Relationship between Mortality and Oral Function of Older People Requiring Long-Term Care in Rural Areas of Japan: A Four-Year Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
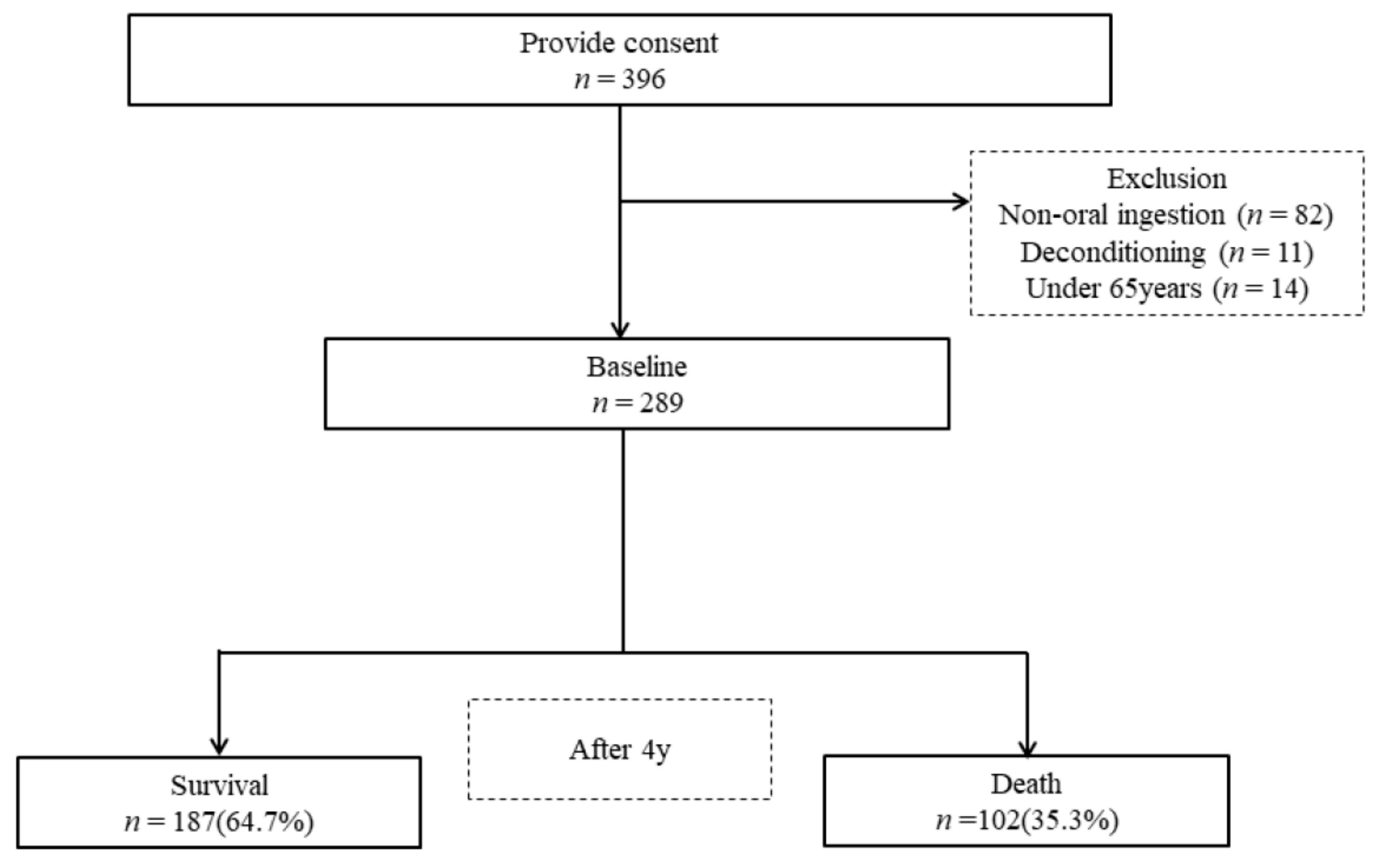
2.1. Study Design and Participants
2.2. Survey Items
2.3. Basic Information
2.4. Evaluation of Activities of Daily Living
2.5. Evaluation of Cognitive Function
2.6. Nutritional Status
2.6.1. Mini Nutritional Assessment®—Short Form (MNA®-SF)
2.6.2. Body Mass Index
2.6.3. Food Morphology
