Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Ethical Approval
2.4. Sample Size and Sampling
2.5. Sampling Procedure
2.6. Data Collection
2.7. Assessment of Overweight/Obesity
2.8. Diagnosis of Type 2 Diabetes Mellitus (T2D)
2.9. Measurement and Definition of Blood Pressure
2.10. Socioeconomic and Environmental Variables
2.11. Data Analysis
3. Results
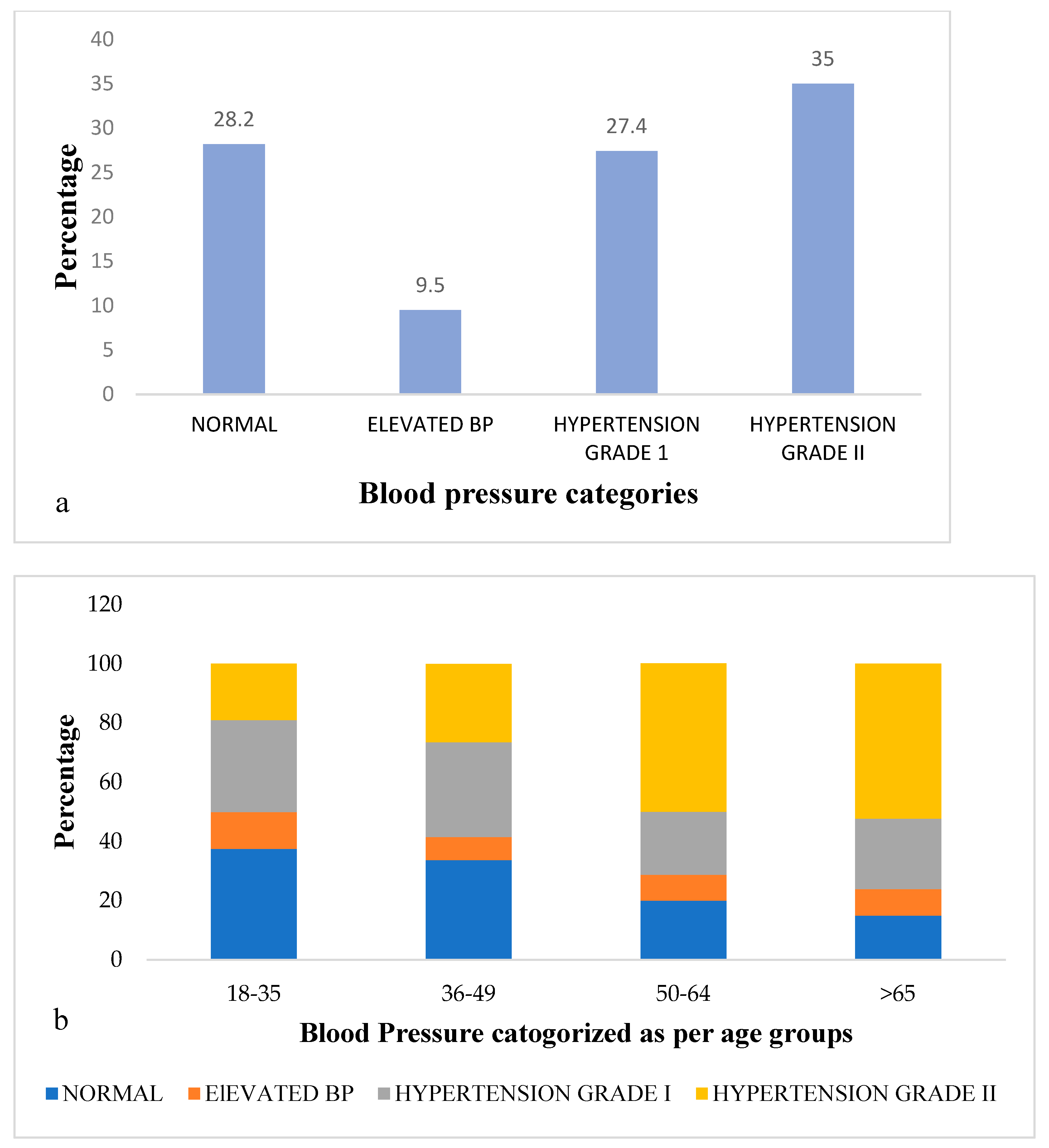
3.1. Participant’s Sociodemographic and Clinical Characteristics and Levels of Blood Pres
3.2. Potential Variables Affecting Treatment Status of Hypertension
4. Discussion
5. Conclusions
Strengths and Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ibrahim, M.M.; Damasceno, A. Hypertension in developing countries. Lancet 2012, 380, 611–619. [Google Scholar] [CrossRef]
- 2. Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Opie, L.H.; Seedat, Y.K. Hypertension in sub-Saharan African populations. Circulation 2005, 112, 3562–3568. [Google Scholar] [CrossRef]
- Gómez-Olivé, F.X.; Ali, S.A.; Made, F.; Kyobutungi, C.; Nonterah, E.; Micklesfield, L.; Alberts, M.; Boua, R.; Hazelhurst, S.; Debpuur, C.; et al. Regional and sex differences in the prevalence and awareness of hypertension: An H3Africa AWI-Gen study across 6 sites in sub-Saharan Africa. Glob. Heart 2017, 12, 81–90. [Google Scholar] [CrossRef]
- Guwatudde, D.; Nankya-Mutyoba, J.; Kalyesubula, R.; Laurence, C.; Adebamowo, C.; Ajayi, I.; Bajunirwe, F.; Njelekela, M.; Chiwanga, F.S.; Reid, T.; et al. The burden of hypertension in sub-Saharan Africa: A four-country cross sectional study. BMC Public Health 2015, 15, 1211. [Google Scholar] [CrossRef]
- Addo, J.; Smeeth, L.; Leon, D.A. Hypertension in sub-saharan Africa: A systematic review. Hypertension 2007, 50, 1012–1018. [Google Scholar] [CrossRef]
- Adeniyi, O.V.; Yogeswaran, P.; Longo-Mbenza, B.; Goon, D.T. Uncontrolled hypertension and its determinants in patients with concomitant type 2 diabetes mellitus (T2DM) in rural South Africa. PLoS ONE 2016, 11, e0150033. [Google Scholar] [CrossRef]
- Damasceno, A.; Azevedo, A.; Silva-Matos, C.; Prista, A.; Diogo, D.; Lunet, N. Hypertension prevalence, awareness, treatment, and control in Mozambique: Urban/rural gap during epidemiological transition. Hypertension 2009, 54, 77–83. [Google Scholar] [CrossRef]
- De Munter, J.S.; Hu, F.B.; Spiegelman, D.; Franz, M.; van Dam, R.M. Whole grain, bran, and germ intake and risk of type 2 diabetes: A prospective cohort study and systematic review. PLoS Med. 2007, 4, e261. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Abahussain, N.A.; Al-Sobayel, H.I.; Qahwaji, D.M.; Musaiger, A.O. Lifestyle factors associated with overweight and obesity among Saudi adolescents. BMC Public Health 2012, 12, 354. [Google Scholar] [CrossRef]
- MacMahon, S.; Alderman, M.H.; Lindholm, L.H.; Liu, L.; Sanchez, R.A.; Seedat, Y.K. Blood-Pressure-Related Disease is a Global Health Priority; Oxford University Press: Oxford, NY, USA, 2008. [Google Scholar]
- Schneider, M.; Bradshaw, D.; Steyn, K.; Norman, R.; Laubscher, R. Poverty and non-communicable diseases in South Africa. Scand. J. Public Health 2009, 37, 176–186. [Google Scholar] [CrossRef]
- Peltzer, K.; Phaswana-Mafuya, N. Hypertension and associated factors in older adults in South Africa. Cardiovasc. J. Afr. 2013, 24, 66. [Google Scholar] [CrossRef]
- Lissner, L.; Wijnhoven, T.; Mehlig, K.; Sjöberg, A.; Kunesova, M.; Yngve, A.; Petrauskiene, A.; Duleva, V.; Rito, A.I.; Breda, J. Socioeconomic inequalities in childhood overweight: Heterogeneity across five countries in the WHO European Childhood Obesity Surveillance Initiative (COSI–2008). Int. J. Obes. 2016, 40, 796–802. [Google Scholar] [CrossRef]
- Longo-Mbenza, B.; Luila, E.L.; M’Buyamba-Kabangu, J. Nutritional status, socio-economic status, heart rate, and blood pressure in African school children and adolescents. Int. J. Cardiol. 2007, 121, 171–177. [Google Scholar] [CrossRef]
