A Rapid Realist Review of Group Psychological First Aid for Humanitarian Workers and Volunteers
Abstract
1. Introduction
1.1. The Problem
1.2. Group Psychological First Aid
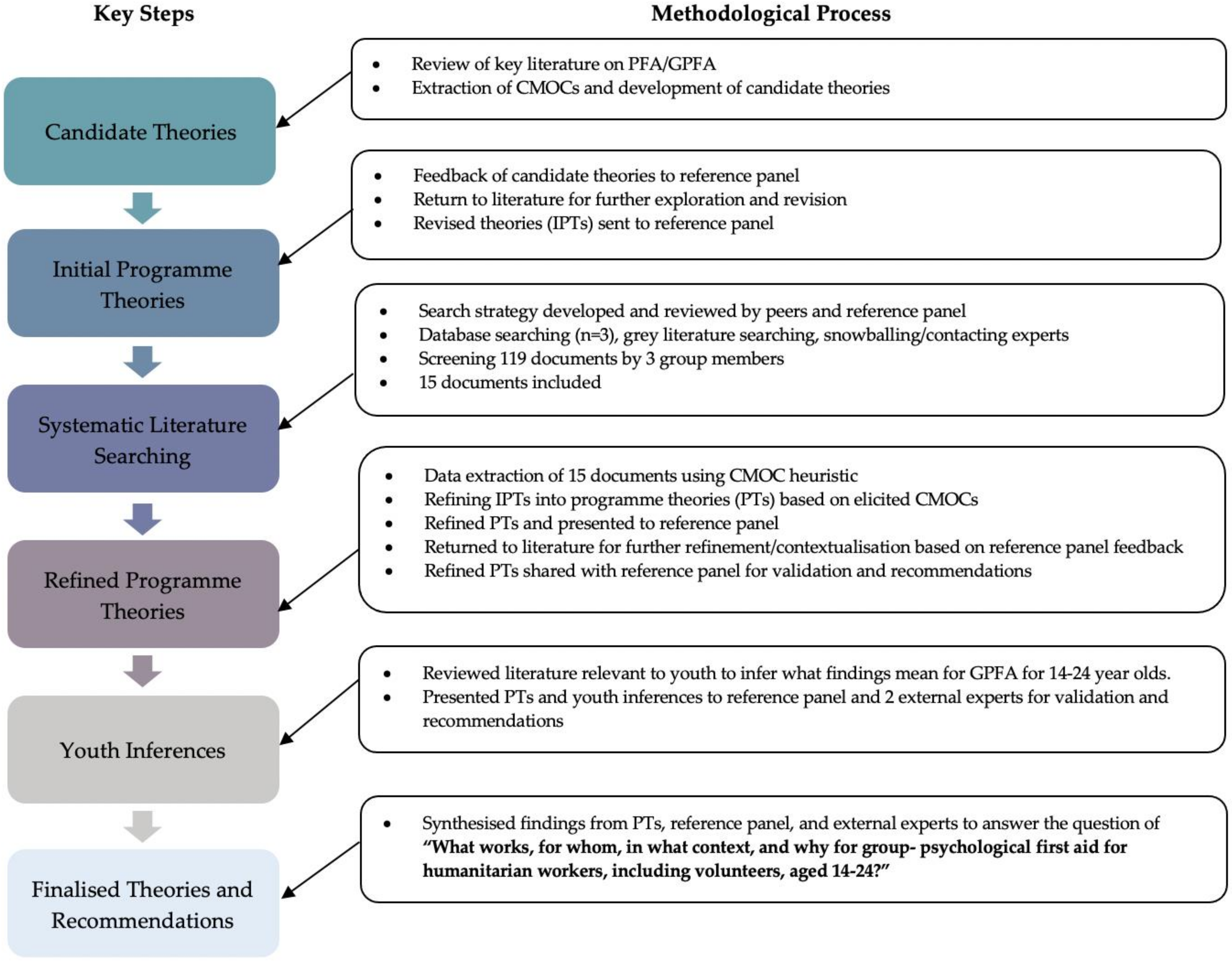
2. Materials and Methods
2.1. Reference Group and Experts
2.2. Preliminary Review of the Literature and Initial Programme Theories
2.3. Systematic Literature Searching
- About (or applicable to) PFA/GPFA;
- Provided in a humanitarian or emergency response;
- Targets youth;
- Targets anxiety and/or depression.
