The Effect of Continuous Low-Intensity Exposure to Electromagnetic Fields from Radio Base Stations to Cancer Mortality in Brazil
Abstract
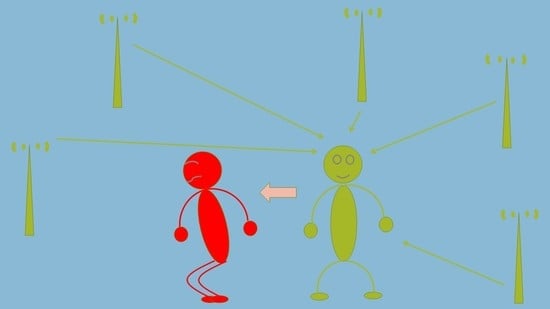
1. Background
2. Methods
3. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Electromagnetic Fields and Public Health Genebra: World Health Organization. 2006. Available online: https://www.who.int/peh-emf/publications/facts/fs304/en/ (accessed on 11 November 2019).
- ANATEL ANDT. SISTEMA DE SERVIÇOS DE TELECOMUNICAÇÕES Brasília. 2019. Available online: https://sistemas.anatel.gov.br/stel/consultas/ListaEstacoesLocalidade/tela.asp (accessed on 10 October 2019).
- WHO. Electromagnetic Fields and Public Health: Mobile Phones Genebra: WHO. 2014. Available online: https://www.who.int/en/news-room/fact-sheets/detail/electromagnetic-fields-and-public-health-mobile-phones (accessed on 11 November 2019).
- Alves, A.A.; de Almeida, M.G.; Ribeiro, M.M. Mapeamento do Posicionamento Geográfico de Estações Radio Base Do Serviço Móvel Celular Utilizando Sensoriamento Remoto Curitiba: Anais XV Simpósio Brasileiro de Sensoriamento Remoto. 2011. Available online: http://marte.sid.inpe.br/col/dpi.inpe.br/marte/2011/07.07.18.44/doc/p0333.pdf?metadatarepository=&mirror=urlib.net/www/2011/03.29.20.55 (accessed on 10 October 2019).
- DOU DOdU. Resolução nº 700, de 28 de Setembro de 2018 Brasília: Agência Nacional de Telecomunicações, ANATEL. 2018. Available online: https://www.anatel.gov.br/legislacao/en/resolucoes/2018/1161-resolucao-700 (accessed on 11 November 2019).
- IARC IAfRoC. IARC CLASSIFIES RADIOFREQUENCY ELECTROMAGNETIC FIELDS AS POSSIBLY CARCINOGENIC to HUMANS France: IARC. 2011. Available online: https://www.iarc.fr/wp-content/uploads/2018/07/pr208_E.pdf (accessed on 11 November 2019).
- Humans IWGotEoCRt. Non-ionizing radiation, Part 2: Radiofrequency electromagnetic fields. IARC Monogr. Eval. Carcinog. Risks Hum. 2013, 102 Pt 2, 1–460. [Google Scholar]
- Dode, A.C.; Leao, M.M.D.; Tejo, F.D.A.; Gomes, A.C.; Dode, D.C.; Dode, M.C.; Moreira, C.W.; Condessa, V.A.; Albinatti, C.; Caiaffa, W.T. Mortality by neoplasia and cellular telephone base stations in the Belo Horizonte municipality, Minas Gerais state, Brazil. Sci. Total Environ. 2011, 409, 3649–3665. [Google Scholar] [CrossRef] [PubMed]
- Levitt, B.B.; Lai, H. Biological effects from exposure to electromagnetic radiation emitted by cell tower base stations and other antenna arrays. Environ. Rev. 2010, 18, 369–395. [Google Scholar] [CrossRef]
- DATASUS MdS. Informações de Saúde (TABNET)—DATASUS 2020. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def (accessed on 4 April 2020).
- INCA. Estatísticas de Câncer Rio de Janeiro: Instituto Nacional do Câncer. 2020. Available online: https://www.inca.gov.br/numeros-de-cancer (accessed on 12 December 2020).
- IBGE. Instituto Brasileiro de Geografia e Estatística. 2017. Available online: http://www.ibge.gov.br/home/ (accessed on 6 June 2017).
