Endocrine Disruptors Acting on Estrogen and Androgen Pathways Cause Reproductive Disorders through Multiple Mechanisms: A Review
Abstract
1. Introduction
2. Objective and Review Questions
3. Results and Discussion
3.1. Effects of EDCs Acting on AR and/or ER
3.1.1. Chromosomal Aberrations
3.1.2. DNA Damage
3.1.3. Epigenetic Modifications
3.1.4. Methylation
3.1.5. Histone Modifications
3.1.6. Micro RNAs
3.1.7. EDCs, Obesity and Fertility
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diamanti-Kandarakis, E.; Bourguignon, J.P.; Giudice, L.C.; Hauser, R.; Prins, G.S.; Soto, A.M.; Zoeller, R.T.; Gore, A.C. Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr. Rev. 2009, 30, 293–342. [Google Scholar] [CrossRef]
- Canipari, R.; De Santis, L.; Cecconi, S. Female fertility and environmental pollution. Int. J. Environ. Res. Public Health 2020, 17, 8802. [Google Scholar] [CrossRef]
- Hotchkiss, A.K.; Rider, C.V.; Blystone, C.R.; Wilson, V.S.; Hartig, P.C.; Ankley, G.T.; Foster, P.M.; Gray, C.L.; Gray, L.E. Fifteen years after “Wingspread”—environmental endocrine disrupters and human and wildlife health: Where we are today and where we need to go. Toxicol. Sci. Off. J. Soc. Toxicol. 2008, 105, 235–259. [Google Scholar] [CrossRef] [PubMed]
- Street, M.E.; Angelini, S.; Bernasconi, S.; Burgio, E.; Cassio, A.; Catellani, C.; Cirillo, F.; Deodati, A.; Fabbrizi, E.; Fanos, V.; et al. Current knowledge on endocrine disrupting chemicals (EDCs) from animal biology to humans, from pregnancy to adulthood: Highlights from a national Italian meeting. Int. J. Mol. Sci. 2018, 19, 1647. [Google Scholar] [CrossRef] [PubMed]
- Carnevali, O.; Santangeli, S.; Forner-Piquer, I.; Basili, D.; Maradonna, F. Endocrine-disrupting chemicals in aquatic environment: What are the risks for fish gametes? Fish Physiol. Biochem. 2018, 44, 1561–1576. [Google Scholar] [CrossRef] [PubMed]
- Fucic, A.; Galea, K.S.; Duca, R.C.; El Yamani, M.; Frery, N.; Godderis, L.; Halldorsson, T.I.; Iavicoli, I.; Ndaw, S.; Ribeiro, E.; et al. Potential health risk of endocrine disruptors in construction sector and plastics industry: A new paradigm in occupational health. Int. J. Environ. Res. Public Health 2018, 15, 1229. [Google Scholar] [CrossRef]
- Docea, A.O.; Vassilopoulou, L.; Fragou, D.; Arsene, A.L.; Fenga, C.; Kovatsi, L.; Petrakis, D.; Rakitskii, V.N.; Nosyrev, A.E.; Izotov, B.N.; et al. CYP polymorphisms and pathological conditions related to chronic exposure to organochlorine pesticides. Toxicol. Rep. 2017, 4, 335–341. [Google Scholar] [CrossRef]
- Rowe, P.J.; Comhaire, F.H.; Hargreave, T.B.; Mahmoud, A.M.A. WHO Manual for the Standardized Investigation, Diagnosis and Management of the Infertile Male; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Salonia, A.; Bettocchi, C.; Carvalho, J.; Corona, G.; Jones, T.H.; Kadioglu, A.; Martinez-Salamanca, J.I.; Minhas, S.; Serefoglu, E.C.; Verze, P. Members of the sexual and reproductive health guidelines panel. In EAU Guidelines on Sexual and Reproductive Health. Edn, Proceedings of the EAU Annual Congress Amsterdam 2020, Amsterdam, The Netherlands, 20–24 March 2020; EAU Guidelines Office: Arnhem, The Netherlands, 2020; ISBN 978-94-92671-07-3. [Google Scholar]
- WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed.; WHO Press, World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Saradha, B.; Mathur, P.P. Effect of environmental contaminants on male reproduction. Environ. Toxicol. Pharmacol. 2006, 21, 34–41. [Google Scholar] [CrossRef]
- Kalliora, C.; Mamoulakis, C.; Vasilopoulos, E.; Stamatiades, G.A.; Kalafati, L.; Barouni, R.; Karakousi, T.; Abdollahi, M.; Tsatsakis, A. Association of pesticide exposure with human congenital abnormalities. Toxicol. Appl. Pharmacol. 2018, 346, 58–75. [Google Scholar] [CrossRef]
- Petrakis, D.; Vassilopoulou, L.; Mamoulakis, C.; Psycharakis, C.; Anifantaki, A.; Sifakis, S.; Docea, A.O.; Tsiaoussis, J.; Makrigiannakis, A.; Tsatsakis, A.M. Endocrine disruptors leading to obesity and related diseases. Int. J. Environ. Res. Public Health 2017, 14, 1282. [Google Scholar] [CrossRef]
- Mamoulakis, C.; Antypas, S.; Stamatiadou, A.; Demetriadis, D.; Kanakas, N.; Loutradis, D.; Miyagawa, I.; Yannakis, D.; Kaponis, A.; Tzonou, A.; et al. Cryptorchidism: Seasonal variations in Greece do not support the theory of light. Andrologia 2002, 34, 194–203. [Google Scholar] [CrossRef]
- Mamoulakis, C.; Avgenakis, G.; Gkatzoudi, C.; Duyker, G.; Zisis, I.E.; Heretis, I.; Antypas, S.; Sofikitis, N.; Spandidos, D.A.; Tsatsakis, A.M.; et al. Seasonal trends in the prevalence of hypospadias: Aetiological implications. Exp. Ther. Med. 2017, 13, 2960–2968. [Google Scholar] [CrossRef][Green Version]
- Karwacka, A.; Zamkowska, D.; Radwan, M.; Jurewicz, J. Exposure to modern, widespread environmental endocrine disrupting chemicals and their effect on the reproductive potential of women: An overview of current epidemiological evidence. Hum. Fertil. 2019, 22, 2–25. [Google Scholar] [CrossRef]
- Raghavan, R.; Romano, M.E.; Karagas, M.R.; Penna, F.J. Pharmacologic and environmental endocrine disruptors in the pathogenesis of hypospadias: A review. Curr. Environ. Health Rep. 2018, 5, 499–511. [Google Scholar] [CrossRef]
