Diet Quality and Mental Health Status among Division 1 Female Collegiate Athletes during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
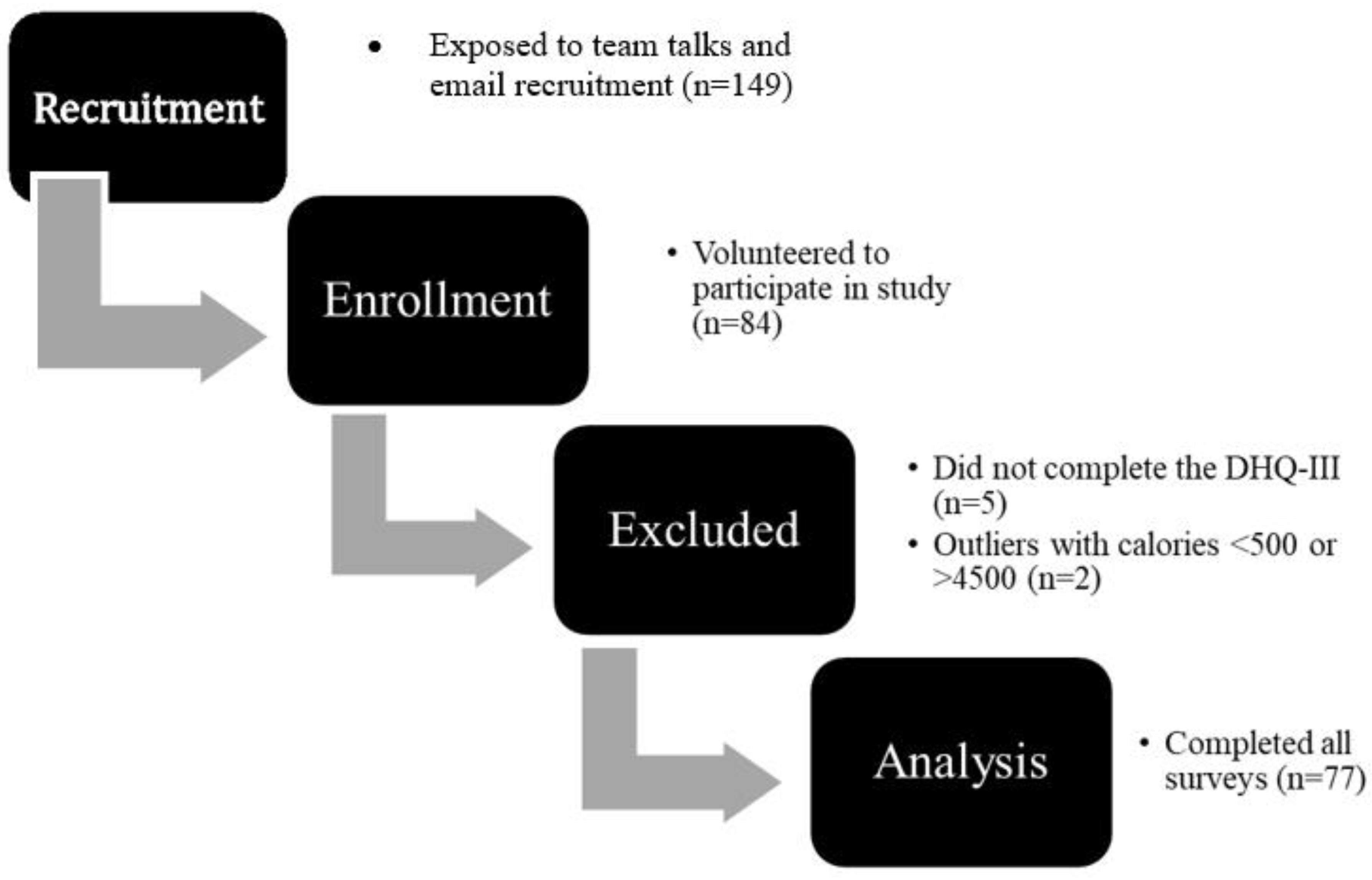
2.1. Participants
Inclusion/Exclusion Criteria
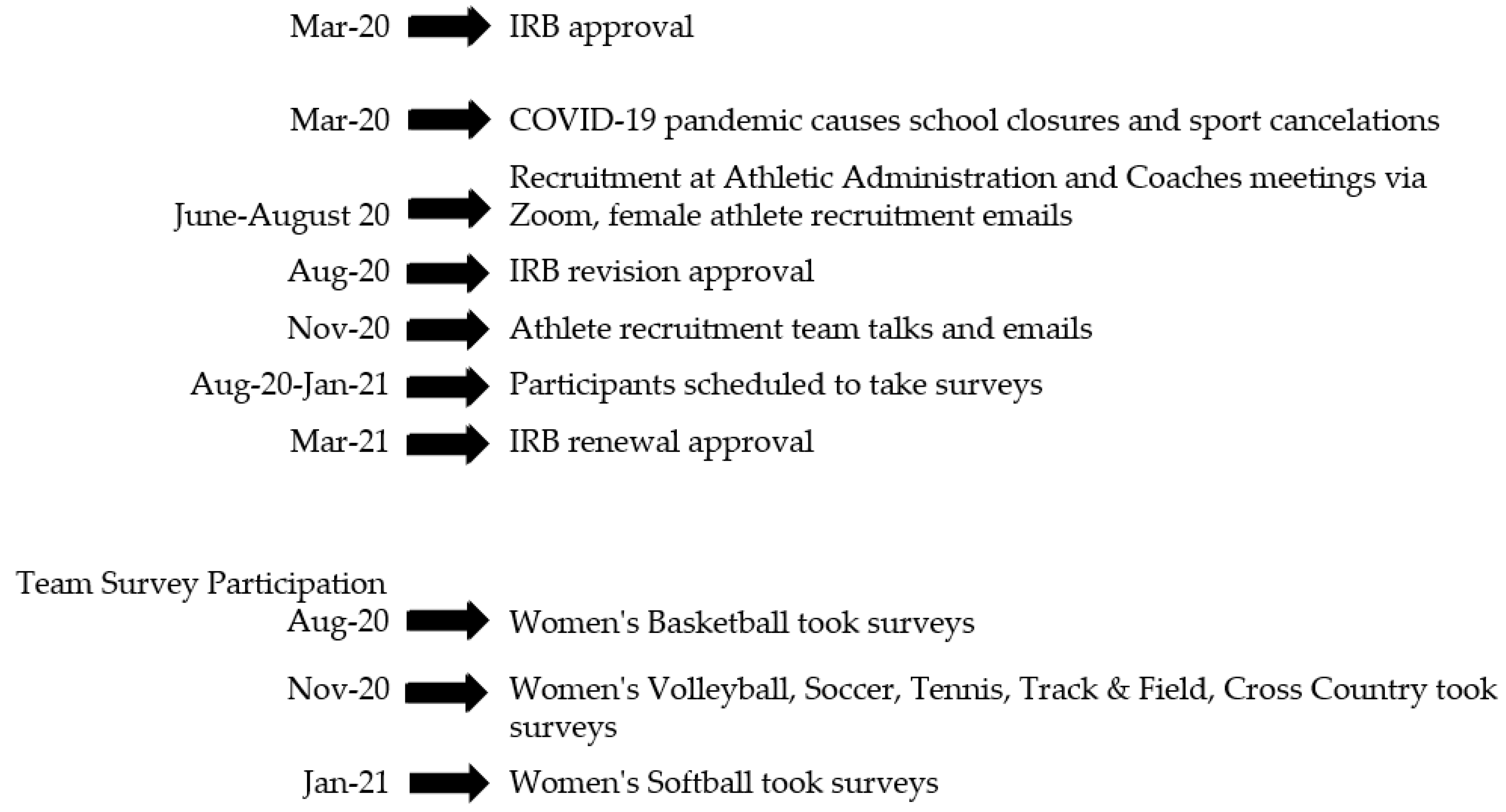
2.2. Study Timeline
2.3. Measures
2.3.1. Depression Anxiety Stress Scale (DASS-21)
2.3.2. Athlete Psychological Strain Questionnaire (APSQ)
2.3.3. COVID Stress Scale (CSS)
2.3.4. Diet History Questionnaire (DHQ-III)
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rao, A.L.; Hong, E.S. Understanding depression and suicide in college athletes: Emerging concepts and future directions. Br. J. Sports Med. 2016, 50, 136–137. [Google Scholar] [CrossRef]
- Reardon, C.L.; Hainline, B.; Aron, C.M.; Baron, D.; Baum, A.L.; Bindra, A.; Budgett, R.; Campriani, N.; Castaldelli-Maia, J.M.; Currie, A.; et al. Mental health in elite athletes: International Olympic Committee consensus statement (2019). Br. J. Sports Med. 2019, 53, 667–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Neil, A.; Berk, M.; Itsiopoulos, C.; Castle, D.; Opie, R.; Pizzinga, J.; Brazionis, L.; Hodge, A.; Mihalopoulos, C.; Chatterton, M.L.; et al. A randomised, controlled trial of a dietary intervention for adults with major depression (the “SMILES” trial): Study protocol. BMC Psychiatry 2014, 13, 114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuoka, Y.; Hamazaki, K. Considering Mental Health from the Viewpoint of Diet: The role and possibilities of nutritional psychiatry. Seishin Shinkeigaku Zasshi = Psychiatr. Neurol. Jpn. 2016, 118, 880–894. [Google Scholar]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L.; et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017, 15, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Firth, J.; Marx, W.; Dash, S.; Carney, R.; Teasdale, S.; Solmi, M.; Stubbs, B.; Schuch, F.; Carvalho, A.F.; Jacka, F.; et al. The effects of dietary improvement on symptoms of depression and anxiety: A meta-analysis of randomized controlled trials. Psychosom. Med. 2019, 81, 265–280. [Google Scholar] [CrossRef] [PubMed]