- Dutta, S.K.; Ghosh, B.; Blackman, C. Radiofrequency radiation-induced calcium ion efflux enhancement from human and other neuroblastoma cells in culture. Bioelectromagnetics 1989, 10, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Fesenko, E.E.; Makar, V.R.; Novoselova, E.G.; Sadovnikov, V.B. Microwaves and cellular immunity. I. Effect of whole body microwave irradiation on tumor necrosis factor production in mouse cells. Bioelectrochem. Bioenergy 1999, 49, 29–35. [Google Scholar] [CrossRef]
- Magras, I.N.; Xenos, T.D. RF radiation-induced changes in the prenatal development of mice. Bioelectromagnetics 1997, 18, 455–461. [Google Scholar] [CrossRef]
- Forgács, Z.; Somosy, Z.; Kubinyi, G.; Bakos, J.; Hudák, A.; Surján, A.; Thuróczy, G. Effect of whole-body 1800MHz GSM-like microwave exposure on testicular steroidogenesis and histology in mice. Reprod. Toxicol. 2006, 22, 111–117. [Google Scholar] [CrossRef]
- Persson, B.; Salford, L.G.; Brun, A. Blood-brain barrier permeability in rats exposed to electromagnetic fields used in wireless communication. Wirel. Netw. 1997, 3, 455–461. [Google Scholar] [CrossRef]
- Phillips, J.L.; Ivaschuk, O.; Ishida-Jones, T.; Jones, R.A.; Campbell-Beachler, M.; Haggren, W. DNA damage in Molt-4 T-lymphoblastoid cells exposed to cellular telephone radiofrequency fields in vitro. Bioelectrochem. Bioenergy 1998, 45, 103–110. [Google Scholar] [CrossRef]
- Belyaev, I.Y.; Markovà, E.; Hillert, L.; Malmgren, L.O.; Persson, B.R. Microwaves from UMTS/GSM mobile phones induce long-lasting inhibition of 53BP1/gamma-H2AX DNA repair foci in human lymphocytes. Bioelectromagnetics 2009, 30, 129–141. [Google Scholar] [CrossRef]
- Kesari, K.K.; Behari, J. Fifty-gigahertz Microwave Exposure Effect of Radiations on Rat Brain. Appl. Biochem. Biotechnol. 2008, 158, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Szudziński, A.; Pietraszek, A.; Janiak, M.; Wrembel, J.; Kałczak, M.; Szmigielski, S. Acceleration of the development of benzopyrene-induced skin cancer in mice by microwave radiation. Arch. Dermatol. Res. 1982, 274, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Szmigielski, S.; Szudzinski, A.; Pietraszek, A.; Bielec, M.; Janiak, M.; Wrembel, J.K. Accelerated development of spontaneous and benzopyrene-induced skin cancer in mice exposed to 2450-MHz microwave radiation. Bioelectromagnetics 1982, 3, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Carlberg, M.; Hedendahl, L.; Koppel, T.; Hardell, L. High ambient radiofrequency radiation in Stockholm city, Sweden. Oncol. Lett. 2018, 17, 1777–1783. [Google Scholar] [CrossRef]
- Hardell, L.; Carlberg, M.; Hedendahl, L.K. Radiofrequency radiation from nearby base stations gives high levels in an apartment in Stockholm, Sweden: A case report. Oncol. Lett. 2018, 15, 7871–7883. [Google Scholar] [CrossRef]
- Koppel, T.; Ahonen, M.; Carlberg, M.; Hedendahl, L.K.; Hardell, L. Radiofrequency radiation from nearby mobile phone base stations-a case comparison of one low and one high exposure apartment. Oncol. Lett. 2019, 18, 5383–5391. [Google Scholar] [CrossRef]
- INCA. Tipos de Câncer Rio de Janeiro: Instituto Nacional do Câncer. 2019. Available online: https://www.inca.gov.br/tipos-de-cancer (accessed on 12 December 2020).
- Beniashvili, D.; Avinoach, I.; Baazov, D.; Zusman, I. Household electromagnetic fields and breast cancer in elderly women. In Vivo 2005, 19, 563–566. [Google Scholar]
- Beniashvili, D.; Avinoach’M, I.; Baasov, D.; Zusman, I. The role of household electromagnetic fields in the development of mammary tumors in women: Clinical case-record observations. Med. Sci. Monit. 2005, 11, CR10-3. [Google Scholar]
- Beniashvili, D.I.; Baazov, D.S. Ultrastructural organization of epiphysis in rats under the action of electromagnetic fields and during mammary carcinogenesi. Georgian Med. News 2005, 127, 61–64. [Google Scholar]
- Mortazavi, S.A.R.; Mortazavi, S.M.J. Women with hereditary breast cancer predispositions should avoid using their smartphones, tablets, and laptops at night. Iran. J. Basic Med. Sci. 2018, 21, 112–115. [Google Scholar]
- Meena, J.K.; Verma, A.; Kohli, C.; Ingle, G.K. Mobile phone use and possible cancer risk: Current perspectives in India. Indian J. Occup. Environ. Med. 2016, 20, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Program USNT. Cell Phone Radio Frequency Radiation: United State of American. 2019. Available online: https://www.ncbi.nlm.nih.gov/pubmed/ (accessed on 11 November 2019).
