Effectiveness of Online Mindfulness-Based Intervention (iMBI) on Inattention, Hyperactivity–Impulsivity, and Executive Functioning in College Emerging Adults with Attention-Deficit/Hyperactivity Disorder: A Study Protocol
Abstract
1. Introduction
1.1. Emerging Adulthood and ADHD
1.2. The Present Study
1.2.1. Management of ADHD to Improve Core Symptoms
1.2.2. Promotion of Non-Pharmacological Interventions
1.2.3. Accessibility of Therapy
1.2.4. Mindfulness-Based Intervention as a Potential Treatment Choice
1.2.5. Online Intervention as a New Treatment Modality
2. Materials and Methods
2.1. Study Intervention
2.1.1. Online Mindfulness-Based Intervention
2.1.2. Enhanced Treatment-as-Usual Control Group
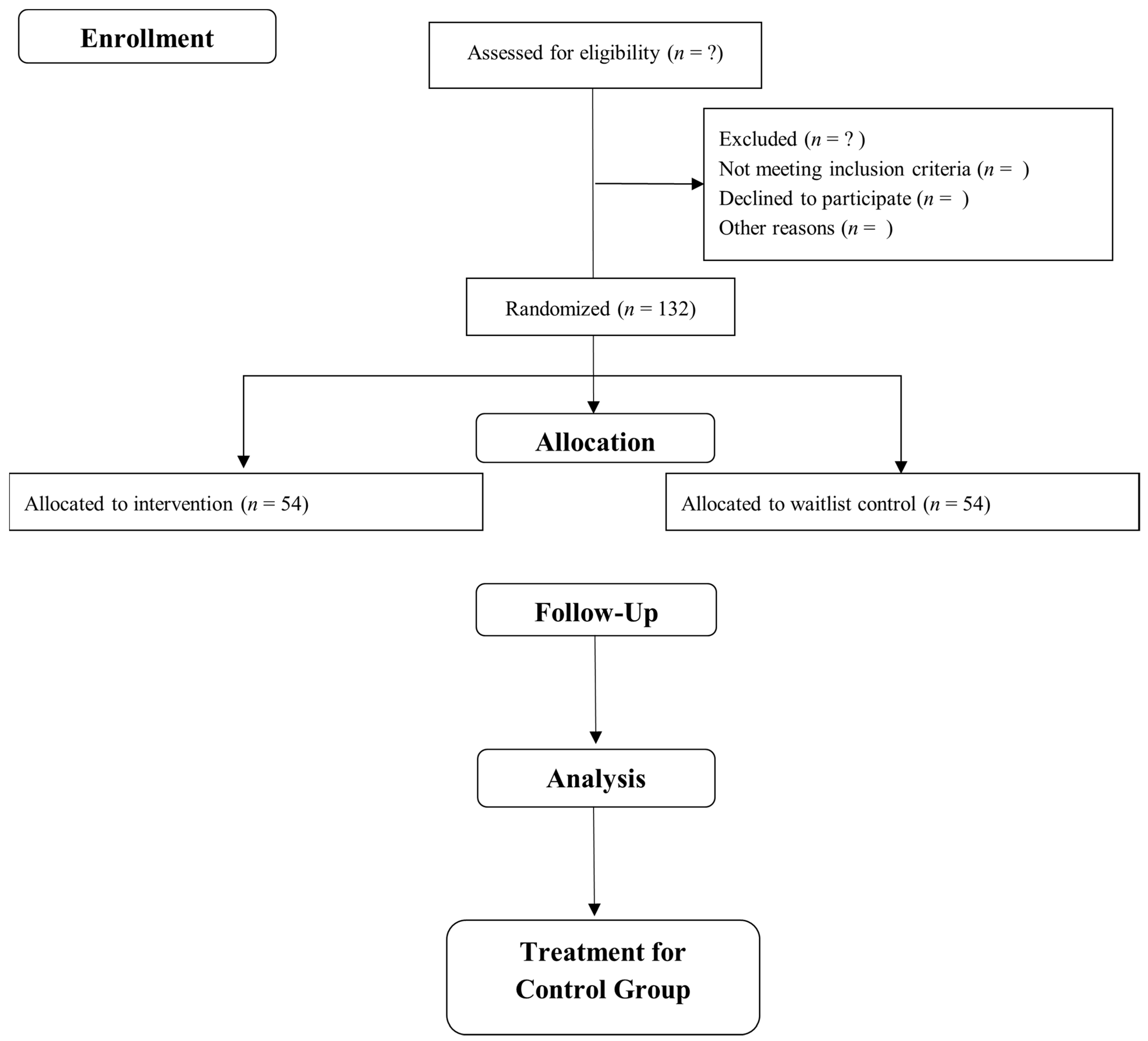
2.2. Study Design
2.3. Randomization
2.4. Study Population
2.5. Sample Size
2.6. Inclusion and Exclusion Criteria
2.7. Treatment Outcome Measures
2.8. Sociodemographic Information and Clinical Characteristics
2.9. Ethical Considerations
2.10. Study Procedures
2.11. Data Analysis
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; DSM-5; American Psychiatric Publishing: Washington, DC, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- Silverstein, M.J.; Faraone, S.V.; Leon, T.L.; Biederman, J.; Spencer, T.J.; Adler, L.A. The Relationship Between Executive Function Deficits and DSM-5-Defined ADHD Symptoms. J. Atten. Disord. 2020, 24, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Agnew-Blais, J.C.; Polanczyk, G.V.; Danese, A.; Wertz, J.; Moffitt, T.E.; Arseneault, L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry 2016, 73, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Adler, L.; Barkley, R.; Biederman, J.; Conners, C.K.; Demler, O.; Faraone, S.V.; Greenhill, L.L.; Howes, M.J.; Secnik, K.; et al. The prevalence and correlates of adult ADHD in the United States: Results from the national comorbidity survey replication. Am. J. Psychiatry 2006, 163, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Tandon, M.; Tillman, R.; Agrawal, A.; Luby, J. Trajectories of ADHD severity over 10 years from childhood into adulthood. ADHD Atten. Deficit Hyperact. Disord. 2016, 8, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Caye, A.; Rocha, T.B.-M.; Anselmi, L.; Murray, J.; Menezes, A.M.B.; Barros, F.C.; Gonçalves, H.; Wehrmeister, F.; Jensen, C.M.; Steinhausen, H.-C.; et al. Attention-deficit/hyperactivity disorder trajectories from Childhood to Young Adulthood. JAMA Psychiatry 2016, 73, 705. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, T.E.; Houts, R.; Asherson, P.; Belsky, D.W.; Corcoran, D.L.; Hammerle, M.; Harrington, H.; Hogan, S.; Meier, M.H.; Polanczyk, G.V.; et al. Is adult ADHD a childhood-onset neurodevelopmental disorder? Evidence from a four-decade longitudinal cohort study. Am. J. Psychiatry 2015, 172, 967–977. [Google Scholar] [CrossRef]
