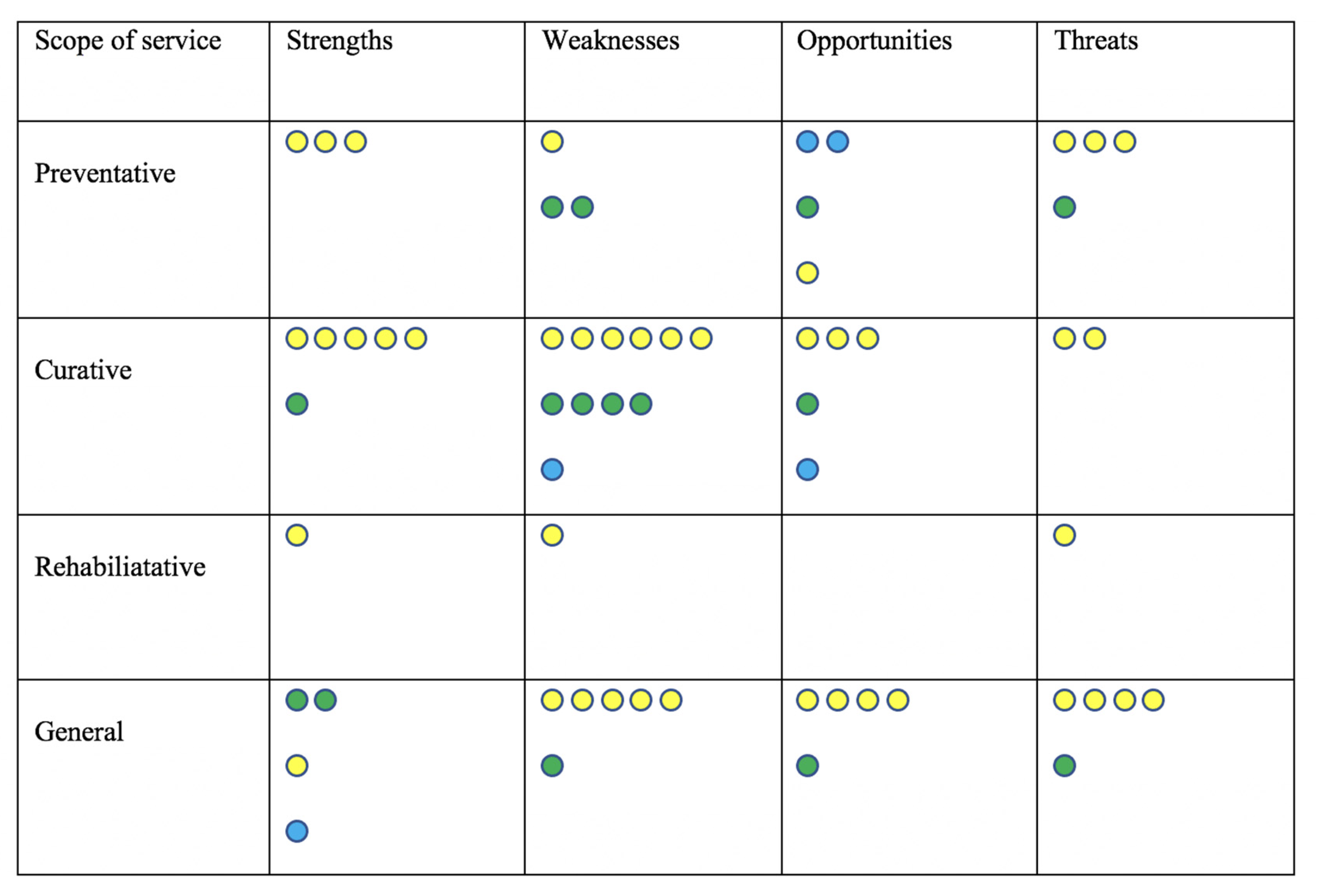
| S—Strengths Avoid over-crowding in health facilities [46] Reduction in long distance travel [46] Minimize risk of serious events such as falls [46] Improve resilience and well-being [47,48] Able to perform an assessment in the living (ecological) environment [46,49,50,51] Service patients from rural communities [52,53] Reduce secondary and tertiary infections [54] Reduce loss to follow up [55] Holistically manage dementia [52,56] Personalized management including reminders [53,57] Reduce caregiver involvement, including nursing home staff [52,58] Promote social connectedness among nursing home residents in particular [44,59] | W—Weaknesses Difficult to treat patients with cognitive impairment, visual acuity issues, and hearing problems [56,60,61,62,63,64] Gauging patient comprehension by providers [65,66] Limitation in physical examination including gait assessment [66,67,68] Lack of older people’s inclusion in the design and user-testing of telehealth interventions [56,61] Greater risk of treatment withdrawal and increased risk of hospitalization [69] Management of video connectivity problems telehealth platforms [70] Maintenance of equipment, including its sanitization and the associated extra burden [55] Lack of privacy for the older person [71] Risk of missing out on clues of elder abuse due to the lack of privacy [70] Lack of familiarity of health care professionals with telehealth platforms [65,72] |
| O—Opportunities Free communication platforms [44,59,73,74,75,76] Readily available web-based training [77,78,79] Standardized documentation and real time reporting to improve quality of care [80] Digital photographs and asynchronous sharing to circumvent connectivity issues [77] Wearable devices, remote monitoring sensors and other technologies as early warning tools [59,81] Automatic speech analysis for diagnosis and monitoring of dementia [82] Enhanced integration of specialty expertise care of nursing home residents [70,83] Possibility of daily community collaborative rounds involving multiple services providers in nursing homes [84] Technology that is easy to understand pertaining to different interfaces, passwords, and maintenance [56,70] | T—Threats Ambiguous/technical jargon for descriptive terms [85] Large variability of available telehealth platforms [70] Lack of sustained insurance reimbursement [11] Digital divide for some due to lack of equipment, limited literacy, and lack of assistance [56,63,72,86,87,88,89,90,91,92,93] Ageism/stigma leading to de-prioritization of older people [94,95] Failure to include older people in standardizing telehealth [56] Lack of tested clinical tools for telehealth use [65,96] Technical failures and patient dropout [89,97] Inaccuracy in telephone consultation [98] Difficulty for regulators in monitoring and ensuring equitable quality of care [52,65,84] |