2.4. Changes to Process—Youth Inferences
3. Results
3.1. Data Analysis and Research Activity
- The inclusion of 15 documents identified through a systematic search of databases (n = 6), websites, and grey literature (n = 9) (See Figure 2);
- Two reference panel virtual meetings, where theories were presented and feedback provided;
- Two feedback reports from the reference panel assessing how input was incorporated, and providing updated findings (programme theories) for their review;
- Review of literature specific to youth/adolescents participating in group interventions and/or youth/adolescents mental health considerations for interventions;
- Two virtual meetings with external experts, where the refined programme theories (PTs) and findings from the youth-related supplemental work were disseminated. Inputs and recommendations were sought, and changes were made to produce finalised programme theories.
3.2. Defining Group Psychological First Aid
3.3. Theory Refinement
3.4. Finalised Theories
3.4.1. Programme Theory 1: Natural Reactions and Adaptive Coping Strategies
Following an acute crisis or period of prolonged distress, if GPFA is delivered early and appropriately, it provides a space to discuss natural reactions, normalise relationships, and address expectations. If this occurs, participants will be better equipped to process experiences early, feel their reactions are normal, and to continue supporting their mental health. This can lead to improved healthy coping strategies, self-awareness, and the management and prevention of distress escalation or re-escalation [42,43,44,45,46,47,48,49,50,51,52].
3.4.2. Programme Theory 2: Meeting Basic Needs
Acute crises and periods of prolonged distress affect individuals differently depending on exposure levels or previous life experiences. Basic resource needs may be disrupted, requiring different levels of physical and psychological support. If GPFA is provided in a comfortable location, complemented by a layered system of supports, this can help meet an individual’s basic physical and/or psychological needs, which can increase their sense of stability, safety, and control. If this occurs, individuals are able to be more emotionally expressive, self-efficacious, and recognise their reactions as natural. This helps to prevent distress escalation through emotional stabilisation, reduced secondary stressors, and helping individuals cope on their own [42,43,48,51,52].
3.4.3. Programme Theory 3: Response Matched to Individual Needs
Acute crises and periods of prolonged distress affect individuals differently depending on exposure levels or previous life experiences. When there is an existing social support/resource system, if GPFA is linked with this system and facilitators can gauge individual reactions and needs, this can enable an open space for members to share reactions, coping strategies, and resources. This can also support individuals to be referred for additional support for them (either through more formal service connections or informal one-on-one meetings with a facilitator). Supporting service connections in group formats can reduce stigma associated with care-seeking and increase access to needs-matched services, reducing secondary stressors and strengthening and individual’s ability to cope on their own [42,43,44,46,47,49,50,51,52,53].
3.4.4. Programme Theory 4: Fostering Support and Social Cohesion
4.1—When GPFA is provided to a small group of individuals who already know each other and share similar experiences and stress levels, it provides an opportunity to discuss reactions and emotions. This helps individuals feel more supported by peers, strengthens group cohesion, validates reactions, and opens communication about mental health. The outcome is the fostering of relationships, reduced isolation, increased sense of safety and belonging, and improved coping [42,43,44,46,47,48,50,51,52,54].
4.2—When GPFA is provided to a small group, who may not know each other but share similar experiences and stress levels, and members can forge new relationships with one another, it can develop and strengthen a sense of belonging to communities, foster relationships, communication, and help group members feel less isolated [42,43,44,46,47,48,50,51,52,54].
3.4.5. Programme Theory 5: Group Composition
When people experience a similar acute crisis or prolonged stress, and GPFA is provided with members and facilitators working at similar levels (or if different, where neither group holds direct authority over the other), power imbalances can be reduced, supporting open and honest sharing. This can also develop a sense of comradery and group cohesion, increasing communication, participation, and attendance [26,42,44,46,47,48,50,51,54].