- Vitola, E.S.; Bau, C.H.D.; Salum, G.A.; Horta, B.L.; Quevedo, L.; Barros, F.C.; Pinheiro, R.T.; Kieling, C.; Rohde, L.A.; Grevet, E.H. Exploring DSM-5 ADHD criteria beyond young adulthood: Phenomenology, psychometric properties and prevalence in a large three-decade birth cohort. Psychol. Med. 2017, 47, 744–754. [Google Scholar] [CrossRef]
- Institute for Public Health. National Health and Morbidity Survey 2015; Institute for Public Health: Kuala Lumpur, Malaysia, 2015; Volume 2, p. 315. [Google Scholar]
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef]
- Arnett, J.J. The evidence for generation we and against generation me. Emerg. Adulthood 2013, 1, 5–10. [Google Scholar] [CrossRef]
- Schwartz, S.J.; Zamboanga, B.L.; Luyckx, K.; Meca, A.; Ritchie, R.A. Identity in emerging adulthood. Emerg. Adulthood 2013, 1, 96–113. [Google Scholar] [CrossRef]
- Simons-Morton, B.; Haynie, D.; Liu, D.; Chaurasia, A.; Li, K.; Hingson, R. The effect of residence, school status, work status, and social influence on the prevalence of alcohol use among emerging adults. J. Stud. Alcohol Drugs 2016, 77, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Arnett, J.J.; Žukauskienė, R.; Sugimura, K. The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. Lancet Psychiatry 2014, 1, 569–576. [Google Scholar] [CrossRef]
- Institute of Public Health. The Third National Health and Morbidity Survey (NHMS III) 2006: Psychiatry; Ministry of Health: Kuala Lumpur, Malaysia, 2008. [Google Scholar]
- Anastopoulos, A.D.; DuPaul, G.J.; Weyandt, L.L.; Morrissey-Kane, E.; Sommer, J.L.; Rhoads, L.H.; Murphy, K.R.; Gormley, M.J.; Gudmundsdottir, B.G. Rates and patterns of comorbidity among first-year college students with ADHD. J. Clin. Child Adolesc. Psychol. 2016, 47, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Graziano, P.A.; Reid, A.; Slavec, J.; Paneto, A.; McNamara, J.P.; Geffken, G.R. ADHD symptomatology and risky health, driving, and financial behaviors in college: The mediating role of sensation seeking and effortful control. J. Atten. Disord. 2014, 19, 179–190. [Google Scholar] [CrossRef]
- Snyder, J.A. The link between ADHD and the risk of sexual victimization among college women. Violence Women 2015, 21, 1364–1384. [Google Scholar] [CrossRef]
- Gray, S.A.; Fettes, P.; Woltering, S.; Mawjee, K.; Tannock, R. Symptom manifestation and impairments in college students with ADHD. J. Learn. Disabil. 2016, 49, 616–630. [Google Scholar] [CrossRef]