- Meegan, A.P.; Perry, I.J.; Phillips, C.M. The association between dietary quality and dietary guideline adherence with mental health outcomes in adults: A cross-sectional analysis. Nutrients 2017, 9, 238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, U.; Mishra, S.; Xu, J.; Levin, S.; Gonzales, J.; Barnard, N.D. A Multicenter Randomized Controlled Trial of a Nutrition Intervention Program in a Multiethnic Adult Population in the Corporate Setting Reduces Depression and Anxiety and Improves Quality of Life: The GEICO Study. Am. J. Heal. Promot. AJHP 2015, 29, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Greenleaf, C.; Petrie, T.A.; Carter, J.; Reel, J.J. Female collegiate athletes: Prevalence of eating disorders and disordered eating behaviors. J. Am. Coll. Health 2009, 57, 489–495. [Google Scholar] [CrossRef]
- Becker, C.B.; McDaniel, L.; Bull, S.; Powell, M.; McIntyre, K. Can we reduce eating disorder risk factors in female college athletes? A randomized exploratory investigation of two peer-led interventions. Body Image 2012, 9, 31–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolanin, A.; Gross, M.; Hong, E. Depression in Athletes: Prevalence and risk factors. Curr. Sports Med. Rep. 2015, 14, 56–60. [Google Scholar] [CrossRef]
- Cox, D.T.C.; Shanahan, D.F.; Hudson, H.L.; Plummer, K.E.; Siriwardena, G.M.; Fuller, R.A.; Anderson, K.; Hancock, S.; Gaston, K.J. Doses of neighborhood nature: The benefits for mental health of living with nature. BioScience 2017, 67, 147–155. [Google Scholar] [CrossRef]
- Vaughan, R.S.; Edwards, E.J.; MacIntyre, T.E. Mental health measurement in a Post COVID-19 World: Psychometric properties and invariance of the DASS-21 in athletes and non-athletes. Front. Psychol. 2020, 11, 590559. [Google Scholar] [CrossRef]
- Buckley, G.; Hall, L.; Lassemillante, A.-C.; Belski, R. Disordered Eating & Body Image of Current and Former Athletes in a Pandemic-What Can We Learn From COVID-19 to Support Athletes Through Transitions? J. Eat Disord. 2021, 9, 73, in review. [Google Scholar]
- Sanborn, V.; Todd, L.; Schmetzer, H.; Manitkul-Davis, N.; Updegraff, J.; Gunstad, J. Prevalence of COVID-19 anxiety in division I student-athletes. J. Clin. Sport Psychol. 2021, 15, 162–176. [Google Scholar] [CrossRef]
- Akbaraly, T.N.; Brunner, E.J.; Ferrie, J.E.; Marmot, M.G.; Kivimaki, M.; Singh-Manoux, A. Dietary pattern and depressive symptoms in middle age. Br. J. Psychiatry J. Ment. Sci. 2009, 195, 408–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Lv, M.-R.; Wei, Y.-J.; Sun, L.; Zhang, J.-X.; Zhang, H.-G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef]