- Tsiaoussis, J.; Hatzidaki, E.; Docea, A.O.; Nikolouzakis, T.K.; Petrakis, D.; Burykina, T.; Mamoulakis, C.; Makrigiannakis, A.; Tsatsakis, A. Molecular and clinical aspects of embryotoxicity induced by acetylcholinesterase inhibitors. Toxicology 2018, 409, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Mollier, J.; Brocklesby, R.W.K.; Caves, C.; Jayasena, C.N.; Minhas, S. Endocrine-disrupting chemicals and male reproductive health. Reprod. Med. Biol. 2020, 19, 243–253. [Google Scholar] [CrossRef]
- Hipwell, A.E.; Kahn, L.G.; Factor-Litvak, P.; Porucznik, C.A.; Siegel, E.L.; Fichorova, R.N.; Hamman, R.F.; Klein-Fedyshin, M.; Harley, K.G. Program collaborators for environmental influences on child health, O. exposure to non-persistent chemicals in consumer products and fecundability: A systematic review. Hum. Reprod. Update 2019, 25, 51–71. [Google Scholar] [CrossRef]
- Katsikantami, I.; Sifakis, S.; Tzatzarakis, M.N.; Vakonaki, E.; Kalantzi, O.I.; Tsatsakis, A.M.; Rizos, A.K. A global assessment of phthalates burden and related links to health effects. Environ. Int. 2016, 97, 212–236. [Google Scholar] [CrossRef]
- Mrema, E.J.; Rubino, F.M.; Brambilla, G.; Moretto, A.; Tsatsakis, A.M.; Colosio, C. Persistent organochlorinated pesticides and mechanisms of their toxicity. Toxicology 2013, 307, 74–88. [Google Scholar] [CrossRef] [PubMed]
- Sifakis, S.; Androutsopoulos, V.P.; Tsatsakis, A.M.; Spandidos, D.A. Human exposure to endocrine disrupting chemicals: Effects on the male and female reproductive systems. Environ. Toxicol. Pharmacol. 2017, 51, 56–70. [Google Scholar] [CrossRef] [PubMed]
- Jeng, H.A. Exposure to endocrine disrupting chemicals and male reproductive health. Front. Public Health 2014, 2, 55. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Health Statistics 2010; WHO Press, World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Vasilopoulos, E.; Fragkiadaki, P.; Kalliora, C.; Fragou, D.; Docea, A.O.; Vakonaki, E.; Tsoukalas, D.; Calina, D.; Buga, A.M.; Georgiadis, G.; et al. The association of female and male infertility with telomere length (Review). Int. J. Mol. Med. 2019, 44, 375–389. [Google Scholar] [CrossRef]
- Joffe, M. Infertility and environmental pollutants. Br. Med. Bull. 2003, 68, 47–70. [Google Scholar] [CrossRef] [PubMed]
- Tsatsakis, A.; Docea, A.O.; Constantin, C.; Calina, D.; Zlatian, O.; Nikolouzakis, T.K.; Stivaktakis, P.D.; Kalogeraki, A.; Liesivuori, J.; Tzanakakis, G.; et al. Genotoxic, cytotoxic, and cytopathological effects in rats exposed for 18 months to a mixture of 13 chemicals in doses below NOAEL levels. Toxicol. Lett. 2019, 316, 154–170. [Google Scholar] [CrossRef] [PubMed]
- Gonsioroski, A.; Mourikes, V.E.; Flaws, J.A. Endocrine disruptors in water and their effects on the reproductive system. Int. J. Mol. Sci. 2020, 21, 1929. [Google Scholar] [CrossRef] [PubMed]
- Di Nisio, A.; Foresta, C. Water and soil pollution as determinant of water and food quality/contamination and its impact on male fertility. Reprod. Biol. Endocrinol. RbE 2019, 17, 4. [Google Scholar] [CrossRef] [PubMed]
- Sharifi-Rad, M.; Anil Kumar, N.V.; Zucca, P.; Varoni, E.M.; Dini, L.; Panzarini, E.; Rajkovic, J.; Tsouh Fokou, P.V.; Azzini, E.; Peluso, I.; et al. Lifestyle, oxidative stress, and antioxidants: Back and forth in the pathophysiology of chronic diseases. Front. Physiol. 2020, 11, 694. [Google Scholar] [CrossRef] [PubMed]
- Tzatzarakis, M.N.; Karzi, V.; Vakonaki, E.; Goumenou, M.; Kavvalakis, M.; Stivaktakis, P.; Tsitsimpikou, C.; Tsakiris, I.; Rizos, A.K.; Tsatsakis, A.M. Bisphenol A in soft drinks and canned foods and data evaluation. Food Addit. Contam. Part B Surveill 2017, 10, 85–90. [Google Scholar] [CrossRef]
- Raherison, C.; Baldi, I.; Pouquet, M.; Berteaud, E.; Moesch, C.; Bouvier, G.; Canal-Raffin, M. Pesticides exposure by air in vineyard rural area and respiratory health in children: A pilot study. Environ. Res. 2019, 169, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, K.; Feary, J. Occupational exposure to pesticides: Time to nip it in the bud? Thorax 2017, 72, 489–490. [Google Scholar] [CrossRef][Green Version]
- Carpenter, D.O. Polychlorinated biphenyls (PCBs): Routes of exposure and effects on human health. Rev. Environ. Health 2006, 21, 1–23. [Google Scholar] [CrossRef]
- Năstăsescu, V.; Mititelu, M.; Goumenou, M.; Docea, A.O.; Renieri, E.; Udeanu, D.I.; Oprea, E.; Arsene, A.L.; Dinu-Pîrvu, C.E.; Ghica, M. Heavy metal and pesticide levels in dairy products: Evaluation of human health risk. Food Chem. Toxicol. 2020, 146, 111844. [Google Scholar] [CrossRef]
- Martenies, S.E.; Perry, M.J. Environmental and occupational pesticide exposure and human sperm parameters: A systematic review. Toxicology 2013, 307, 66–73. [Google Scholar] [CrossRef]
- Vested, A.; Giwercman, A.; Bonde, J.P.; Toft, G. Persistent organic pollutants and male reproductive health. Asian J. Androl. 2014, 16, 71–80. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, L.; Robertson, K.M.; Jones, M.E.; Simpson, E.R. Estrogen and spermatogenesis. Endocr. Rev. 2001, 22, 289–318. [Google Scholar] [CrossRef] [PubMed]
- Kula, K.; Walczak-Jedrzejowska, R.; Slowikowska-Hilczer, J.; Oszukowska, E. Estradiol enhances the stimulatory effect of FSH on testicular maturation and contributes to precocious initiation of spermatogenesis. Mol. Cell. Endocrinol. 2001, 178, 89–97. [Google Scholar] [CrossRef]