2.7. Oral Assessment
2.7.1. Number of Teeth Present
2.7.2. Rinsing Ability
2.7.3. Articulation of /TA/
2.7.4. Modified Water Swallowing Test (MWST)
2.7.5. Oral Hygiene Status
2.7.6. Oral Dryness
2.8. Statistical Analysis
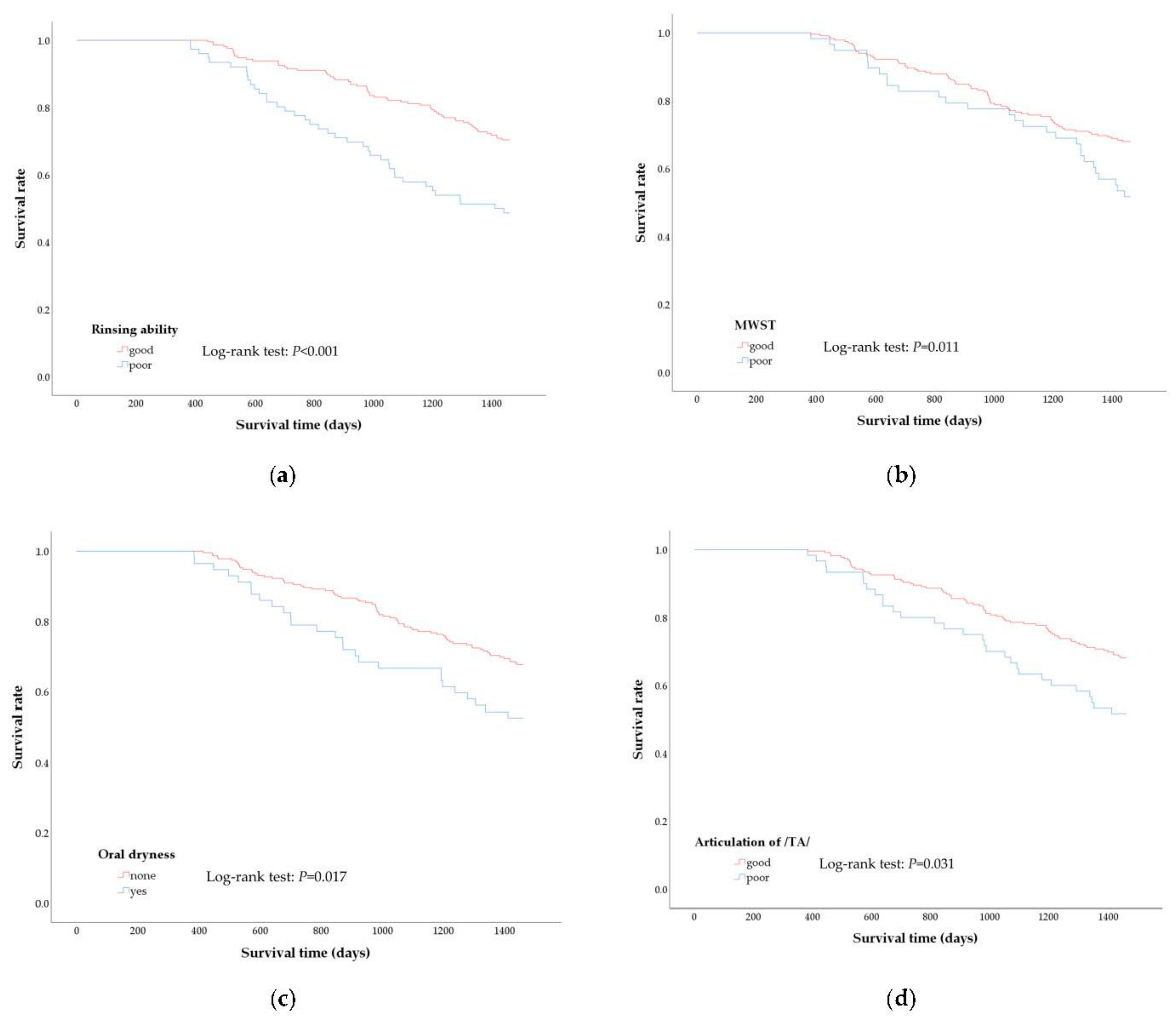
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health. Labor and Welfare. Status of Long-Term Care Insurance System. Available online: https://www.mhlw.go.jp/english/wp/wp-hw3/dl/10-06.pdf (accessed on 6 January 2021).
