Smartphone Use and Willingness to Pay for HIV Treatment-Assisted Smartphone Applications among HIV-Positive Patients in Urban Clinics of Vietnam
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Sampling Method, and Data Collection
2.2. Instruments
2.3. Data Analysis
2.4. Ethical Consideration
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Code | Questions | Answers |
|---|---|---|
| S1 | What operational system are you using? | 1. iOS 2. Android 3. Other (please specify) |
| S2 | How long have you used smartphone? | (month) |
| S3 | On the average, how many hours per day do you use smartphone? | hour(s)/day |
| S4 | How many health-related apps have you used since the last 30 days? | 0. No → S11 number of apps |
| S5 | On the average, how many minutes per day do you spend for using health-related apps? | minutes |
| S6 | When do you often use those health-related apps? | 1. In the early morning when you wake up 2. In the late morning 3. At noon 4. Afternoon 5. Evening 6. Before nigh sleep |
| S7 | On the average, how many minutes per time do you spend for using health-related apps? | minutes |
| S8 | What is the functionality of the health-related apps you use most? | 1.Taking pill reminder 2. Smoking cessation 3. Drinking cessation 4. Receiving health-related information 5. Connecting with physicians 6. Other (please specify) |
| S9 | If 100 means “completely useful”, 0 means “completely useless” how much would you rate the above-mentioned health-related app? | (points) |
| S10 | If 100 means “complete satisfaction”, 0 means “complete dissatisfaction” how much would you rate the above-mentioned health-related app? | (points) |
| S11 | Do you want a smartphone-based HIV/AIDS treatment-assisted app? | 1.Yes 2. No→ S13 |
| S12 | To what extent do you perceive necessity of the above-mentioned app? | 1.Very necessary 2. Necessary 3. So-so 4. Unnecessary 5. Very unnecessary |
| S13 | Are you willing to pay for a smartphone app that assists you in taking pill reminder, managing your medical records, updating health-related information, and contacting nearby physicians and health facilities? | 1.Yes 2. No→ S15 |
| S14 | How much are you willing to pay for the above-mentioned app? | thousand VND/month → End survey |
| S15 | Why aren’t you willing to pay for the above-mentioned app? | 1.Unnecessary 2. Unaffordable 3. Fear of HIV disclosure, stigmatization 4. Other (please specify) |
| Variables | WTP for Smartphone App | Natural Log of the Amount of WTP | ||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Education (Elementary school or less-ref) | ||||||||
| Secondary school | 0.91 | 0.74; 1.13 | −0.23 | −0.52; 0.06 | ||||
| High school | 0.97 | 0.79; 1.20 | −0.03 | −0.33; 0.26 | ||||
| Above high school | 1.15 | 0.94; 1.39 | −0.09 | −0.39; 0.22 | ||||
| Marital status (single-ref) | ||||||||
| Separate/Divorced/Widow | 1.46 *** | 1.17; 1.82 | ||||||
| Having spouse/partner | 1.28 ** | 1.06; 1.56 | ||||||
| Age (years) | −0.01 ** | −0.03; −0.00 | ||||||
| Duration of ART (years) | 0.96 *** | 0.94; 0.99 | ||||||
| Using alcohol (Yes vs. No-ref) | −0.16 * | −0.34; 0.02 | 0.28 ** | 0.07; 0.49 | ||||
| Initial CD4 cell count | 1.00 | 1.00; 1.00 | ||||||
| Using health services in the last 12 months (Yes vs. No -ref) | 1.04 *** | 1.02; 1.07 | 1.01 * | 1.00; 1.02 | −0.06 ** | −0.12; −0.01 | −0.03 | −0.06; 0.01 |