- Carreau, S.; Lambard, S.; Delalande, C.; Denis-Galeraud, I.; Bilinska, B.; Bourguiba, S. Aromatase expression and role of estrogens in male gonad: A review. Reprod. Biol. Endocrinol. RbE 2003, 1, 35. [Google Scholar] [CrossRef]
- Schulster, M.; Bernie, A.M.; Ramasamy, R. The role of estradiol in male reproductive function. Asian J. Androl. 2016, 18, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Bakker, J.; Baum, M.J. Role for estradiol in female-typical brain and behavioral sexual differentiation. Front. Neuroendocrinol. 2008, 29, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Kuiper, G.G.; Lemmen, J.G.; Carlsson, B.; Corton, J.C.; Safe, S.H.; van der Saag, P.T.; van der Burg, B.; Gustafsson, J.A. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology 1998, 139, 4252–4263. [Google Scholar] [CrossRef]
- Fang, H.; Tong, W.; Branham, W.S.; Moland, C.L.; Dial, S.L.; Hong, H.; Xie, Q.; Perkins, R.; Owens, W.; Sheehan, D.M. Study of 202 natural, synthetic, and environmental chemicals for binding to the androgen receptor. Chem. Res. Toxicol. 2003, 16, 1338–1358. [Google Scholar] [CrossRef]
- Kojima, H.; Katsura, E.; Takeuchi, S.; Niiyama, K.; Kobayashi, K. Screening for estrogen and androgen receptor activities in 200 pesticides by in vitro reporter gene assays using Chinese hamster ovary cells. Environ. Health Perspect. 2004, 112, 524–531. [Google Scholar] [CrossRef]
- Lemaire, G.; Mnif, W.; Mauvais, P.; Balaguer, P.; Rahmani, R. Activation of alpha- and beta-estrogen receptors by persistent pesticides in reporter cell lines. Life Sci. 2006, 79, 1160–1169. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, S.; Shiraishi, F.; Kitamura, S.; Kuroki, H.; Jin, K.; Kojima, H. Characterization of steroid hormone receptor activities in 100 hydroxylated polychlorinated biphenyls, including congeners identified in humans. Toxicology 2011, 289, 112–121. [Google Scholar] [CrossRef]
- Svobodová, K.; Placková, M.; Novotná, V.; Cajthaml, T. Estrogenic and androgenic activity of PCBs, their chlorinated metabolites and other endocrine disruptors estimated with two in vitro yeast assays. Sci. Total Environ. 2009, 407, 5921–5925. [Google Scholar] [CrossRef] [PubMed]
- Hamers, T.; Kamstra, J.H.; Sonneveld, E.; Murk, A.J.; Kester, M.H.; Andersson, P.L.; Legler, J.; Brouwer, A. In vitro profiling of the endocrine-disrupting potency of brominated flame retardants. Toxicol. Sci. 2006, 92, 157–173. [Google Scholar] [CrossRef] [PubMed]
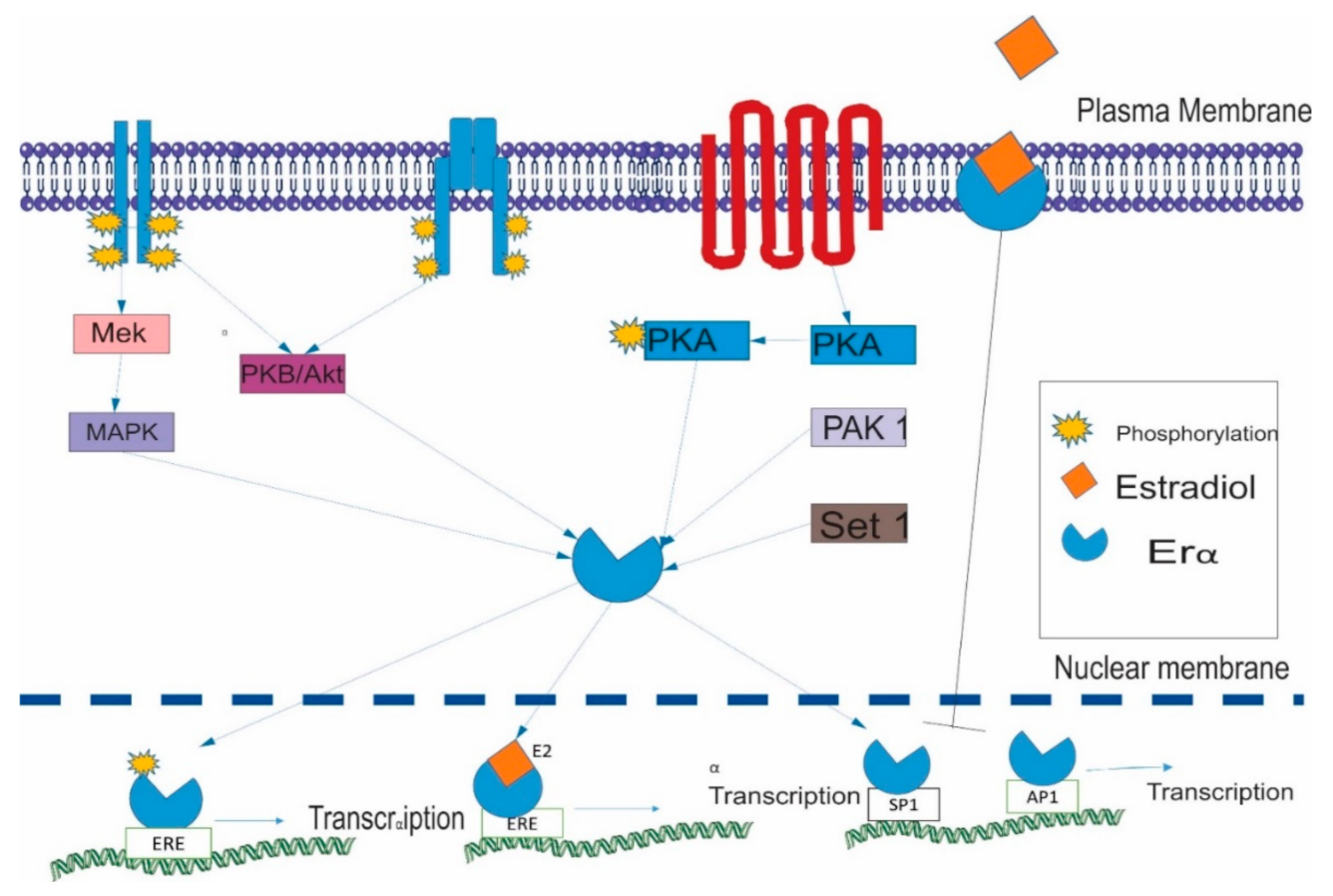
- Marino, M.; Galluzzo, P.; Ascenzi, P. Estrogen signaling multiple pathways to impact gene transcription. Curr. Genom. 2006, 7, 497–508. [Google Scholar] [CrossRef]
- Revankar, C.M.; Cimino, D.F.; Sklar, L.A.; Arterburn, J.B.; Prossnitz, E.R. A transmembrane intracellular estrogen receptor mediates rapid cell signaling. Science 2005, 307, 1625–1630. [Google Scholar] [CrossRef]
- Likhite, V.S.; Stossi, F.; Kim, K.; Katzenellenbogen, B.S.; Katzenellenbogen, J.A. Kinase-specific phosphorylation of the estrogen receptor changes receptor interactions with ligand, deoxyribonucleic acid, and coregulators associated with alterations in estrogen and tamoxifen activity. Mol. Endocrinol. 2006, 20, 3120–3132. [Google Scholar] [CrossRef]
- Hamilton, K.J.; Arao, Y.; Korach, K.S. Estrogen hormone physiology: Reproductive findings from estrogen receptor mutant mice. Reprod. Biol. 2014, 14, 3–8. [Google Scholar] [CrossRef]
- Barone, I.; Brusco, L.; Fuqua, S.A. Estrogen receptor mutations and changes in downstream gene expression and signaling. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2010, 16, 2702–2708. [Google Scholar] [CrossRef]
- Roy, A.K.; Tyagi, R.K.; Song, C.S.; Lavrovsky, Y.; Ahn, S.C.; Oh, T.S.; Chatterjee, B. Androgen receptor: Structural domains and functional dynamics after ligand-receptor interaction. Ann. N. Y. Acad. Sci. 2001, 949, 44–57. [Google Scholar] [CrossRef]
- Liao, R.S.; Ma, S.; Miao, L.; Li, R.; Yin, Y.; Raj, G.V. Androgen receptor-mediated non-genomic regulation of prostate cancer cell proliferation. Transl. Urol. 2013, 2, 187–196. [Google Scholar] [CrossRef]
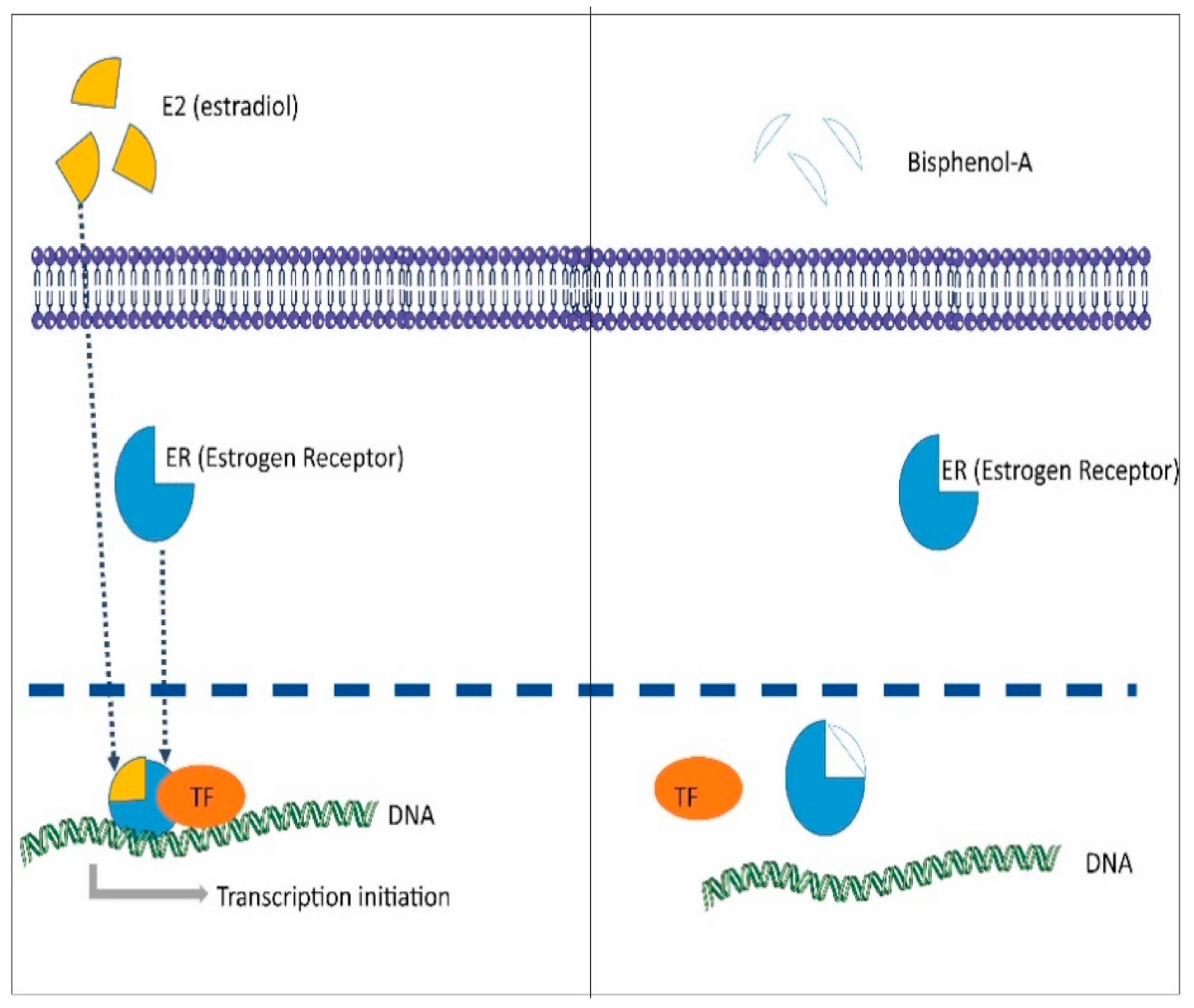
- Rubin, B.S. Bisphenol A: An endocrine disruptor with widespread exposure and multiple effects. J. Steroid Biochem. Mol. Biol. 2011, 127, 27–34. [Google Scholar] [CrossRef]
- Crain, D.A.; Eriksen, M.; Iguchi, T.; Jobling, S.; Laufer, H.; LeBlanc, G.A.; Guillette, L.J., Jr. An ecological assessment of bisphenol-A: Evidence from comparative biology. Reprod. Toxicol. 2007, 24, 225–239. [Google Scholar] [CrossRef]
- Ikezuki, Y.; Tsutsumi, O.; Takai, Y.; Kamei, Y.; Taketani, Y. Determination of bisphenol a concentrations in human biological fluids reveals significant early prenatal exposure. Hum. Reprod. 2002, 17, 2839–2841. [Google Scholar] [CrossRef]
- Jeseta, M.; Crha, T.; Zakova, J.; Ventruba, P. Bisphenols in the pathology of reproduction. Ceska Gynekol. 2019, 84, 161–165. [Google Scholar] [PubMed]
- Pivonello, C.; Muscogiuri, G.; Nardone, A.; Garifalos, F.; Provvisiero, D.P.; Verde, N.; de Angelis, C.; Conforti, A.; Piscopo, M.; Auriemma, R.S.; et al. Bisphenol A: An emerging threat to female fertility. Reprod. Biol. Endocrinol. RbE 2020, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Adegoke, E.O.; Rahman, M.S.; Pang, M.G. Bisphenols threaten male reproductive health via testicular cells. Front. Endocrinol. 2020, 11, 624. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, Z.; Liu, F. Chronic exposure of BPA impairs male germ cell proliferation and induces lower sperm quality in male mice. Chemosphere 2021, 262, 127880. [Google Scholar] [CrossRef]
