Accuracy of Community Informant Led Detection of Maternal Depression in Rural Pakistan
Abstract
1. Introduction
2. Material and Methods
2.1. Setting
2.2. Recruitment of LHWs and Peers
2.3. Instruments
2.3.1. CIDT-MD
2.3.2. Structured Clinical Interviews of DSM Disorders (SCID)
2.3.3. Training of Community Informants to Use CIDT-MD
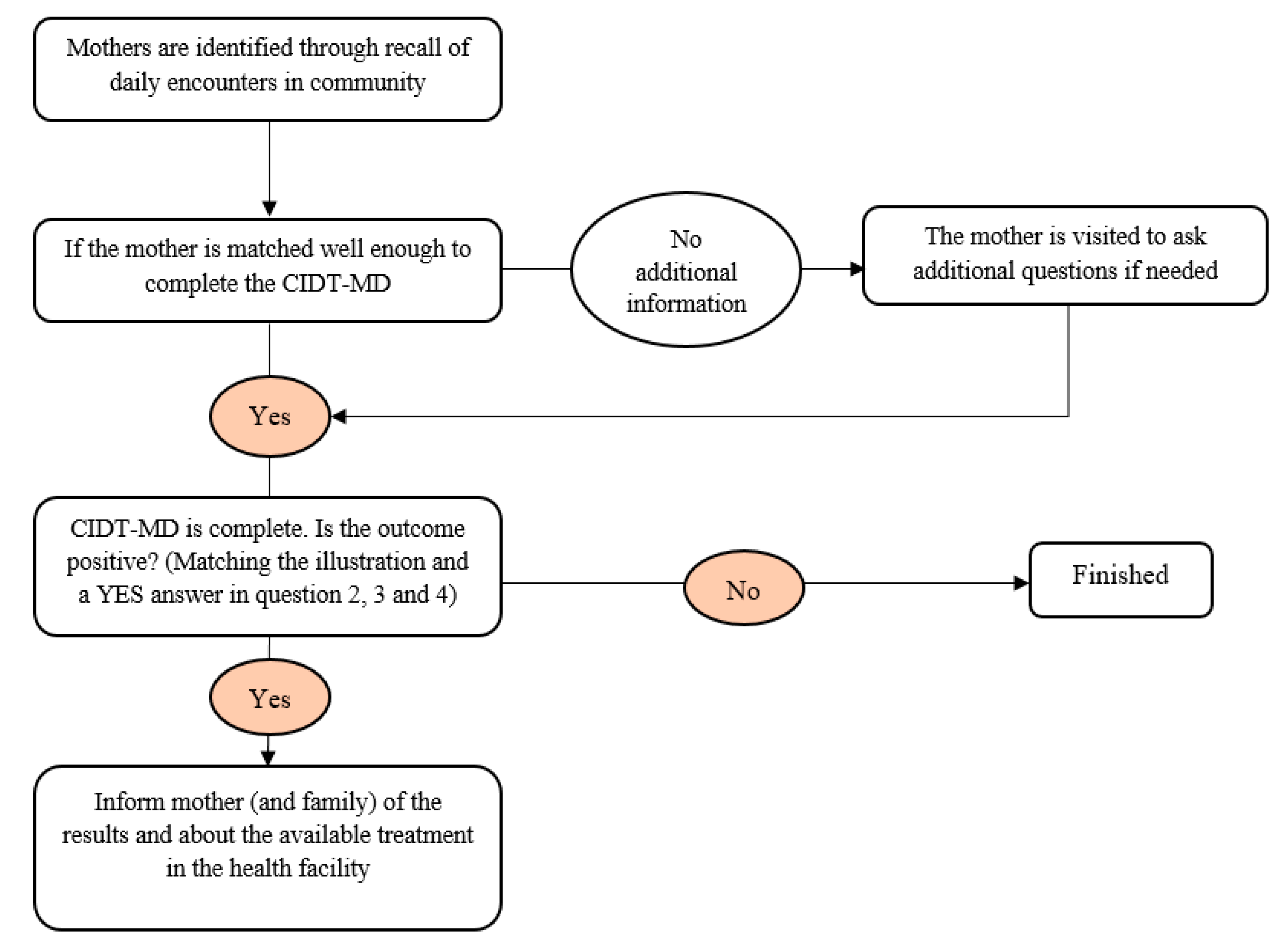
2.4. Data Collection Procedure
2.5. Sample Size
2.6. Ethics
2.7. Study Variables
2.8. Data Analysis
2.8.1. Descriptive Statistics
2.8.2. Face Validity of CIDT-MD
2.8.3. Content Validity
2.8.4. Construct Validity
2.8.5. Goodness of Fit
2.8.6. Reliability
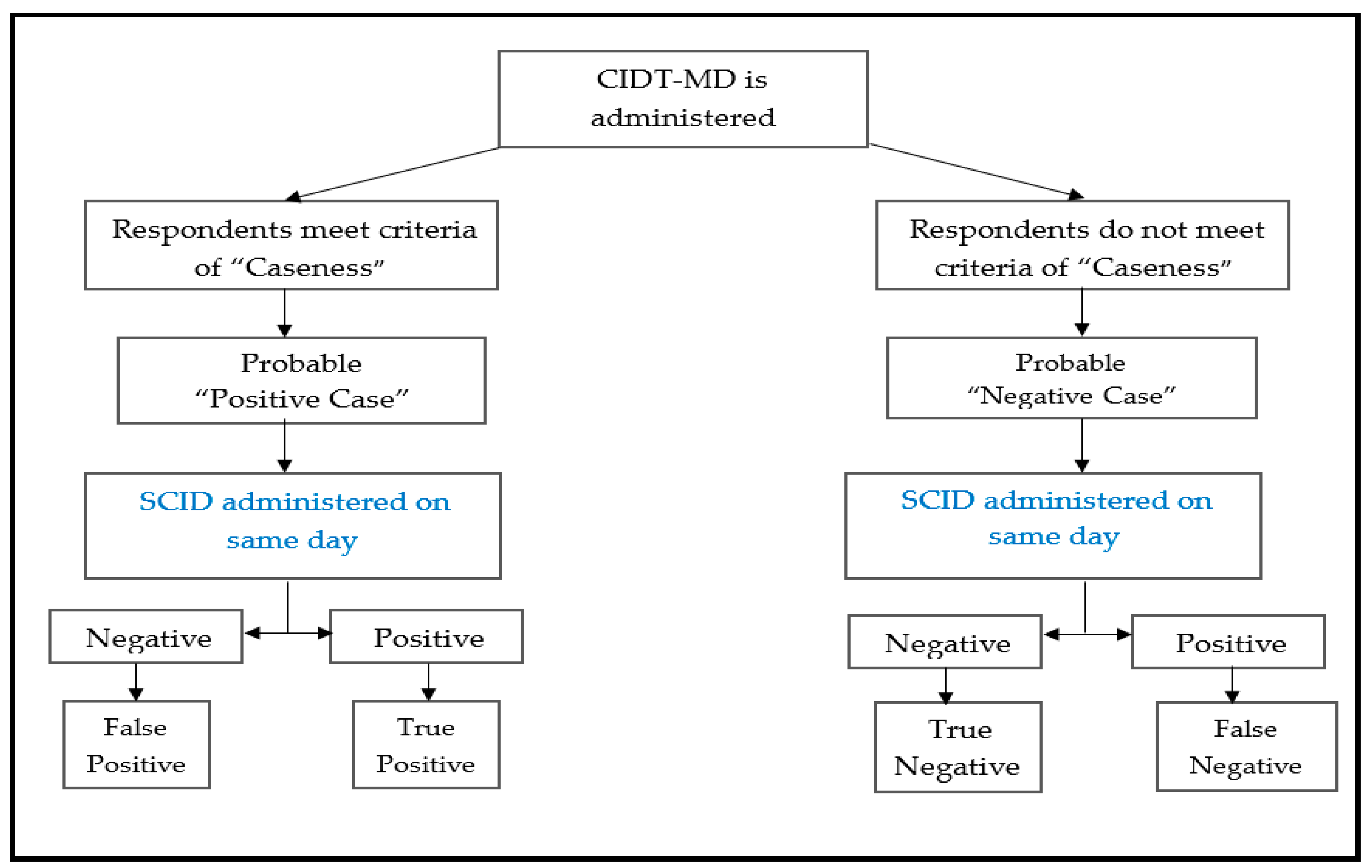
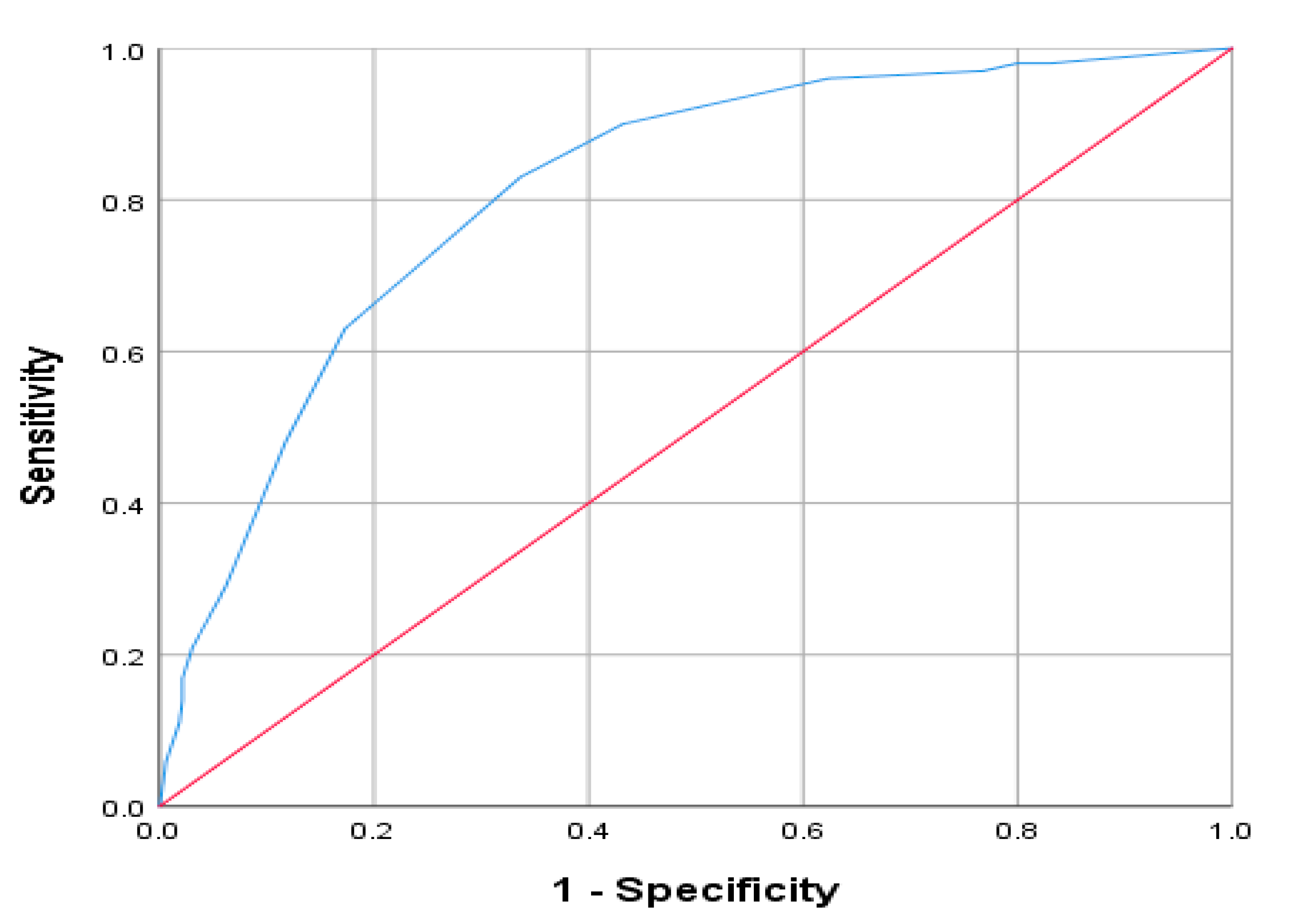
2.8.7. Criterion Validity
2.8.8. Known Group Validity
3. Results
3.1. Participant Characteristics
3.2. Face Validity
3.3. Content Validity
3.4. Construct Validity
3.5. Uni-Dimensionality Measures & Goodness of Fit
3.6. Reliability
3.7. Criterion Validity
3.8. Known Group Validity
4. Discussion
4.1. Future Implications
4.2. Strengths & Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of Maternal Depression, Risk Factors, and Child Outcomes in Low-Income and Middle-Income Countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef]