- Rao, T.S.S.; Asha, M.R.; Ramesh, B.N.; Rao, K.S.J. Understanding nutrition, depression and mental illnesses. Indian J. Psychiatry 2008, 50, 77–82. [Google Scholar] [CrossRef]
- Lai, J.S.; Hiles, S.; Bisquera, A.; Hure, A.; McEvoy, M.; Attia, J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am. J. Clin. Nutr. 2013, 99, 181–197. [Google Scholar] [CrossRef] [Green Version]
- Kim, W.K.; Shin, D.; Song, W.O. Are dietary patterns associated with depression in U.S. adults? J. Med. Food 2016, 19, 1074–1084. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Sánchez-Pedreño, F.O.; Van der Does, W.; Martínez-González, M.A. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Lange, K.W. Diet, exercise, and mental disorders—Public health challenges of the future. Mov. Nutr. Heal. Dis. 2018, 2. [Google Scholar] [CrossRef]
- Meng, X.; D’Arcy, C. Comorbidity between lifetime eating problems and mood and anxiety disorders: Results from the canadian community health survey of mental health and well-being. Eur. Eat. Disord. Rev. 2015, 23, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Joy, E.; Kussman, A.; Nattiv, A. 2016 update on eating disorders in athletes: A comprehensive narrative review with a focus on clinical assessment and management. Br. J. Sports Med. 2016, 50, 154–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ackerman, K.; Stellingwerff, T.; Elliott-Sale, K.J.; Baltzell, A.; Cain, M.; Goucher, K.; Fleshman, L.; Mountjoy, M.L. #REDS (Relative Energy Deficiency in Sport): Time for a revolution in sports culture and systems to improve athlete health and performance. Br. J. Sports Med. 2020, 54, 369–370. [Google Scholar] [CrossRef]
- Rossi, K.A. Nutritional aspects of the female athlete. Clin. Sports Med. 2017, 36, 627–653. [Google Scholar] [CrossRef]
- Bratland-Sanda, S.; Sundgot-Borgen, J. Eating disorders in athletes: Overview of prevalence, risk factors and recommendations for prevention and treatment. Eur. J. Sport Sci. 2013, 13, 499–508. [Google Scholar] [CrossRef]
- Krebs, P.A.; Dennison, C.R.; Kellar, L.; Lucas, J. Gender differences in eating disorder risk among NCAA division i cross country and track student-athletes. J. Sports Med. 2019, 2019, 5035871. [Google Scholar] [CrossRef] [Green Version]