- Castellini, C.; Totaro, M.; Parisi, A.; D’Andrea, S.; Lucente, L.; Cordeschi, G.; Francavilla, S.; Francavilla, F.; Barbonetti, A. Bisphenol A and male fertility: Myths and realities. Front. Endocrinol. 2020, 11, 353. [Google Scholar] [CrossRef]
- Chianese, R.; Troisi, J.; Richards, S.; Scafuro, M.; Fasano, S.; Guida, M.; Pierantoni, R.; Meccariello, R. Bisphenol A in reproduction: Epigenetic effects. Curr. Med. Chem. 2018, 25, 748–770. [Google Scholar] [CrossRef]
- Machtinger, R.; Orvieto, R. Bisphenol A, oocyte maturation, implantation, and IVF outcome: Review of animal and human data. Reprod. Biomed. Online 2014, 29, 404–410. [Google Scholar] [CrossRef]
- Dobrzynska, M.M.; Gajowik, A.; Radzikowska, J.; Tyrkiel, E.J.; Jankowska-Steifer, E.A. Male-mediated F1 effects in mice exposed to bisphenol A, either alone or in combination with X-irradiation. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2015, 789–790, 36–45. [Google Scholar] [CrossRef]
- Bisphenol, A. Action Plan Summary. Available online: https://www.epa.gov/sites/production/files/2015-09/documents/bpa_action_plan.pdf (accessed on 11 October 2020).
- Matsushima, A.; Kakuta, Y.; Teramoto, T.; Koshiba, T.; Liu, X.; Okada, H.; Tokunaga, T.; Kawabata, S.; Kimura, M.; Shimohigashi, Y. Structural evidence for endocrine disruptor bisphenol A binding to human nuclear receptor ERR gamma. J. Biochem. 2007, 142, 517–524. [Google Scholar] [CrossRef]
- Montes-Grajales, D.; Olivero-Verbel, J. Computer-aided identification of novel protein targets of bisphenol A. Toxicol. Lett. 2013, 222, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Bouskine, A.; Nebout, M.; Brucker-Davis, F.; Benahmed, M.; Fenichel, P. Low doses of bisphenol A promote human seminoma cell proliferation by activating PKA and PKG via a membrane G-protein-coupled estrogen receptor. Environ. Health Perspect. 2009, 117, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, J.; Li, Q.; Zhang, T.; Deng, Z.; Lian, J.; Jia, D.; Li, R.; Zheng, T.; Ding, X.; et al. Low concentration of BPA induces mice spermatocytes apoptosis via GPR30. Oncotarget 2017, 8, 49005–49015. [Google Scholar] [CrossRef]
- Rehan, M.; Ahmad, E.; Sheikh, I.A.; Abuzenadah, A.M.; Damanhouri, G.A.; Bajouh, O.S.; AlBasri, S.F.; Assiri, M.M.; Beg, M.A. Androgen and progesterone receptors are targets for bisphenol A (BPA), 4-methyl-2,4-bis-(P-hydroxyphenyl)pent-1-ene--A potent metabolite of BPA, and 4-tert-octylphenol: A computational insight. PLoS ONE 2015, 10, e0138438. [Google Scholar] [CrossRef] [PubMed]
- Asencio-Hernandez, J.; Kieffer, B.; Delsuc, M.A. NMR WaterLOGSY reveals weak binding of bisphenol A with amyloid fibers of a conserved 11 residue peptide from androgen receptor. PLoS ONE 2016, 11, e0161948. [Google Scholar] [CrossRef] [PubMed]
- UN. Stockholm Convention on Persistent Organic Pollutants. Available online: http://www.pops.int/TheConvention/Overview/tabid/3351/Default.aspx (accessed on 11 October 2020).
- WHO. The Use of DDT in Malaria Vector Control. WHO Position Statement; WHO Press, World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Thomas, P.; Dong, J. Binding and activation of the seven-transmembrane estrogen receptor GPR30 by environmental estrogens: A potential novel mechanism of endocrine disruption. J. Steroid Biochem. Mol. Biol. 2006, 102, 175–179. [Google Scholar] [CrossRef]
- Zhuang, S.; Zhang, J.; Wen, Y.; Zhang, C.; Liu, W. Distinct mechanisms of endocrine disruption of DDT-related pesticides toward estrogen receptor alpha and estrogen-related receptor gamma. Environ. Toxicol. Chem. 2012, 31, 2597–2605. [Google Scholar] [CrossRef]
- Campagna, M.; Satta, G.; Fadda, D.; Pili, S.; Cocco, P. Male fertility following occupational exposure to dichlorodiphenyltrichloroethane (DDT). Environ. Int. 2015, 77, 42–47. [Google Scholar] [CrossRef]
- Jurewicz, J.; Hanke, W.; Radwan, M.; Bonde, J.P. Environmental factors and semen quality. Int. J. Occup. Med. Environ. Health 2009, 22, 305–329. [Google Scholar] [CrossRef] [PubMed]
- Messaros, B.M.; Rossano, M.G.; Liu, G.; Diamond, M.P.; Friderici, K.; Nummy-Jernigan, K.; Daly, D.; Puscheck, E.; Paneth, N.; Wirth, J.J. Negative effects of serum p,p′-DDE on sperm parameters and modification by genetic polymorphisms. Environ. Res. 2009, 109, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Hu, J. Effects of p,p′-DDE exposure on gonadal development and gene expression in Japanese medaka (Oryzias latipes). J. Environ. Sci. 2008, 20, 347–352. [Google Scholar] [CrossRef]
- Mahugija, J.A.M.; Kayombo, A.; Peter, R. Pesticide residues in raw and processed maize grains and flour from selected areas in Dar es Salaam and Ruvuma, Tanzania. Chemosphere 2017, 185, 137–144. [Google Scholar] [CrossRef]
- Watanabe, T.; Fujihara, H.; Hirose, J.; Suenaga, H.; Kimura, N. Use of biphenyl/polychlorinated biphenyl-degrading bacteria for the production of useful aromatic compounds. Sustain. Hum. 2016, 12, 5. [Google Scholar]
- Fiedler, H. 12. Polychlorinated Biphenyls (PCBs): Uses and Environmental Releases. Available online: http://www.chem.unep.ch/pops/POPs_Inc/proceedings/bangkok/FIEDLER1.html (accessed on 11 October 2020).