- Griffiths, P.L.; Sheppard, Z.A.; Johnson, W.; Cameron, N.; Pettifor, J.M.; Norris, S.A. Associations between household and neighbourhood socioeconomic status and systolic blood pressure among urban South African adolescents. J. Biosoc. Sci. 2012, 44, 433–458. [Google Scholar] [CrossRef][Green Version]
- Afrifa–Anane, E.; Agyemang, C.; Codjoe, S.N.A.; Ogedegbe, G.; Aikins, A.D.-G. The association of physical activity, body mass index and the blood pressure levels among urban poor youth in Accra, Ghana. BMC Public Health 2015, 15, 269. [Google Scholar] [CrossRef][Green Version]
- Hu, G.; Barengo, N.C.; Tuomilehto, J.; Lakka, T.A.; Nissinen, A.; Jousilahti, P. Relationship of physical activity and body mass index to the risk of hypertension: A prospective study in Finland. Hypertension 2004, 43, 25–30. [Google Scholar] [CrossRef]
- Juraschek, S.P.; Blaha, M.J.; Whelton, S.P.; Blumenthal, R.; Jones, S.R.; Keteyian, S.J.; Schairer, J.; Brawner, C.A.; Al-Mallah, M.H. Physical fitness and hypertension in a population at risk for cardiovascular disease: The Henry Ford ExercIse Testing (FIT) project. J. Am. Heart Assoc. 2014, 3, e001268. [Google Scholar] [CrossRef]
- Väistö, J.; Eloranta, A.-M.; Viitasalo, A.; Tompuri, T.; Lintu, N.; Karjalainen, P.; Lampinen, E.-K.; Ågren, J.; Laaksonen, D.E.; Lakka, H.-M.; et al. Physical activity and sedentary behaviour in relation to cardiometabolic risk in children: Cross-sectional findings from the Physical Activity and Nutrition in Children (PANIC) study. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 55. [Google Scholar] [CrossRef]
- Al-Goblan, A.S.; Al-Alfi, M.A.; Khan, M.Z. Mechanism linking diabetes mellitus and obesity. Diabetes Metab. Syndr. Obes. Targets Ther. 2014, 7, 587. [Google Scholar] [CrossRef]
- Goran, M.I.; Ball, G.D.; Cruz, M.L. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J. Clin. Endocrinol. Metab. 2003, 88, 1417–1427. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Godman, B.; Basu, D.; Pillay, Y.; Mwita, J.C.; Rwegerera, G.M.; Paramadhas, B.D.A.; Tiroyakgosi, C.; Okwen, P.M.; Niba, L.L.; Nonvignon, J.; et al. Review of ongoing activities and challenges to improve the care of patients with type 2 diabetes across Africa and the implications for the future. Front. Pharmacol. 2020, 11. [Google Scholar] [CrossRef]
- Mbanya, J.C.N.; Motala, A.A.; Sobngwi, E.; Assah, F.K.; Enoru, S.T. Diabetes in sub-saharan africa. Lancet 2010, 375, 2254–2266. [Google Scholar] [CrossRef]
- Cois, A.; Ehrlich, R. Analysing the socioeconomic determinants of hypertension in South Africa: A structural equation modelling approach. BMC Public Health 2014, 14, 414. [Google Scholar] [CrossRef]
- Ataklte, F.; Erqou, S.; Kaptoge, S.; Taye, B.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Burden of undiagnosed hypertension in sub-saharan Africa: A systematic review and meta-analysis. Hypertension 2015, 65, 291–298. [Google Scholar] [CrossRef]
- Adebolu, F.A.; Naidoo, M. Blood pressure control amongst patients living with hypertension presenting to an urban district hospital outpatient clinic in Kwazulu-Natal. Afr. J. Prim. Health Care Fam. Med. 2014, 6, 1–6. [Google Scholar] [CrossRef]
- Dennison, C.R.; Peer, N.; Steyn, K.; Levitt, N.S.; Hill, M.N. Determinants of hypertension care and control among peri-urban Black South Africans: The HiHi study. Ethn. Dis. 2007, 17, 484–491. [Google Scholar]
- Duncan, P.; Howe, L.; Manakusa, Z.; Purdy, S. Determinants of blood pressure control in rural KwaZulu-Natal, South Africa. South Afr. Fam. Pract. 2014, 56, 297–304. [Google Scholar] [CrossRef][Green Version]