- Takata, Y.; Ansai, T.; Awano, S.; Hamasaki, T.; Yoshitake, Y.; Kimura, Y.; Sonoki, K.; Wakisaka, M.; Fukuhara, M.; Takehara, T. Relationship of physical fitness to chewing in an 80-year-old population. Oral Dis. 2004, 10, 44–49. [Google Scholar] [CrossRef]
- Petersen, P.E.; Yamamoto, T. Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2005, 33, 81–92. [Google Scholar] [CrossRef]
- Aida, J.; Kondo, K.; Yamamoto, T.; Hirai, H.; Nakade, M.; Osaka, K.; Sheiham, A.; Tsakos, G.; Watt, R.G. Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. J. Dent. Res. 2011, 90, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Norrie, P.T.; Villarosa, A.R.; Kong, A.C.; Clark, S.; Macdonald, S.; Srinivas, R.; Anlezark, J.; George, A. Oral health in residential aged care: Perceptions of nurses and management staff. Nurs. Open. 2020, 7, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Aida, J.; Kondo, K.; Hirai, H.; Nakade, M.; Yamamoto, T.; Hanibuchi, T.; Osaka, K.; Sheiham, A.; Tsakos, G.; Watt, R.G. Association between dental status and incident disability in an older Japanese population. J. Am. Geriatr. Soc. 2012, 60, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Adachi, M.; Ishihara, K.; Abe, S.; Okuda, K.; Ishikawa, T. Effect of professional oral health care on the elderly living in nursing homes. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 191–195. [Google Scholar] [CrossRef]
- Furuta, M.; Yamashita, Y. Oral health and swallowing problems. Curr. Phys. Med. Rehabil. Rep. 2013, 1, 216–222. [Google Scholar] [CrossRef]
- Vesey, S. Dysphagia and quality of life. Br. J. Commun. Nurs. 2013, 18, S14–S19. [Google Scholar] [CrossRef]
- Lieu, P.K.; Chong, M.S.; Seshadri, R. The impact of swallowing disorders in the elderly. Ann. Acad. Med. Singapore. 2001, 30, 148–154. [Google Scholar]
- Tanaka, T.; Takahashi, K.; Hirano, H.; Kikutani, T.; Watanabe, Y.; Ohara, Y.; Furuya, H.; Tetsuo, T.; Akishita, M.; Iijima, K. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1661–1667. [Google Scholar] [CrossRef]
- Enomoto, R.; Kikutani, T.; Suzuki, A.; Inaba, S. Relationship between eating dysfunction and life span and mortality in institutionalized elderly people. Nihon Ronen Igakkai Zasshi 2007, 44, 95–101. [Google Scholar] [CrossRef]
- Hoshino, D.; Watanabe, Y.; Edahiro, A.; Kugimiya, Y.; Igarashi, K.; Motokawa, K.; Ohara, Y.; Hirano, H.; Myers, M.; Hironaka, S.; et al. Association between simple evaluation of eating and swallowing function and mortality among patients with advanced dementia in nursing homes: 1-year prospective cohort study. Arch. Gerontol. Geriatr. 2020, 87, 103969. [Google Scholar] [CrossRef]
- Morishita, S.; Watanabe, Y.; Ohara, Y.; Edahiro, A.; Sato, E.; Suga, T.; Hirano, H. Factors associated with older adults’ need for oral hygiene management by dental professionals. Geriatr. Gerontol. Int. 2016, 16, 956–962. [Google Scholar] [CrossRef]
- Murakami, K.; Hirano, H.; Watanabe, Y.; Edahiro, A.; Ohara, Y.; Yoshida, H.; Kim, H.; Takagi, D.; Hironaka, S. Relationship between swallowing function and the skeletal muscle mass of older adults requiring long-term care. Geriatr. Gerontol. Int. 2015, 15, 1185–1192. [Google Scholar] [CrossRef]
- Mahoney, F.L.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State. Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Morris, J.C. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology 1993, 43, 2412–2414. [Google Scholar] [CrossRef] [PubMed]
- Washington University Alzheimer’s Disease Research Center. Global Clinical Dementia Rating (CDR) Based on CDR Box Scores. Available online: https://biostat.wustl.edu/adrc/cdrpgm/index.html (accessed on 6 January 2021).