- Li, X.; Ye, L.; Wang, X.; Wang, X.; Liu, H.; Qian, X.; Zhu, Y.; Yu, H. Molecular docking, molecular dynamics simulation, and structure-based 3D-QSAR studies on estrogenic activity of hydroxylated polychlorinated biphenyls. Sci. Total Environ. 2012, 441, 230–238. [Google Scholar] [CrossRef]
- Meeker, J.D.; Hauser, R. Exposure to polychlorinated biphenyls (PCBs) and male reproduction. Syst. Biol. Reprod. Med. 2010, 56, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, G.; Venkataraman, P.; Arunkumar, A.; Vignesh, R.C.; Aruldhas, M.M.; Arunakaran, J. Ameliorative effect of vitamins (alpha-tocopherol and ascorbic acid) on PCB (Aroclor 1254) induced oxidative stress in rat epididymal sperm. Reprod. Toxicol. 2007, 23, 239–245. [Google Scholar] [CrossRef]
- Cok, I.; Durmaz, T.C.; Durmaz, E.; Satiroglu, M.H.; Kabukcu, C. Determination of organochlorine pesticide and polychlorinated biphenyl levels in adipose tissue of infertile men. Environ. Monit. Assess. 2010, 162, 301–309. [Google Scholar] [CrossRef]
- McGlynn, K.A.; Guo, X.; Graubard, B.I.; Brock, J.W.; Klebanoff, M.A.; Longnecker, M.P. Maternal pregnancy levels of polychlorinated biphenyls and risk of hypospadias and cryptorchidism in male offspring. Environ. Health Perspect. 2009, 117, 1472–1476. [Google Scholar] [CrossRef] [PubMed]
- Donat-Vargas, C.; Akesson, A.; Berglund, M.; Glynn, A.; Wolk, A.; Kippler, M. Dietary exposure to polychlorinated biphenyls and risk of breast, endometrial and ovarian cancer in a prospective cohort. Br. J. Cancer 2016, 115, 1113–1121. [Google Scholar] [CrossRef]
- Cohn, B.A.; Cirillo, P.M.; Sholtz, R.I.; Ferrara, A.; Park, J.S.; Schwingl, P.J. Polychlorinated biphenyl (PCB) exposure in mothers and time to pregnancy in daughters. Reprod. Toxicol. 2011, 31, 290–296. [Google Scholar] [CrossRef]
- Engel, A.; Buhrke, T.; Imber, F.; Jessel, S.; Seidel, A.; Volkel, W.; Lampen, A. Agonistic and antagonistic effects of phthalates and their urinary metabolites on the steroid hormone receptors ERalpha, ERbeta, and AR. Toxicol. Lett. 2017, 277, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Sarath Josh, M.K.; Pradeep, S.; Vijayalekshmy Amma, K.S.; Sudha Devi, R.; Balachandran, S.; Sreejith, M.N.; Benjamin, S. Human ketosteroid receptors interact with hazardous phthalate plasticizers and their metabolites: An in silico study. J. Appl. Toxicol. JAT 2016, 36, 836–843. [Google Scholar] [CrossRef]
- Wang, S.W.; Wang, S.S.; Wu, D.C.; Lin, Y.C.; Ku, C.C.; Wu, C.C.; Chai, C.Y.; Lee, J.N.; Tsai, E.M.; Lin, C.L.; et al. Androgen receptor-mediated apoptosis in bovine testicular induced pluripotent stem cells in response to phthalate esters. Cell Death Dis. 2013, 4, e907. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Chen, X.; Hu, G.; Wang, S.; Xu, R.; Zhu, Q.; Li, X.; Wang, M.; Lian, Q.Q.; Ge, R.S. Comparison of the effects of dibutyl and monobutyl phthalates on the steroidogenesis of rat immature leydig cells. Biomed Res. Int. 2016, 2016, 1376526. [Google Scholar] [CrossRef] [PubMed]
- Sekaran, S.; Jagadeesan, A. In utero exposure to phthalate downregulates critical genes in Leydig cells of F1 male progeny. J. Cell. Biochem. 2015, 116, 1466–1477. [Google Scholar] [CrossRef]
- Zhou, C.; Gao, L.; Flaws, J.A. Prenatal exposure to an environmentally relevant phthalate mixture disrupts reproduction in F1 female mice. Toxicol. Appl. Pharmacol. 2017, 318, 49–57. [Google Scholar] [CrossRef]
- Metzler, M.; Pfeiffer, E.; Schuler, M.; Rosenberg, B. Effects of estrogens on microtubule assembly: Significance for aneuploidy. In Hormonal Carcinogenesis II; Li, J.J., Li, S.A., Gustafsson, J.Å., Nandi, S., Sekely, L.I., Eds.; Springer: New York, NY, USA, 1996. [Google Scholar]
- Hodes-Wertz, B.; Grifo, J.; Ghadir, S.; Kaplan, B.; Laskin, C.A.; Glassner, M.; Munne, S. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil. Steril. 2012, 98, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.S.; Gao, H.; Zhao, Y.; Ma, S. Aneuploidy and DNA fragmentation in morphologically abnormal sperm. Int. J. Androl. 2010, 33, e163–e179. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Steinmetz, G.; Montillet, G.; Perrard, M.H.; Loundou, A.; Durand, P.; Guichaoua, M.R.; Prat, O. Exposure to low-dose bisphenol A impairs meiosis in the rat seminiferous tubule culture model: A physiotoxicogenomic approach. PLoS ONE 2014, 9, e106245. [Google Scholar] [CrossRef]
- Hunt, P.A.; Koehler, K.E.; Susiarjo, M.; Hodges, C.A.; Ilagan, A.; Voigt, R.C.; Thomas, S.; Thomas, B.F.; Hassold, T.J. Bisphenol a exposure causes meiotic aneuploidy in the female mouse. Curr. Biol. 2003, 13, 546–553. [Google Scholar] [CrossRef]
- Allard, P.; Colaiacovo, M.P. Bisphenol A impairs the double-strand break repair machinery in the germline and causes chromosome abnormalities. Proc. Natl. Acad. Sci. USA 2010, 107, 20405–20410. [Google Scholar] [CrossRef]
- Aghajanpour-Mir, S.M.; Zabihi, E.; Akhavan-Niaki, H.; Keyhani, E.; Bagherizadeh, I.; Biglari, S.; Behjati, F. The genotoxic and cytotoxic effects of bisphenol-A (BPA) in MCF-7 cell line and amniocytes. Int. J. Mol. Cell. Med. 2016, 5, 19–29. [Google Scholar]
- McAuliffe, M.E.; Williams, P.L.; Korrick, S.A.; Altshul, L.M.; Perry, M.J. Environmental exposure to polychlorinated biphenyls and p,p’-DDE and sperm sex-chromosome disomy. Environ. Health Perspect. 2012, 120, 535–540. [Google Scholar] [CrossRef]
- Perry, M.J.; Young, H.A.; Grandjean, P.; Halling, J.; Petersen, M.S.; Martenies, S.E.; Karimi, P.; Weihe, P. sperm aneuploidy in faroese men with lifetime exposure to dichlorodiphenyldichloroethylene (p,p-DDE) and polychlorinated biphenyl (PCB) pollutants. Environ. Health Perspect. 2016, 124, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Governini, L.; Guerranti, C.; De Leo, V.; Boschi, L.; Luddi, A.; Gori, M.; Orvieto, R.; Piomboni, P. Chromosomal aneuploidies and DNA fragmentation of human spermatozoa from patients exposed to perfluorinated compounds. Andrologia 2015, 47, 1012–1019. [Google Scholar] [CrossRef]
- Aitken, R.J.; De Iuliis, G.N. Origins and consequences of DNA damage in male germ cells. Reprod. Biomed. Online 2007, 14, 727–733. [Google Scholar] [CrossRef]
- Tunc, O.; Tremellen, K. Oxidative DNA damage impairs global sperm DNA methylation in infertile men. J. Assist. Reprod. Genet. 2009, 26, 537–544. [Google Scholar] [CrossRef]
- Garcia-Rodriguez, A.; Gosalvez, J.; Agarwal, A.; Roy, R.; Johnston, S. DNA damage and repair in human reproductive cells. Int. J. Mol. Sci. 2018, 20, 31. [Google Scholar] [CrossRef]
- Sikka, S.C.; Wang, R. Endocrine disruptors and estrogenic effects on male reproductive axis. Asian J. Androl. 2008, 10, 134–145. [Google Scholar] [CrossRef]