| Having any health problems (Yes vs. No-ref) | 1.10 | 0.97; 1.24 | ||||||
| Variables | WTP for Smartphone App | Natural Log of the Amount of WTP | ||||||
|---|---|---|---|---|---|---|---|---|
| ≤40 Years Old | >40 Years Old | ≤40 Years Old | >40 Years Old | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Marital status (single-ref) | ||||||||
| Separate/divorced/widow | 1.19 ** | 1.01; 1.40 | ||||||
| Having spouse/partner | 1.13 | 0.98; 1.30 | ||||||
| Sex (Female vs. Male–ref) | 1.25 ** | 1.01; 1.55 | ||||||
| Duration of ART (years) | 0.97 ** | 0.95; 0.99 | ||||||
| Current drug user (Yes vs. No-ref) | 0.83 * | 0.67; 1.02 | ||||||
| Current smoker (Yes vs. No-ref) | 0.90 * | 0.80; 1.01 | 1.32 ** | 1.03; 1.69 | ||||
| Initial CD4 cell count | 1.00 * | 1.00; 1.00 | ||||||
| Self-rate health status (score) | 0.01 * | −0.00; 0.01 | 0.01 * | −0.00; 0.01 | ||||
| Using health services in the last 12 months (Yes vs. No-ref) | 1.02 *** | 1.01; 1.04 | 1.03 *** | 1.01; 1.05 | −0.06 ** | −0.11; −0.01 | −0.06 ** | −0.11; −0.01 |
References
- Parczewski, M.; Siwak, E.; Leszczyszyn-Pynka, M.; Cielniak, I.; Burkacka, E.; Pulik, P.; Witor, A.; Muller, K.; Zasik, E.; Grzeszczuk, A.; et al. Meeting the WHO 90% target: Antiretroviral treatment efficacy in Poland is associated with baseline clinical patient characteristics. J. Int. Aids Soc. 2017, 20, 21847. [Google Scholar] [CrossRef]
- Safren, S.A.; Mayer, K.H.; Ou, S.S.; McCauley, M.; Grinsztejn, B.; Hosseinipour, M.C.; Kumarasamy, N.; Gamble, T.; Hoffman, I.; Celentano, D.; et al. Adherence to Early Antiretroviral Therapy: Results From HPTN 052, a Phase III, Multinational Randomized Trial of ART to Prevent HIV-1 Sexual Transmission in Serodiscordant Couples. J. Acquir. Immune Defic. Syndr. 2015, 69, 234–240. [Google Scholar] [CrossRef]
- Lundgren, J.D.; Babiker, A.G.; Gordin, F.; Emery, S.; Grund, B.; Sharma, S.; Avihingsanon, A.; Cooper, D.A.; Fätkenheuer, G.; Llibre, J.M.; et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N. Engl. J. Med. 2015, 373, 795–807. [Google Scholar] [CrossRef] [PubMed]
- Mburu, G.; Igbinedion, E.; Lim, S.H.; Paing, A.Z.; Yi, S.; Elbe, S.; Mwai, G.W. Outcomes of HIV treatment from the private sector in low-income and middle-income countries: A systematic review protocol. BMJ Open 2020, 10, e031844. [Google Scholar] [CrossRef]
- Rossouw, T.; Tucker, J.D.; van Zyl, G.U.; Sikwesi, K.; Godfrey, C. Barriers to HIV remission research in low- and middle-income countries. J. Int. Aids Soc. 2017, 20, 21521. [Google Scholar] [CrossRef] [PubMed]
- Gardner, E.M.; Hullsiek, K.H.; Telzak, E.E.; Sharma, S.; Peng, G.; Burman, W.J.; MacArthur, R.D.; Chesney, M.; Friedland, G.; Mannheimer, S.B. Antiretroviral medication adherence and class- specific resistance in a large prospective clinical trial. Aids (Lond. Engl.) 2010, 24, 395–403. [Google Scholar] [CrossRef]
- Penn, A.W.; Azman, H.; Horvath, H.; Taylor, K.D.; Hickey, M.D.; Rajan, J.; Negussie, E.K.; Doherty, M.; Rutherford, G.W. Supportive interventions to improve retention on ART in people with HIV in low- and middle-income countries: A systematic review. PLoS ONE 2018, 13, e0208814. [Google Scholar] [CrossRef]