- O’Callaghan, P.; Sharma, D. Severity of symptoms and quality of life in medical students with ADHD. J. Atten. Disord. 2014, 18, 654–658. [Google Scholar] [CrossRef]
- Johnson, K.A.; Wiersema, J.R.; Kuntsi, J. What would Karl Popper say? Are current psychological theories of ADHD falsifiable? Behav. Brain Funct. 2009, 5, 15. [Google Scholar] [CrossRef]
- Curatolo, P.; D’Agati, E.; Moavero, R. The neurobiological basis of ADHD. Ital. J. Pediatr. 2010, 36, 79. [Google Scholar] [CrossRef]
- Willcutt, E.G.; Doyle, A.E.; Nigg, J.T.; Faraone, S.V.; Pennington, B.F. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biol. Psychiatry 2005, 57, 1336–1346. [Google Scholar] [CrossRef]
- Orban, S.A.; Rapport, M.D.; Friedman, L.M.; Kofler, M.J. Executive function/cognitive training for children with ADHD: Do results warrant the hype and cost? ADHD Rep. 2014, 22, 8–14. [Google Scholar] [CrossRef]
- Tamminga, H.G.H.; Reneman, L.; Huizenga, H.M.; Geurts, H.M. Effects of methylphenidate on executive functioning in attention-deficit/hyperactivity disorder across the lifespan: A meta-regression analysis. Psychol. Med. 2016, 46, 1791–1807. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Clinical Excellence (NICE); National Institute for Health and Care Excellence. Attention Deficit/Hyperactivity Disorder:Diagnosis and Management; NICE: London, UK, 2008; Volume 22, pp. 27–29. [Google Scholar]
- Maia, C.R.M.; Cortese, S.; Caye, A.; Deakin, T.K.; Polanczyk, G.V.; Polanczyk, C.A.; Rohde, L.A.P. Long-term efficacy of methylphenidate immediate-release for the treatment of childhood ADHD: A systematic review and meta-analysis. J. Atten. Disord. 2017, 21, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Punja, S.; Zorzela, L.; Hartling, L.; Urichuk, L.; Vohra, S. Long-acting versus short-acting methylphenidate for paediatric ADHD: A systematic review and meta-analysis of comparative efficacy. BMJ Open 2013, 3, e002312. [Google Scholar] [CrossRef] [PubMed]
- Gray, W.N.; Kavookjian, J.; Shapiro, S.K.; Wagoner, S.T.; Schaefer, M.R.; Resmini Rawlinson, A.; Hinnant, J.B. Transition to college and adherence to prescribed attention deficit hyperactivity disorder medication. J. Dev. Behav. Pediatr. 2018, 39, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Frank, E.; Ozon, C.; Nair, V.; Othee, K. Examining why patients with attention-deficit/hyperactivity disorder lack adherence to medication over the long term: A review and analysis. J. Clin. Psychiatry 2015, 76, 1459–1468. [Google Scholar] [CrossRef]
- Ministry of Health. Clinical Practice Guidelines: Management of Attention Deficit Hyperactivity Disorder in Children and Adolescents; Ministry of Health: Putrajaya, Malaysia, 2008; p. 67.
