Risk Assessment on Suicide Death and Attempt among Chinese Rural Youths Aged 15–34 Years
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample and the General Design
2.2. Interview Procedure
2.3. Measures
2.4. Ethics Statement
2.5. Statistical Methods
3. Results
3.1. Study Samples
3.2. Suicide Risk Assessment Model
3.3. Validity of The Assessment Model among Training Samples
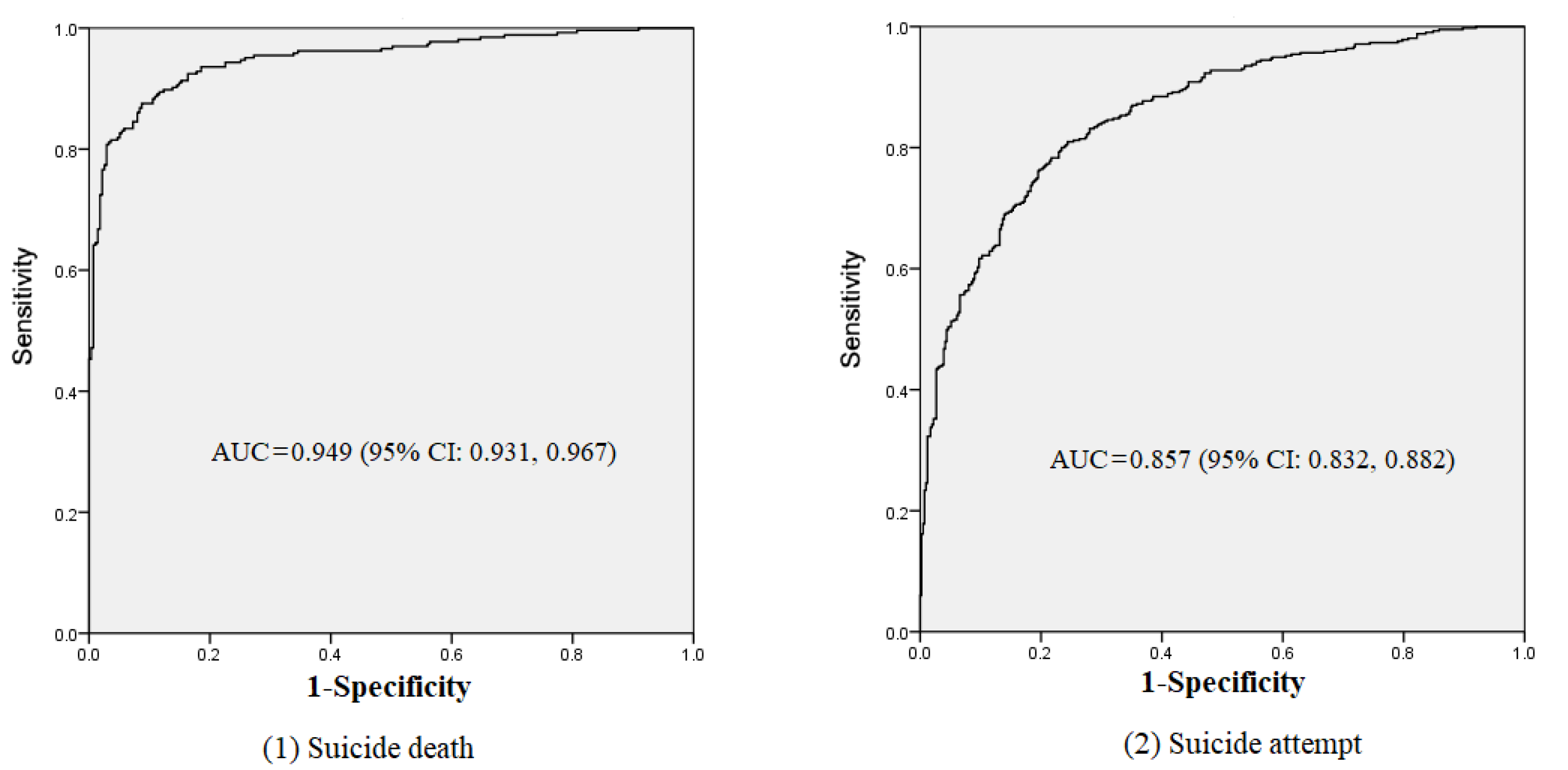
3.4. Performance of the Assessment Model
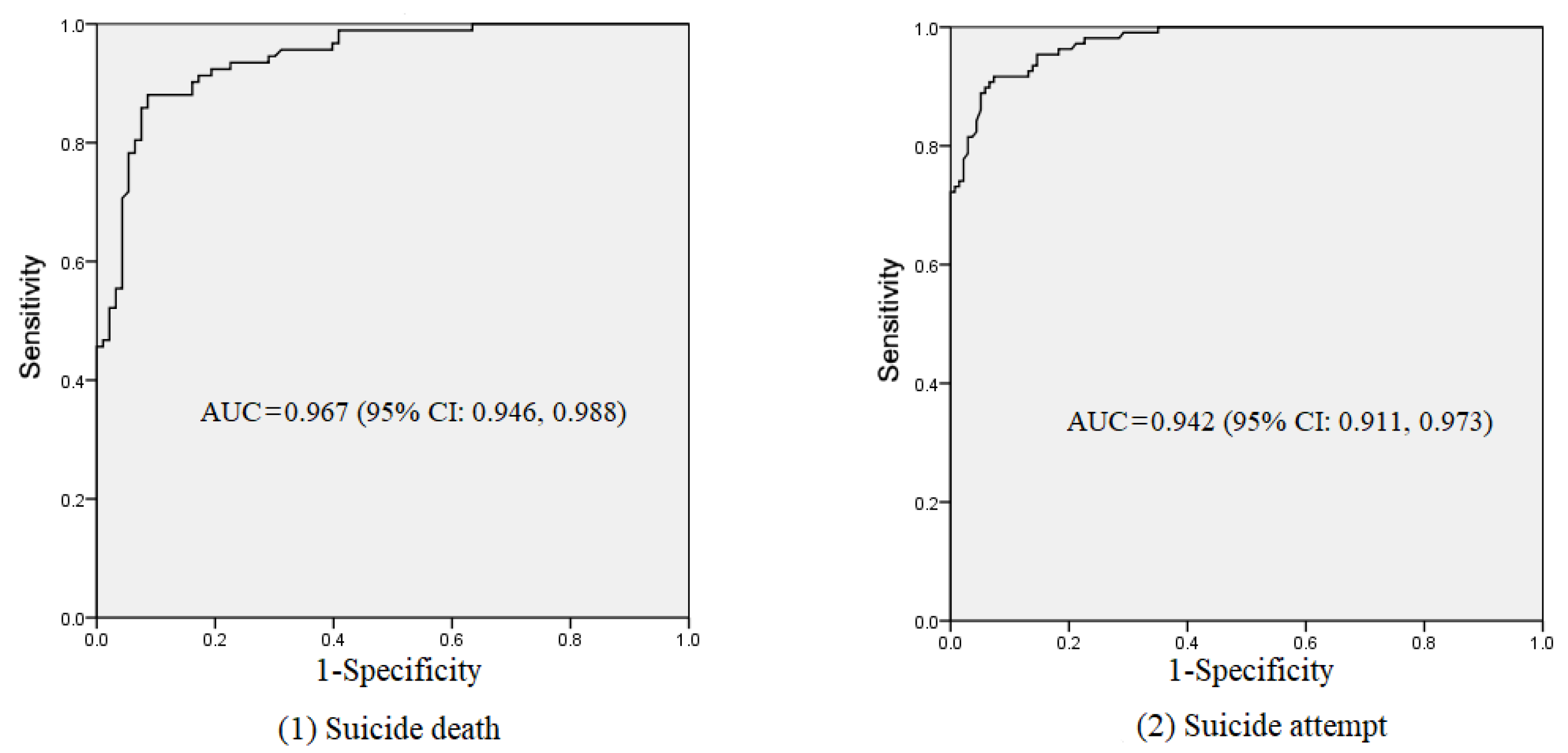
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Suicide worldwide in 2019: Global Health Estimates. Available online: https://www.who.int/publications/i/item/9789240026643 (accessed on 16 June 2021).