- Herba, C.M.; Glover, V.; Ramchandani, P.G.; Rondon, M.B. Maternal Depression and Mental Health in Early Childhood: An Examination of Underlying Mechanisms in Low-Income and Middle-Income Countries. Lancet Psychiatry 2016, 3, 983–992. [Google Scholar] [CrossRef]
- Hanlon, C. Maternal depression in low- and middle-income countries. Int. Health 2012, 5, 4–5. [Google Scholar] [CrossRef] [PubMed]
- De silva, M.J.; Lee, L.; Fuhr, D.C.; Rathod, S.; Chisholm, D.; Schellenberg, J.; Patel, V. Estimating the Coverage of Mental Health Pro-grammes: A Systematic Review. Int. J. Epidemiol. 2014, 43, 341–353. [Google Scholar] [CrossRef]
- Weinmann, S.; Koesters, M. Mental Health Service Provision in Low and Middle-Income Countries: Recent Developments. Curr. Opin. Psychiatry 2016, 29, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Munodawafa, M.; Mall, S.; Lund, C.; Schneider, M. Process evaluations of task sharing interventions for perinatal depression in low and middle income countries (LMIC): A systematic review and qualitative meta-synthesis. BMC Health Serv. Res. 2018, 18, 205. [Google Scholar] [CrossRef]
- Grote, N.K.; Katon, W.J.; Russo, J.E.; Lohr, M.J.; Curran, M.; Galvin, E.; Carson, K. Collaborative Care for Perinatal Depression in Socioec-onomically Disadvantaged Women: A Randomized Trial. Depress Anxiety 2015, 32, 821–834. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. mhGAP Intervention Guide Mental Health Gap Action Programme Version 2.0 for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings; mhGAP Interv Guid Ment Neurol Subst Use Disord Non-Specialized Heal Settings Ment Heal Gap Action Program; World Health Organization: Geneva, Switzerland, 2016; pp. 1–173. [Google Scholar]
- Hossain, S.J.; Roy, B.R.; Hossain, A.T.; Mehrin, F.; Tipu, S.M.M.U.; Tofail, F.; El Arifeen, S.; Tran, T.D.; Fisher, J.; Hamadani, J.D. Prevalence of Maternal Postpartum Depression, Health-Seeking Behavior and Out of Pocket Payment for Physical Illness and Cost Coping Mechanism of the Poor Families in Bangladesh: A Rural Community-Based Study. Int. J. Environ. Res. Public Health 2020, 17, 4727. [Google Scholar] [CrossRef]
- Azale, T.; Fekadu, A.; Hanlon, C. Treatment gap and help-seeking for postpartum depression in a rural African setting. BMC Psychiatry 2016, 16, 196. [Google Scholar] [CrossRef]
- Jordans, M.J.D.; Kohrt, B.A.; Luitel, N.P.; Lund, C.; Komproe, I.H. Proactive Community Case-Finding to Facilitate Treatment Seek-ing for Mental Disorders. Nepal. Bull. World Health Organ. 2017, 95, 531–536. [Google Scholar] [CrossRef]
- Jordans, M.J.D.; Kohrt, B.A.; Luitel, N.P.; Komproe, I.H.; Lund, C. Accuracy of proactive case finding for mental disorders by community informants in Nepal. Br. J. Psychiatry 2015, 207, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Ali, G.C.; Ryan, G.; De Silva, M.J. Validated Screening Tools for Common Mental Disorders in Low and Middle Income Coun-tries: A Systematic Review. PLoS ONE 2016, 11, e0156939. [Google Scholar] [CrossRef] [PubMed]