- Sundgot-Borgen, J.; Torstveit, M.K. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin. J. Sport Med. 2004, 14, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Sysko, R.; Glasofer, D.R.; Hildebrandt, T.; Klimek, P.; Mitchell, J.E.; Berg, K.C.; Peterson, C.B.; Wonderlich, S.A.; Walsh, B.T. The eating disorder assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. Int. J. Eat. Disord. 2015, 48, 452–463. [Google Scholar] [CrossRef] [Green Version]
- Greenleaf, C.; Petrie, T. Eating Disorders. In Routledge Companion to Sport and Exercise Psychology: Global Perspectives and Fundamental Concepts; International Perspectives on Key Issues in Sport and Exercise Psychology; Routledge/Taylor & Francis Group: New York, NY, USA, 2014; pp. 837–851. ISBN 978-1-84872-128-9. [Google Scholar]
- Clifford, T.; Blyth, C. A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in University sports teams. Eat. Weight. Disord.-Stud. Anorex.Bulim. Obes. 2019, 24, 473–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Power, K.; Kovacs, S.; Butcher-Poffley, L.; Wu, J.; Sarwer, D. Disordered eating and compulsive exercise in collegiate athletes: Applications for sport and research. Sport J. 2020, 21, 1–29. [Google Scholar]
- Petrie, T.A.; Greenleaf, C.; Reel, J.; Carter, J. Prevalence of eating disorders and disordered eating behaviors among male collegiate athletes. Psychol. Men Masc. 2008, 9, 267–277. [Google Scholar] [CrossRef] [Green Version]
- Lis, D.; Stellingwerff, T.; Shing, C.M.; Ahuja, K.; Fell, J. Exploring the popularity, experiences, and beliefs surrounding gluten-free diets in nonceliac athletes. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Devrim-Lanpir, A.; Hill, L.; Knechtle, B. Efficacy of popular diets applied by endurance athletes on sports performance: Beneficial or detrimental? A narrative review. Nutrients 2021, 13, 491. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, M.; Sundgot-Borgen, J.K.; Burke, L.M.; Ackerman, K.E.; Blauwet, C.; Constantini, N.; Lebrun, C.; Lundy, B.; Melin, A.K.; Meyer, N.L.; et al. IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br. J. Sports Med. 2018, 52, 687–697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petkus, D.L.; Murray-Kolb, L.E.; De Souza, M.J. The unexplored crossroads of the female athlete triad and iron deficiency: A narrative review. Sports Med. 2017, 47, 1721–1737. [Google Scholar] [CrossRef]