- Ministry of Health. Human Resources for Health Country Profiles 2015; Ministry of Health: Putrajaya, Malaysia, 2016; ISBN 978-967-5398-66-7.
- Yellowlees, P.M.; Hilty, D.M.; Mucic, D. Global/worldwide e-mental health: International and futuristic perspectives of telepsychiatry and the future. In E-Mental Health; Springer: Berlin/Heidelberg, Germany, 2016; pp. 233–249. [Google Scholar]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Random House Publishing Group: New York, NY, USA, 2013; ISBN 0-345-53972-9. [Google Scholar]
- Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 1982, 4, 33–47. [Google Scholar] [CrossRef]
- Fjorback, L.O.; Arendt, M.; Ørnbøl, E.; Fink, P.; Walach, H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy - a systematic review of randomized controlled trials. Acta Psychiatr. Scand. 2011, 124, 102–119. [Google Scholar] [CrossRef]
- Shonin, E.; Van Gordon, W.; Griffiths, M.D. Mindfulness-based interventions: Towards mindful clinical integration. Front. Psychol. 2013, 4, 194. [Google Scholar] [CrossRef]
- Allen, M.; Dietz, M.; Blair, K.S.; van Beek, M.; Rees, G.; Vestergaard-Poulsen, P.; Lutz, A.; Roepstorff, A. Cognitive-affective neural plasticity following active-controlled mindfulness intervention. J. Neurosci. 2012, 32, 15601–15610. [Google Scholar] [CrossRef]
- Holzel, B.K.; Lazar, S.W.; Gard, T.; Schuman-Olivier, Z.; Vago, D.R.; Ott, U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect. Psychol. Sci. 2011, 6, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Hölzel, B.K.; Ott, U.; Hempel, H.; Hackl, A.; Wolf, K.; Stark, R.; Vaitl, D. Differential engagement of anterior cingulate and adjacent medial frontal cortex in adept meditators and non-meditators. Neurosci. Lett. 2007, 421, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Janssen, L.; Kan, C.C.; Carpentier, P.J.; Sizoo, B.; Hepark, S.; Schellekens, M.P.J.; Donders, A.R.T.; Buitelaar, J.K.; Speckens, A.E.M. Mindfulness-based cognitive therapy v. treatment as usual in adults with ADHD: A multicentre, single-blind, randomised controlled trial. Psychol. Med. 2019, 49, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.-Y.; Ma, Y.; Fan, Y.; Feng, H.; Wang, J.; Feng, S.; Lu, Q.; Hu, B.; Lin, Y.; Li, J.; et al. Central and autonomic nervous system interaction is altered by short-term meditation. Proc. Natl. Acad. Sci. USA 2009, 106, 8865–8870. [Google Scholar]
- Thanissaro, P.N.; Kulupana, S. Buddhist teen worldview: Some normative background for health professionals. Contemp. Buddhism 2015, 16, 28–42. [Google Scholar] [CrossRef]
- Jankowski, T.; Holas, P. Metacognitive model of mindfulness. Conscious. Cogn. 2014, 28, 64–80. [Google Scholar] [CrossRef]
- Solem, S.; Thunes, S.S.; Hjemdal, O.; Hagen, R.; Wells, A. A metacognitive perspective on mindfulness: An empirical investigation. BMC Psychol. 2015, 3, 24. [Google Scholar] [CrossRef]
- Valk, S.L.; Bernhardt, B.C.; Trautwein, F.; Böckler, A.; Kanske, P.; Guizard, N.; Collins, D.L.; Singer, T. Structural plasticity of the social brain: Differential change after socio-affective and cognitive mental training. Sci. Adv. 2017, 3, 1–11. [Google Scholar] [CrossRef]
- Poissant, H.; Moreno, A.; Potvin, S.; Mendrek, A. A meta-analysis of mindfulness-based interventions in adults with attention-deficit hyperactivity disorder: Impact on ADHD Symptoms, depression, and executive functioning. Mindfulness 2020, 11, 2669–2681. [Google Scholar] [CrossRef]
- Malaysian Communications and Multimedia Commission. Communications and Multimedia: Pocket Book of Statistics. Malaysia, June 2019. Available online: https://www.mcmc.gov.my/skmmgovmy/media/General/pdf/Pocket-Book-C-M_2019.pdf (accessed on 9 November 2020).