- IBGE. Pesquisa Nacional de Saúde 2019 Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; Rio de Janeiro, Brazil. 2020. Available online: https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=downloads (accessed on 12 December 2020).
- MS. PORTARIA Nº 1.220, DE 3 DE JUNHO DE 2014 Brasília: Ministério da Saúde. 2014. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2014/prt1220_03_06_2014.html (accessed on 12 December 2020).
- Filho, V.W.; Boffetta, P.; Colin, D.; Moncau, J.E. Familial cancer aggregation and the risk of lung cancer. Sao Paulo Med. J. 2002, 120, 38–44. [Google Scholar] [CrossRef] [PubMed]
- INCA. Consumo de Cigarro per Capita Rio de Janeiro: Ministério da Saúde. 2019. Available online: https://www.inca.gov.br/en/node/1421 (accessed on 4 April 2019).
- Jemal, A.; Torre, L.; Soerjomataram, I. The Cancer Atlas: American Cancer Society, 3rd ed.; 2019; Available online: https://canceratlas.cancer.org/wp-content/uploads/2019/10/ACS_CA3_Book.pdf (accessed on 12 December 2020).
- Yang, X.; Ni, Y.; Yuan, Z.; Chen, H.; Plymoth, A.; Jin, L.; Chen, X.; Lu, M.; Ye, W. Very hot tea drinking increases esophageal squamous cell carcinoma risk in a high-risk area of China: A population-based case-control study. Clin. Epidemiol. 2018, 10, 1307–1320. [Google Scholar] [CrossRef] [PubMed]
- Holmes, R.S.; Vaughan, T.L. Epidemiology and Pathogenesis of Esophageal Cancer. Semin. Radiat. Oncol. 2007, 17, 2–9. [Google Scholar] [CrossRef]
- Pinho, V.F.; Coutinho, E.S. Risk factors for breast cancer: A systematic review of studies with female samples among the general population in Brazil. Cad. Saude Publica 2005, 21, 351–360. [Google Scholar] [CrossRef]
- CDC CfDCaP. Breast Cancer Washington: U.S. Department of Health & Human Services. 2018. Available online: https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm (accessed on 4 April 2019).
- Lima, C.A.; Palmeira, J.A.V.; Cipolotti, R. Fatores associados ao câncer do colo uterino em Propriá, Sergipe, Brasil. Cad. Saúde Pública 2006, 22, 2151–2156. [Google Scholar] [CrossRef]
- Panis, C.; Kawasaki, A.C.B.; Pascotto, C.R.; Justina, E.Y.D.; Vicentini, G.E.; Lucio, L.C.; Prates, R.T.C. Critical review of cancer mortality using hospital records and potential years of life lost. Einstein 2018, 16, eAO4018. [Google Scholar] [CrossRef]
- das Neves, F.J.; Mattos, I.E.; Koifman, R.J. Colon and rectal cancer mortality in Brazilian capitals, 1980–1997. Arq. Gastroenterol. 2005, 42, 63–70. [Google Scholar]
- Ferreira, F.R.; Nascimento, L.F.C. Mortality due to cutaneous melanoma in south region of Brazil: A spatial approach*. An. Bras. Dermatol. 2016, 91, 437–441. [Google Scholar] [CrossRef]
- França, E.B.; Passos, V.M.A.; Malta, D.C.; Duncan, B.B.; Ribeiro, A.L.P.; Guimarães, M.D.C.; Abreu, D.M.X.; Vasconcelos, A.M.N.; Carneiro, M.; Teixeira, R.; et al. Cause-specific mortality for 249 causes in Brazil and states during 1990-2015: A systematic analysis for the global burden of disease study 2015. Popul. Health Metr. 2017, 15, 39. [Google Scholar] [CrossRef]
- Guerra, M.R.; Bustamante-Teixeira, M.T.; Corrêa, C.S.L.; Abreu, D.M.X.; Curado, M.P.; Mooney, M.; Naghavi, M.; Teixeira, R.; França, E.B.; Malta, D.C. Magnitude and variation of the burden of cancer mortality in Brazil and Federation Units, 1990 and 2015. Rev. Bras. Epidemiol. 2017, 20, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Dela Cruz, C.S.; Tanoue, L.T.; Matthay, R.A. Lung cancer: Epidemiology, etiology, and prevention. Clin. Chest. Med. 2011, 32, 605–644. [Google Scholar] [CrossRef] [PubMed]