3.4.6. Programme Theory 6: Sustainability and Accessibility
Following an acute crisis or period of prolonged distress, when GPFA is linked into complementary supports safely and with cultural competence, GPFA can improve support and access to these support services through increasing visibility and reducing stigma associated with care-seeking. The outcome may be more individuals accessing ongoing support, reduced secondary stressors, decreased isolation, and more sustained support [26,42,43,44,52,54].
3.4.7. Programme Theory 7: The Facilitators
Acute crises and periods of prolonged distress affect individuals differently depending on exposure levels or previous life experiences. When GPFA is provided by appropriately trained facilitators (ideally two), who are able to gauge individual reactions and needs, groups can be composed based on similar distress levels or needs. A second facilitator supports severely distressed members by taking them aside and providing or linking them to more specialised care. This protects individuals’ dignity, reduces the exposure of the member to secondary trauma, and ensures needs-matched care [43,44,46,49,51,52,53,54].
4. Discussion
4.1. Youth and GPFA
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Detailed Search Strategy, Returns, and Inclusion/Exclusion Criteria
| Population 1 (OR) | Population 2 (OR) | Exposure (OR) | Intervention (OR) |
|---|---|---|---|
| Humanitarian workers Humanitarian volunteers Emergency workers Emergency volunteers Crisis workers Crisis volunteers Relief workers Relief aid workers NGO staff NGO volunteer | Youth Young persons Young adults Adolescent | Trauma Traumatic event Critical incident Emergency Crisis Humanitarian crisis Acute crisis Disaster Terrorism Depression Anxiety | Psychological first aid PFA Group psychological first aid G-PFA Team PFA Stress first aid SFA Mental health first aid Psychoeducation |
| Website | Date | Reviewed | Included |
|---|---|---|---|
| WHO | 31 August 2020 | 7 | 0 |
| 1 September 2020 | 2 | 0 | |
| United Nations | 1 September 2020 | 1 | 0 |
| MHPSS Network | 2 September 2020 | 6 | 3 |
| Relief Web | 2 September 2020 | 8 | 6 |
| Elrha | 3 September 2020 | 5 | 0 |
| ICRC | 4 September 2020 | 6 | 0 |
| IFRC | 4 September 2020 | 5 | 0 |
| Inclusion Criteria: | Exclusion Criteria: |
|---|---|
Main subject, or important area of the wider topic discussed, must be:
| Main subject of literature is:
|
Appendix B. Initial Programme Theories
References
- Jachens, L.; Houdmont, J.; Thomas, R. Work-related stress in a humanitarian context: A qualitative investigation. Disasters 2018, 42, 619–634. [Google Scholar] [CrossRef]
- Connorton, E.; Perry, M.J.; Hemenway, D.; Miller, M. Humanitarian Relief Workers and Trauma-related Mental Illness. Epidemiol. Rev. 2012, 34, 145–155. [Google Scholar] [CrossRef]
- Lopes Cardozo, B.; Gotway Crawford, C.; Eriksson, C.; Zhu, J.; Sabin, M.; Ager, A.; Foy, D.; Snider, L.; Scholte, W.; Kaiser, R.; et al. Psychological distress, depression, anxiety, and burnout among international humanitarian aid workers: A longitudinal study. PLoS ONE 2012, 7, e44948. [Google Scholar] [CrossRef]
- Lopes Cardozo, B.; Holtz, T.H.; Kaiser, R.; Gotway, C.A.; Ghitis, F.; Toomey, E.; Salama, P. The Mental Health of Expatriate and Kosovar Albanian Humanitarian Aid Workers. Disasters 2005, 29, 152–170. [Google Scholar] [CrossRef]
- Musa, S.A.; Hamid, A.A.R.M. Psychological problems among aid workers operating in Darfur. Soc. Behav. Personal. Int. J. 2008, 36, 407–416. [Google Scholar] [CrossRef]