- Vellas, B.; Villars, H.; Abellan, G.; Soto, M.E.; Rolland, Y.; Guigoz, Y.; Morley, J.E.; Chumlea, W.; Salva, A.; Rubenstein, L.Z.; et al. Overview of the MNA®-Its history and challenges. J. Nutr. Health Aging. 2006, 10, 456–465. [Google Scholar] [PubMed]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment Short-Form (MNA®-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging. 2009, 13, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Academy of Nutrition and Dietetics. IDDSI Framework and Detailed Level Definitions. International Dysphagia Diet Standardisation Initiative. July 2019. Available online: https://iddsi.org/Framework (accessed on 6 January 2021).
- Sato, E.; Hirano, H.; Watanabe, Y.; Edahiro, A.; Sato, K.; Yamane, G.; Katakura, A. Detecting signs of dysphagia in patients with Alzheimer’s disease with oral feeding in daily life. Geriatr. Gerontol. Int. 2014, 14, 549–555. [Google Scholar] [CrossRef]
- Zenner, P.M.; Losinski, D.S.; Mills, R.H. Using cervical auscultation in the clinical dysphagia examination in long-term care. Dysphagia 1995, 10, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Tohara, H.; Saitoh, E.; Mays, K.A.; Kuhlemeier, K.; Palme, J.B. Three tests for predicting aspiration without videofluorography. Dysphagia 2003, 18, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Hirano, H.; Watanabe, Y.; Tohara, H.; Sato, E.; Sato, K.; Katakura, A. An examination of factors related to aspiration and silent aspiration in older adults requiring long-term care in rural Japan. J. Oral Rehabil. 2016, 43, 103–110. [Google Scholar] [CrossRef]
- Kakinoki, Y.; Nishihara, T.; Arita, M.; Shibuya, K.; Ishikawa, M. Usefulness of new wetness tester for diagnosis of dry mouth in disabled patients. Gerodontology 2004, 21, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Astor, F.C.; Hanft, K.L.; Ciocon, J.O. Xerostomia: A prevalent condition in the elderly. Ear Nose Throat J. 1999, 78, 476–479. [Google Scholar] [CrossRef]
- Marcott, S.; Dewan, K.; Kwan, M.; Baik, F.; Lee, Y.J.; Sirjani, D. Where dysphagia begins: Polypharmacy and xerostomia. Fed. Pract. 2020, 37, 234–241. [Google Scholar]
- Edwin, C.K.T.; Duangjai, L.; Gunilla, S.E.; Ylva, H.; Kristina, J. Medications that cause dry mouth as an adverse effect in older people: A systematic review and metaanalysis. J. Am. Geriatr. Soc. 2018, 66, 76–84. [Google Scholar]
- Visvanathan, V.; Nix, P. Managing the patient presenting with xerostomia: A review. Int. J. Clin. Pract. 2010, 64, 404–407. [Google Scholar] [CrossRef]
- Navazesh, M.; Kumar, S.K.S. Xerostomia: Prevalence, diagnosis, and management. Compend. Contin. Educ. Dent. 2009, 30, 326–334. [Google Scholar]
- Malicka, B.; Kaczmarek, U.; Skośkiewicz-Malinowska, K. Prevalence of xerostomia and the salivary flow rate in diabetic patients. Adv. Clin. Exp. Med. 2014, 23, 225–233. [Google Scholar] [CrossRef]
