Moral Distress Trajectories of Physicians 1 Year after the COVID-19 Outbreak: A Grounded Theory Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants’ Recruiting
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Participants
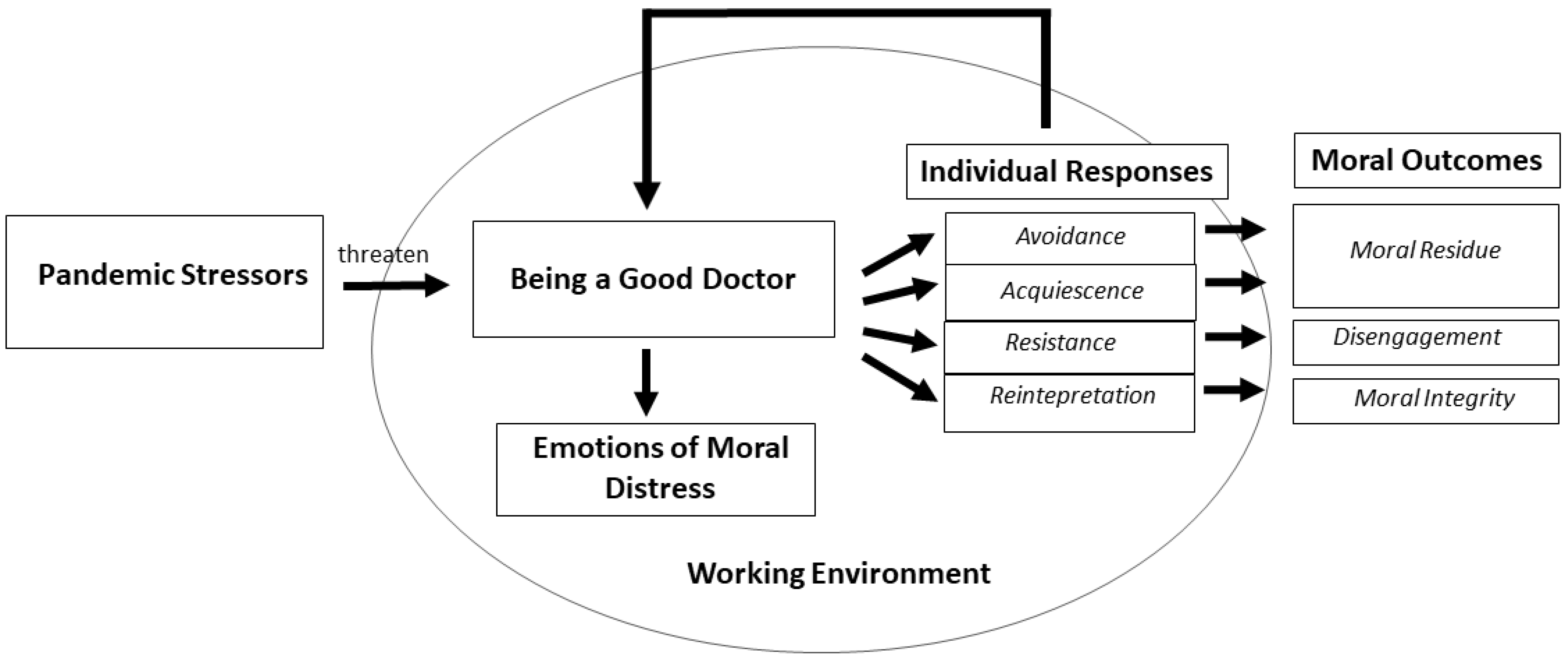
3.2. Model of the Moral Distress Process
3.2.1. Pandemic Stressors
- Limited Healthcare Resources. One of the main factors that caused moral distress was the experience that resources were woefully inadequate: not enough oxygen, not enough ICU beds, not enough physicians. The stressful experience of working with limited resources was a difficult shift, and fostered the sense of not providing good care. “We didn’t have any more beds in the ICU, we found ourselves distributing opioid to do palliative care to people who normally we would have saved”. #12.