- Xin, F.; Jiang, L.; Liu, X.; Geng, C.; Wang, W.; Zhong, L.; Yang, G.; Chen, M. Bisphenol A induces oxidative stress-associated DNA damage in INS-1 cells. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2014, 769, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Ayres, S.; Abplanalp, W.; Liu, J.H.; Subbiah, M.T. Mechanisms involved in the protective effect of estradiol-17beta on lipid peroxidation and DNA damage. Am. J. Physiol. 1998, 274, E1002–E1008. [Google Scholar] [CrossRef] [PubMed]
- Weinhold, B. Epigenetics: The science of change. Environ. Health Perspect. 2006, 114, A160–A167. [Google Scholar] [CrossRef]
- Shi, Y.; Qi, W.; Xu, Q.; Wang, Z.; Cao, X.; Zhou, L.; Ye, L. The role of epigenetics in the reproductive toxicity of environmental endocrine disruptors. Environ. Mol. Mutagen. 2020. [Google Scholar] [CrossRef]
- Anway, M.D.; Cupp, A.S.; Uzumcu, M.; Skinner, M.K. Epigenetic transgenerational actions of endocrine disruptors and male fertility. Science 2005, 308, 1466–1469. [Google Scholar] [CrossRef]
- Anway, M.D.; Skinner, M.K. Epigenetic transgenerational actions of endocrine disruptors. Endocrinology 2006, 147, S43–S49. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, M. Expression of various genes is controlled by DNA methylation during mammalian development. J. Cell. Biochem. 2003, 88, 899–910. [Google Scholar] [CrossRef]
- Dumasia, K.; Kumar, A.; Deshpande, S.; Balasinor, N.H. Estrogen signaling, through estrogen receptor beta, regulates DNA methylation and its machinery in male germ line in adult rats. Epigenetics 2017, 12, 476–483. [Google Scholar] [CrossRef][Green Version]
- Xiong, G.; Lin, T.; Wei, G. MP70-16 the mechanism of environmental endocrine disruptors (dehp) induces epigenetic transgenerational inheritance of cryptorchidism. J. Urol. 2016, 195, e912–e913. [Google Scholar] [CrossRef]
- Kamstra, J.H.; Sales, L.B.; Alestrom, P.; Legler, J. Differential DNA methylation at conserved non-genic elements and evidence for transgenerational inheritance following developmental exposure to mono(2-ethylhexyl) phthalate and 5-azacytidine in zebrafish. Epigenetics Chromatin 2017, 10, 20. [Google Scholar] [CrossRef]
- Cui, X.; Jing, X.; Wu, X.; Yan, M.; Li, Q.; Shen, Y.; Wang, Z. DNA methylation in spermatogenesis and male infertility. Exp. Ther. Med. 2016, 12, 1973–1979. [Google Scholar] [CrossRef] [PubMed]
- Laing, L.V.; Viana, J.; Dempster, E.L.; Trznadel, M.; Trunkfield, L.A.; Uren Webster, T.M.; van Aerle, R.; Paull, G.C.; Wilson, R.J.; Mill, J.; et al. Bisphenol A causes reproductive toxicity, decreases dnmt1 transcription, and reduces global DNA methylation in breeding zebrafish (Danio rerio). Epigenetics 2016, 11, 526–538. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.; Zhang, Y.; Liu, Y.; Zhang, T.; Wang, Z. Enhanced GSH synthesis by bisphenol A exposure promoted DNA methylation process in the testes of adult rare minnow Gobiocypris rarus. Aquat. Toxicol. 2016, 178, 99–105. [Google Scholar] [CrossRef]
- Yin, L.; Dai, Y.; Jiang, X.; Liu, Y.; Chen, H.; Han, F.; Cao, J.; Liu, J. Role of DNA methylation in bisphenol A exposed mouse spermatocyte. Environ. Toxicol. Pharmacol. 2016, 48, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Faulk, C.; Kim, J.H.; Jones, T.R.; McEachin, R.C.; Nahar, M.S.; Dolinoy, D.C.; Sartor, M.A. Bisphenol A-associated alterations in genome-wide DNA methylation and gene expression patterns reveal sequence-dependent and non-monotonic effects in human fetal liver. Environ. Epigenetics 2015, 1. [Google Scholar] [CrossRef]
- Nahar, M.S.; Liao, C.; Kannan, K.; Harris, C.; Dolinoy, D.C. In utero bisphenol A concentration, metabolism, and global DNA methylation across matched placenta, kidney, and liver in the human fetus. Chemosphere 2015, 124, 54–60. [Google Scholar] [CrossRef]
- Faulk, C.; Kim, J.H.; Anderson, O.S.; Nahar, M.S.; Jones, T.R.; Sartor, M.A.; Dolinoy, D.C. Detection of differential DNA methylation in repetitive DNA of mice and humans perinatally exposed to bisphenol A. Epigenetics 2016, 11, 489–500. [Google Scholar] [CrossRef]
- Dhimolea, E.; Wadia, P.R.; Murray, T.J.; Settles, M.L.; Treitman, J.D.; Sonnenschein, C.; Shioda, T.; Soto, A.M. Prenatal exposure to BPA alters the epigenome of the rat mammary gland and increases the propensity to neoplastic development. PLoS ONE 2014, 9, e99800. [Google Scholar] [CrossRef] [PubMed]
- Kitraki, E.; Nalvarte, I.; Alavian-Ghavanini, A.; Ruegg, J. Developmental exposure to bisphenol A alters expression and DNA methylation of Fkbp5, an important regulator of the stress response. Mol. Cell. Endocrinol. 2015, 417, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Xia, W.; Wang, D.Q.; Wan, Y.J.; Xu, B.; Chen, X.; Li, Y.Y.; Xu, S.Q. Hepatic DNA methylation modifications in early development of rats resulting from perinatal BPA exposure contribute to insulin resistance in adulthood. Diabetologia 2013, 56, 2059–2067. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.L.; Wang, Q.; Trevino, L.S.; Bosland, M.C.; Chen, J.; Medvedovic, M.; Prins, G.S.; Kannan, K.; Ho, S.M.; Walker, C.L. Identification of secretaglobin Scgb2a1 as a target for developmental reprogramming by BPA in the rat prostate. Epigenetics 2015, 10, 127–134. [Google Scholar] [CrossRef]
- Anderson, O.S.; Kim, J.H.; Peterson, K.E.; Sanchez, B.N.; Sant, K.E.; Sartor, M.A.; Weinhouse, C.; Dolinoy, D.C. novel epigenetic biomarkers mediating bisphenol a exposure and metabolic phenotypes in female mice. Endocrinology 2017, 158, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Sartor, M.A.; Rozek, L.S.; Faulk, C.; Anderson, O.S.; Jones, T.R.; Nahar, M.S.; Dolinoy, D.C. Perinatal bisphenol A exposure promotes dose-dependent alterations of the mouse methylome. BMC Genom. 2014, 15, 30. [Google Scholar] [CrossRef]
- Liu, Y.; Yuan, C.; Chen, S.; Zheng, Y.; Zhang, Y.; Gao, J.; Wang, Z. Global and cyp19a1a gene specific DNA methylation in gonads of adult rare minnow Gobiocypris rarus under bisphenol A exposure. Aquat. Toxicol. 2014, 156, 10–16. [Google Scholar] [CrossRef]
- Desaulniers, D.; Xiao, G.H.; Lian, H.; Feng, Y.L.; Zhu, J.; Nakai, J.; Bowers, W.J. Effects of mixtures of polychlorinated biphenyls, methylmercury, and organochlorine pesticides on hepatic DNA methylation in prepubertal female Sprague-Dawley rats. Int. J. Toxicol. 2009, 28, 294–307. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Hannigan, B.; Crews, D. Embryonic PCB exposure alters phenotypic, genetic, and epigenetic profiles in turtle sex determination, a biomarker of environmental contamination. Endocrinology 2014, 155, 4168–4177. [Google Scholar] [CrossRef] [PubMed]