- de Groot, P.M.; Wu, C.C.; Carter, B.W.; Munden, R.F. The epidemiology of lung cancer. Transl. Lung Cancer Res. 2018, 7, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Barta, J.A.; Powell, C.A.; Wisnivesky, J.P. Global Epidemiology of Lung Cancer. Ann. Glob. Health 2019, 85, 8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y. Epidemiology of esophageal cancer. World J. Gastroenterol. 2013, 19, 5598–5606. [Google Scholar] [CrossRef] [PubMed]
- Asombang, A.W.; Chishinga, N.; Nkhoma, A.; Chipaila, J.; Nsokolo, B.; Manda-Mapalo, M.; Montiero, J.F.G.; Banda, L.; Dua, K.S. Systematic review and meta-analysis of esophageal cancer in Africa: Epidemiology, risk factors, management and outcomes. World J. Gastroenterol. 2019, 25, 4512–4533. [Google Scholar] [CrossRef]
- Araújo, A.R. Boletim UFMG: Radiações Perigosas: Universidade Federal de Belo Horizonte. 2010. Available online: https://www.ufmg.br/online/arquivos/anexos/Bol%201689_pag_centrais.pdf (accessed on 1 January 2020).
- Hare, E. RF Exposure and You, 1st ed.; The American Radio Relay League: Newington, CT, USA, 1998. [Google Scholar]
- MRE MdRE. Engenharia: Elétrica—Segurança—Ambiental Belo Horizonte. 2020. Available online: http://www.mreengenharia.com.br/ (accessed on 1 January 2020).
- de Sousa, A.M.V.; Teixeira, C.C.A.; da Silva Medeiros, S.; Nunes, S.J.C.; de Oliveira Salvador, P.T.C.; de Barros, R.M.B.; de Lima, F.F.S.; do Nascimento, G.G.C.; dos Santos, J.; de Souza, D.L.B.; et al. Mortalidade por câncer do colo do útero no estado do Rio Grande do Norte, no período de 1996 a 2010: Tendência temporal e projeções até 2030. Epidemiol. Serviços Saúde 2016, 25, 311–322. [Google Scholar]
- Carvalho, J.B.; Paes, N.A. Taxas de mortalidade por câncer corrigidas para os idosos dos estados do Nordeste brasileiro. Ciência Saúde Coletiva 2019, 24, 3857–3866. [Google Scholar] [CrossRef]

| Breast | Cervix | Lung | Esophagus | All Cancers | |
|---|---|---|---|---|---|
| Median/105 (IQR) | Median/105 (IQR) | Median/105 (IQR) | Median/105 (IQR) | Median/105 (IQR) | |
| RBS-sign | * | * | * | * | * |
| ≤500 | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 7.30 (44.94) |
| 501–1000 | 1.16 (27.11) | 2.74 (26.30) | 0.00 (38.97) | 0.00 (0.00) | 26.32 (382.14) |
| 1001–2000 | 20.12 (54.53) | 7.38 (25.79) | 4.47 (63.42) | 0.00 (8.74) | 71.95 (500.43) |
| >2000 | 27.33 (63.06) | 9.56 (16.43) | 9.58 (76.46) | 1.62 (14.21) | 111.68 (552.78) |
| Sex-sign | * | * | * | ||
| Female | 3.77 (46.88) | 0.00 (3.17) | 75.31 (360.87) | ||
| Male | 4.31 (98.82) | 0.45 (22.06) | 56.49 (540.97) | ||
| Age group-sign | * | * | * | * | * |
| <30 | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 5.75 (4.53) |
| 30–49 | 9.89 (13.56) | 6.75 (7.31) | 1.81 (4.39) | 0.00 (1.13) | 38.59 (44.90) |
| 50–69 | 43.43 (20.19) | 15.02 (14.71) | 34.08 (42.50) | 6.75 (16.28) | 258.79 (240.76) |
| ≥60 | 91.18 (64.51) | 27.35 (37.02) | 159.40 (159.63) | 20.31 (39.68) | 1178.11 (1012.72) |
| Year-sign | NS | NS | NS | NS | NS |
| 2010–2011 | 16.95 (52.66) | 6.29 (19.36) | 4.44 (64.91) | 0.00 (8.87) | 68.76 (508.70) |
| 2012–2013 | 15.98 (56.94) | 6.42 (19.09) | 4.13 (66.30) | 0.00 (10.29) | 65.09 (501.19) |