- Intensified Patient Triage. In the context of limited healthcare resources, physicians were confronted with the struggle of triaging patients. Although the experience of triage was familiar to many, it was extraordinarily difficult because of the sheer volume of consequential decisions to make, and triage criteria that differed from pre-pandemic standards. “There was a time during which we assessed nearly 250 patients a day…We lowered the standard of care at that point and that was difficult for me to bear.” #6. “I felt like a judge who should play God and say: «You live, you die». I became like a robot to survive.” #2.
- Changeable Selection Criteria. Another distressing factor was the lack of consistency of the selection criteria due to the rapid changes in knowledge about the disease, or to the different interpretation of selection criteria within the team. The changeable selection criteria led to a deep sense of injustice. “For me the lack of fairness was unjustifiable because every day they changed the cards on the table. If you had a particularly wired colleague (on the shift before you) who occupied all the beds and ventilators, then you had nothing left for the other patients. There are rules that apply to everyone. Otherwise, it’s all random!” #9.
- Limited Therapeutic/Clinical Knowledge. Many physicians reported that acting in the context of limited knowledge of the disease and therapeutics was a source of moral distress. Oftentimes the limited clinical knowledge led to the use of drugs and/or procedures without sufficient clinical evidence, thereby risking damage to patients. “Sometimes, we do damage that is irreversible because there is still no guideline, there is no standardized procedure, there is no blood gas reference to say now you better intubate, now no.” #14.
- Patient Isolation. Another factor triggering moral distress was patient isolation and the separation from family members during such meaningful moments as during the end-of-life. Many physicians found themselves as witness to patients’ loneliness, and thrust into intimate moments at the end-of-life, further amplifying moral distress. “I remember a patient with whom we were doing palliation. One evening, at the end of my shift, I saw him looking at a yellow frame containing photos of his children and grandchildren. He was crying, aware that he would die. He died the next day and only I witnessed this scene. I still carry the scene with me like a flash of sadness. Maybe we could have done more to connect him with his family, other than video calls.” #6.
3.2.2. Emotions of Moral Distress
- Powerlessness and Inadequacy. The predominant feeling related to the experience of moral distress was a deep sense of powerlessness to provide care that could be considered as adequate. “Our weapons par excellence are the endotracheal tubes and the ventilators. We used them but it was like water for the patients. It didn’t change anything. I remember sudden deaths without the possibility of doing anything. It’s the powerlessness that comes to the surface.” #14.
- Frustration and Anger. The impossibility of upholding the standard of care or acting according to one’s conscience was often followed by frustration and anger. “Every day we asked for supplies. We asked for anything in order not to see people die, but there were no resources! So, I was a frustrated person.” #4.
- Sadness. Many physicians described sadness when witnessing overwhelming situations where they felt impotent to fulfill their vision of what it meant to Be a Good Doctor. Sadness emerged as an intimate response when bearing witness to human suffering on such a massive scale. “During the very first days…I heard only the sound of sirens, the beds seemed to be never enough, the patients were going very bad, they dropped like flies. Those days I said crying: «It will be a massacre!» I really had to say that I was suffering for humankind.” #1.
3.2.3. Individual Responses
- Avoidance. Some physicians tried to protect themselves by avoiding exposure to morally stressful conditions or tasks, such as communicating with patients’ family members by phone. Others, especially during triage, avoided human contact with critical patients to mitigate moral distress. “I was so exhausted that I didn’t want to look patients in the face anymore. I could not make it to see the umpteenth patient who did not breathe. For this reason, I used to take the patient’s chart…and I would say: «This one is to be intubated, this one is not».” #2.
- Acquiescence. Another response to moral distress was to passively follow the orders, and accept the realities without challenging them. Faced with the incongruence between their own values and the grim reality, some physicians silenced and disregarded their professional values in order to accommodate with the situation. “I remember a recent young patient, who arrived in the ED, suffering from a tumor with a poor prognosis. He was probably also affected by COVID because he had the characteristic symptoms, but my colleagues did not want to test him for COVID to discharge him quickly and prevent him from occupying an additional bed, given the poor prognosis. I felt very guilty towards the patient and his family.” #3.