| Older People and Caregivers Participate in communication technology training [61,73,85,91,94] Make an informed decision to use telehealth for health care services assessing the pros and cons [44,52,68,70] Discuss concerns with health care providers and explore solutions to mitigate concerns [70] Be part of blended communities that bring together online and in-person activities [91,99] Be involved in the process of standardization of telehealth use for geriatric care [70,85] | Physicians and Other Health Care Providers Get trained in assessing patients using video conference [52] Convert current in-person screening and diagnostic tools into digital versions [52] Dedicate time in asking patients questions about concerns and barriers to accessing technology [93] Redirect patients to educational community resources for telehealth use when necessary [95] |
| Technology Develop automatic speech analysis to diagnose and monitor dementia [82] Improve technology to accommodate age-related sensory and cognitive impairment [46,63,64,94] Replace ambiguous/technical jargon with easily understandable terms [64,100] Develop larger touchscreen tablets to make visual acuity less of a barrier [64,94] Use a simple and timely back-up process in the event of equipment or connectivity failure [70,97] Address hacking risk by ensuring the use of secure software [70] | Governance/Health Systems Provide educational outreach to support older adults to use digital devices [87,91,94] Ensure sanitization of telemedicine equipment [101] Sustain reimbursement for telehealth services beyond the COVID-19 pandemic [102,103] Integrate telehealth within the training curricula for both health and social care professionals and practitioners [65,70] Provide equipment such as tablets, laptops, or devices that can connect to the TV for older people and caregivers [97] Ensure free internet service to all, including older people [91,94] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doraiswamy, S.; Jithesh, A.; Mamtani, R.; Abraham, A.; Cheema, S. Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis. Int. J. Environ. Res. Public Health 2021, 18, 1755. https://doi.org/10.3390/ijerph18041755
Doraiswamy S, Jithesh A, Mamtani R, Abraham A, Cheema S. Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis. International Journal of Environmental Research and Public Health. 2021; 18(4):1755. https://doi.org/10.3390/ijerph18041755
Chicago/Turabian StyleDoraiswamy, Sathyanarayanan, Anupama Jithesh, Ravinder Mamtani, Amit Abraham, and Sohaila Cheema. 2021. "Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis" International Journal of Environmental Research and Public Health 18, no. 4: 1755. https://doi.org/10.3390/ijerph18041755
APA StyleDoraiswamy, S., Jithesh, A., Mamtani, R., Abraham, A., & Cheema, S. (2021). Telehealth Use in Geriatrics Care during the COVID-19 Pandemic—A Scoping Review and Evidence Synthesis. International Journal of Environmental Research and Public Health, 18(4), 1755. https://doi.org/10.3390/ijerph18041755