- Amankwaa, I.; Boateng, D.; Quansah, D.Y.; Akuoko, C.P.; Evans, C. Effectiveness of short message services and voice call interventions for antiretroviral therapy adherence and other outcomes: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0204091. [Google Scholar] [CrossRef] [PubMed]
- Muessig, K.E.; Le Grand, S.; Horvath, K.J.; Bauermeister, J.A.; Hightow-Weidman, L.B. Recent mobile health interventions to support medication adherence among HIV-positive MSM. Curr. Opin. HIV Aids 2017, 12, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Pantoja, T.; Opiyo, N.; Lewin, S.; Paulsen, E.; Ciapponi, A.; Wiysonge, C.S.; Herrera, C.A.; Rada, G.; Peñaloza, B.; Dudley, L.; et al. Implementation strategies for health systems in low-income countries: An overview of systematic reviews. Cochrane Database Syst. Rev. 2017, 9, Cd011086. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Dang, A.K.; Truong, N.T.; Ha, G.H.; Nguyen, H.L.T.; Do, H.N.; Nguyen, T.Q.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Depression and Quality of Life among Patients Living with HIV/AIDS in the Era of Universal Treatment Access in Vietnam. Int. J. Environ. Res. Public Health 2018, 15, 2888. [Google Scholar] [CrossRef]
- Do, T.N.; Nguyen, T.M.; Do, M.H.; Masaya, K.; Dang, T.B.; Pham, T.L.; Yoshikawa, K.; Cao, T.T.; Nguyen, T.T.; Bui, D.D.; et al. Combining cohort analysis and monitoring of HIV early-warning indicators of drug resistance to assess antiretroviral therapy services in Vietnam. Clin. Infect. Dis. 2012, 54 (Suppl. 4), S306–S312. [Google Scholar] [CrossRef]
- Guideline of HIV/Aids Treatment and Care; Ministry of Health: Hanoi, Vietnam, 2017.
- Report on HIV/Aids Prevention and Control in the First Six Months of 2016 and the Key Tasks in the Last 6 Months of 2016; Ministry of Health: Hanoi, Vietnam, 2016.
- Tran, B.X.; Houston, S. Mobile phone-based antiretroviral adherence support in Vietnam: Feasibility, patient‘s preference, and willingness-to-pay. Aids Behav. 2012, 16, 1988–1992. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Tran, B.X.; Hwang, L.Y.; Markham, C.M.; Swartz, M.D.; Vidrine, J.I.; Phan, H.T.; Latkin, C.A.; Vidrine, D.J. Effects of cigarette smoking and nicotine dependence on adherence to antiretroviral therapy among HIV-positive patients in Vietnam. Aids Care 2016, 28, 359–364. [Google Scholar] [CrossRef]
- Mai, H.T.; Le, G.M.; Tran, B.X.; Do, H.N.; Latkin, C.A.; Nguyen, L.T.; Thai, T.P.T.; Le, H.T.; Ngo, A.T.; Nguyen, C.T.; et al. Adherence to antiretroviral therapy among HIV/ AIDS patients in the context of early treatment initiation in Vietnam. Patient Prefer Adherence 2018, 12, 2131–2137. [Google Scholar] [CrossRef]
- Than, P.Q.T.; Tran, B.X.; Nguyen, C.T.; Truong, N.T.; Thai, T.P.T.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Stigma against patients with HIV/AIDS in the rapid expansion of antiretroviral treatment in large drug injection-driven HIV epidemics of Vietnam. Harm Reduct. J. 2019, 16, 6. [Google Scholar] [CrossRef] [PubMed]
- Silver, L.; Johnson, C.; Jiang, J.; Anderson, M.; Rainie, L. Use of Smartphones and Social Media is Common across Most Emerging Economies. Available online: https://www.pewresearch.org/internet/2019/03/07/use-of-smartphones-and-social-media-is-common-across-most-emerging-economies/ (accessed on 10 April 2020).