- Zubaran, C.; Schumacher, M.; Roxo, M.R.; Foresti, K. Screening Tools for Postpartum Depression: Validity and Cultural Dimen-sions. Afr. J. Psychiatry 2010, 13, 357–365. [Google Scholar]
- Kagee, A.; Tsai, A.C.; Lund, C.; Tomlinson, M. Screening for common mental disorders in low resource settings: Reasons for caution and a way forward. Int. Health 2013, 5, 11–14. [Google Scholar] [CrossRef]
- Hanlon, C.; Medhin, G.; Alem, A.; Araya, M.; Abdulahi, A.; Hughes, M.; Tesfaye, M.; Wondimagegn, D.; Patel, V.; Prince, M. Detecting perinatal common mental disorders in Ethiopia: Validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. J. Affect. Disord. 2008, 108, 251–262. [Google Scholar] [CrossRef]
- Van Heyningen, T.; Honikman, S.; Tomlinson, M.; Field, S.; Myer, L. Comparison of Mental Health Screening Tools for Detecting Antenatal Depression and Anxiety Disorders in South African Women. PLoS ONE 2018, 13, e0193697. [Google Scholar] [CrossRef]
- Pakistan Ministry of Health; PHC Wing. National Program for Family Planning and Primary Health Care: The Lady Health Workers’ Programme. 2008. Available online: http://www.who.int/pmnch/countries/ali_akhtar_hakro_Pakistan.pdf (accessed on 1 November 2020).