- Thormar, S.B.; Gersons, B.P.; Juen, B.; Marschang, A.; Djakababa, M.N.; Olff, M. The mental health impact of volunteering in a disaster setting: A review. J. Nerv. Ment. Dis. 2010, 198, 529–538. [Google Scholar] [CrossRef]
- Strohmeier, H.; Scholte, W.F. Trauma-related mental health problems among national humanitarian staff: A systematic review of the literature. Eur. J. Psychotraumatol. 2015, 6, 28541. [Google Scholar] [CrossRef]
- Hazeldine, S.; Baillie Smith, M. IFRC Global Review of Volunteering Report; IFRC: Geneva, Switzerland, 2015. [Google Scholar]
- Eriksson, C.B.; Bjorck, J.P.; Larson, L.C.; Walling, S.M.; Trice, G.A.; Fawcett, J.; Abernethy, A.D.; Foy, D.W. Social support, organisational support, and religious support in relation to burnout in expatriate humanitarian aid workers. Ment. Health Relig. Cult. 2009, 12, 671–686. [Google Scholar] [CrossRef]
- Aldamman, K.; Tamrakar, T.; Dinesen, C.; Wiedemann, N.; Murphy, J.; Hansen, M.; Badr, E.E.; Reid, T.; Vallières, F. Caring for the mental health of humanitarian volunteers in traumatic contexts: The importance of organisational support. Eur. J. Psychotraumatol. 2019, 10, 1694811. [Google Scholar] [CrossRef]
- Solanki, H. Mindfulness and Wellbeing. In Mental Health and Humanitarian aid Workers: A Shift of Emphasis from Treatment to Prevention; Action Against Hunger: London, UK, 2015. [Google Scholar]
- Vareilles, G.; Marchal, B.; Kane, S.; Petrič, T.; Pictet, G.; Pommier, J. Understanding the motivation and performance of community health volunteers involved in the delivery of health programmes in Kampala, Uganda: A realist evaluation. BMJ Open 2015, 5, e008614. [Google Scholar] [CrossRef][Green Version]
- van Schie, S.; Güntert, S.T.; Oostlander, J.; Wehner, T. How the Organizational Context Impacts Volunteers: A Differentiated Perspective on Self-determined Motivation. Volunt. Int. J. Volunt. Nonprofit Organ. 2015, 26, 1570–1590. [Google Scholar] [CrossRef]
- Kok, M.C.; Dieleman, M.; Taegtmeyer, M.; Broerse, J.E.; Kane, S.S.; Ormel, H.; Tijm, M.M.; de Koning, K.A. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. 2014. [Google Scholar] [CrossRef]
- Snider, L. Caring for Volunteers: A Psychosocial Support Toolkit; IFRC: Copenhagen, Denmark, 2012; pp. 1–71. [Google Scholar]
- Shultz, J.M.; Forbes, D. Psychological First Aid: Rapid proliferation and the search for evidence. Disaster Health 2013, 2, 3–12. [Google Scholar] [CrossRef]
- van Emmerik, A.A.P.; Kamphuis, J.H.; Hulsbosch, A.M.E.; Paul, M.G. Single session debriefing after psychological trauma: A meta-analysis. Lancet 2002, 360, 766–771. [Google Scholar] [CrossRef]
- Carlier, I.V.E.; Lamberts, R.D.; Uchelen, A.J.V.; Gersons, B.P.R. Disaster-related post-traumatic stress in police officers: A field study of the impact of debriefing. Stress Med. 1998, 14, 143–148. [Google Scholar] [CrossRef]
- Mayou, R.; Ehlers, A.; Hobbs, M. Psychological debriefing for road traffic accident victims. Three-year follow-up of a randomised controlled trial. Br. J. Psychiatry J. Ment. Sci. 2000, 176, 589–593. [Google Scholar] [CrossRef]
- Snider, L.; Van Ommeren, M.; Schafer, A. Psychological First Aid: Guide for Field Workers; World Health Organization: Geneva, Switzerland, 2011; p. 60. [Google Scholar]
- IFRC. Guidelines for Caring for Staff and Volunteers in Crises; IFRC: Copenhagen, Denmark, 2019. [Google Scholar]
- Hobfoll, S.; Watson, P.; Bell, C.; Bryant, R.; Brymer, M.; Friedman, M.; Friedman, M.; Gersons, B.; de Jong, J.; Layne, C.; et al. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry 2007, 70, 283–315. [Google Scholar] [CrossRef]