- Wahbeh, H.; Svalina, M.N.; Oken, B.S. Group, one-on-one, or Internet? Preferences for mindfulness meditation delivery format and their predictors. Open Med. J. 2014, 1, 66–74. [Google Scholar] [CrossRef]
- Pettersson, R.; Söderström, S.; Edlund-Söderström, K.; Nilsson, K.W. Internet-based cognitive behavioral therapy for adults with ADHD in outpatient psychiatric care: A randomized trial. J. Atten. Disord. 2017, 21, 508–521. [Google Scholar] [CrossRef] [PubMed]
- Spijkerman, M.P.J.; Pots, W.T.M.; Bohlmeijer, E.T. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin. Psychol. Rev. 2016, 45, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Zylowska, L.; Ackerman, D.L.; Yang, M.H.; Futrell, J.L.; Horton, N.L.; Hale, T.S.; Pataki, C.; Smalley, S.L. Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. J. Atten. Disord. 2008, 11, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.T.; McIntyre, E.M.; English, J.S.; Dennis, M.F.; Beckham, J.C.; Kollins, S.H. A pilot trial of mindfulness meditation training for ADHD in adulthood: Impact on core symptoms, executive functioning, and emotion dysregulation. J. Atten. Disord. 2017, 21, 1105–1120. [Google Scholar] [CrossRef] [PubMed]
- Schoenberg, P.L.A.; Hepark, S.; Kan, C.C.; Barendregt, H.P.; Buitelaar, J.K.; Speckens, A.E.M. Effects of mindfulness-based cognitive therapy on neurophysiological correlates of performance monitoring in adult attention-deficit/hyperactivity disorder. Clin. Neurophysiol. 2014, 125, 1407–1416. [Google Scholar] [CrossRef]
- Hepark, S.; Janssen, L.; de Vries, A.; Schoenberg, P.L.A.; Donders, R.; Kan, C.C.; Speckens, A.E.M. The efficacy of adapted MBCT on core symptoms and executive functioning in adults with ADHD: A preliminary randomized controlled trial. J. Atten. Disord. 2019, 23, 351–362. [Google Scholar] [CrossRef]
- Bueno, V.F.; Kozasa, E.H.; Da Silva, M.A.; Alves, T.M.T.M.; Louza, M.R.; Pompeia, S.; Louzã, M.R.; Pompéia, S. Mindfulness meditation improves mood, quality of life, and attention in adults with attention deficit hyperactivity disorder. BioMed Res. Int. 2015, 2015, 962857. [Google Scholar] [CrossRef]
- Janssen, L.; de Vries, A.M.; Hepark, S.; Speckens, A.E.M.; Vries, A.M.D.; Hepark, S.; Speckens, A.E.M. The feasibility, effectiveness, and process of change of mindfulness-based cognitive therapy for adults with ADHD: A mixed-method pilot study. J. Atten. Disord. 2017, 24, 928–942. [Google Scholar] [CrossRef]
- Gu, Y.; Xu, G.; Zhu, Y. A randomized controlled trial of mindfulness-based cognitive therapy for college students with ADHD. J. Atten. Disord. 2018, 22, 388–399. [Google Scholar] [CrossRef]
- Edel, M.-A.M.-A.; Hölter, T.; Wassink, K.; Juckel, G. A comparison of mindfulness-based group training and skills group training in adults with ADHD: An open study. J. Atten. Disord. 2017, 21, 533–539. [Google Scholar] [CrossRef]
- Crane, R.S.; Brewer, J.; Feldman, C.; Kabat-Zinn, J.; Santorelli, S.; Williams, J.M.G.; Kuyken, W. What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 2017, 47, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Doig, G.S.; Simpson, F. Randomization and allocation concealment: A practical guide for researchers. J. Crit. Care 2005, 20, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, J.A. University students with attention deficit hyperactivity disorder (ADHD): A literature review. Ir. J. Psychol. Med. 2017, 35, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Ustun, B.; Adler, L.A.; Rudin, C.; Faraone, S.V.; Spencer, T.J.; Berglund, P.; Gruber, M.J.; Kessler, R.C. The world health organization adult attention-deficit/hyperactivity disorder self-report screening scale for DSM-5. JAMA Psychiatry 2017, 74, 520–526. [Google Scholar] [CrossRef]