- Lu, T.Y.; Chen, J.H.; Du, J.K.; Lin, Y.C.; Ho, P.S.; Lee, C.H.; Hu, C.Y.; Huang, H.L. Dysphagia and masticatory performance as a mediator of the xerostomia to quality of life relation in the older population. BMC Geriatr. 2020, 20, 521. [Google Scholar] [CrossRef]
- Barbe, A.G.; Schmidt, P.; Bussmann, M.; Kunter, H.; Noack, M.J.; Röhrig, G. Xerostomia and hyposalivation in orthogeriatric patients with fall history and impact on oral health-related quality of life. Clin. Interv. Aging. 2018, 13, 1971–1979. [Google Scholar] [CrossRef]
- Dormenval, V.; Budtz-Jørgensen, E.; Mojon, P.; Bruyère, A.; Rapin, C.H. Associations between malnutrition, poor general health and oral dryness in hospitalized elderly patients. Age Ageing. 1998, 27, 123–128. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lugger, K.E. Dysphagia in the elderly stroke patient. J Neurosci Nurs. 1994, 26, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, Y.; Fu, B.; Yonemoto, K.; Akifusa, S.; Shibata, Y.; Takeshita, T.; Minomiya, T.; Kiyohara, Y.; Yamashita, Y. Stimulated salivary flow rate and oral health status. J. Oral Sci. 2017, 59, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Yoneyama, T.; Yoshida, M.; Ohrui, T.; Mukaiyama, H.; Okamot, H.; Hoshiba, K.; Ihara, S.; Yanagisawa, S.; Ariumi, S.; Morita, T.; et al. Oral care reduces pneumonia in older patients in nursing homes. J. Am. Geriatr. Soc. 2002, 50, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Marik, P.E.; Kaplan, D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003, 124, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Motokawa, K.; Yasuda, J.; Mikami, Y.; Edahiro, A.; Morishita, S.; Shirobe, M.; Ohara, Y.; Nohara, K.; Hirano, H.; Watanabe, Y. The Mini Nutritional Assessment-Short Form as a predictor of nursing home mortality in Japan: A 30-month longitudinal study. Arch. Gerontol. Geriatr. 2020, 86, 103945. [Google Scholar] [CrossRef]
- Nykänen, I.; Lönnroos, E.; Kautiainen, H.; Sulkava, R.; Hartikainen, S. Nutritional screening in a population-based cohort of community-dwelling older people. Eur. J. Public Health. 2013, 23, 405–409. [Google Scholar] [CrossRef]
- Kim, J.J.; Lee, Y.; Won, C.W.; Lee, K.E.; Chon, D. Nutritional status and frailty in community-dwelling older Korean adults: The Korean frailty and aging cohort study. J. Nutr. Health Aging. 2018, 22, 774–778. [Google Scholar] [CrossRef]
- Sonoki, K.; Akifusa, S.; Fukuhara, M.; Soh, I.; Awano, S.; Ansai, T. The impact of diabetes mellitus on mortality in Japanese individuals who are 80 years old in the general population. J. Jpn. Diab. Soc. 2017, 60, 515–523. [Google Scholar]
- Lin, C.C.; Sun, S.S.; Kao, A.; Lee, C.C. Impaired salivary function in patients with noninsulin-dependent diabetes mellitus with xerostomia. J. Diabetes Complicat. 2002, 16, 176–179. [Google Scholar] [CrossRef]
- Chavez, E.M.; Taylor, G.W.; Borrell, L.N.; Ship, J.A. Salivary function and glycemic control in older persons with diabetes. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 89, 305–311. [Google Scholar] [CrossRef]