| 2014–2015 | 17.36 (56.05) | 8.29 (19.52) | 4.13 (65.15) | 0.00 (9.54) | 65.56 (491.10) |
| 2016–2017 | 18.01 (52.08) | 7.62 (16.66) | 3.54 (65.52) | 0.00 (8.22) | 61.87 (444.41) |
| Breast | Cervix | Lung | Esophagus | All Cancers | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | Sign | RR | Sign | RR | Sign | RR | Sign | RR | Sign | |
| Fixed effects | ||||||||||
| Log RBS | 1.25 | *** | 2.18 | *** | 1.14 | *** | 1.18 | ** | 1.15 | *** |
| Sex | ||||||||||
| Female | 1.00 | 1.00 | 1.00 | |||||||
| Male | 1.97 | *** | 4.88 | *** | 1.42 | *** | ||||
| Age group | ||||||||||
| <30 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 30–49 | 37.59 | *** | 13.82 | *** | 20.11 | *** | 73.84 | *** | 6.06 | *** |
| 50–69 | 132.29 | *** | 30.74 | *** | 323.80 | *** | 876.50 | *** | 40.73 | *** |
| ≥60 | 297.55 | *** | 53.88 | *** | 1250.63 | *** | 2154.44 | *** | 164.61 | *** |
| Year | ||||||||||
| 2010–2011 | 1.00 | 1.00 | 1.00 | 0.00 | 1.00 | |||||
| 2012–2013 | 0.97 | NS | 0.78 | *** | 0.97 | NS | 0.96 | NS | 0.98 | * |
| 2014–2015 | 0.96 | NS | 0.62 | *** | 0.93 | ** | 0.88 | *** | 0.95 | *** |
| 2016–2017 | 0.81 | ** | 0.46 | *** | 0.84 | *** | 0.76 | *** | 0.84 | *** |
| Random effects | ||||||||||
| Std Dev | Std Dev | Std Dev | Std Dev | |||||||
| Capital (intercept) | 0.61 | *** | 1.55 | *** | 0.19 | *** | 0.86 | *** | 0.28 | *** |
| Sqrt GDP (slope) | 0.00 | *** | 0.01 | *** | 0.00 | *** | 0.00 | *** | 0.00 | *** |
| Area/Km2 (slope) | 0.00 | NS | 0.00 | NS | 0.00 | NS | 0.00 | * | 0.00 | NS |
| Deviance | 12274 | 8345 | 24732 | 10364 | 100918 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, N.C.P.; Dode, A.C.; de Noronha Andrade, M.K.; O’Dwyer, G.; Monteiro, D.L.M.; Reis, I.N.C.; Rodrigues, R.P.; Frossard, V.C.; Lino, V.T.S. The Effect of Continuous Low-Intensity Exposure to Electromagnetic Fields from Radio Base Stations to Cancer Mortality in Brazil. Int. J. Environ. Res. Public Health 2021, 18, 1229. https://doi.org/10.3390/ijerph18031229
Rodrigues NCP, Dode AC, de Noronha Andrade MK, O’Dwyer G, Monteiro DLM, Reis INC, Rodrigues RP, Frossard VC, Lino VTS. The Effect of Continuous Low-Intensity Exposure to Electromagnetic Fields from Radio Base Stations to Cancer Mortality in Brazil. International Journal of Environmental Research and Public Health. 2021; 18(3):1229. https://doi.org/10.3390/ijerph18031229
Chicago/Turabian StyleRodrigues, Nádia Cristina Pinheiro, Adilza Condessa Dode, Mônica Kramer de Noronha Andrade, Gisele O’Dwyer, Denise Leite Maia Monteiro, Inês Nascimento Carvalho Reis, Roberto Pinheiro Rodrigues, Vera Cecília Frossard, and Valéria Teresa Saraiva Lino. 2021. "The Effect of Continuous Low-Intensity Exposure to Electromagnetic Fields from Radio Base Stations to Cancer Mortality in Brazil" International Journal of Environmental Research and Public Health 18, no. 3: 1229. https://doi.org/10.3390/ijerph18031229
APA StyleRodrigues, N. C. P., Dode, A. C., de Noronha Andrade, M. K., O’Dwyer, G., Monteiro, D. L. M., Reis, I. N. C., Rodrigues, R. P., Frossard, V. C., & Lino, V. T. S. (2021). The Effect of Continuous Low-Intensity Exposure to Electromagnetic Fields from Radio Base Stations to Cancer Mortality in Brazil. International Journal of Environmental Research and Public Health, 18(3), 1229. https://doi.org/10.3390/ijerph18031229