- Maris, R.W.; Berman, A.L.; Silverman, M.M. Comprehensive Textbook of Suicidology; The Guilford Press: New York, NY, USA, 2000. [Google Scholar]
- Phillips, M.R.; Li, X.; Zhang, Y. Suicide rates in China, 1995–99. Lancet 2002, 359, 835–840. [Google Scholar] [CrossRef]
- Zhang, J.; Sun, L.; Liu, Y.; Zhang, J. The Change in Suicide Rates between 2002 and 2011 in China. Suicide Life-Threat. Behav. 2014, 44, 560–568. [Google Scholar] [CrossRef]
- Preventing Suicide: A Global Imperative. Available online: https://www.who.int/publications/i/item/9789241564779 (accessed on 17 August 2014).
- Sun, J.; Guo, X.; Zhang, J.; Jia, C.; Xu, A. Suicide rates in Shandong, China, 1991–2010: Rapid decrease in rural rates and steady increase in male–female ratio. J. Affect. Disord. 2013, 146, 361–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claassen, C.A.; Harvilchuck-Laurenson, J.D.; Fawcett, J. Prognostic Models to Detect and Monitor the Near-Term Risk of Suicide: State of the science. Am. J. Prev. Med. 2014, 47, S181–S185. [Google Scholar] [CrossRef] [PubMed]
- Beck, R.W.; Morris, J.B.; Beck, A.T. Cross-Validation of the Suicidal Intent Scale. Psychol. Rep. 1974, 34, 445–446. [Google Scholar] [CrossRef]
- Beck, A.T. Beck Scale for Suicide Ideation; Psychological Corporation: San Antonio, TX, USA, 1991. [Google Scholar]
- Harriss, L.; Hawton, K.; Zahl, D. Value of measuring suicidal intent in the assessment of people attending hospital following self-poisoning or self-injury. Br. J. Psychiatry 2005, 186, 60–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stefansson, J.; Nordström, P.; Jokinen, J. Suicide Intent Scale in the prediction of suicide. J. Affect. Disord. 2012, 136, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Clopton, J.R.; Jones, W.C. Use of the MMPI in the prediction of suicide. J. Clin. Psychol. 1975, 31, 52–54. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.T. Manual for the Beck Hopelessness Scale; Psychological Corporation: San Antonio, TX, USA, 1993. [Google Scholar]
- Carroll, B.J. The Dexamethasone Suppression Test for Melancholia. Br. J. Psychiatry 1982, 140, 292–304. [Google Scholar] [CrossRef] [PubMed]
- López-Ibor, J.J.J.; Saiz-Ruiz, J.; Cobos, J.P.D.L. Biological Correlations of Suicide and Aggressivity in Major Depressions (with Melancholia): 5-Hydroxyindoleacetic Acid and Cortisol in Cerebral Spinal Fluid, Dexamethasone Suppression Test and Therapeutic Response to 5-Hydroxytryptophan. Neuropsychobiology 1985, 14, 67–74. [Google Scholar] [CrossRef]
- Ryan, C.J.; Large, M.M.; Callaghan, S. Suicide risk assessment: Where are we now? The Medical Journal of Australia 2013, 199, 534. [Google Scholar] [CrossRef] [PubMed]
- mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings (Version 2.0). Available online: https://www.who.int/publications/i/item/9789241549790 (accessed on 24 June 2019).