- Remais, J.V.; Zeng, G.; Li, G.; Tian, L.; Engelgau, M.M. Convergence of non-communicable and infectious diseases in low-and middle-income countries. Int. J. Epidemiol. 2013, 42, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Stuckler, D.; Basu, S.; McKee, M. Health care capacity and allocations among South Africa’s provinces: Infrastructure–inequality traps after the end of apartheid. Am. J. Public Health 2011, 101, 165–172. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki. Recommendations Guiding Medical Doctors in Biomedical Research Involving Human Subjects; World Medical Association: Ferney-Voltaire, France, 1975. [Google Scholar]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- World Health Organization. WHO Consultation on Obesity. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000; pp. 1–253. [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes-2020 abridged for primary care providers. Clin. Diabetes Publ. Am. Diabetes Assoc. 2020, 38, 10. [Google Scholar]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Uranga, J.A.; López-Miranda, V.; Lombó, F.; Abalo, R. Food, nutrients and nutraceuticals affecting the course of inflammatory bowel disease. Pharmacol. Rep. 2016, 68, 816–826. [Google Scholar] [CrossRef]
- Monakali, S.; Goon, D.T.; Seekoe, E.; Owolabi, E.O. Prevalence, awareness, control and determinants of hypertension among primary health care professional nurses in Eastern Cape, South Africa. Afr. J. Prim. Health Care Fam. Med. 2018, 10, 1–5. [Google Scholar] [CrossRef]
- Masilela, C.; Pierce, B.; Adeniyi, O.V.; Benjeddou, M. Cross-sectional study of prevalence and determinants of uncontrolled Hypertension among South African adult residents of Mkhondo municipality. BMC Public Health 2020, 20, 1069. [Google Scholar] [CrossRef]
- Department of Health SAMRC. South Africa Demographic and Health Survey 2016: Key Indicator Report; Statistics South Africa: Pretoria, South Africa, 2017. [Google Scholar]
- Cooper, R.; Rotimi, C.; Ataman, S.; McGee, D.; Osotimehin, B.; Kadiri, S.; Muna, W.; Kingue, S.; Fraser, H.; Forrester, T.; et al. The prevalence of hypertension in seven populations of west African origin. Am. J. Public Health 1997, 87, 160–168. [Google Scholar] [CrossRef]
- Agyemang, C. Rural and urban differences in blood pressure and hypertension in Ghana, West Africa. Public Health 2006, 120, 525–533. [Google Scholar] [CrossRef]
- Weimann, A.; Dai, D.; Oni, T. A cross-sectional and spatial analysis of the prevalence of multimorbidity and its association with socioeconomic disadvantage in South Africa: A comparison between 2008 and 2012. Soc. Sci. Med. 2016, 163, 144–156. [Google Scholar] [CrossRef] [PubMed]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. The South African National Health and Nutrition Examination Survey, 2012: SANHANES-1: The Health and Nutritional Status of the Nation; Human Sciences Research Council: Cape Town, South Africa, 2014. [Google Scholar]
- Kandala, N.-B.; Tigbe, W.; Manda, S.O.; Stranges, S. Geographic variation of hypertension in Sub-Saharan Africa: A case study of South Africa. Am. J. Hypertens. 2013, 26, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Jardim, T.V.; Reiger, S.; Abrahams-Gessel, S.; Gomez-Olive, F.X.; Wagner, R.G.; Wade, A.; Bärnighausen, T.W.; Salomon, J.; Tollman, S.; Gaziano, T.A. Hypertension management in a population of older adults in rural South Africa. J. Hypertens. 2017, 35, 1283. [Google Scholar] [CrossRef] [PubMed]
- Bosu, W.K.; Reilly, S.T.; Aheto, J.M.K.; Zucchelli, E. Hypertension in older adults in Africa: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0214934. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Micah, F.B.; Emmett, L.; Kerry, S.M.; Antwi, S.; Martin-Peprah, R.; Phillips, R.O.; Plange-Rhule, J.; Eastwood, J.B. Prevalence, detection, management, and control of hypertension in Ashanti, West Africa. Hypertension 2004, 43, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- De Ramirez, S.S.; Enquobahrie, D.; Nyadzi, G.; Mjungu, D.; Magombo, F.; Ramirez, M.; Sachs, S.E.; Willett, W. Prevalence and correlates of hypertension: A cross-sectional study among rural populations in sub-Saharan Africa. J. Hum. Hypertens. 2010, 24, 786–795. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef]