- Everly, G.S.; Phillips, S.B.; Kane, D.; Feldman, D. Introduction to and Overview of Group Psychological First Aid. Brief Treat. Crisis Interv. 2006, 6, 130–136. [Google Scholar] [CrossRef]
- Hansen, P. Training in Psychological First Aid for Red Cross and Red Crescent Societies: Module 4: PFA in Groups—Support to Teams; IFRC: Copenhagen, Denmark, 2018. [Google Scholar]
- Dieltjens, T.; Moonens, I.; Van Praet, K.; De Buck, E.; Vandekerckhove, P. A Systematic Literature Search on Psychological First Aid: Lack of Evidence to Develop Guidelines. PLoS ONE 2014, 9, e114714. [Google Scholar] [CrossRef]
- Schafer, A.; Snider, L.; Sammour, R. A reflective learning report about the implementation and impacts of Psychological First Aid (PFA) in Gaza. Disaster Health 2016, 3, 1–10. [Google Scholar] [CrossRef]
- WHO; CBM; World Vision; UNICEF. Psychological First Aid for Ebola Virus Disease Outbreak; WHO: Gevena, Switzerland, 2014; pp. 1–60. [Google Scholar]
- Youth Custody Service; NHS. COVID-19 Guide: Psychological First Aid for Children and Young People; NHS: London, UK, 2020; pp. 1–5. Available online: https://www.england.nhs.uk/coronavirus/publication/covid-19-guide-psychological-first-aid-for-children-and-young-people/ (accessed on 10 October 2020).
- WHO. Psychological First Aid for All: Supporting People in the Aftermath of Crisis Events; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Fox, J.H.; Burkle, F.M.; Bass, J.; Pia, F.A.; Epstein, J.L.; Markenson, D. The Effectiveness of Psychological First Aid as a Disaster Intervention Tool: Research Analysis of Peer-Reviewed Literature From 1990–2010. Disaster Med. Public Health Prep. 2012, 6, 247–252. [Google Scholar] [CrossRef]
- Sijbrandij, M.; Horn, R.; Esliker, R.; O’May, F.; Reiffers, R.; Ruttenberg, L.; Stam, K.; de Jong, J.; Ager, A. The Effect of Psychological First Aid Training on Knowledge and Understanding about Psychosocial Support Principles: A Cluster-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 484. [Google Scholar] [CrossRef]
- Ulman, K.H. Group Interventions for Treatment of Psychological Trauma: Module 1: Group Interventions for Treatment of Trauma in Adults; American Group Psychotherapy Association: New York, NY, USA, 2004. [Google Scholar]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Rycroft-Malone, J.; McCormack, B.; Hutchinson, A.M.; DeCorby, K.; Bucknall, T.K.; Kent, B.; Schultz, A.; Snelgrove-Clarke, E.; Stetler, C.B.; Titler, M.; et al. Realist synthesis: Illustrating the method for implementation research. Implement. Sci. 2012, 7, 1–10. [Google Scholar] [CrossRef]
- Pawson, R. Evidence-based Policy: The Promise of ‘Realist Synthesis’. Sage Publ. 2002, 8, 340–358. [Google Scholar] [CrossRef]
- Pawson, R.; Tilley, N. Realistic Evaluation; SAGE: London, England, 1997. [Google Scholar]
- Dalkin, S.M.; Greenhalgh, J.; Jones, D.; Cunningham, B.; Lhussier, M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement. Sci. 2015, 10. [Google Scholar] [CrossRef]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards: Realist syntheses. BMC Med. 2013, 11, 1–14. [Google Scholar] [CrossRef]
- Saul, J.E.; Willis, C.D.; Bitz, J.; Best, A. A time-responsive tool for informing policy making: Rapid realist review. Implement. Sci. 2013, 8, 103. [Google Scholar] [CrossRef]
- British Red Cross. Life after Lockdown: Tackling Loneliness Among those Left Behind; British Red Cross: London, UK, 2020; pp. 1–19. Available online: https://www.redcross.org.uk/about-us/what-we-do/we-speak-up-for-change/life-after-lockdown-tackling-loneliness (accessed on 10 October 2020).