- Resistance. Another possible response was proactive resistance to situations or orders that were perceived as morally wrong. Confronted with the incongruence between one’s own values and the desperate reality, some physicians spoke up to their superiors, and further expressed concern about morally questionable practices or behaviors. Some issued formal complaints to political institutions, and/or proposed new healthcare procedures, whereas others, in specific situations, disregarded certain rules perceived as unethical. “Unfortunately, the approach was “We are at war. There are generals and there are soldiers: soldiers obey what the generals say. Therefore, it was necessary to carry out even improper orders that had to do with the death of people. I had several fights due to the fact that I just couldn’t handle some of the orders.” #8.
- Reinterpretation. Another possible response among physicians was to reinterpret their role as a Good Doctor by reframing the reality, recognizing the exceptional circumstances, and engaging their creativity to achieve different ways to care for patients. This creative, adaptive process required deep emotional labor. “In the first week when I put the patients naked in a black sack, I suffered, and I asked myself “With my being a doctor, what can I preserve and what might I be able to change?” And from there, I started to write my name on the gown, so that the patients knew who I was, to take care of the daily phone calls to relatives… and to fight at the Ministry of Health so that the deceased could be put dressed in the sacks. I prayed for them while we closed the sack. Well, I don’t know if these things helped the patients, but they helped me! I started to regain my sense of purpose again with the things I believed in with all of myself.” #1.
3.2.4. Working Environment
- Team Culture. The team culture to which physicians belonged served to modulate moral distress. For some, a supportive team, which was open to discussion, permitted physicians not to feel abandoned while struggling with moral distress. “I worked in a very organized structure with a group of culturally prepared people, some of whom are old friends. I believe that having the technical and human resources (available), helped me not to feel inadequate.” #1. On the contrary, physicians who worked within less supportive team cultures reported a sense of loneliness and responsibility that amplified moral distress.
- Organizational Culture. Organizational culture also played a prominent role in modulating physicians’ moral distress. Physicians who perceived their organization as supportive, oriented to listening, and motivated to respond to the problems arising during the pandemic reported diminished moral distress. On the contrary, physicians who perceived their organization as repressive, “military oriented”, and unresponsive to suggestions reported an exacerbation of the moral distress emotional experience, which easily led to disengagement. “You work a lot, but you think little. And this thing here during the pandemic has become devastating. The mantra was: «You don’t have to think. Act because I think for you.» But when in complex situations you stop thinking then you do atrocious things.”#8.
3.2.5. Moral Outcomes
- Moral Residue. Some physicians, especially those who utilized avoidance or acquiescence in response to moral distress, and who experienced a hierarchical, individualistic, or rigid work environment, reported lingering feelings of shame, regret, self-doubt, and guilt for not being able to act differently to effect change as if they should have been able to do so. “I felt dirty, ugly inside having to say “No, there are no beds”. I would go home and cry. I had come to not want to see my daughter anymore. I didn’t want to see my face next to hers in the video call. I felt like I was dirtying her.” #9.
- Disengagement. Some physicians reported feelings of loneliness, resignation, disillusionment, and lack of motivation, especially those who used resistance as the main response to moral distress, and who perceived their Working Environment as hierarchical, individualistic, and unresponsive to their suggestions. As a result, some physicians felt emotionally disengaged from the hospital, with a withdrawal in energy and a diminished sense of belonging. Disengagement was followed by the desire to change positions, or to leave the hospital and the profession altogether. “The long wake of this situation was a detachment from the hospital management, a divestment, a disillusionment. Before COVID the hospital was like my home, now it’s a rented house.” #12.
- Moral integrity. Some physicians, especially those who used reinterpretation in response to moral distress, and who perceived the Working Environment as participatory, collaborative, and receptive to suggestions, reported moral integrity and a restored sense of Being a Good Doctor. They described having been challenged, but emerging with a feeling of integrity, wholeness, and peace of conscience. “We don’t always manage to cure but we can always care for. This helped me to preserve my wholeness during the pandemic because even on the worst days it can be honorable…knowing that you have done things right.” #1.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19) Situation Report. Available online: http://www.who.it/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 2 July 2021).