- Posner, K.; Oquendo, M.A.; Gould, M.; Stanley, B.; Davies, M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): Classification of Suicidal Events in the FDA’s Pediatric Suicidal Risk Analysis of Antidepressants. Am. J. Psychiatry 2007, 164, 1035–1043. [Google Scholar] [CrossRef] [PubMed]
- Patterson, W.M.; Dohn, H.H.; Bird, J.; Patterson, G.A. Evaluation of suicidal patients: The SAD PERSONS scale. J. Psychosom. Res. 1983, 24, 343–349. [Google Scholar] [CrossRef]
- Conrad, A.K.; Jacoby, A.M.; Jobes, D.A.; Lineberry, T.W.; Shea, C.E.; Ewing, T.D.A.; Schmid, P.J.; Ellenbecker, S.M.; Lee, J.L.; Fritsche, K.; et al. A Psychometric Investigation of the Suicide Status Form II with a Psychiatric Inpatient Sample. Suicide Life-Threat. Behav. 2009, 39, 307–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimeff, L.A.; Jobes, D.A.; Chalker, S.A.; Piehl, B.M.; Duvivier, L.L.; Lok, B.C.; Zalake, M.; Chung, J.; Koerner, K. A novel engagement of suicidality in the emergency department: Virtual Collaborative Assessment and Management of Suicidality. Gen. Hosp. Psychiatry 2020, 63, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Lu, Q.; Chen, X.; Liu, F. Retranslation and test of the reliability and validity for suicide risk assessment Scale. Chin. J. Pract. Nurs. 2018, 34, 1841–1845. [Google Scholar]
- Wang, Z.; Bian, Q.; He, J.; Shu, J.; Kong, Y.; Yang, L.; Zhou, J.; Chen, S. Reliability and validity analysis of the Columbia Suicide Screening Questionnaire in middle school students. Chin. J. Behav. Med. Brain Sci. 2019, 28, 1037–1042. [Google Scholar]
- Tan, R.; Deying, H.; Liu, Y.; Ke, X.; Wang, Y.; Zhou, Y.; Teng, F. Development of an indicator system for evaluating mental health in inpatients. Chin. J. Nurs. 2018, 53, 1096–1099. [Google Scholar]
- Yang, X.; Tong, H. Suicidal Risk Assessment and Related Social-psychological Factors in College Students. Chin. J. Clin. Psychol. 2010, 18, 695–698. [Google Scholar]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.; Greenhill, L.; Shen, S.; et al. The Columbia–Suicide Severity Rating Scale: Initial Validity and Internal Consistency Findings from Three Multisite Studies with Adolescents and Adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jobes, D.A.; Kahn-Greene, E.; Greene, J.A.; Goeke-Morey, M. Clinical Improvements of Suicidal Outpatients: Examining Suicide Status Form Responses as Predictors and Moderators. Arch. Suicide Res. 2009, 13, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Jobes, D.A. The Collaborative Assessment and Management of Suicidality (CAMS): An Evolving Evidence-Based Clinical Approach to Suicidal Risk. Suicide Life-Threat. Behav. 2012, 42, 640–653. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Xie, B.; Bian, Q.; Wan, L. Reliability and validity of the Columbia Suicide Screen for suicide risk assessment in senior middle school students. Chin. J. Psychiatry 2015, 48, 104–108. [Google Scholar] [CrossRef]