- Tolin, D.F.; Gilliam, C.; Wootton, B.M.; Bowe, W.; Bragdon, L.B.; Davis, E.; Hannan, S.E.; Steinman, S.A.; Worden, B.; Hallion, L.S. Psychometric Properties of a Structured Diagnostic Interview for DSM-5 Anxiety, Mood, and Obsessive-Compulsive and Related Disorders. Assessment 2018, 25, 3–13. [Google Scholar] [CrossRef]
- Raven, J.; Rust, J.; Chan, F.; Zhou, X. Raven’s Progressive Matrices, 2nd ed.; Pearson Assessment: Bloomington, MN, USA, 2018. [Google Scholar]
- Kessler, R.C.; Adler, L.; Ames, M.; Demler, O.; Faraone, S.; Hiripi, E.; Howes, M.J.; Jin, R.; Secnik, K.; Spencer, T.; et al. The World Health Organization adult ADHD self-report scale (ASRS): A short screening scale for use in the general population. Psychol. Med. 2005, 35, 245–256. [Google Scholar] [CrossRef]
- Holst, Y.; Thorell, L.B. Adult executive functioning inventory (ADEXI): Validity, reliability, and relations to ADHD. Int. J. Methods Psychiatr. Res. 2018, 27, e1567. [Google Scholar] [CrossRef]
| Session | Outcome Variables | ||
|---|---|---|---|
| Inattention | Hyperactivity–Impulsivity | Executive Functioning | |
| Session 1: Introduction to ADHD and Mindfulness | ✓ | ✓ | ✓ |
| Session 2: ADHD through the Lens of Mindfulness | ✓ | ✓ | |
| Session 3: Thinking, Noting, and Feeling | ✓ | ✓ | ✓ |
| Session 4: Mindful Awareness of Physical Sensation | ✓ | ✓ | |
| Session 5: Mindfully Attend to Inattention | ✓ | ✓ | |
| Session 6: Time Management with Mindfulness | ✓ | ✓ | |
| Session 7: Mindful Awareness of Communication | ✓ | ✓ | |
| Session 8: Review and Future Practices | ✓ | ||
| Total Number of Sessions | 5 | 5 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pheh, K.-S.; Tan, K.-A.; Ibrahim, N.; Sidik, S.M. Effectiveness of Online Mindfulness-Based Intervention (iMBI) on Inattention, Hyperactivity–Impulsivity, and Executive Functioning in College Emerging Adults with Attention-Deficit/Hyperactivity Disorder: A Study Protocol. Int. J. Environ. Res. Public Health 2021, 18, 1257. https://doi.org/10.3390/ijerph18031257
Pheh K-S, Tan K-A, Ibrahim N, Sidik SM. Effectiveness of Online Mindfulness-Based Intervention (iMBI) on Inattention, Hyperactivity–Impulsivity, and Executive Functioning in College Emerging Adults with Attention-Deficit/Hyperactivity Disorder: A Study Protocol. International Journal of Environmental Research and Public Health. 2021; 18(3):1257. https://doi.org/10.3390/ijerph18031257
Chicago/Turabian StylePheh, Kai-Shuen, Kit-Aun Tan, Normala Ibrahim, and Sherina Mohd Sidik. 2021. "Effectiveness of Online Mindfulness-Based Intervention (iMBI) on Inattention, Hyperactivity–Impulsivity, and Executive Functioning in College Emerging Adults with Attention-Deficit/Hyperactivity Disorder: A Study Protocol" International Journal of Environmental Research and Public Health 18, no. 3: 1257. https://doi.org/10.3390/ijerph18031257
APA StylePheh, K.-S., Tan, K.-A., Ibrahim, N., & Sidik, S. M. (2021). Effectiveness of Online Mindfulness-Based Intervention (iMBI) on Inattention, Hyperactivity–Impulsivity, and Executive Functioning in College Emerging Adults with Attention-Deficit/Hyperactivity Disorder: A Study Protocol. International Journal of Environmental Research and Public Health, 18(3), 1257. https://doi.org/10.3390/ijerph18031257