- Vu, T.M.T.; Boggiano, V.L.; Tran, B.X.; Nguyen, L.H.; Tran, T.T.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Sexual Risk Behaviors of Patients with HIV/AIDS over the Course of Antiretroviral Treatment in Northern Vietnam. Int. J. Environ. Res. Public Health 2018, 15, 1106. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Nguyen, L.H.; Nguyen, C.T.; Phan, H.T.T.; Latkin, C.A. Alcohol abuse increases the risk of HIV infection and diminishes health status of clients attending HIV testing services in Vietnam. Harm Reduct. J. 2016, 13, 6. [Google Scholar] [CrossRef]
- Niakan, S.; Mehraeen, E.; Noori, T.; Gozali, E. Web and Mobile Based HIV Prevention and Intervention Programs Pros and Cons—A Review. Stud. Health Technol. Inf. 2017, 236, 319–327. [Google Scholar]
- Shet, A.; Arumugam, K.; Rodrigues, R.; Rajagopalan, N.; Shubha, K.; Raj, T.; D’Souza, G.; De Costa, A. Designing a mobile phone-based intervention to promote adherence to antiretroviral therapy in South India. Aids Behav. 2010, 14, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Pop-Eleches, C.; Thirumurthy, H.; Habyarimana, J.P.; Zivin, J.G.; Goldstein, M.P.; de Walque, D.; MacKeen, L.; Haberer, J.; Kimaiyo, S.; Sidle, J.; et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: A randomized controlled trial of text message reminders. AIDS 2011, 25, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Nguyen, Q.N.; Dang, A.K.; Vu, G.T.; Hoang, V.Q.; La, P.V.; Hoang, D.A.; Van Dam, N.; Vuong, T.T.; Nguyen, L.H.; et al. Acceptability of and willingness to pay for using a smartphone-based vaccination application in a Vietnamese cohort. Patient Prefer Adherence 2018, 12, 2583–2591. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Le, X.T.T.; Nguyen, P.N.; Le, Q.N.H.; Mai, H.T.; Nguyen, H.L.T.; Le, H.T.; Tran, T.T.; Latkin, C.A.; Zhang, M.W.B.; et al. Feasibility of e-Health Interventions on Smoking Cessation among Vietnamese Active Internet Users. Int. J. Environ. Res. Public Health 2018, 15, 165. [Google Scholar] [CrossRef] [PubMed]
- Lam, J.A.; Dang, L.T.; Phan, N.T.; Trinh, H.T.; Vu, N.C.; Nguyen, C.K. Mobile Health Initiatives in Vietnam: Scoping Study. Jmir Mhealth Uhealth 2018, 6, e106. [Google Scholar] [CrossRef]