- Mohsin, S.; Atif, N.; Rabbani, W.; Tariq, A.; Khan, S.A.; Tariq, M.S.S. Cultural Adaptation of Community Informant Tool for Detec-tion of Maternal Depression in Rural Pakistan. Front. Psychiatry 2020. under review. [Google Scholar]
- Gelaye, B.; Tadesse, M.G.; Williams, M.A.; Fann, J.R.; Stoep, A.V.; Zhou, X.-H.A. Assessing validity of a depression screening instrument in the absence of a gold standard. Ann. Epidemiol. 2014, 24, 527–531. [Google Scholar] [CrossRef]
- Chorwe-Sungania, G.; Chipps, J. A systematic review of screening instruments for depression for use in antenatal services in low resource settings. BMC Psychiatry 2017, 17, 112. [Google Scholar] [CrossRef]
- Subba, P.; Luitel, N.P.; Kohrt, B.A.; Jordans, M.J.D. Improving detection of mental health problems in community settings in Nepal: Development and pilot testing of the community informant detection tool. Confl. Health 2017, 11, 28. [Google Scholar] [CrossRef]
- Sikander, S.; Ahmad, I.; Bates, L.M.; Gallis, J.; Hagaman, A.; O’Donnell, K.; Turner, E.L.; Zaidi, A.; Rahman, A.; Maselko, J. Cohort Profile: Perinatal Depression and Child Socio-Emotional Development; The Bachpan Cohort Study from Rural Pakistan. BMJ Open 2019, 9, e025644. [Google Scholar] [CrossRef] [PubMed]
- Maselko, J.; Sikander, S.; Turner, E.L.; Bates, L.M.; Ahmad, I.; Atif, N.; Baranov, V.; Bhalotra, S.; Bibi, A.; Bibi, T.; et al. Effectiveness of a Peer-Delivered, Psychosocial Intervention on Maternal Depression and Child Development at 3 Years Postnatal: A Cluster Randomised Trial in Pakistan. Lancet Psychiatry 2020, 7, 775–787. [Google Scholar] [CrossRef]
- First, M.B. Structured Clinical Interview for the DSM (SCID). Encycl. Clin. Psychol. 2015, 1–6. [Google Scholar] [CrossRef]
- Gorman, L.L.; O’Hara, M.W.; Figueiredo, B.; Hayes, S.; Jacquemain, F.; Kammerer, M.; Klier, C.M.; Rosi, S.; Seneviratne, G.; Sutter-Dallay, A.-L. Adaptation of the Structured Clinical Interview for DSM-IV Disorders for assessing depression in women during pregnancy and post-partum across countries and cultures. Br. J. Psychiatry 2004, 184, s17–s23. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Iqbal, Z.; Waheed, W.; Hussain, N. Translation and cultural adaptation of health questionnaires. J. Pak. Med. Assoc. 2003, 53, 142–147. [Google Scholar]
- Gallis, J.A.; Maselko, J.; O’Donnell, K.; Song, K.; Saqib, K.; Turner, E.L.; Sikander, S. Criterion-related validity and reliability of the Urdu version of the patient health questionnaire in a sample of community-based pregnant women in Pakistan. PeerJ 2018, 6, e5185. [Google Scholar] [CrossRef]
- Mhatre, V.H.; Kelsey, C.; Martin, J.-A.L. Does Interviewer Status Matter? An examination of Lay Interviewers and Medical Doctor Interviewers in an Epidemiological Study in Vietnam. Bone 2012, 23, 17. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624763/pdf/nihms412728.pdf (accessed on 2 November 2020).