- Mountjoy, M.; Sundgot-Borgen, J.; Burke, L.M.; Carter, S.; Constantini, N.; Lebrun, C.; Meyer, N.; Sherman, R.; Steffen, K.; Budgett, R.; et al. The IOC consensus statement: Beyond the female athlete triad—Relative Energy Deficiency in sport (RED-S). Br. J. Sports Med. 2014, 48, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Lester, David Mind, Body and Sport: Suicidal Tendencies|NCAA.Org—The Official Site of the NCAA. Available online: https://www.ncaa.org/sport-science-institute/mind-body-and-sport-suicidal-tendencies (accessed on 25 October 2021).
- Wolanin, A.; Gross, M.; Marks, D.; Panchoo, K.; Gross, M. Prevalence of Clinically Elevated Depressive Symptoms in College Athletes and Differences by Gender and Sport|British Journal of Sports Medicine. Available online: https://bjsm.bmj.com/content/50/3/167 (accessed on 25 October 2021).
- Rice, S.M.; Parker, A.; Mawren, D.; Clifton, P.; Harcourt, P.; Lloyd, M.; Kountouris, A.; Smith, B.; McGorry, P.D.; Purcell, R. Preliminary psychometric validation of a brief screening tool for athlete mental health among male elite athletes: The Athlete Psychological Strain Questionnaire. Int. J. Sport Exerc. Psychol. 2019, 18, 1–16. [Google Scholar] [CrossRef]
- Morrey, L.B.; Roberts, W.O.; Wichser, L. Exercise-related Mental Health Problems and Solutions during the COVID-19 Pandemic. Curr. Sports Med. Rep. 2020, 19, 194–195. [Google Scholar] [CrossRef] [PubMed]
- NCAA Student-Athlete Well-Being Study. Available online: https://www.ncaa.org/about/resources/media-center/news/survey-shows-student-athletes-grappling-mental-health-issues (accessed on 29 October 2021).
- Soubliere, D.; Gitimu, P. Female athletes and eating disorders|The Sport Journal. Available online: https://thesportjournal.org/article/female-athletes-and-eating-disorders/ (accessed on 1 December 2021).
- Rice, S.M.; Gwyther, K.; Santesteban-Echarri, O.; Baron, D.; Gorczynski, P.; Gouttebarge, V.; Reardon, C.L.; Hitchcock, M.E.; Hainline, B.; Purcell, R. Determinants of anxiety in elite athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 722–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute of Mental Health (NIMH). Available online: https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-institute-mental-health-nimh (accessed on 29 October 2021).