- Joffres, M.; Falaschetti, E.; Gillespie, C.; Robitaille, C.; Loustalot, F.; Poulter, N.; McAlister, F.A.; Johansen, H.; Baclic, O.; Campbell, N. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: A cross-sectional study. BMJ Open 2013, 3. [Google Scholar] [CrossRef]
- Ibrahim, M.M. Hypertension in developing countries: A major challenge for the future. Curr. Hypertens. Rep. 2018, 20, 38. [Google Scholar] [CrossRef]
- Wandai, M.E.; Norris, S.A.; Aagaard-Hansen, J.; Manda, S.O. Geographical influence on the distribution of the prevalence of hypertension in South Africa: A multilevel analysis. Cardiovasc. J. Afr. 2020, 31, 47–54. [Google Scholar] [CrossRef]
- Kotwani, P.; Kwarisiima, D.; Clark, T.D.; Kabami, J.; Geng, E.H.; Jain, V.; Chamie, G.; Petersen, M.L.; Thirumurthy, H.; Kamya, M.R.; et al. Epidemiology and awareness of hypertension in a rural Ugandan community: A cross-sectional study. BMC Public Health 2013, 13, 1151. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, E.O.; Ter Goon, D.; Adeniyi, O.V.; Seekoe, E. Social epidemiology of hypertension in Buffalo City Metropolitan Municipality (BCMM): Cross-sectional study of determinants of prevalence, awareness, treatment and control among South African adults. BMJ Open 2017, 7, e014349. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dalal, S.; Beunza, J.J.; Volmink, J.; Adebamowo, C.; Bajunirwe, F.; Njelekela, M.; Mozaffarian, D.; Fawzi, W.; Willett, W.; Adami, H.O.; et al. Non-communicable diseases in sub-Saharan Africa: What we know now. Int. J. Epidemiol. 2011, 40, 885–901. [Google Scholar] [CrossRef] [PubMed]
- Thorogood, M.; Connor, M.; Tollman, S.; Hundt, G.L.; Fowkes, G.; Marsh, J. A cross-sectional study of vascular risk factors in a rural South African population: Data from the Southern African Stroke Prevention Initiative (SASPI). BMC Public Health 2007, 7, 326. [Google Scholar] [CrossRef] [PubMed]
- Mosha, N.R.; Mahande, M.; Juma, A.; Mboya, I.; Peck, R.; Urassa, M.; Michael, D.; Todd, J. Prevalence, awareness and factors associated with hypertension in North West Tanzania. Glob. Health Action 2017, 10, 1321279. [Google Scholar] [CrossRef]
- Alberts, M.; Urdal, P.; Steyn, K.; Stensvold, I.; Tverdal, A.; Nel, J.H.; Steyn, N.P. Prevalence of cardiovascular diseases and associated risk factors in a rural black population of South Africa. Eur. J. Cardiovasc. Prev. Rehabil. 2005, 12, 347–354. [Google Scholar] [CrossRef]
- Mkhonto, S.S.; Labadarios, D.; Mabaso, M.L. Association of body weight and physical activity with blood pressure in a rural population in the Dikgale village of Limpopo Province in South Africa. BMC Res. Notes 2012, 5, 118. [Google Scholar] [CrossRef][Green Version]
- Nshisso, L.D.; Reese, A.; Gelaye, B.; Lemma, S.; Berhane, Y.; Williams, M.A. Prevalence of hypertension and diabetes among Ethiopian adults. Diabetes Metab. Syndr. Clin. Res. Rev. 2012, 6, 36–41. [Google Scholar] [CrossRef][Green Version]
- Lionakis, N.; Mendrinos, D.; Sanidas, E.; Favatas, G.; Georgopoulou, M. Hypertension in the elderly. World J. Cardiol. 2012, 4, 135. [Google Scholar] [CrossRef]
- Pickering, T.G.; Hall, J.E.; Appel, L.J.; Falkner, B.E.; Graves, J.; Hill, M.N.; Kurtz, T.; Sheps, S.G.; Roccella, E.J. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on high blood pressure research. Hypertension 2005, 45, 142–161. [Google Scholar]