- Chen, S.; Fang, Y.; Chiu, H.; Fan, H.; Jin, T.; Conwell, Y. Validation of the nine-item Patient Health Questionnaire to screen for major depression in a Chinese primary care population. Asia-Pac. Psychiatry 2013, 5, 61–68. [Google Scholar] [CrossRef]
- Chin, W.Y.; Choi, E.P.H.; Chan, K.T.Y.; Wong, C.K.H. The Psychometric Properties of the Center for Epidemiologic Studies Depres-sion Scale in Chinese Primary Care Patients: Factor Structure, Construct Validity, Reliability, Sensitivity and Responsive-ness. PLoS ONE 2015, 10, e0135131. [Google Scholar] [CrossRef]
- Gelaye, B.; Williams, M.A.; Lemma, S.; Deyessa, N.; Bahretibeb, Y.; Shibre, T.; Wondimagegn, D.; Lemenhe, A.; Fann, J.R.; Stoep, A.V.; et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013, 210, 653–661. [Google Scholar] [CrossRef]
- Hanlon, C.; Medhin, G.; Selamu, M.; Breuer, E.; Worku, B.; Hailemariam, M.; Lund, C.; Prince, M.; Fekadu, A. Validity of brief screening questionnaires to detect depression in primary care in Ethiopia. J. Affect. Disord. 2015, 186, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, M.; Ohtsuki, T.; Yonemoto, N.; Kawashima, Y.; Saitoh, A.; Oikawa, Y.; Kurosawa, M.; Muramatsu, K.; Furukawa, T.A.; Yamada, M. Validity of the Patient Health Questionnaire (PHQ)-9 and PHQ-2 in general internal medicine primary care at a Japanese rural hospital: A cross-sectional study. Gen. Hosp. Psychiatry 2013, 35, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-I.; Yeh, Z.-T.; Huang, H.-C.; Sun, F.-J.; Tjung, J.-J.; Hwang, L.-C.; Shih, Y.-H.; Yeh, A.W.-C. Validation of Patient Health Questionnaire for depression screening among primary care patients in Taiwan. Compr. Psychiatry 2011, 52, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Azah, M.N.; Shah, M.E.; Juwita, S.; Bahri, I.S.; Rushidi, W.M.; Jamil, Y.M. Validation of the Malay Version Brief Patient Health Questionnaire (PHQ-9) among Adult Attending Family Medicine Clinics. Int. Med. J. 2005, 12, 259–263. [Google Scholar]
- Zuithoff, N.P.; Vergouwe, Y.; King, M.; Nazareth, I.; Van Wezep, M.J.; Moons, K.G.; Geerlings, M.I. The Patient Health Questionnaire-9 for Detection of Major Depressive Disorder in Primary Care: Consequences of Current Thresholds in a Cross-sectional Study. BMC Fam. Pract. 2010, 11. [Google Scholar] [CrossRef] [PubMed]
- Breedlove, G.; Fryzelka, D. Depression Screening During Pregnancy. J. Midwifery Women’s Health 2011, 56, 18–25. [Google Scholar] [CrossRef]
- Parsons, C.E.; Young, K.S.; Rochat, T.J.; Kringelbach, M.L.; Stein, A. Postnatal depression and its effects on child development: A review of evidence from low- and middle-income countries. Br. Med. Bull. 2011, 101, 57–79. [Google Scholar] [CrossRef]
- Mitchell, A.; Coyne, J.; Mitchell, A.J. Screening for postnatal depression: Barriers to success. BJOG Int. J. Obstet. Gynaecol. 2008, 116, 11–14. [Google Scholar] [CrossRef]
- Paulden, M.; Palmer, S.; Hewitt, C.; Gilbody, S. Screening for Postnatal Depression in Primary Care: Cost Effectiveness Analy-sis. BMJ 2010, 340, 253. [Google Scholar] [CrossRef]
- Rahman, A.; Malik, A.; Sikander, S.; Roberts, C.; Creed, F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. Lancet 2008, 372, 902–909. [Google Scholar] [CrossRef]