- Inter-Agency Standing Committee. IASC Guidelines for Mental Health and Psychosocial Support in Emergency Settings; IASC: Geneva, Switzerland, 2007; p. 205. [Google Scholar]
- Landoy, B.V.N.; Hechanova, M.R.M.; Ramos, P.A.P.; Kintanar, N.S.M. The Application and Adaptation of Psychological First Aid: The Filipino Psychologists’ Experience After Typhoon Haiyan. Psychol. Assoc. Phillipines 2015, 48, 81–104. [Google Scholar]
- Hechanova, M.R.M.; Ramos, P.A.P.; Waelde, L. Group-based mindfulness informed psychological first aid after Typhoon Haiyan. Disaster Prev. Manag. 2015, 24, 610–618. [Google Scholar] [CrossRef]
- Hussein Rasheed, R. Refugees Deliver Mental Health Services to Locked down Camps in Iraq; ReliefWeb: Duhok, Iraq, 2020. [Google Scholar]
- International Alert. Supporting the Volunteers on Front Line of Ukraine Conflict; International Alert: Kyiv, Ukraine, 2017; Available online: https://www.international-alert.org/news/supporting-volunteers-front-line-ukraine-conflict (accessed on 10 October 2020).
- Phillippine Government. Surigao Quake Survivors Receive Psych First Aid, Psychosocial Support; ReliefWeb: Cotabato City, Phillipines, 2017; Available online: https://reliefweb.int/report/philippines/surigao-quake-survivors-receive-psych-first-aid-psychosocial-support (accessed on 10 October 2020).
- Mail & Gaurdian. Ebola Burials Traumatise Aid Workers; Mail & Gaurdian: Johannesburg, South Africa, 2015. [Google Scholar]
- IFRC. Coping with Crisis—Focus: Volunteers—Capacity Building; IFRC: Copenhagen, Denmark, 2015; pp. 1–24. [Google Scholar]
- Shultz, J.M.; Kelly, F.; Forbes, D.; Verdeli, H.; Leon, G.R.; Rosen, A.; Neria, Y. Triple threat trauma: Evidence-based mental health response for the 2011 Japan disaster. Prehosp. Disaster Med. 2011, 26, 141–145. [Google Scholar] [CrossRef][Green Version]
- Alisic, E.; Conroy, R.; Magyar, J.; Babl, F.E.; O’Donnell, M.L. Psychosocial care for seriously injured children and their families: A qualitative study among emergency department nurses and physicians. Injury 2014, 45, 1452–1458. [Google Scholar] [CrossRef]
- Turunen, T.; Haravuori, H.; Pihlajamäki, J.J.; Marttunen, M.; Punamäki, R.-L. Framework of the outreach after a school shooting and the students perceptions of the provided support. Eur. J. Psychotraumatol. 2014, 5. [Google Scholar] [CrossRef]
- Legerski, J.-P.; Vernberg, E.M.; Noland, B.J. A qualitative analysis of barriers, challenges, and successes in meeting the needs of Hurricane Katrina evacuee families. Community Ment. Health J. 2012, 48, 729–740. [Google Scholar] [CrossRef]
- Akoury-Dirani, L.; Sahakian, T.S.; Hassan, F.Y.; Hajjar, R.V.; El Asmar, K. Psychological first aid training for Lebanese field workers in the emergency context of the Syrian refugees in Lebanon. Psychol. Trauma Theory Res. Pract. Policy 2015, 7, 533–538. [Google Scholar] [CrossRef]
- Waterman, S.; Hunter, E.C.M.; Cole, C.L.; Evans, L.J.; Greenberg, N.; Rubin, G.J.; Beck, A. Training peers to treat Ebola centre workers with anxiety and depression in Sierra Leone. Int. J. Soc. Psychiatry 2018, 64, 156–165. [Google Scholar] [CrossRef]
- Uhernik, J.A.; Husson, M.A. Psychological first aid: An evidence informed approach for acute disaster behavioral health response. In Compelling Counseling Interventions: VISTAS, 200(9); 2009; pp. 271–280. Available online: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.551.5248&rep=rep1&type=pdf (accessed on 10 October 2020).