- Winkelman, W.J.; Leonard, K.J.; Rossos, P.G. Patient-perceived usefulness of online electronic medical records: Employing grounded theory in the development of information and communication technologies for use by patients living with chronic illness. J. Am. Med. Inf. Assoc. 2005, 12, 306–314. [Google Scholar] [CrossRef]
- Tang, P.C.; Ash, J.S.; Bates, D.W.; Overhage, J.M.; Sands, D.Z. Personal health records: Definitions, benefits, and strategies for overcoming barriers to adoption. J. Am. Med. Inf. Assoc. 2006, 13, 121–126. [Google Scholar] [CrossRef]
- Dhanireddy, S.; Walker, J.; Reisch, L.; Oster, N.; Delbanco, T.; Elmore, J.G. The urban underserved: Attitudes towards gaining full access to electronic medical records. Health Expect. Int. J. Public Particip. Health Care Health Policy 2014, 17, 724–732. [Google Scholar] [CrossRef]
- Tran, B.X.; Duong, A.T.; Nguyen, L.T.; Hwang, J.; Nguyen, B.T.; Nguyen, Q.T.; Nong, V.M.; Vu, P.X.; Ohinmaa, A. Financial burden of health care for HIV/AIDS patients in Vietnam. Trop. Med. Int. Health 2013, 18, 212–218. [Google Scholar] [CrossRef]
- Tran, B.X.; Nguyen, L.T.; Nguyen, N.H.; Hoang, Q.V.; Hwang, J. Determinants of antiretroviral treatment adherence among HIV/AIDS patients: A multisite study. Glob. Health Action 2013, 6, 19570. [Google Scholar] [CrossRef][Green Version]
- Hiregoudar, V.; Bellara, R.; Goud, T.G. Proportion and Determinants of Adherence to Antiretroviral Therapy among HIV Positive People Registered Under ART Center in South India. Int. J. Prev. Med. 2019, 10, 206. [Google Scholar] [CrossRef]
- Van Tam, V.; Pharris, A.; Thorson, A.; Alfven, T.; Larsson, M. “It is not that I forget, it’s just that I don’t want other people to know”: Barriers to and strategies for adherence to antiretroviral therapy among HIV patients in Northern Vietnam. Aids Care 2011, 23, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Ceylan, E.; Koç, A.; İnkaya, A.; Ünal, S. Determination of medication adherence and related factors among people living with HIV/AIDS in a Turkish university hospital. Turk. J. Med. Sci. 2019, 49, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Fleming, M.; Do, H.P.; Nguyen, L.H.; Latkin, C.A. Quality of life improvement, social stigma and antiretroviral treatment adherence: Implications for long-term HIV/AIDS care. Aids Care 2018, 30, 1524–1531. [Google Scholar] [CrossRef]
| Characteristics | n | % |