- Vergano, M.; Bertolini, G.; Giannini, A.; Gristina, G.R.; Livigni, S.; Mistraletti, G.; Riccioni, L.; Petrini, F. Clinical ethics recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances: The Italian perspective during the COVID-19 epidemic. Crit. Care 2020, 24, 1–3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nacoti, M.; Ciocca, A.; Giupponi, A.; Brambillasca, P.; Lussana, F.; Pisano, M.; Goisis, G.; Bonacina, D.; Fazzi, F.; Naspro, R.; et al. At the Epicenter of the COVID-19 Pandemic and humanitarian crises in Italy: Changing perspectives on preparation and mitigation. NEJM Catal. Innov. Care Deliv. 2020, 1, 1–5. [Google Scholar]
- Paterlini, M. On the front lines of coronavirus: The Italian response to COVID-9. BMJ 2020, 368, m1065. [Google Scholar] [CrossRef] [Green Version]
- Pennestrì, F.; Gaudioso, A.; Jani, A.; Bottinelli, E.; Banfi, G. Is administered competition suitable for dealing with a public health emergency? Lessons from the local healthcare system at the centre of early COVID-19 outbreak in Italy. Central Eur. J. Public Health 2021, 29, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Curley, M.A.Q.; Broden, E.G.; Meyer, E.C. Alone, the hardest part. Intensive Care Med. 2020, 46, 1974–1976. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, 1. [Google Scholar] [CrossRef] [Green Version]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Donkers, M.A.; Gilissen, V.J.; Candel, M.J.; van Dijk, N.M.; Kling, H.; Heijnen-Panis, R.; Pragt, E.; van der Horst, I.; Pronk, S.A.; van Mook, W.N.K.A. Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Med. Ethics 2021, 22, 1–12. [Google Scholar] [CrossRef]
- Kok, N.; Hoedemaekers, A.; van der Hoeven, H.; Zegers, M.; van Gurp, J. Recognizing and supporting morally injured ICU professionals during the COVID-19 pandemic. Intensive Care Med. 2020, 46, 1653–1654. [Google Scholar] [CrossRef]
- Jameton, A. Nursing Practice: The Ethical Issues; Prentice-Hall: Englewood Cliffs, NJ, USA, 1984. [Google Scholar]
- Batho, D.; Pitton, C. What Is Moral Distress? Experiences and Responses. Available online: https://powerlessness.essex.ac.uk/wp-content/uploads/2018/02/MoralDistressGreenPaper1.pdf (accessed on 1 July 2021).
- Epstein, E.; Hamric, A.B. Moral distress, moral residue, and the crescendo effect. J. Clin. Ethics 2009, 20, 330–342. [Google Scholar]
- Webster, G.; Bayliss, F. Moral Residue. In Margin of Error: The Ethics of Mistakes in the Practice of Medicine; Rubin, S.B., Zoloth, L., Eds.; University Publishing Group: Hagerstown, MD, USA, 2000. [Google Scholar]
- Wilkinson, J.M. Moral distress in nursing practice: Experience and effect. Nurs. Forum. 1987, 23, 16–29. [Google Scholar] [CrossRef] [PubMed]
- Lamiani, G.; Dordoni, P.; Argentero, P. Value congruence and depressive symptoms among critical care clinicians: The mediating role of moral distress. Stress Health 2018, 34, 135–142. [Google Scholar] [CrossRef]
- Fumis, R.R.L.; Amarante, G.A.J.; Nascimento, A.D.F.; Junior, J.M.V. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann. Intensive Care 2017, 7, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Naboureh, A.; Imanipour, M.; Salehi, T. Moral distress and intention to leave intensive care units: A correlational study. Clin. Ethics 2021, 16, 234–239. [Google Scholar] [CrossRef]
- Glaser, G.B.; Strauss, L.A. The Discovery of Grounded Theory: Strategies for Qualitative Research; Aldine Publishing Company: New Brunswick, QC, Canada, 1967. [Google Scholar]