- Solomon, O.; Yousefi, P.; Huen, K.; Gunier, R.B.; Escudero-Fung, M.; Barcellos, L.F.; Eskenazi, B.; Holland, N. Prenatal phthalate exposure and altered patterns of DNA methylation in cord blood. Environ. Mol. Mutagen. 2017, 58, 398–410. [Google Scholar] [CrossRef]
- Barakat, R.; Lin, P.C.; Park, C.J.; Zeineldin, M.; Zhou, S.; Rattan, S.; Brehm, E.; Flaws, J.A.; Ko, C.J. Germline-dependent transmission of male reproductive traits induced by an endocrine disruptor, di-2-ethylhexyl phthalate, in future generations. Sci. Rep. 2020, 10, 5705. [Google Scholar] [CrossRef]
- Walker, C.; Ghazisaeidi, S.; Collet, B.; Boisvert, A.; Culty, M. In utero exposure to low doses of genistein and di-(2-ethylhexyl) phthalate (DEHP) alters innate immune cells in neonatal and adult rat testes. Andrology 2020, 8, 943–964. [Google Scholar] [CrossRef]
- Manikkam, M.; Haque, M.M.; Guerrero-Bosagna, C.; Nilsson, E.E.; Skinner, M.K. Pesticide methoxychlor promotes the epigenetic transgenerational inheritance of adult-onset disease through the female germline. PLoS ONE 2014, 9, e102091. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Li, S.S. Epigenetic effects of environmental chemicals bisphenol A and phthalates. Int. J. Mol. Sci. 2012, 13, 10143–10153. [Google Scholar] [CrossRef]
- Annunziato, A. DNA Packaging: Nucleosomes and chromatin. Nat. Educ. 2008, 1, 26. [Google Scholar]
- Strahl, B.D.; Allis, C.D. The language of covalent histone modifications. Nature 2000, 403, 41–45. [Google Scholar] [CrossRef]
- Cedar, H.; Bergman, Y. Linking DNA methylation and histone modification: Patterns and paradigms. Nat. Rev. Genet. 2009, 10, 295–304. [Google Scholar] [CrossRef]
- Bredfeldt, T.G.; Greathouse, K.L.; Safe, S.H.; Hung, M.C.; Bedford, M.T.; Walker, C.L. Xenoestrogen-induced regulation of EZH2 and histone methylation via estrogen receptor signaling to PI3K/AKT. Mol. Endocrinol. 2010, 24, 993–1006. [Google Scholar] [CrossRef] [PubMed]
- Greathouse, K.L.; Bredfeldt, T.; Everitt, J.I.; Lin, K.; Berry, T.; Kannan, K.; Mittelstadt, M.L.; Ho, S.M.; Walker, C.L. Environmental estrogens differentially engage the histone methyltransferase EZH2 to increase risk of uterine tumorigenesis. Mol. Cancer Res. MCR 2012, 10, 546–557. [Google Scholar] [CrossRef] [PubMed]
- Warita, K.; Mitsuhashi, T.; Sugawara, T.; Tabuchi, Y.; Tanida, T.; Wang, Z.Y.; Matsumoto, Y.; Yokoyama, T.; Kitagawa, H.; Miki, T.; et al. Direct effects of diethylstilbestrol on the gene expression of the cholesterol side-chain cleavage enzyme (P450scc) in testicular Leydig cells. Life Sci. 2010, 87, 281–285. [Google Scholar] [CrossRef]
- Bhan, A.; Hussain, I.; Ansari, K.I.; Bobzean, S.A.; Perrotti, L.I.; Mandal, S.S. Bisphenol-A and diethylstilbestrol exposure induces the expression of breast cancer associated long noncoding RNA HOTAIR in vitro and in vivo. J. Steroid Biochem. Mol. Biol. 2014, 141, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Rutkowska, A.; Rachon, D. Bisphenol A (BPA) and its potential role in the pathogenesis of the polycystic ovary syndrome (PCOS). Gynecol. Endocrinol. Off. J. Int. Soc. Gynecol. Endocrinol. 2014, 30, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Casati, L.; Sendra, R.; Colciago, A.; Negri-Cesi, P.; Berdasco, M.; Esteller, M.; Celotti, F. Polychlorinated biphenyls affect histone modification pattern in early development of rats: A role for androgen receptor-dependent modulation? Epigenomics 2012, 4, 101–112. [Google Scholar] [CrossRef]
- Casati, L.; Sendra, R.; Poletti, A.; Negri-Cesi, P.; Celotti, F. Androgen receptor activation by polychlorinated biphenyls: Epigenetic effects mediated by the histone demethylase Jarid1b. Epigenetics 2013, 8, 1061–1068. [Google Scholar] [CrossRef]
- Otsuka, S.; Ishihara, A.; Yamauchi, K. Ioxynil and tetrabromobisphenol A suppress thyroid-hormone-induced activation of transcriptional elongation mediated by histone modifications and RNA polymerase II phosphorylation. Toxicol. Sci. Off. J. Soc. Toxicol. 2014, 138, 290–299. [Google Scholar] [CrossRef]
- Gottardo, F.; Liu, C.G.; Ferracin, M.; Calin, G.A.; Fassan, M.; Bassi, P.; Sevignani, C.; Byrne, D.; Negrini, M.; Pagano, F.; et al. Micro-RNA profiling in kidney and bladder cancers. Urol. Oncol. 2007, 25, 387–392. [Google Scholar] [CrossRef]
- Nothnick, W.B. The role of micro-RNAs in the female reproductive tract. Reproduction 2012, 143, 559–576. [Google Scholar] [CrossRef]
- Papaioannou, M.D.; Nef, S. microRNAs in the testis: Building up male fertility. J. Androl. 2010, 31, 26–33. [Google Scholar] [CrossRef]
- Wang, C.; Yang, C.; Chen, X.; Yao, B.; Yang, C.; Zhu, C.; Li, L.; Wang, J.; Li, X.; Shao, Y.; et al. Altered profile of seminal plasma microRNAs in the molecular diagnosis of male infertility. Clin. Chem. 2011, 57, 1722–1731. [Google Scholar] [CrossRef]
- He, Z.; Kokkinaki, M.; Pant, D.; Gallicano, G.I.; Dym, M. Small RNA molecules in the regulation of spermatogenesis. Reproduction 2009, 137, 901–911. [Google Scholar] [CrossRef]
- Vrijens, K.; Bollati, V.; Nawrot, T.S. MicroRNAs as potential signatures of environmental exposure or effect: A systematic review. Environ. Health Perspect. 2015, 123, 399–411. [Google Scholar] [CrossRef]
- Bunay, J.; Larriba, E.; Patino-Garcia, D.; Urriola-Munoz, P.; Moreno, R.D.; Del Mazo, J. Combined proteomic and miRNome analyses of mouse testis exposed to an endocrine disruptors chemicals mixture reveals altered toxicological pathways involved in male infertility. Mol. Hum. Reprod. 2019, 25, 156–169. [Google Scholar] [CrossRef]
- Avissar-Whiting, M.; Veiga, K.R.; Uhl, K.M.; Maccani, M.A.; Gagne, L.A.; Moen, E.L.; Marsit, C.J. Bisphenol A exposure leads to specific microRNA alterations in placental cells. Reprod. Toxicol. 2010, 29, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Sabry, R.; Yamate, J.; Favetta, L.; LaMarre, J. MicroRNAs: Potential targets and agents of endocrine disruption in female reproduction. J. Toxicol. Pathol. 2019, 32, 213–221. [Google Scholar] [CrossRef]
- Klinge, C.M. Estrogen Regulation of MicroRNA Expression. Curr. Genom. 2009, 10, 169–183. [Google Scholar] [CrossRef]
- Veiga-Lopez, A.; Luense, L.J.; Christenson, L.K.; Padmanabhan, V. Developmental programming: Gestational bisphenol-A treatment alters trajectory of fetal ovarian gene expression. Endocrinology 2013, 154, 1873–1884. [Google Scholar] [CrossRef]
- Lite, C.; Ahmed, S.; Santosh, W.; Seetharaman, B. Prenatal exposure to bisphenol-A altered miRNA-224 and protein expression of aromatase in ovarian granulosa cells concomitant with elevated serum estradiol levels in F1 adult offspring. J. Biochem. Mol. Toxicol. 2019, 33, e22317. [Google Scholar] [CrossRef] [PubMed]