|---|---|---|
| Sex (n = 495) | ||
| Male | 282 | 57.0 |
| Female | 213 | 43.0 |
| Marital status (n = 495) | ||
| Single | 84 | 17.0 |
| Separate/divorce/widow | 69 | 13.9 |
| Having spouse/partner | 342 | 69.1 |
| Education (n = 495) | ||
| Elementary school or under | 48 | 9.7 |
| Secondary school | 152 | 30.7 |
| High school | 169 | 34.1 |
| Above high school | 126 | 25.5 |
| Employment status (n = 495) | ||
| Unemployed | 27 | 5.5 |
| White-collar workers | 45 | 9.1 |
| Blue-collar workers/farmers | 94 | 19.0 |
| Self-employed | 34 | 6.9 |
| Others | 295 | 59.6 |
| Self-reported HIV stage (n = 487) | ||
| Asymptomatic | 465 | 95.5 |
| Symptomatic | 22 | 4.5 |
| Last time forget taking an HIV pill (n = 483) | ||
| Never | 416 | 86.1 |
| Last week | 13 | 2.7 |
| Last 1–2 week | 6 | 1.2 |
| Last 2–4 week | 3 | 0.6 |
| Last 1–3 months | 14 | 2.9 |
| Last more than 3 months | 16 | 3.3 |
| Does not remember | 15 | 3.1 |
| Uses alcohol (n = 495) | 250 | 50.5 |
| Smoked in the last 30 days (n = 495) | 161 | 32.5 |
| History of drug use (n = 495) | 115 | 23.2 |
| Current drug use (n = 495) | 4 | 0.8 |
| Using health service in the last 12 months (n = 495) | 98 | 19.8 |
| Mean | SD | |
| Age (n = 495) | 37.8 | 6.6 |
| Monthly household income (thousand VND) (n = 495) | 5361.0 | 7358.1 |
| CD4 first (n = 481) | 271.5 | 239.1 |
| CD4 last (n = 478) | 529.3 | 267.8 |
| Duration in ART (years) (n = 488) | 6.2 | 2.8 |
| Adherence score (0–100) (n = 476) | 94.0 | 10.3 |
| Self-reported health status (0–100) (n = 495) | 77.9 | 16.2 |
| Characteristics | n | % |
|---|---|---|
| Using health-related application(s) in the last 30 days (n = 495) | 36 | 7.3 |
| Function used the most (n = 36) | ||
| Smoking cessation | 1 | 2.8 |
| Physical activity | 8 | 22.2 |
| Remind medication | 27 | 75.0 |
| Day session when using apps (n = 36) | ||
| Early morning | 21 | 58.3 |
| Morning | 3 | 8.3 |
| Noon | 1 | 2.8 |
| Afternoon | 2 | 5.6 |
| Evening | 6 | 16.7 |
| Before night sleep | 3 | 8.3 |
| WTP for smartphone apps (n = 495) | 410 | 82.8 |
| Mean | SD | |
| Duration of smartphone use (month) (n = 495) | 28.7 | 21.2 |
| Time of smartphone use per day (hours) (n = 36) | 3.4 | 1.8 |
| Time of health-related application use per day (minutes) (n = 36) | 14.3 | 11.0 |
| Perceived usefulness of health-related apps (0–100) (n = 36) | 85.3 | 13.2 |