- Zhao, F. Comprehensive evaluation of agricultural development scale among the provinces and cities in China. China Secur. Futures 2011, 7, 160. [Google Scholar]
- Fang, L.; Zhang, J. Validity of Proxy Data Obtained by Different Psychological Autopsy Information Reconstruction Techniques. J. Int. Med. Res. 2010, 38, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wieczorek, W.; Conwell, Y.; Tu, X.-M.; Wu, B.Y.-W.; Xiao, S.; Jia, C. Characteristics of young rural Chinese suicides: A psychological autopsy study. Psychol. Med. 2009, 40, 581–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Li, Z.-Y.; Xiao, S.-Y.; Zhou, L.; Jia, C.-X.; Pan, G.-W. Mental disorder and suicide among youths in rural China: A case control study based on consecutive samples from Hunan, Liaoning and Shandong provinces. Chin. J. Epidemiol. 2012, 33, 588–592. [Google Scholar]
- Sun, L.; Zhang, J. Gender differences among medically serious suicide attempters aged 15–54 years in rural China. Psychiatry Res. 2017, 252, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lin, L. The Moderating Effects of Impulsivity on Chinese Rural Young Suicide. J. Clin. Psychol. 2013, 70, 579–588. [Google Scholar] [CrossRef]
- Zhang, J.; Xu, H. The Effects of Religion, Superstition, and Perceived Gender Inequality on the Degree of Suicide Intent: A Study of Serious Attempters in China. Omega J. Death Dying 2007, 55, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Lorant, V.; Kunst, A.E.; Huisman, M.; Costa, G.; Mackenbach, J. Socio-economic inequalities in suicide: A European comparative study. Br. J. Psychiatry 2005, 187, 49–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, C.-X.; Zhang, J. Characteristics of Young Suicides by Violent Methods in Rural China. J. Forensic Sci. 2011, 56, 674–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paykel, E.S.; Prusoff, B.A.; Uhlenhuth, E.H. Scaling of Life Events. Arch. Gen. Psychiatry 1971, 25, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ma, Z. Patterns of life events preceding the suicide in rural young Chinese: A case control study. J. Affect. Disord. 2012, 140, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Kong, Y.Y.; Zhang, J.; Jia, S.H.; Zhou, L. Reliability and Validity of the Beck Hopelessness Scale for Adolescents. Chin. Ment. Health J. 2007, 21, 686–689. [Google Scholar]
- Koenig, H.G.; Westlund, R.E.; George, L.K.; Hughes, D.C.; Blazer, D.G.; Hybels, C. Abbreviating the Duke Social Support Index for Use in Chronically Ill Elderly Individuals. J. Psychosom. Res. 1993, 34, 61–69. [Google Scholar] [CrossRef]
- Jia, C.; Zhang, J. Psychometric characteristics of the Duke Social Support Index in a young rural Chinese population. Death Stud. 2012, 36, 858–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickman, S.J. Functional and dysfunctional impulsivity: Personality and cognitive correlates. J. Pers. Soc. Psychol. 1990, 58, 95–102. [Google Scholar] [CrossRef]