- Darnton-Hill, I.; Nishida, C.; James, W. A life course approach to diet, nutrition and the prevention of chronic diseases. Public Health Nutr. 2004, 7, 101–121. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Lurie, M.N.; Bärnighausen, T.; McGarvey, S.T.; Newell, M.-L.; Tanser, F. Determinants and spatial patterns of adult overweight and hypertension in a high HIV prevalence rural South African population. Health Place 2012, 18, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- Mashiane, J.T.; Monyeki, K.D.; Kengne, A.P.; Rosina, N.M.; Monyeki, M.S. Ellisras longitudinal study 2017: The relationship between dietary intake and body mass index among young rural adults in South Africa aged 18 to 30 years (ELS 18). South Afr. J. Diabetes Vasc. Dis. 2019, 16, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Foulds, H.J.; Bredin, S.S.; Warburton, D.E. The relationship between hypertension and obesity across different ethnicities. J. Hypertens. 2012, 30, 359–367. [Google Scholar] [CrossRef]
- Gorzelniak, K.; Engeli, S.; Janke, J.; Luft, F.C.; Sharma, A.M. Hormonal regulation of the human adipose-tissue renin–angiotensin system: Relationship to obesity and hypertension. J. Hypertens. 2002, 20, 965–973. [Google Scholar] [CrossRef]
- Redón, J.; Cea-Calvo, L.; Moreno, B.; Monereo, S.; Gil-Guillén, V.; Lozano, J.V.; Martí-Canales, J.C.; Llisterri, J.L.; Aznar, J.; Christina, F.P. Independent impact of obesity and fat distribution in hypertension prevalence and control in the elderly. J. Hypertens. 2008, 26, 1757–1764. [Google Scholar] [CrossRef]
- Rudatsikira, E.; Muula, A.S.; Mulenga, D.; Siziya, S. Prevalence and correlates of obesity among Lusaka residents, Zambia: A population-based survey. Int. Arch. Med. 2012, 5, 1–6. [Google Scholar] [CrossRef]
- Cheung, B.M.; Li, C. Diabetes and hypertension: Is there a common metabolic pathway? Curr. Atheroscler. Rep. 2012, 14, 160–166. [Google Scholar] [CrossRef]
- Landsberg, L.; Molitch, M. Diabetes and hypertension: Pathogenesis, prevention and treatment. Clin. Exp. Hypertens. 2004, 26, 621–628. [Google Scholar] [CrossRef]
- Shukla, A.; Kumar, K.; Singh, A. Association between obesity and selected morbidities: A study of BRICS countries. PLoS ONE 2014, 9, e94433. [Google Scholar] [CrossRef]
- Alaba, O.; Chola, L. Socioeconomic inequalities in adult obesity prevalence in South Africa: A decomposition analysis. Int. J. Environ. Res. Public Health 2014, 11, 3387–3406. [Google Scholar] [CrossRef] [PubMed]
- Alwan, A. Global Status Report on Noncommunicable Diseases 2010; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Kruger, H.S.; Puoane, T.; Senekal, M.; van der Merwe, M.-T. Obesity in South Africa: Challenges for government and health professionals. Public Health Nutr. 2005, 8, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.K.; Kliewer, W.; Plybon, L.; Sica, D.A. Socioeconomic status and blood pressure reactivity in healthy black adolescents. Hypertension 2000, 35, 496–500. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kagura, J.; Adair, L.S.; Pisa, P.T.; Griffiths, P.L.; Pettifor, J.M.; Norris, S.A. Association of socioeconomic status change between infancy and adolescence, and blood pressure, in South African young adults: Birth to Twenty Cohort. BMJ Open 2016, 6, e008805. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, M.; Nunes, A. The psychosocial determinants of hypertension. Nutr. Metab. Cardiovasc. Dis. 2003, 13, 52–59. [Google Scholar] [CrossRef]
- Bell, A.C.; Adair, L.S.; Popkin, B.M. Understanding the role of mediating risk factors and proxy effects in the association between socio-economic status and untreated hypertension. Soc. Sci. Med. 2004, 59, 275–283. [Google Scholar] [CrossRef]
- Cozier, Y.; Palmer, J.; Horton, N.; Fredman, L.; Rosenberg, L. Neighborhood socioeconomic status and the incidence of hypertension in the black women’s health study. Ann. Epidemiol. 2004, 14, 599. [Google Scholar] [CrossRef]