| Satisfaction with health-related apps (0–100) (n = 36) | 86.9 | 12.8 |
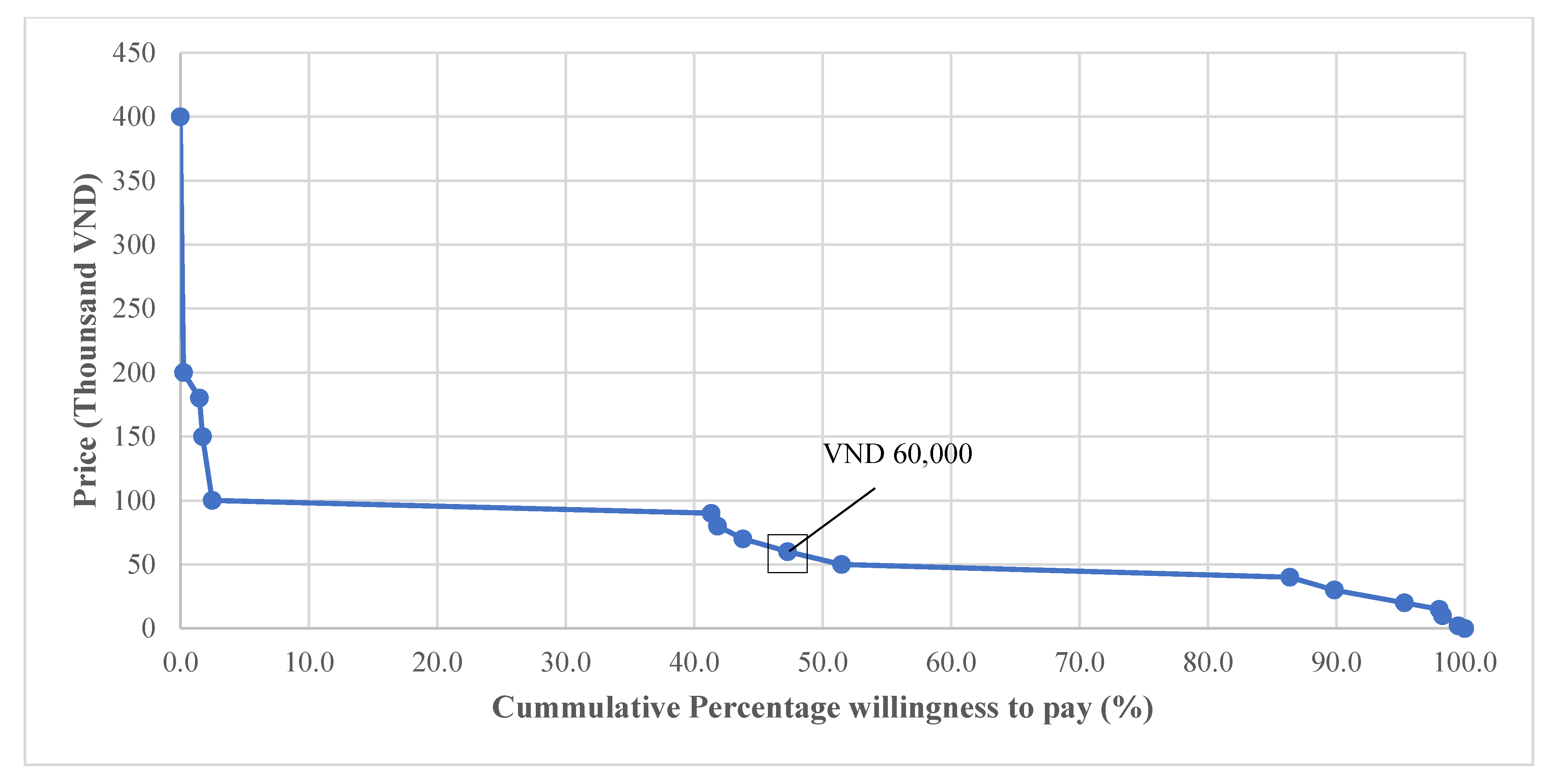
| Amount of WTP (thousand VND/month) (n = 404) | 72.1 | 36.3 |
| Characteristics | WTP for Smartphone App | Amount of WTP | p-Value | |||
|---|---|---|---|---|---|---|
| W | % | p-Value | Mean | SD | ||
| Sex | ||||||
| Male | 221 | 79.8 | 0.06 | 74.6 | 39.3 | 0.18 |
| Female | 182 | 86.3 | 68.9 | 32.0 | ||
| Marital status | ||||||
| Single | 62 | 74.7 | 0.049 | 82.6 | 51.0 | 0.10 |
| Separate/divorce/widow | 61 | 89.7 | 70.2 | 26.2 | ||
| Having spouse/partner | 280 | 83.1 | 70.1 | 33.8 | ||
| Education | ||||||
| Elementary school or less | 38 | 79.2 | 0.36 | 74.2 | 40.1 | 0.48 |
| Secondary school | 119 | 79.3 | 67.3 | 28.8 | ||
| High school | 139 | 83.2 | 73.3 | 31.1 | ||
| Above high school | 107 | 87.0 | 75.1 | 47.0 | ||
| Job | ||||||
| Unemployed | 22 | 81.5 | 0.79 | 68.6 | 30.8 | 0.90 |
| White-collar workers | 35 | 81.4 | 69.4 | 33.3 | ||
| Blue-collar Workers | 77 | 81.9 | 72.5 | 35.0 | ||
| Self-employed | 30 | 90.9 | 73.2 | 37.8 | ||
| Others | 239 | 82.1 | 72.5 | 37.5 | ||
| HIV stage | ||||||
| Asymptomatic | 379 | 82.8 | 0.91 | 72.3 | 36.5 | 0.44 |
| Symptomatic | 18 | 81.8 | 67.2 | 33.6 | ||
| Last time forgot taking pill | ||||||
| Never | 339 | 82.5 | 0.64 | 73.0 | 37.5 | 0.83 |
| Last week | 11 | 84.6 | 76.4 | 28.0 | ||
| Last 1–2 week | 6 | 100.0 | 61.7 | 19.4 | ||
| Last 2–4 week | 3 | 100.0 | 66.7 | 28.9 | ||
| Last 1–3 months | 11 | 78.6 | 72.7 | 26.1 | ||
| more than 3 months | 11 | 68.8 | 63.2 | 37.8 | ||
| Does not remember | 11 | 78.6 | - | - | ||
| Use Alcohol | 95 | 79.2 | 0.26 | 72.7 | 27.0 | 0.35 |
| Smoke last 30 days | 128 | 80.5 | 0.40 | 71.0 | 32.1 | 0.96 |
| History of drug use | 88 | 77.9 | 0.13 | 72.3 | 34.7 | 0.87 |
| Household monthly income (VND/month) | ||||||
| ≤3 million | 129 | 83.2 | 0.83 | 72.4 | 44.7 | 0.55 |
| 3 to 4 million | 50 | 78.1 | 69.2 | 26.3 | ||
| 4 to 5 million | 91 | 84.3 | 70.5 | 30.3 | ||
| 5 to 7 million | 65 | 84.4 | 79.6 | 39.1 | ||
| >7 million | 68 | 81.0 | 68.3 | 27.8 | ||
| Characteristics | WTP for Smartphone App | Natural Log of the Amount of WTP | ||
|---|---|---|---|---|
| OR | 95% CI | Β | 95% CI | |
| Socio-demographic Characteristics | ||||