- Gao, Q.; Zhang, J.; Jia, C. Psychometric properties of the Dickman Impulsivity Instrument in suicide victims and living controls of rural China. J. Affect. Disord. 2011, 132, 368–374. [Google Scholar] [CrossRef] [Green Version]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P); New York State Psychiatric Institute: New York, NY, USA, 2002. [Google Scholar]
- Sun, L.; Zhang, J. Characteristics of Chinese rural young suicides: Who did not have a strong intent to die. Compr. Psychiatry 2014, 57, 73–78. [Google Scholar] [CrossRef] [Green Version]
- Sun, L.; Zhang, J. Coping Skill as a Moderator Between Negative Life Events and Suicide Among Young People in Rural China. J. Clin. Psychol. 2014, 71, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Conwell, Y.; Zhou, L.; Jiang, C. Culture, risk factors and suicide in rural China: A psychological autopsy case control study. Acta Psychiatr. Scand. 2004, 110, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, N.; Tu, X.-M.; Xiao, S.; Jia, C. Risk factors for rural young suicide in China: A case–control study. J. Affect. Disord. 2011, 129, 244–251. [Google Scholar] [CrossRef] [Green Version]
- Lyu, J.; Wang, Y.; Shi, H.; Zhang, J. Early warnings for suicide attempt among Chinese rural population. J. Affect. Disord. 2018, 238, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Kovacs, M.; Garrison, B. Hopelessness and eventual suicide: A 10-year prospective study of pa-tients hospitalized with suicidal ideation. Am. J. Psychiatry 1985, 142, 559–563. [Google Scholar]
- Bolton, J.M.; Robinson, J. Population-Attributable Fractions of Axis I and Axis II Mental Disorders for Suicide Attempts: Findings from a Representative Sample of the Adult, Noninstitutionalized US Population. Am. J. Public Health 2010, 100, 2473–2480. [Google Scholar] [CrossRef]
- Bagge, C.L.; Glenn, C.R.; Lee, H.-J. Quantifying the impact of recent negative life events on suicide attempts. J. Abnorm. Psychol. 2013, 122, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Assink, M.; Van Der Put, C.E.; Stams, G.J.J.M. The Development and Validation of an Actuarial Risk Assessment Tool for the Prediction of First-Time Offending. Int. J. Offender Ther. Comp. Criminol. 2014, 60, 847–864. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.E.; Johnson, E.; Lawrence, J.M.; Rossom, R.C.; Ahmedani, B.; Lynch, F.L.; Beck, A.; Waitzfelder, B.; Ziebell, R.; Penfold, R.B.; et al. Predicting Suicide Attempts and Suicide Deaths Following Outpatient Visits Using Electronic Health Records. Am. J. Psychiatry 2018, 175, 951–960. [Google Scholar] [CrossRef]
- Hawes, M.; Yaseen, Z.; Briggs, J.; Galynker, I. The Modular Assessment of Risk for Imminent Suicide (MARIS): A proof of concept for a multi-informant tool for evaluation of short-term suicide risk. Compr. Psychiatry 2016, 72, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.; Mortensen, P.B. Specific characteristics of suicide in China. Acta Psychiatr. Scand. 2001, 103, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Eskin, M. The effects of religious versus secular education on suicide ideation and suicidal attitudes in adolescents in Turkey. Soc. Psychiatry Psychiatr. Epidemiology 2004, 39, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Thomas, D.L. Familial and Religious Influences on Suicidal Ideation. In Religion, Mental Health and the Latter-Day Saints; Judd, D.K., Ed.; Religious Studies Center at Brigham Young University: Provo, UT, USA, 1999; pp. 215–235. [Google Scholar]