- Subar, A.F.; Thompson, F.E.; Kipnis, V.; Midthune, D.; Hurwitz, P.; McNutt, S.; McIntosh, A.; Rosenfeld, S. Comparative validation of the block, willett, and national cancer institute food frequency questionnaires the eating at America’s table study. Am. J. Epidemiol. 2001, 154, 1089–1099. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J.G. Development and initial validation of the COVID stress scales. J. Anxiety Disord. 2020, 72, 102232. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Kipnis, V.; Troiano, R.; Midthune, D.; Schoeller, D.A.; Bingham, S.; Sharbaugh, C.O.; Trabulsi, J.; Runswick, S.; Ballard-Barbash, R.; et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: The open study. Am. J. Epidemiol. 2003, 158, 1–13. [Google Scholar] [CrossRef]
- Sunami, A.; Sasaki, K.; Suzuki, Y.; Oguma, N.; Ishihara, J.; Nakai, A.; Yasuda, J.; Yokoyama, Y.; Yoshizaki, T.; Tada, Y.; et al. Validity of a semi-quantitative food frequency questionnaire for collegiate athletes. J. Epidemiol. 2016, 26, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Reardon, C.L.; Factor, R.M. Sport psychiatry. Sports Med. 2010, 40, 961–980. [Google Scholar] [CrossRef] [PubMed]
- de Bruin, A.P.; Oudejans, R.R.D.; Bakker, F.C.; Woertman, L. Contextual body image and athletes’ disordered eating: The contribution of athletic body image to disordered eating in high performance women athletes. Eur. Eat. Disord. Rev. 2011, 19, 201–215. [Google Scholar] [CrossRef] [Green Version]
- Smith, K.; Harmon, M. Body Image of Collegiate Athletes: Its key factors. Int. J. Exerc. Sci. Conf. Proc. 2021, 2, 77. [Google Scholar]
- Torres-McGehee, T.M.; Pritchett, K.L.; Zippel, D.; Minton, D.M.; Cellamare, A.; Sibilia, M. Sports nutrition knowledge among collegiate athletes, coaches, athletic trainers, and strength and conditioning specialists. J. Athl. Train. 2012, 47, 205–211. [Google Scholar] [CrossRef] [Green Version]
- Chang, C.; Putukian, M.; Aerni, G.; Diamond, A.; Hong, G.; Ingram, Y.; Reardon, C.L.; Wolanin, A. Mental health issues and psychological factors in athletes: Detection, management, effect on performance and prevention: American Medical Society for Sports Medicine Position Statement—Executive Summary. Br. J. Sports Med. 2019, 54, 216–220. [Google Scholar] [CrossRef] [PubMed]
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Exercise Physiology: Nutrition, Energy, and Human Performance; Wolters Kluwer Health/Lippincott Williams & Wilkins: Baltimore, Maryland, 2015. [Google Scholar]
- Turocy, P.S.; DePalma, B.F.; Horswill, C.A.; Laquale, K.M.; Martin, T.J.; Perry, A.C.; Somova, M.J.; Utter, A.C. National athletic trainers’ association position statement: Safe weight loss and maintenance practices in sport and exercise. J. Athl. Train. 2011, 46, 322–336. [Google Scholar] [CrossRef] [Green Version]