- Kao, C.H.; Tsai, S.C.; Sun, S.S. Scintigraphic evidence of poor salivary function in type 2 diabetes. Diabetes Care 2001, 24, 952–953. [Google Scholar] [CrossRef]
- Hartelius, L.; Lillvik, M. Lip and tongue function differently affected in individuals with multiple sclerosis. Folia Phoniatr. Logop. 2003, 55, 1–9. [Google Scholar] [CrossRef]
- Edahiro, A.; Hirano, H.; Yamada, R.; Chiba, Y.; Watanabe, Y. Comparative study of eating behavior in elderly patients with Alzheimer’s disease and vascular dementia: A first report―Comparison of disturbed eating behavior. Nihon Ronen Igakkai Zasshi. 2013, 50, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Navazesh, M. Methods for collecting saliva. Ann. NY Acad. Sci. 1993, 694, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Navazesh, M.; Christensen, C.M. A comparison of whole mouth resting and stimulated salivary measurement procedures. J. Dent. Res. 1982, 61, 1158–1162. [Google Scholar] [CrossRef] [PubMed]
- Vitali, C.; Bombardieri, S.; Moutsopoulos, H.M.; Balestrieri, G.; Bencivelli, W.; Bernstein, R.M.; Bjerrum, K.B.; Braga, S.; Coil, J.; de Vita, S.; et al. Preliminary criteria for the classification of Sjögren’s syndrome. Results of a prospective concerted action supported by the European Community. Arthritis Rheu. 1993, 36, 340–347. [Google Scholar] [CrossRef]
- Leite, R.S.; Marlow, N.M.; Fernandes, J.K.; Hermayer, K. Oral health and type 2 diabetes. Am. J. Med. Sci. 2013, 345, 271–273. [Google Scholar] [CrossRef]
- Takahashi, F.; Takahashi, K.; Morita, O. Oral dryness examinations: Use of an oral moisture checking device and a modified cotton method. Prosthodont. Res. Pract. 2006, 5, 26–30. [Google Scholar] [CrossRef]
- Sundaram, M.; Manikandan, S.; Satheesh, B.; Srinivasan, D.; Jayapal, D.; Kumar, D. Comparative evaluation of xerostomia among diabetic and nondiabetic subjects wearing complete denture. J. Pharm. Bioallied. Sci. [CrossRef] [PubMed]
- Kikutani, T.; Tamura, F.; Tashiro, H.; Yoshida, M.; Konishi, K.; Hamada, R. Relationship between oral bacteria count and pneumonia onset in elderly nursing home residents. Geriatr. Gerontol. Int. 2015, 15, 417–421. [Google Scholar] [CrossRef]
- Ogama, N.; Suzuki, S. Adverse effects and appetite suppression associated with particle beam therapy in patients with head and neck cancer. Jpn, J. Nurs. Sci. 2012, 9, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, Y.; Saito, M.; Nonoyama, T.; Tadokoro, Y. Oral factors associated with swallowing function in independent elders. Oral Health Prev. Dent. 2020, 18, 683–692. [Google Scholar] [PubMed]
- Shindo, H.; Kikutani, T.; Yoshida, M.; Yajima, Y.; Tamura, F. Signs for identifying risk factors for aspiration pneumonia in elderly people needing nursing care. Arch. Med. Res. 2016, 4. Available online: https://esmed.org/MRA/mra/article/view/754 (accessed on 17 January 2021).