| Age (years) | −0.01 ** | −0.02; 0.00 | ||
| Marital status (single-ref) | ||||
| Separate/divorced/widow | 1.28 *** | 1.09; 1.50 | ||
| Having spouse/partner | 1.18 *** | 1.03; 1.36 | ||
| Education (Elementary school or less-ref) | ||||
| Secondary school | 1.00 | 0.85; 1.19 | ||
| High school | 1.07 | 0.90; 1.26 | ||
| Above high school | 1.16 * | 0.99; 1.37 | ||
| Clinical Characteristics | ||||
| Using health services in the last 12 months (Yes vs. No -ref) | 1.03 *** | 1.01; 1.04 | −0.04 ** | −0.07; −0.01 |
| Duration of ART (years) | 0.98 ** | 0.96; 0.99 | ||
| Using alcohol (Yes vs. No-ref) | 0.94 | 0.87; 1.02 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bui, T.M.; Hoang, M.T.; Ngo, T.V.; Do, C.D.; Nghiem, S.H.; Byrnes, J.; Phung, D.T.; Nguyen, T.H.T.; Vu, G.T.; Do, H.T.; et al. Smartphone Use and Willingness to Pay for HIV Treatment-Assisted Smartphone Applications among HIV-Positive Patients in Urban Clinics of Vietnam. Int. J. Environ. Res. Public Health 2021, 18, 1467. https://doi.org/10.3390/ijerph18041467
Bui TM, Hoang MT, Ngo TV, Do CD, Nghiem SH, Byrnes J, Phung DT, Nguyen THT, Vu GT, Do HT, et al. Smartphone Use and Willingness to Pay for HIV Treatment-Assisted Smartphone Applications among HIV-Positive Patients in Urban Clinics of Vietnam. International Journal of Environmental Research and Public Health. 2021; 18(4):1467. https://doi.org/10.3390/ijerph18041467
Chicago/Turabian StyleBui, Thu Minh, Men Thi Hoang, Toan Van Ngo, Cuong Duy Do, Son Hong Nghiem, Joshua Byrnes, Dung Tri Phung, Trang Huyen Thi Nguyen, Giang Thu Vu, Hoa Thi Do, and et al. 2021. "Smartphone Use and Willingness to Pay for HIV Treatment-Assisted Smartphone Applications among HIV-Positive Patients in Urban Clinics of Vietnam" International Journal of Environmental Research and Public Health 18, no. 4: 1467. https://doi.org/10.3390/ijerph18041467
APA StyleBui, T. M., Hoang, M. T., Ngo, T. V., Do, C. D., Nghiem, S. H., Byrnes, J., Phung, D. T., Nguyen, T. H. T., Vu, G. T., Do, H. T., Latkin, C. A., Ho, R. C. M., & Ho, C. S. H. (2021). Smartphone Use and Willingness to Pay for HIV Treatment-Assisted Smartphone Applications among HIV-Positive Patients in Urban Clinics of Vietnam. International Journal of Environmental Research and Public Health, 18(4), 1467. https://doi.org/10.3390/ijerph18041467