- Steyn, K.; Kazenellenbogen, J.M.; Lombard, C.J.; Bourne, L.T. Urbanization and the risk for chronic diseases of lifestyle in the black population of the Cape Peninsula, South Africa. J. Cardiovasc. Risk 1997, 4, 135–142. [Google Scholar] [CrossRef]
- Poti, J.M.; Braga, B.; Qin, B. Ultra-processed food intake and obesity: What really matters for health—Processing or nutrient content? Curr. Obes. Rep. 2017, 6, 420–431. [Google Scholar] [CrossRef]
- Mayén, A.-L.; Bovet, P.; Marti-Soler, H.; Viswanathan, B.; Gedeon, J.; Paccaud, F.; Marques-Vidal, P.; Stringhini, S. Socioeconomic differences in dietary patterns in an East African Country: Evidence from the Republic of Seychelles. PLoS ONE 2016, 11, e0155617. [Google Scholar] [CrossRef]
- Benkeser, R.; Biritwum, R.; Hill, A. Prevalence of overweight and obesity and perception of healthy and desirable body size in urban, Ghanaian women. Ghana Med. J. 2012, 46, 66–75. [Google Scholar] [PubMed]
- Levitt, N.S. Diabetes in Africa: Epidemiology, management and healthcare challenges. Heart 2008, 94, 1376–1382. [Google Scholar] [CrossRef] [PubMed]
- Abubakari, A.-R.; Lauder, W.; Jones, M.; Kirk, A.; Agyemang, C.; Bhopal, R. Prevalence and time trends in diabetes and physical inactivity among adult West African populations: The epidemic has arrived. Public Health 2009, 123, 602–614. [Google Scholar] [CrossRef] [PubMed]
- Muyer, M.T.; Muls, E.; Mapatano, M.A.; Makulo, R.; Mvitu, M.; Kimenyembo, W.; Mandja, M.; Kimbondo, P.; Bieleli, E.; Kaïmbo, D.K.W.; et al. Estimating prevalence of diabetes in a Congolese town was feasible. J. Clin. Epidemiol. 2011, 64, 172–181. [Google Scholar] [CrossRef]
- Adeniyi, O.V.; Longo-Mbenza, B.; Ter Goon, D. Female sex, poverty and globalization as determinants of obesity among rural South African type 2 diabetics: A cross-sectional study. BMC Public Health 2015, 15, 298. [Google Scholar] [CrossRef]
- Malhotra, R.; Chan, A.; Malhotra, C.; Østbye, T. Prevalence, awareness, treatment and control of hypertension in the elderly population of Singapore. Hypertens. Res. Off. J. Jpn. Soc. Hypertens. 2010, 33, 1223–1231. [Google Scholar] [CrossRef]
- Wu, Y.; Tai, E.S.; Heng, D.; Tan, C.E.; Low, L.P.; Lee, J. Risk factors associated with hypertension awareness, treatment, and control in a multi-ethnic Asian population. J. Hypertens. 2009, 27, 190–197. [Google Scholar] [CrossRef]
- Nteta, T.P.; Mokgatle-Nthabu, M.; Oguntibeju, O.O. Utilization of the primary health care services in the Tshwane Region of Gauteng Province, South Africa. PLoS ONE 2010, 5, e13909. [Google Scholar] [CrossRef]
- Desormais, I.; Amidou, S.A.; Houehanou, Y.C.; Houinato, S.D.; Gbagouidi, G.N.; Preux, P.M.; Aboyans, V.; Lacroix, P. The prevalence, awareness, management and control of hypertension in men and women in Benin, West Africa: The TAHES study. BMC Cardiovasc. Disord. 2019, 19, 303. [Google Scholar] [CrossRef]
- Peacock, D.; Redpath, J.; Weston, M.; Evans, K.; Daub, A.; Greig, A. Literature Review on Men, Gender, Health and HIV and AIDS in South Africa; Sonke Gender Justice Network: Johannesburg, South Africa, 2008. [Google Scholar]
- Springer, K.W.; Mouzon, D.M. “Macho men” and preventive health care: Implications for older men in different social classes. J. Health Soc. Behav. 2011, 52, 212–227. [Google Scholar] [CrossRef]
- Zajacova, A.; Lawrence, E.M. The relationship between education and health: Reducing disparities through a contextual approach. Annu. Rev. Public Health 2018, 39, 273–289. [Google Scholar] [CrossRef] [PubMed]
- Seow, L.S.E.; Subramaniam, M.; Abdin, E.; Vaingankar, J.A.; Chong, S.A. Hypertension and its associated risks among Singapore elderly residential population. J. Clin. Gerontol. Geriatr. 2015, 6, 125–132. [Google Scholar] [CrossRef]