- WHO. Support based on the Psychological First Aid Principles in People Recently Exposed to a Traumatic Event; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Horn, R.; O’May, F.; Esliker, R.; Gwaikolo, W. The myth of the 1-day training: The effectiveness of psychosocial support capacity-building during the Ebola outbreak in West Africa. Glob. Ment. Health 2019, 6. [Google Scholar] [CrossRef]
- Crepeau-Hobson, F.; Sievering, K.S.; Armstrong, C.; Stonis, J. A Coordinated Mental Health Crisis Response: Lessons Learned From Three Colorado School Shootings. J. Sch. Violence 2012, 11, 207–225. [Google Scholar] [CrossRef]
- Grover, S. 5 Reasons Group Therapy Is the Best Choice Struggling Teens; Psychology Today: New York, NY, USA, 2017. [Google Scholar]
- Glodich, A.; Allen, J.G. Adolescents Exposed to Violence and Abuse: A Review of the Group Therapy Literature with an Emphasis on Preventing Trauma Reenactment. J. Child Adolesc. Group Ther. 1998, 8, 135–154. [Google Scholar] [CrossRef]
- Hoag, M.J.; Burlingame, G.M. Evaluating the Effectiveness of Child and Adolescent Group Treatment: A Meta-Analytic Review. J. Clin. Child Psychol. 1997, 26, 234–246. [Google Scholar] [CrossRef]
- Kelly, M.; Coughlan, B. A theory of youth mental health recovery from a parental perspective. Child Adolesc. Ment. Health 2019, 24, 161–169. [Google Scholar] [CrossRef]
- Coholic, D.; Dano, K.; Sindori, S.; Eys, M. Group work in mindfulness-based interventions with youth: A scoping review. Soc. Work Groups 2019, 42, 259–274. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corey, J.; Vallières, F.; Frawley, T.; De Brún, A.; Davidson, S.; Gilmore, B. A Rapid Realist Review of Group Psychological First Aid for Humanitarian Workers and Volunteers. Int. J. Environ. Res. Public Health 2021, 18, 1452. https://doi.org/10.3390/ijerph18041452
Corey J, Vallières F, Frawley T, De Brún A, Davidson S, Gilmore B. A Rapid Realist Review of Group Psychological First Aid for Humanitarian Workers and Volunteers. International Journal of Environmental Research and Public Health. 2021; 18(4):1452. https://doi.org/10.3390/ijerph18041452
Chicago/Turabian StyleCorey, Julia, Frédérique Vallières, Timothy Frawley, Aoife De Brún, Sarah Davidson, and Brynne Gilmore. 2021. "A Rapid Realist Review of Group Psychological First Aid for Humanitarian Workers and Volunteers" International Journal of Environmental Research and Public Health 18, no. 4: 1452. https://doi.org/10.3390/ijerph18041452
APA StyleCorey, J., Vallières, F., Frawley, T., De Brún, A., Davidson, S., & Gilmore, B. (2021). A Rapid Realist Review of Group Psychological First Aid for Humanitarian Workers and Volunteers. International Journal of Environmental Research and Public Health, 18(4), 1452. https://doi.org/10.3390/ijerph18041452