- Strauss, A.; Corbin, J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques, 2nd ed.; SAGE Publications Inc.: London, UK, 1990. [Google Scholar]
- Wocial, L.D.; Weaver, M.T. Development and psychometric testing of a new tool for detecting moral distress: The Moral Distress Thermometer. J. Adv. Nurs. 2013, 69, 167–174. [Google Scholar] [CrossRef]
- Lamiani, G.; Giannini, A.; Fossati, I.; Prandi, E.; Vegni, E. Parental experience of end-of life care in the pediatric intensive care unit. Minerva Anestesiol 2013, 79, 1334–1343. [Google Scholar] [PubMed]
- Rogers, C.R. Client-Centered Therapy: Its Current Practice, Implications and Theory; Constable: London, UK, 1951. [Google Scholar]
- Charmaz, K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis; SAGE Publications Inc.: London, UK, 2006. [Google Scholar]
- Hallberg, L.R.-M. The “core category” of grounded theory: Making constant comparisons. Int. J. Qual. Stud. Health Well-Being 2006, 1, 141–148. [Google Scholar] [CrossRef] [Green Version]
- Kanaris, C. Moral distress in the intensive care unit during the pandemic: The burden of dying alone. Intensive Care Med. 2021, 47, 141–143. [Google Scholar] [CrossRef]
- Mistraletti, G.; Gristina, G.; Mascarin, S.; Iacobone, E.; Giubbilo, I.; Bonfanti, S.; Fiocca, F.; Fullin, G.; Fuselli, E.; Bocci, M.G.; et al. How to communicate with families living in complete isolation. BMJ Support. Palliat. Care 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hamric, A.B.; Borchers, C.T.; Epstein, E. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Prim. Res. 2012, 3, 1–9. [Google Scholar] [CrossRef]
- Boulton, A.J.; Yeung, J.; Bassford, C.; Slowther, A.M. Moral Distress amongst Intensive Care Unit Professions in the UK: A Qualitative Study. rs.3.rs:764234. [Preprint]. [Posted 5 August 2021]. Available online: https://www.researchsquare.com/article/rs-764234/v1 (accessed on 28 August 2021).
- Lamiani, G.; Setti, I.; Barlascini, L.; Vegni, E.; Argentero, P. Measuring moral distress among critical care clinicians: Validation and psychometric properties of the Italian Moral Distress Scale-Revised. Crit. Care Med. 2017, 45, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Smallwood, N.; Pascoe, A.; Karimi, L.; Willis, K. Moral distress and perceived community views are associated with mental health symptoms in frontline health workers during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 8723. [Google Scholar] [CrossRef]
- Carse, A.; Rushton, C.H. Harnessing the promise of moral distress: A Call for re-orientation. J. Clin. Ethics 2017, 28, 15–29. [Google Scholar]
- Rushton, C.H. Moral resilience. In Transforming Moral Suffering in Healthcare; Oxford University: New York, NY, USA, 2018; p. 26. [Google Scholar]
- Villa, G.; Pennestrì, F.; Rosa, D.; Giannetta, N.; Sala, R.; Mordacci, R.; Manara, D.F. Moral distress in community and hospital settings for the care of elderly people. A grounded theory qualitative study. Healthcare 2021, 9, 1307. [Google Scholar] [CrossRef]
- Pauly, B.; Varcoe, C.; Storch, J.; Newton, L. Registered nurses’ perceptions of moral distress and ethical climate. Nurs. Ethics 2009, 16, 561–573. [Google Scholar] [CrossRef]
- Bruce, C.R.; Miller, S.M.; Zimmerman, J.L. A qualitative study exploring moral distress in the ICU team: The importance of unit functionality and intrateam dynamics. Crit. Care Med. 2015, 43, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Garros, D.; Austin, W.; Carnevale, F. Moral distress in Pediatric Intensive Care. JAMA Pediatr. 2015, 169, 885–886. [Google Scholar] [CrossRef]