- Steinbach, U. Social networks, institutionalization, and mortality among elderly people in the United States. J. Gerontol. 1992, 47, 183–190. [Google Scholar] [CrossRef]
- Luppa, M.; Luck, T.; Matschinger, H.; König, H.H.; Riedel Heller, S.G. Predictors of nursing home admission of individuals without a dementia diagnosis before admission: Results from the Leipzig Longitudinal Study of the Aged (LEILA 75+). BMC Health Serv. Res. 2010, 10, 186. [Google Scholar] [CrossRef] [PubMed]
- Strayer, M.S. Perceived barriers to oral health care among the home-bound. Spec. Care Dentist. 1995, 15, 113–118. [Google Scholar] [CrossRef]
- Strayer, M.S. Dental health among homebound elderly. J. Public Health Dent. 1993, 53, 12–16. [Google Scholar] [CrossRef]
| All (n = 289) | Survival (n = 187) | Death (n = 102) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| n (%) | Median | n (%) | Median | n (%) | Median | ||
| (Q1,Q3) | (Q1,Q3) | (Q1,Q3) | |||||
| Age (years) | 86 | 85 | 88 | <0.001 a | |||
| (81,90) | (79,90) | (84,93) | |||||
| Gender | |||||||
| Women | 222(76.8) | 151(80.7) | 71(69.6) | 0.032 b | |||
| Men | 67(23.2) | 36(19.3) | 31(30.4) | ||||
| Observation period (days) | 1461 | 1461 | 934 | <0.001 a | |||
| (1137,1461) | (1461,1461) | (632.5, 1197.8) | |||||
| Facility classification | |||||||
| Home care | 59(20.4) | 42(22.5) | 17(16.7) | 0.115 b | |||
| Elderly facility/medical ward | 178(61.6) | 107(57.2) | 71(69.6) | ||||
| Group home for senile people | 52(18.0) | 38(20.3) | 14(13.7) | ||||
| Medical history (presence) | |||||||
| Respiratory disease | 10(3.5) | 5(2.7) | 5(4.9) | 0.322 b | |||
| Aspiration pneumonia | 7(2.4) | 4(2.1) | 3(2.9) | 0.672 b | |||
| Cerebrovascular disorder | 105(36.3) | 67(35.8) | 38(37.3) | 0.810 b | |||
| Circulatory disorder | 90(31.1) | 56(29.9) | 34(33.3) | 0.552 b | |||
| Neoplastic disease | 21(7.3) | 12(6.4) | 9(8.8) | 0.451 b | |||
| Neurological disease | 7(2.4) | 5(2.7) | 2(2.0) | 0.706 b | |||
| Parkinson’s disease | 8(2.8) | 6(3.2) | 2(2.0) | 0.537 b | |||
| Diabetes mellitus | 48(16.6) | 27(14.4) | 21(20.6) | 0.179 b | |||
| Number of medications | |||||||
| ≦3 types | 66(22.8) | 35(18.7) | 31(30.4) | 0.067 b | |||
| ≧4 types | 213(73.7) | 146(78.1) | 67(65.7) | ||||
| Unknown | 10(3.5) | 6(3.2) | 4(3.9) | ||||
| BI (score) | 45 | 55 | 15 | <0.001 a | |||
| (10,7) | (15,80) | (5,50) | |||||
| CDR (score) | |||||||
| 0/0.5 | 51(17.6) | 38(20.3) | 13(12.7) | 0.001 b | |||
| 1 | 78(27.0) | 61(32.6) | 17(16.7) | ||||
| 2 | 87(30.1) | 52(27.8) | 35(34.3) | ||||
| 3 | 73(25.3) | 36(19.3) | 37(36.3) | ||||
| BMI (kg/m2) | 21.3 | 22.2 | 20.2 | <0.001 a | |||
| (19.1, 24.5) | (19.8, 25.3) | (17.7, 23.1) | |||||
| MNA®-SF (score) | |||||||
| Normal nutritional status | 83(28.8) | 66(35.3) | 17(16.8) | <0.001 b | |||
| At risk of malnutrition | 153(53.1) | 99(52.9) | 54(53.5) | ||||
| Malnourished | 52(18.1) | 22(11.8) | 30(29.7) | ||||
| Food type | |||||||
| Regular diet | 136(47.1) | 101(54.0) | 35(34.3) | 0.001 b | |||
| Defined formula diet | 153(52.9) | 86(46.0) | 67(65.7) | ||||
| Number of present teeth | 0 | 0 | 0 | 0.236 a | |||
| (0,5) | (0,6) | (0, 4.3) | |||||
| Rinsing ability (poor) | 76(26.3) | 37(19.8) | 39(38.2) | 0.001 b | |||