- Tsai, A.C.; Tomlinson, M.; Dewing, S.; Ingrid, M.; Harwood, J.M.; Chopra, M.; Rotheram-Borus, M.J. Antenatal Depression Case-Finding by Com-munity Health Workers in South Africa: Feasibility of a Mobile Phone Application. Arch. Womens Ment. Health 2014, 17, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.; Eaton, J.; Radtke, B.; George, C.; Manuel, B.V.; De Silva, M.J.; Patel, V. Three models of community mental health services in low-income countries. Int. J. Ment. Health Syst. 2011, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Anthoine, E.; Moret, L.; Regnault, A.; Sébille, V.; Hardouin, J.-B. Sample size used to validate a scale: A review of publications on newly-developed patient reported outcomes measures. Health Qual. Life Outcomes 2014, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, A.; Boström, K.B.; Gustavsson, P.; Ekselius, L. Which instruments to support diagnosis of depression have sufficient accuracy? A systematic review. Nord. J. Psychiatry 2015, 69, 497–508. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Thornicroft, G. Packages of Care for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: PLoS Medicine Series. PLoS Med. 2009, 6, e1000160. [Google Scholar] [CrossRef] [PubMed]
- Waclawski, E.R. Health Measurement Scales—A Practical Guide to Their Development and Use. Occup. Med. 2010, 60, 156. [Google Scholar] [CrossRef]
- Weobong, B.; Akpalu, B.; Doku, V.; Owusu-Agyei, S.; Hurt, L.; Kirkwood, B.; Prince, M.J. The comparative validity of screening scales for postnatal common mental disorder in Kintampo, Ghana. J. Affect. Disord. 2009, 113, 109–117. [Google Scholar] [CrossRef]
- Fallon, V.; Halford, J.C.G.; Bennett, K.M.; Harrold, J.A. The Postpartum Specific Anxiety Scale: Development and preliminary validation. Arch. Women’s Ment. Health 2016, 19, 1079–1090. [Google Scholar] [CrossRef]
- Flora, D.B.; LaBrish, C.; Chalmers, R.P. Old and New Ideas for Data Screening and Assumption Testing for Exploratory and Confirmatory Factor Analysis. Front. Psychol. 2012, 3, 55. [Google Scholar] [CrossRef]
- Gaskin, C.J.; Happell, B. On exploratory factor analysis: A review of recent evidence, an assessment of current practice, and recommendations for future use. Int. J. Nurs. Stud. 2014, 51, 511–521. [Google Scholar] [CrossRef]
- Green, E.; Tuli, H.; Kwobah, E.; Menya, D.; Chesire, I.; Schmidt, C. Developing and validating a perinatal depression screening tool in Kenya blending Western criteria with local idioms: A mixed methods study. J. Affect. Disord. 2018, 228, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Hafeez, A.; Mohamud, B.K.; Shiekh, M.R.; Shah, S.A.I.; Jooma, R. Lady health workers programme in Pakistan: Challenges, achievements and the way forward. J. Pak. Med. Assoc. 2011, 61, 210–215. [Google Scholar] [PubMed]
| Variables | CIDT-MD | p-Value | SCID | p-Value | ||
|---|---|---|---|---|---|---|
| Depressed | Non Depressed | Depressed | Non Depressed | |||
| n = 150 (35%) | n = 275 (65%) | n = 100 (23.5%) | n = 325 (76.4%) | |||
| Women’s Age | ||||||
| 18–27 | 65 (43.3%) | 128 (46.5%) | 0.07 | 46 (46%) | 147 (45.2%) | 0.84 |
| 28–37 | 79 (52.6%) | 139 (50.5%) | 52 (52%) | 168 (51.7%) | ||
| ≥38 | 6 (4%) | 8 (3%) | 2 (2%) | 10 (3.1%) | ||
| Family Structure | ||||||
| Joint | 65 (43.3%) | 107 (39%) | 0.05 | 47 (47%) | 157 (48.3%) | 0.63 |
| Multiple Households | 26 (17.3%) | 30 (11%) | 14 (14%) | 125 (38.4%) | ||
| Nuclear | 58 (30.6%) | 136 (49.4%) | 38 (38%) | 43 (13.2%) | ||
| Number of Children | ||||||
| None | 8 (5.3%) | 33 (12.1%) | 0.06 | 8 (8%) | 33 (10.2%) | 0.23 |
| 1–3 | 107 (71.3%) | 207 (75.2%) | 58 (58%) | 243 (74.7%) | ||
| >3 | 35 (23.3%) | 35 (12.7%) | 26 (26%) | 49 (15%) | ||
| Women Education | ||||||
| None | 20 (13.3%) | 21 (7.7%) | 0.02 | 13 (13%) | 26 (8%) | 0.004 |
| Primary | 28 (18.7%) | 31 (11.4% | 20 (20%) | 38 (11.6%) | ||
| Middle | 23 (15.3%) | 29 (10.6%) | 15 (15%) | 40.2(13%) | ||
| Secondary | 40 (26.7%) | 95 (34%) | 27 (27%) | 103 (31.6%) | ||
| Higher Secondary | 23 (15.3%) | 34 (12.5%) | 15 (15%) | 43 (13.2%) | ||