- Leng, B.; Jin, Y.; Li, G.; Chen, L.; Jin, N. Socioeconomic status and hypertension: A meta-analysis. J. Hypertens. 2015, 33, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Damacena, G.N.; Szwarcwald, C.L.; Malta, D.C.; de Souza, P.R.B., Jr.; Vieira, M.L.F.P.; Pereira, C.A.; Neto, O.L.D.; da Silva, J.B., Jr. O processo de desenvolvimento da Pesquisa Nacional de Saúde no Brasil, 2013. Epidemiol. Serviços Saúde 2015, 24, 197–206. [Google Scholar] [CrossRef]
- Foster, A.D.; Rosenzweig, M.R. Microeconomics of technology adoption. Annu. Rev. Econ. 2010, 2, 395–424. [Google Scholar] [CrossRef]
- Cutler, D.; Deaton, A.; Lleras-Muney, A. The determinants of mortality. J. Econ. Perspect. 2006, 20, 97–120. [Google Scholar] [CrossRef]
- Molenaar, E.A.; Hwang, S.-J.; Vasan, R.S.; Grobbee, D.E.; Meigs, J.B.; D’Agostino, R.B.; Levy, D.; Fox, C.S. Burden and rates of treatment and control of cardiovascular disease risk factors in obesity: The Framingham Heart Study. Diabetes Care 2008, 31, 1367–1372. [Google Scholar] [CrossRef]
- Rose, S.A.; Turchin, A.; Grant, R.W.; Meigs, J.B. Documentation of body mass index and control of associated risk factors in a large primary care network. BMC Health Serv. Res. 2009, 9, 236. [Google Scholar] [CrossRef]
- Surka, S.; Steyn, K.; Everett-Murphy, K.; Gaziano, T.A.; Levitt, N. Knowledge and perceptions of risk for cardiovascular disease: Findings of a qualitative investigation from a low-income peri-urban community in the Western Cape, South Africa. Afr. J. Prim. Health Care Fam. Med. 2015, 7. [Google Scholar] [CrossRef]
- Rampamba, E.M.; Meyer, J.C.; Helberg, E.; Godman, B. Knowledge of hypertension and its management among hypertensive patients on chronic medicines at primary health care public sector facilities in South Africa; findings and implications. Expert Rev. Cardiovasc. Ther. 2017, 15, 639–647. [Google Scholar] [CrossRef]
- Risenga, P.R.; Botha, A.; Tjallinks, J. Shangaan patients and traditional healers management strategies of hypertension in Limpopo Province. Curationis 2007, 30, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.; Walke, A.; MacLeod, M.J. Patient compliance in hypertension: Role of illness perceptions and treatment beliefs. J. Hum. Hypertens. 2004, 18, 607–613. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total Sample % | Blood Pressure Scores 1 | ||
|---|---|---|---|---|
| Normal BP | Hypertension | p-Value | ||
| Gender | ||||
| Male | 14.9% | 34.9% | 65.1% | 0.061 |
| Female | 85.1% | 25.1% | 74.9 % | |
| Age categories | ||||
| 18–35 | 26.0% | 37.5% | 62.5% | <0.001 |
| 36–49 | 31.4% | 33.7% | 66.2% | |
| 50–64 | 30.2% | 20.0% | 80.0% | |
| ≥65 | 12.6% | 14.9% | 85.0% | |
| Education | ||||
| None/primary | 29.4% | 23.9% | 76.1% | 0.215 |
| High school | 52.9% | 26.3% | 73.7% | |
| Tertiary | 17.7% | 33.7% | 66.3% | |
| Relationship status | 0.984 | |||
| Single | 61.1% | 26.5% | 73.5% | |
| In a relationship | 38.9% | 26.6% | 73.4% | |
| Employed | 0.948 | |||
| Yes | 43.9% | 26.4% | 73.6% | |
| No | 56.1% | 26.7% | 73.3% | |
| Monthly income | ||||
| <R1000 | 58.9% | 22.7% | 77.3% | 0.039 |
| ≥R1000 | 41.1% | 30.4% | 69.6% | |
| Body Mass Index | ||||
| Normal | 27.2% | 42.9% | 57.1% | <0.001 |
| Overweight | 25.2% | 32.3% | 67.1% | |
| Obese | 47.6% | 17.1% | 82.9% | |
| Blood glucose reading | ||||
| Normal range | 59.3% | 30.8% | 69.2% | 0.037 |
| Prediabetic range | 21.8% | 18.8% | 81.2% | |
| Diabetic range | 18.8% | 24.8% | 75.2% | |
| Physical activity | ||||
| No (<150 min) | 53.5% | 25.3 | 74.7% | 0.361 |
| Yes (≥ 150 min) | 46.5% | 28.7% | 71.3% | |
| Adherence to Westernized diet | ||||
| Low | 11.9% | 52.9% | 47.1% | <0.001 |
| Moderate | 35.1% | 28.9% | 71.1% | |
| High | 53.1% | 18.1% | 81.9% | |
| Beliefs about hypertension control | ||||
| Hypertension cannot be controlled with medication | 84.5% | 29.3% | 70.6% | 0.342 |
| Hypertension can be controlled with diet | 22.3% | 26.2% | 73.7% | 0.969 |
| Variable | aOR 1 | 95% CI | p |