| Articulation of/TA/(poor) | 60(20.8) | 31(16.6) | 29(28.4) | 0.018 b | |||
| MWST (poor) | 58(20.1) | 30(16.0) | 28(27.5) | 0.021 b | |||
| State of dental plaque (present) | 102(35.3) | 64(34.2) | 38(37.3) | 0.606 b | |||
| State of tongue coating (present) | 151(52.2) | 98(52.4) | 53(52.0) | 0.942 b | |||
| Oral dryness (present) | 57(19.7) | 30(16.0) | 27(26.5) | 0.033 b | |||
| Variable | H.R. | 95%CI | p-Value | ||
|---|---|---|---|---|---|
| Age | 1.07 | 1.03 | − | 1.11 | <0.001 |
| Gender (woman = 1) | 0.38 | 0.23 | − | 0.63 | <0.001 |
| BI | 0.98 | 0.97 | − | 1.00 | 0.006 |
| Medical history (yes = 1) | |||||
| Aspiration pneumonia | 1.33 | 0.36 | − | 5.01 | 0.670 |
| Cerebrovascular disorder | 0.97 | 0.63 | − | 1.51 | 0.901 |
| Circulatory disorder | 1.17 | 0.74 | − | 1.86 | 0.503 |
| Neoplastic disease | 1.98 | 0.94 | − | 4.17 | 0.071 |
| Diabetes mellitus | 1.80 | 1.07 | − | 3.04 | 0.028 |
| Number of medications (≧3 types = 1) | 0.91 | 0.56 | − | 1.46 | 0.682 |
| CDR | |||||
| 0/0.5 | Reference | ||||
| 1 | 0.74 | 0.33 | − | 1.66 | 0.471 |
| 2 | 0.99 | 0.46 | − | 2.14 | 0.983 |
| 3 | 1.31 | 0.53 | − | 3.23 | 0.559 |
| MNA®-SF | |||||
| Normal nutritional status | Reference | ||||
| At risk of malnutrition | 1.17 | 0.60 | − | 2.31 | 0.641 |
| Malnourished | 1.66 | 0.74 | − | 3.74 | 0.218 |
| Food morphology (defined formula diet = 1) | 0.86 | 0.47 | − | 1.56 | 0.621 |
| Rinsing ability (poor = 1) | 1.18 | 0.70 | − | 2.00 | 0.538 |
| Articulation of /TA/ (poor = 1) | 0.71 | 0.39 | − | 1.31 | 0.272 |
| MWST (poor = 1) | 0.92 | 0.54 | − | 1.57 | 0.770 |
| Oral dryness (yes = 1) | 1.83 | 1.12 | − | 3.00 | 0.015 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morishita, S.; Ohara, Y.; Iwasaki, M.; Edahiro, A.; Motokawa, K.; Shirobe, M.; Furuya, J.; Watanabe, Y.; Suga, T.; Kanehisa, Y.; et al. Relationship between Mortality and Oral Function of Older People Requiring Long-Term Care in Rural Areas of Japan: A Four-Year Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 1723. https://doi.org/10.3390/ijerph18041723
Morishita S, Ohara Y, Iwasaki M, Edahiro A, Motokawa K, Shirobe M, Furuya J, Watanabe Y, Suga T, Kanehisa Y, et al. Relationship between Mortality and Oral Function of Older People Requiring Long-Term Care in Rural Areas of Japan: A Four-Year Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(4):1723. https://doi.org/10.3390/ijerph18041723
Chicago/Turabian StyleMorishita, Shiho, Yuki Ohara, Masanori Iwasaki, Ayako Edahiro, Keiko Motokawa, Maki Shirobe, Junichi Furuya, Yutaka Watanabe, Takeo Suga, Yayoi Kanehisa, and et al. 2021. "Relationship between Mortality and Oral Function of Older People Requiring Long-Term Care in Rural Areas of Japan: A Four-Year Prospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 4: 1723. https://doi.org/10.3390/ijerph18041723
APA StyleMorishita, S., Ohara, Y., Iwasaki, M., Edahiro, A., Motokawa, K., Shirobe, M., Furuya, J., Watanabe, Y., Suga, T., Kanehisa, Y., Ohuchi, A., & Hirano, H. (2021). Relationship between Mortality and Oral Function of Older People Requiring Long-Term Care in Rural Areas of Japan: A Four-Year Prospective Cohort Study. International Journal of Environmental Research and Public Health, 18(4), 1723. https://doi.org/10.3390/ijerph18041723