| Graduate | 12 (8%) | 44 (16.1%) | 9 (9%) | 48 (15%) | ||
| Masters | 4 (2.7%) | 22 (8.1%) | 1 (1%) | 25 (8%) | ||
| Husband Education | ||||||
| None | 16 (10.7%) | 12 (4.4%) | 0.05 | 10 (10%) | 18 (5.5%) | 0.04 |
| Primary | 13 (8.7%) | 19 (7%) | 11 (11%) | 21 (6.5%) | ||
| Middle | 24 (16%) | 53 (19.4%) | 21 (21%) | 56 (17.2%) | ||
| Secondary | 75 (50%) | 119 (43.1%) | 42 (40.2%) | 152 (46.2%) | ||
| Higher Secondary | 13 (8.7%) | 40 (14.7%) | 9 (9%) | 44 (13.5%) | ||
| Graduate | 6 (4%) | 20 (7.3%) | 4 (4%) | 22 (6.8%) | ||
| Masters | 3 (2%) | 11 (4%) | 3 (3%) | 12 (3.7%) | ||
| Income | ||||||
| Did not know | 21 (14%) | 36 (13.1%) | 0.23 | 13 (13%) | 45 (13.8%) | 0.36 |
| 10000–20,000 | 46 (30.6%) | 114 (41.4%) | 32 (32%) | 128 (45.5%) | ||
| 21,000–30,000 | 49 (12.6%) | 78 (28.3%) | 35 (35%) | 92 (28.3%) | ||
| 31,000–40,000 | 24 (16%) | 30 (11%) | 14 (14%) | 41 (12.6%) | ||
| 41,000–50,000 | 7 (4.6%) | 12 (4.3%) | 3 (3%) | 16 (5%) | ||
| >51,000 | 3 (2%) | 3 (1.1%) | 3 (3%) | 3 (1%) | ||
| Items | Corrected Item-Total Correlation | Squared Multiple Correlation | Cronbach’s Alpha if Item Deleted | Factor Loading | Communality |
|---|---|---|---|---|---|
| Difficulty in sleeping | 0.783 | 0.655 | 0.853 | 0.64 | 0.42 |
| Loss of appetite | 0.750 | 0.626 | 0.854 | 0.57 | 0.32 |
| Agitation | 0.703 | 0.532 | 0.857 | 0.59 | 0.35 |
| Lack of Concentration | 0.778 | 0.663 | 0.853 | 0.67 | 0.45 |
| Helplessness | 0.730 | 0.605 | 0.856 | 0.57 | 0.32 |
| Fatigue | 0.689 | 0.551 | 0.858 | 0.68 | 0.46 |
| Lack of Interest | 0.581 | 0.413 | 0.866 | 0.76 | 0.58 |
| Low mood | 0.767 | 0.698 | 0.854 | 0.84 | 0.70 |
| Suicidal ideation | 0.374 | 0.495 | 0.873 | 0.85 | 0.71 |
| Day to day functioning | 0.157 | 0.309 | 0.877 | 0.80 | 0.67 |
| Chronicity | 0.312 | 0.322 | 0.873 | 0.65 | 0.42 |
| Self-harm/Suicidal Ideation | 0.113 | 0.274 | 0.879 | 0.73 | 0.54 |
| Stressors | Response | Mean | Standard Deviation | p-Value |
|---|---|---|---|---|
| Overwhelmed with domestic responsibility | No | 3.67 | 3.19 | <0.001 |
| Yes | 4.70 | 2.65 | ||
| Poverty | No | 3.82 | 2.96 | <0.001 |
| Yes | 5.60 | 2.64 | ||
| Ailments | No | 3.83 | 3.06 | <0.001 |
| Yes | 5.13 | 2.55 | ||
| Experience of domestic violence | No | 3.86 | 2.78 | <0.001 |
| Yes | 8.28 | 2.71 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohsin, S.; Waqas, A.; Atif, N.; Rabbani, M.W.; Ali Khan, S.; Bilal, S.; Sharif, M.; Bibi, A.; Sikander, S. Accuracy of Community Informant Led Detection of Maternal Depression in Rural Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 1075. https://doi.org/10.3390/ijerph18031075
Mohsin S, Waqas A, Atif N, Rabbani MW, Ali Khan S, Bilal S, Sharif M, Bibi A, Sikander S. Accuracy of Community Informant Led Detection of Maternal Depression in Rural Pakistan. International Journal of Environmental Research and Public Health. 2021; 18(3):1075. https://doi.org/10.3390/ijerph18031075
Chicago/Turabian StyleMohsin, Shamaila, Ahmed Waqas, Najia Atif, Muhamamd Waqas Rabbani, Shahzad Ali Khan, Samina Bilal, Maria Sharif, Amina Bibi, and Siham Sikander. 2021. "Accuracy of Community Informant Led Detection of Maternal Depression in Rural Pakistan" International Journal of Environmental Research and Public Health 18, no. 3: 1075. https://doi.org/10.3390/ijerph18031075
APA StyleMohsin, S., Waqas, A., Atif, N., Rabbani, M. W., Ali Khan, S., Bilal, S., Sharif, M., Bibi, A., & Sikander, S. (2021). Accuracy of Community Informant Led Detection of Maternal Depression in Rural Pakistan. International Journal of Environmental Research and Public Health, 18(3), 1075. https://doi.org/10.3390/ijerph18031075