- Wallner-Liebmann, S.J.; Kruschitz, R.; Hübler, K.; Hamlin, M.; Schnedl, W.; Moser, M.; Tafeit, E. A measure of obesity: BMI versus subcutaneous fat patterns in young athletes and nonathletes. Coll. Antropol. 2013, 37, 351–357. [Google Scholar] [PubMed]
- Bulik, C.M.; Marcus, M.D.; Zerwas, S.; Levine, M.; La Via, M. The Changing “Weightscape” of bulimia nervosa. Am. J. Psychiatry 2012, 169, 1031–1036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Revilla, M.; Ochoa, C. Ideal and maximum length for a web survey. Int. J. Mark. Res. 2017, 59, 557–565. [Google Scholar] [CrossRef]
- Pinkerton, J.V.; Guico-Pabia, C.J.; Taylor, H.S. Menstrual cycle-related exacerbation of disease. Am. J. Obstet. Gynecol. 2010, 202, 221–231. [Google Scholar] [CrossRef]
- Fukushima, K.; Fukushima, N.; Sato, H.; Yokota, J.; Uchida, K. Association between nutritional level, menstrual-related symptoms, and mental health in female medical students. PLoS ONE 2020, 15, e0235909. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, M.; Trambacz-Oleszak, S. The Association between menstrual cycle characteristics and perceived body image: A cross-sectional survey of polish female adolescents. J. Biosoc. Sci. 2016, 48, 374–390. [Google Scholar] [CrossRef] [PubMed]
| Study Variable | |
|---|---|
| mean (SD) | |
| Age | 19.3 (1.46) |
| n (%) | |
| Year | |
| First year (Freshman) | 25 (32.91) |
| Second year (Sophomore) | 14 (17.72) |
| Third year (Junior) | 21 (26.58) |
| Fourth and Fifth year (Senior) | 17 (22.78) |
| Race | |
| Non-Hispanic White | 54 (68.35) |
| Non-Hispanic Black | 3 (3.80) |
| Hispanic | 7 (7.59) |
| Other | 16 (20.25) |
| Sport | |
| Volleyball | 12 (15.19) |
| Basketball | 11 (13.92) |
| Softball | 17 (21.52) |
| Tennis | 8 (10.13) |
| Track and Field/Cross Country | 10 (12.66) |
| Soccer | 21 (26.58) |
| Current Living Situation | |
| On-Campus | 28 (35.44) |
| Off-Campus | 50 (63.29) |
| With Parents | 1 (1.27) |
| Married | |
| Yes | 2 (2.53) |
| No | 75 (97.47) |
| Living Situation from March 2020-July 2020 | |
| On-Campus | 4 (5.06) |
| Off-Campus with roommates | 16 (20.25) |
| At home with family | 53 (67.09) |
| Other | 6 (7.59) |
| Working a job outside of sport and schooling | |
| Yes | 13 (16.46) |
| No | 66 (83.54) |
| Do you have an Eating Disorder? | |
| Yes | 2 (2.53) |
| No | 75 (97.47) |
| If yes, has your ED been diagnosed by a doctor? | |
| Yes | |
| No | 2 (100) |
| Did COVID create financial hardship for you? | |
| Yes | 16 (20.25) |
| No | 63 (79.75) |
| Were you able to maintain your normal, pre-competition diet during quarantine? | |