- Wortzel, H.S.; Nazem, S.; Bahraini, N.H.; Matarazzo, B.B. Why Suicide Risk Assessment Still Matters. J. Psychiatr. Pract. 2017, 23, 436–440. [Google Scholar] [CrossRef]
| Suicide Death (n = 540) | Suicide Attempt (n = 825) | |||||
|---|---|---|---|---|---|---|
| Case | Control | Case | Control | |||
| n | 265 (49.1) | 275 (50.9) | 415 (50.3) | 410 (49.7) | ||
| Gender | 0.93 | 0.01 | ||||
| Male | 143 (54.0) | 137 (49.8) | 170 (41.0) | 169 (41.2) | ||
| Female | 122 (46.0) | 138 (50.2) | 245 (59.0) | 241 (58.8) | ||
| Age | 26.18 ± 6.17 | 25.09 ± 6.23 | 2.04 * | 26.48 ± 5.28 | 26.56 ± 5.28 | −0.24 |
| Education years | 7.16 ± 2.64 | 8.67 ± 2.11 | −7.38 *** | 7.47 ± 2.86 | 9.18 ± 2.93 | −8.49 *** |
| Marital status | 1.72 | 2.29 | ||||
| Never married | 89 (33.6) | 78 (28.4) | 59 (14.2) | 44 (10.7) | ||
| Ever married | 176 (66.4) | 197 (71.6) | 356 (85.8) | 366 (89.3) | ||
| Economic status | 72.33 *** | 36.43 *** | ||||
| Very poor | 131 (49.4) | 42 (15.3) | 113 (27.2) | 44 (10.7) | ||
| Others | 134 (50.6) | 233 (84.7) | 302 (72.8) | 366 (89.3) | ||
| Living alone | 2.98 | 0.70 | ||||
| Yes | 21 (7.9) | 12 (4.4) | 13 (3.1) | 9 (2.2) | ||
| No | 244 (92.1) | 263 (95.6) | 402 (96.9) | 401 (97.8) | ||
| Occupation | 0.64 | 0.30 | ||||
| Agricultural worker | 121 (45.7) | 135 (49.1) | 227 (54.7) | 232 (56.6) | ||
| Others | 144 (54.3) | 140 (50.9) | 188 (45.3) | 178 (43.4) | ||
| Religious belief | 13.50 *** | 4.25 * | ||||
| Yes | 75 (28.3) | 42 (15.3) | 81 (19.5) | 58 (14.1) | ||
| No | 190 (71.7) | 233 (84.7) | 334 (80.5) | 352 (85.9) | ||
| Pesticide at home | 8.25 ** | 0.85 | ||||
| Yes | 198 (74.7) | 174 (63.3) | 257 (61.9) | 241 (58.8) | ||
| No | 67 (25.3) | 101 (36.7) | 158 (38.1) | 169 (41.2) | ||
| Family suicide history | 45.43 *** | 19.31 *** | ||||
| Yes | 60 (22.6) | 9 (3.3) | 35 (8.4) | 7 (1.7) | ||
| No | 205 (77.4) | 266 (96.7) | 380 (91.6) | 403 (98.3) | ||
| Negative life events | 3.48 ± 2.33 | 1.44 ± 1.57 | 11.97 *** | 1.84 ± 0.66 | 0.66 ± 1.10 | 11.15 *** |
| Hopelessness | 69.77 ± 13.79 | 47.85 ± 7.93 | 22.73 *** | 51.04 ± 15.73 | 36.94 ± 10.79 | 15.00 *** |
| Social interaction | 6.14 ± 1.73 | 7.40 ± 1.69 | −8.56 *** | 7.75 ± 2.25 | 9.08 ± 1.85 | −9.20 *** |
| Subjected support | 14.48 ± 3.40 | 18.43 ± 2.40 | −15.65 *** | 19.33 ± 33.33 | 20.10 ± 1.51 | −0.47 * |
| Instrumental support | 9.11±2.86 | 10.64±1.86 | −7.37 *** | 10.87±2.13 | 11.46±1.34 | −4.81 *** |
| Impulsivity | 14.53±5.24 | 12.21±3.76 | 5.91 *** | 10.30±4.14 | 9.12±3.01 | 4.70 *** |