- Prentice, T.M.; Gillam, L.; Davis, P.G.; Janvier, A. Always a burden? Healthcare providers’ perspectives on moral distress. Arch. Dis. Child.-Fetal Neonatal Ed. 2018, 103, F441–F445. [Google Scholar] [CrossRef]
- Sabin, J.E. Using Moral Distress for Organizational Improvement. J. Clin. Ethics 2017, 28, 33–36. [Google Scholar] [PubMed]
- van Schaik, M.V.; Pasman, H.R.; Widdershoven, G.; Molewijk, B.; Metselaar, S. CURA—An ethics support instrument for nurses in palliative care. Feasibility and first perceived outcomes. HEC Forum 2021. Advance online publication. [Google Scholar] [CrossRef]
| Order | Questions |
|---|---|
| 1 | Moral distress has been defined as the distress experienced when you feel you cannot act according to what you think is correct/right in your profession. Does this experience resonate with you during this pandemic time in any way? |
| 2 | Do you recall a situation, since the beginning of the pandemic, where you think you experienced moral distress? |
| 3 | How did you feel in that situation? |
| 4 | What helped you to navigate/cope with that situation? |
| Partecipant Code | Sex | Age | Experience (Years) | Work Setting during Pandemic | Role | Triage Responsibility (Yes/No) | Number of COVID-19 Patients Assisted | Moral Distress Score (0–10) |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 44 | 19 | ICU | Attending | No | 50–100 | 1 |
| 2 | F | 49 | 24 | ED | Attending | Yes | 50–100 | 7 |
| 3 | F | 32 | 6 | ED | Consultant | No | >200 | 6 |
| 4 | F | 51 | 22 | ICU and sub-intensive | Chief | Yes | >200 | 2 |
| 5 | M | 50 | 10 | ICU | Attending | Yes | 100–200 | 3 |
| 6 | M | 45 | 19 | ICU | Attending | Yes | >200 | 5 |
| 7 | M | 48 | 23 | ICU | Attending | Yes | 100–200 | 1 |
| 8 | M | 42 | 15 | ED | Attending | Yes | 100–200 | 8 |
| 9 | M | 55 | 30 | ICU | Chief | Yes | 100–200 | 6 |
| 10 | F | 41 | 15 | ED | Attending | No | >200 | 7 |
| 11 | M | 46 | 20 | ICU | Attending | No | 50–100 | 5 |
| 12 | F | 43 | 10 | ICU and ALS vehicle | Attending | Yes | >200 | 8 |
| 13 | F | 46 | 18 | ICU | Attending | No | >200 | 5 |
| 14 | F | 47 | 22 | ED | Chief | Yes | >200 | 2 |
| 15 | F | 51 | 24 | ICU | Attending | Yes | >200 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamiani, G.; Biscardi, D.; Meyer, E.C.; Giannini, A.; Vegni, E. Moral Distress Trajectories of Physicians 1 Year after the COVID-19 Outbreak: A Grounded Theory Study. Int. J. Environ. Res. Public Health 2021, 18, 13367. https://doi.org/10.3390/ijerph182413367
Lamiani G, Biscardi D, Meyer EC, Giannini A, Vegni E. Moral Distress Trajectories of Physicians 1 Year after the COVID-19 Outbreak: A Grounded Theory Study. International Journal of Environmental Research and Public Health. 2021; 18(24):13367. https://doi.org/10.3390/ijerph182413367
Chicago/Turabian StyleLamiani, Giulia, Davide Biscardi, Elaine C. Meyer, Alberto Giannini, and Elena Vegni. 2021. "Moral Distress Trajectories of Physicians 1 Year after the COVID-19 Outbreak: A Grounded Theory Study" International Journal of Environmental Research and Public Health 18, no. 24: 13367. https://doi.org/10.3390/ijerph182413367
APA StyleLamiani, G., Biscardi, D., Meyer, E. C., Giannini, A., & Vegni, E. (2021). Moral Distress Trajectories of Physicians 1 Year after the COVID-19 Outbreak: A Grounded Theory Study. International Journal of Environmental Research and Public Health, 18(24), 13367. https://doi.org/10.3390/ijerph182413367