| Yes | 52 (65.82) |
| No | 27 (34.18) |
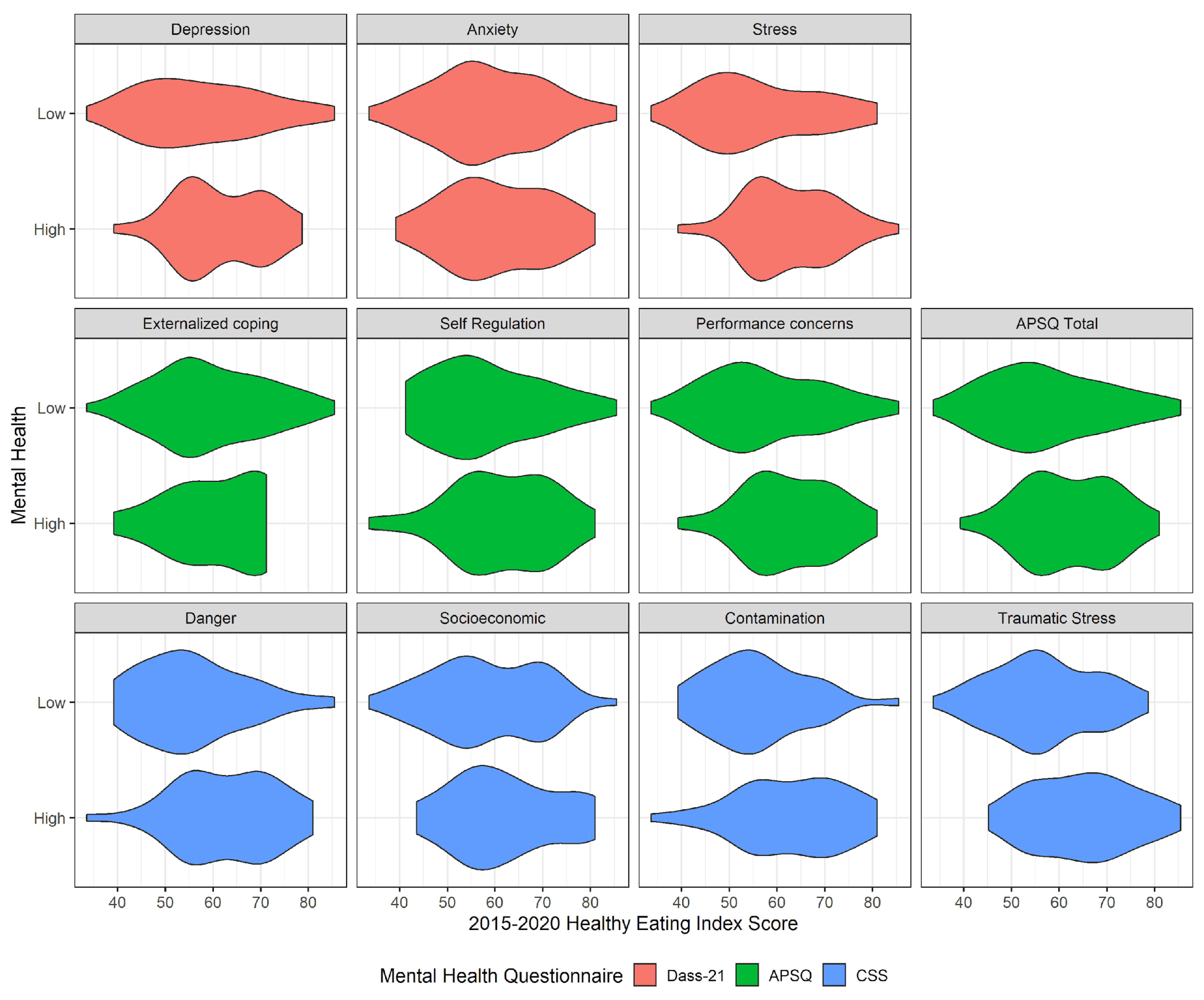
| n (%) | HEI, Mean (SD) | p-Value | |
|---|---|---|---|
| DASS-21 * | |||
| Depression | 0.109 | ||
| Low (<8) | 36 (46.8) | 57.5 (12.8) | |
| High (8+) | 41 (53.2) | 61.7 (9.5) | |
| Anxiety | 0.511 | ||
| Low (<3) | 37 (48.1) | 58.8 (11.8) | |
| High (3+) | 40 (51.9) | 60.6 (10.9) | |
| Stress | 0.015 | ||
| Low (<8) | 34 (44.2) | 56.1 (12.4) | |
| High (8+) | 43 (55.8) | 62.6 (9.5) | |
| APSQ * | |||
| Externalized Coping | 0.765 | ||
| Low (<3) | 64 (83.1) | 59.6 (11.5) | |
| High (3+) | 13 (16.9) | 60.5 (10.2) | |
| Self-Regulation | 0.218 | ||
| Low (<10) | 40 (51.9) | 58.2 (11.6) | |
| High (10+) | 37 (48.1) | 61.4 (10.8) | |
| Performance Concerns | 0.048 | ||
| Low (<9) | 43 (55.8) | 57.5 (12.1) | |
| High (9+) | 34 (44.2) | 62.5 (9.6) | |
| APSQ Total | 0.082 | ||
| Low (<20) | 38 (49.4) | 57.5 (12.4) | |
| High (20+) | 39 (50.6) | 61.9 (9.7) | |
| CSS * | |||
| Danger | 0.007 | ||
| Low (<4) | 34 (44.2) | 55.9 (11.1) | |
| High (4+) | 43 (55.8) | 62.8 (10.6) | |
| Socioeconomic Consequences | 0.151 | ||
| Low (<2) | 45 (58.4) | 58.2 (11.4) | |
| High (2+) | 32 (41.6) | 61.9 (10.9) | |
| Contamination | 0.006 | ||
| Low (=0) | 36 (46.8) | 56.0 (10.2) | |
| High (1+) | 41 (53.2) | 63.0 (11.3) | |
| Traumatic Stress | 0.003 | ||
| Low (=0) | 50 (64.9) | 56.9 (10.7) | |
| High (1+) | 27 (35.1) | 64.9 (10.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christensen, N.; van Woerden, I.; Aubuchon-Endsley, N.L.; Fleckenstein, P.; Olsen, J.; Blanton, C. Diet Quality and Mental Health Status among Division 1 Female Collegiate Athletes during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 13377. https://doi.org/10.3390/ijerph182413377
Christensen N, van Woerden I, Aubuchon-Endsley NL, Fleckenstein P, Olsen J, Blanton C. Diet Quality and Mental Health Status among Division 1 Female Collegiate Athletes during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(24):13377. https://doi.org/10.3390/ijerph182413377
Chicago/Turabian StyleChristensen, Natalie, Irene van Woerden, Nicki L. Aubuchon-Endsley, Pamela Fleckenstein, Janette Olsen, and Cynthia Blanton. 2021. "Diet Quality and Mental Health Status among Division 1 Female Collegiate Athletes during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 24: 13377. https://doi.org/10.3390/ijerph182413377
APA StyleChristensen, N., van Woerden, I., Aubuchon-Endsley, N. L., Fleckenstein, P., Olsen, J., & Blanton, C. (2021). Diet Quality and Mental Health Status among Division 1 Female Collegiate Athletes during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(24), 13377. https://doi.org/10.3390/ijerph182413377