- Tilghman, S.L.; Bratton, M.R.; Segar, H.C.; Martin, E.C.; Rhodes, L.V.; Li, M.; McLachlan, J.A.; Wiese, T.E.; Nephew, K.P.; Burow, M.E. Endocrine disruptor regulation of microRNA expression in breast carcinoma cells. PLoS ONE 2012, 7, e32754. [Google Scholar] [CrossRef]
- Chou, W.C.; Lee, P.H.; Tan, Y.Y.; Lin, H.C.; Yang, C.W.; Chen, K.H.; Chuang, C.Y. An integrative transcriptomic analysis reveals bisphenol A exposure-induced dysregulation of microRNA expression in human endometrial cells. Toxicol. Vitr. Int. J. Publ. Assoc. Bibra 2017, 41, 133–142. [Google Scholar] [CrossRef]
- Jacobs, M.N.; Marczylo, E.L.; Guerrero-Bosagna, C.; Ruegg, J. Marked for life: Epigenetic effects of endocrine disrupting chemicals. Annu. Rev. Environ. Resour. 2017, 42, 105–160. [Google Scholar] [CrossRef]
- Broughton, D.E.; Moley, K.H. Obesity and female infertility: Potential mediators of obesity’s impact. Fertil. Steril. 2017, 107, 840–847. [Google Scholar] [CrossRef]
- Kahn, B.E.; Brannigan, R.E. Obesity and male infertility. Curr. Opin. Urol. 2017, 27, 441–445. [Google Scholar] [CrossRef]
- Cardoso, A.M.; Alves, M.G.; Mathur, P.P.; Oliveira, P.F.; Cavaco, J.E.; Rato, L. Obesogens and male fertility. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2017, 18, 109–125. [Google Scholar] [CrossRef]
- Jung, D.; Becher, H.; Edler, L.; Flesch-Janys, D.; Gurn, P.; Konietzko, J.; Manz, A.; Papke, O. Elimination of beta-hexachlorocyclohexane in occupationally exposed persons. J. Toxicol. Environ. Health 1997, 51, 23–34. [Google Scholar] [CrossRef]
- Skinner, M.K.; Manikkam, M.; Tracey, R.; Guerrero-Bosagna, C.; Haque, M.; Nilsson, E.E. Ancestral dichlorodiphenyltrichloroethane (DDT) exposure promotes epigenetic transgenerational inheritance of obesity. BMC Med. 2013, 11, 228. [Google Scholar] [CrossRef] [PubMed]
- Crain, D.A.; Janssen, S.J.; Edwards, T.M.; Heindel, J.; Ho, S.M.; Hunt, P.; Iguchi, T.; Juul, A.; McLachlan, J.A.; Schwartz, J.; et al. Female reproductive disorders: The roles of endocrine-disrupting compounds and developmental timing. Fertil. Steril. 2008, 90, 911–940. [Google Scholar] [CrossRef]
- Ge, R.S.; Chen, G.R.; Tanrikut, C.; Hardy, M.P. Phthalate ester toxicity in Leydig cells: Developmental timing and dosage considerations. Reprod. Toxicol. 2007, 23, 366–373. [Google Scholar] [CrossRef]
- Barker, D.J. The developmental origins of adult disease. J. Am. Coll. Nutr. 2004, 23, 588s–595s. [Google Scholar] [CrossRef] [PubMed]
- Katz, T.A.; Yang, Q.; Treviño, L.S.; Walker, C.L.; Al-Hendy, A. Endocrine-disrupting chemicals and uterine fibroids. Fertil. Steril. 2016, 106, 967–977. [Google Scholar] [CrossRef]
- Brouard, V.; Guénon, I.; Bouraima-Lelong, H.; Delalande, C. Differential effects of bisphenol A and estradiol on rat spermatogenesis’ establishment. Reprod. Toxicol. 2016, 63, 49–61. [Google Scholar] [CrossRef]
- Milligan, S.R.; Khan, O.; Nash, M. Competitive binding of xenobiotic oestrogens to rat alpha-fetoprotein and to sex steroid binding proteins in human and rainbow trout (Oncorhynchus mykiss) plasma. Gen. Comp. Endocrinol. 1998, 112, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Rattan, S.; Zhou, C.; Chiang, C.; Mahalingam, S.; Brehm, E.; Flaws, J.A. Exposure to endocrine disruptors during adulthood: Consequences for female fertility. J. Endocrinol. 2017, 233, R109–R129. [Google Scholar] [CrossRef]



| EDCs | Pathway/Receptor | Antagonist/Agonist | Reference |
|---|---|---|---|
| BPA | ER | Agonist | [44] |
| AR | Antagonist | [45] | |
| DDTs | ER | Agonist | [46] |
| ER | Agonist | [47] | |
| ER | Agonist | [44] | |
| AR | Antagonist | [46] | |
| AR | Antagonist | [47] | |
| PCBs | AR | Agonist, antagonist | [48] |
| ER | Agonist | [48] | |
| AR | Agonist | [49] | |
| PBDEs | ER | Agonist, antagonist | [50] |
| AR | Antagonist | [50] |
| EDC | Species | Concentration | Locus/Genes | Reference |
|---|---|---|---|---|
| BPA | Wistar Furth rat | 250 μg/kg/day | transcriptional initiation site of the alpha-lactalbumin gene | [131] |
| Female Wistar Rat | 40 μg/kg/day | Fkbp5 | [132] | |
| Mouse | 0–80 uM | Mybph, Prkcd | [127] | |
| Pregnant Wistar rat | 50 μg/kg/day | ↓ hepatic glucokinase, ↑Gck | [133] | |
| Rat | 10 μg/kg/day | ↑ Scgb2a1 | [134] | |
| Mouse | 50 ng/kg, 50/kg μg, 50 mg/kg | Jak-2, Rxr, Rfxap, Tmem 238 | [135] | |
| Mouse | 50 μg and 50 mg/kg/day | Myh7b, Slc22a | [136] | |
| Rare minnow Gobiocypris rarus | 15 μg/L | ↓cyp19a1a | [137] | |
| Methyl mercury | Rat | 2 mg/Kg/Day | ↓ DNMT (global hypomethylation) | [138] |
| PCBs | Rat | 1.1 mg/kg/day | ↓DNMT-1, 3a, 3b (global hypomethylation) | [138] |
| Slider turtle | 0–200 μg/L | Aromatase promoter | [139] | |
| DEHP | Human | - | IFT140, TESC and PRDM8 | [140] |
| Rat | 100 mg | Dnmt3a, Dnmt3b and Dnmt1 | [98] | |
| Mouse | 20 or 200 μg/kg/day | Y chromosome genes (↓ Sry; ↑Eif2s3y; ↑chromodomain protein; ↑Cdyl; ↑Zfy2) | [141] | |
| (DEHP in mixture with genistein) | Rat | 0.1 and 10 mg/kg/day | Kitlg, Rsk2, Nr3c1, Nqo1, Lif, Fyn, Dep-1, Gpr116, Pfn2 and Ptgr1 | [142] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amir, S.; Shah, S.T.A.; Mamoulakis, C.; Docea, A.O.; Kalantzi, O.-I.; Zachariou, A.; Calina, D.; Carvalho, F.; Sofikitis, N.; Makrigiannakis, A.; et al. Endocrine Disruptors Acting on Estrogen and Androgen Pathways Cause Reproductive Disorders through Multiple Mechanisms: A Review. Int. J. Environ. Res. Public Health 2021, 18, 1464. https://doi.org/10.3390/ijerph18041464
Amir S, Shah STA, Mamoulakis C, Docea AO, Kalantzi O-I, Zachariou A, Calina D, Carvalho F, Sofikitis N, Makrigiannakis A, et al. Endocrine Disruptors Acting on Estrogen and Androgen Pathways Cause Reproductive Disorders through Multiple Mechanisms: A Review. International Journal of Environmental Research and Public Health. 2021; 18(4):1464. https://doi.org/10.3390/ijerph18041464
Chicago/Turabian StyleAmir, Saira, Syed Tahir Abbas Shah, Charalampos Mamoulakis, Anca Oana Docea, Olga-Ioanna Kalantzi, Athanasios Zachariou, Daniela Calina, Felix Carvalho, Nikolaos Sofikitis, Antonios Makrigiannakis, and et al. 2021. "Endocrine Disruptors Acting on Estrogen and Androgen Pathways Cause Reproductive Disorders through Multiple Mechanisms: A Review" International Journal of Environmental Research and Public Health 18, no. 4: 1464. https://doi.org/10.3390/ijerph18041464
APA StyleAmir, S., Shah, S. T. A., Mamoulakis, C., Docea, A. O., Kalantzi, O.-I., Zachariou, A., Calina, D., Carvalho, F., Sofikitis, N., Makrigiannakis, A., & Tsatsakis, A. (2021). Endocrine Disruptors Acting on Estrogen and Androgen Pathways Cause Reproductive Disorders through Multiple Mechanisms: A Review. International Journal of Environmental Research and Public Health, 18(4), 1464. https://doi.org/10.3390/ijerph18041464