|---|---|---|---|
| Gender: Reference: female | 1 | ||
| male | 1.18 | 0.63–2.21 | 0.609 |
| Age categories: Reference 18–35 | 1 | ||
| 36–49 | 0.80 | 0.46–1.40 | 0.439 |
| 50–64 | 1.87 | 1.03–3.39 | 0.039 |
| ≥65 | 3.20 | 1.34–7.63 | 0.009 |
| Income: Reference < 1000 | |||
| ≥1000 | 1.47 | 0.95–4.29 | 0.087 |
| BMI: Reference normal | |||
| Normal | 1 | ||
| overweight | 1.53 | 0.85–2.73 | 0.149 |
| Obese | 3.52 | 2.01–6.18 | <0.001 |
| Blood glucose: Reference Normal | |||
| Normal range | 1 | ||
| Prediabetic range | 1.04 | 0.58–1.85 | 0.907 |
| Diabetic range | 2.24 | 1.06–4.72 | 0.034 |
| Adherence to Westernized diet: Reference Low | |||
| Low | 1 | ||
| Moderate | 2.94 | 1.57–5.51 | 0.001 |
| High | 5.35 | 2.85–10.05 | <0.001 |
| Variables | Bivariate Associations 1 | Multivariate Associations 2 | ||||
|---|---|---|---|---|---|---|
| Treated Hypertension (43.6%) | Untreated Hypertension (56.4%) | p-Value | aOR | 95% CI | p | |
| Gender | ||||||
| Female | 46.9% | 53.1% | 0.002 | 1 | ||
| Male | 19.4% | 80.6% | 2.93 | 1.90–7.95 | 0.034 | |
| Age categories | <0.001 | |||||
| 18–35 | 25.0% | 75.0% | 1 | |||
| 36–49 | 34.0% | 66.0% | 0.85 | 0.40–1.80 | 0.666 | |
| 50–64 | 52.6% | 47.4% | 0.45 | 0.22–0.95 | 0.035 | |
| ≥65 | 66.7% | 33.4% | 0.19 | 0.07–0.48 | 0.000 | |
| Education | ||||||
| None/primary | 52.4% | 47.6% | 0.052 | 1 | ||
| High school | 37.8% | 62.2% | 1.57 | 0.86–2.67 | 0.140 | |
| Tertiary | 46.7% | 53.3% | 1.64 | 0.68–3.92 | 0.268 | |
| Relationship status | ||||||
| Single | 45.3% | 54.7% | 0.454 | - | ||
| In a relationship | 41.1% | 58.9% | ||||
| Employed | ||||||
| yes | 38.7% | 61.3% | 0.127 | |||
| no | 47.2% | 52.8% | ||||
| Monthly income | ||||||
| <R1000 | 42.1% | 57.9% | 0.474 | |||
| ≥R1000 | 46.1% | 53.9% | ||||
| Body Mass Index | ||||||
| Underweight/normal | 25.8% | 74.2% | <0.001 | 1 | ||
| Overweight | 37.2% | 62.8% | 0.512 | 0.23–1.16 | 0.109 | |
| Obese | 52.0% | 48.0% | 0.304 | 0.15–0.64 | 0.002 | |
| Blood glucose reading | ||||||
| Normal range | 40.2% | 59.8% | 0.163 | - | ||
| Prediabetic range | 42.9% | 57.1% | ||||
| Diabetic range | 54.1% | 45.9% | ||||
| Physical activity | ||||||
| No (<150 min) | 45.7 | 54.3% | 0.419 | - | ||
| Yes (≥150 min) | 41.3% | 58.7% | ||||
| Adherence to westernized diet | ||||||
| Low | 63.0% | 37.0% | 0.106 | - | ||
| Moderate | 42.2% | 57.8% | ||||
| High | 41.7% | 58.3% | ||||
| Beliefs about hypertension control | ||||||
| Hypertension cannot be controlled with medication | 57.4% | 42.6% | 0.026 | 3.02 | 1.50–6.09 | 0.002 |
| Hypertension can be controlled with diet | 40.0% | 60.0% | 0.489 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, J.R.; Mabhida, S.E.; Myers, B.; Apalata, T.; Nicol, E.; Benjeddou, M.; Muller, C.; Johnson, R. Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa. Int. J. Environ. Res. Public Health 2021, 18, 1215. https://doi.org/10.3390/ijerph18031215
Sharma JR, Mabhida SE, Myers B, Apalata T, Nicol E, Benjeddou M, Muller C, Johnson R. Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa. International Journal of Environmental Research and Public Health. 2021; 18(3):1215. https://doi.org/10.3390/ijerph18031215
Chicago/Turabian StyleSharma, Jyoti Rajan, Sihle E. Mabhida, Bronwyn Myers, Teke Apalata, Edward Nicol, Mongi Benjeddou, Christo Muller, and Rabia Johnson. 2021. "Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa" International Journal of Environmental Research and Public Health 18, no. 3: 1215. https://doi.org/10.3390/ijerph18031215
APA StyleSharma, J. R., Mabhida, S. E., Myers, B., Apalata, T., Nicol, E., Benjeddou, M., Muller, C., & Johnson, R. (2021). Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa. International Journal of Environmental Research and Public Health, 18(3), 1215. https://doi.org/10.3390/ijerph18031215