| Mental disorder | 122.35 *** | 56.81 *** | ||||
| Yes | 120 (45.3) | 12 (4.4) | 83 (20.0) | 13 (3.2) | ||
| No | 145 (54.7) | 263 (95.6) | 332 (80.0) | 397 (96.8) | ||
| Suicide Death (n = 540) | Suicide Attempt (n = 825) | ||||||
|---|---|---|---|---|---|---|---|
| β | OR | 95% CI | β | OR | 95% CI | ||
| Education years | −0.243 | 0.784 *** | 0.685, 0.898 | −0.209 | 0.811 *** | 0.757, 0.869 | |
| Very poor | - | - | - | 0.663 | 1.941 ** | 1.198, 3.144 | |
| Agricultural worker | 0.772 | 2.163 * | 1.175, 3.984 | 0.614 | 1.847 *** | 1.271, 2.685 | |
| Family suicide history | 1.919 | 6.817 *** | 2.338, 19.875 | 1.431 | 4.182 ** | 1.463, 11.951 | |
| Negative life events | 0.258 | 1.294 ** | 1.097, 1.525 | 0.484 | 1.622 *** | 1.393, 1.888 | |
| Hopelessness | 0.152 | 1.164 *** | 1.127, 1.201 | 0.061 | 1.063 *** | 1.046, 1.080 | |
| Social interaction | - | - | - | −0.157 | 0.855 *** | 0.782, 0.934 | |
| Impulsivity | 0.140 | 1.151 *** | 1.078, 1.228 | 0.065 | 1.067 ** | 1.016, 1.121 | |
| Mental disorder | 2.042 | 7.705 *** | 3.081, 19.266 | 0.844 | 2.325 * | 1.089, 4.963 | |
| Constant | −10.062 | 0.000 *** | - | −1.283 | 0.277 | 0.757, 0.869 | |
| R2 | 0.751 | 0.481 | |||||
| Suicide Death (n = 245) | Suicide Attempt (n = 185) | |||||
|---|---|---|---|---|---|---|
| Case | Control | Case | Control | |||
| n | 108 (44.1) | 137 (55.9) | 92 (49.7) | 93 (50.3) | ||
| Gender | 1.16 | 0.01 | ||||
| Male | 57 (52.8) | 63 (46.0) | 35 (38.0) | 36 (38.7) | ||
| Female | 51 (47.2) | 74 (54.0) | 57 (62.0) | 57 (61.3) | ||
| Age | 26.91 ± 5.96 | 26.60 ± 5.67 | 0.41 | 27.84 ± 5.33 | 27.72 ± 5.10 | 0.15 |
| Education years | 8.09 ± 3.05 | 10.12 ± 2.64 | −5.56 *** | 9.35 ± 2.58 | 12.40 ± 3.71 | −6.49 *** |
| Marital status | 1.00 | 2.42 | ||||
| Never married | 33 (30.6) | 34 (24.8) | 16 (17.4) | 25 (26.9) | ||
| Ever married | 75 (69.4) | 103 (75.2) | 76 (82.6) | 68 (73.1) | ||
| Economic status | 48.08 *** | 6.64 ** | ||||
| Very poor | 53 (49.1) | 13 (9.5) | 16 (17.4) | 5 (5.4) | ||
| Others | 55 (50.9) | 124 (90.5) | 76 (82.6) | 88 (94.6) | ||
| Living alone | 6.24 * | 2.55 | ||||
| Yes | 13 (12.0) | 5 (3.6) | 7 (7.6) | 14 (15.1) | ||
| No | 95 (88.0) | 132 (96.4) | 85 (92.4) | 79 (84.9) | ||
| Occupation | 6.91 ** | 13.66 *** | ||||
| Agricultural worker | 66 (61.1) | 105 (76.6) | 60 (65.2) | 82 (88.2) | ||
| Others | 42 (38.9) | 32 (23.4) | 32 (34.8) | 11 (11.8) | ||
| Religious belief | 2.82 | 0.05 | ||||
| Yes | 33 (30.6) | 29 (21.2) | 22 (23.9) | 21 (22.6) | ||
| No | 75 (69.4) | 108 (78.8) | 70 (76.1) | 72 (77.4) | ||
| Pesticide at home | 8.20 ** | 8.75 ** | ||||
| Yes | 86 (79.6) | 86 (62.8) | 36 (39.1) | 18 (19.4) | ||
| No | 22 (20.4) | 51 (37.2) | 56 (60.9) | 75 (80.6) | ||
| Family Suicide history | 16.56 *** | 4.77 * | ||||
| Yes | 23 (21.3) | 6 (4.4) | 7 (7.6) | 1 (1.1) | ||
| No | 85 (78.7) | 131 (95.6) | 85 (92.4) | 92 (98.9) | ||
| Negative life events | 2.99 ± 2.31 | 0.45 ± 0.95 | 11.65 *** | 2.07 ± 2.18 | 0.24 ± 0.48 | 7.91 *** |
| Hopelessness | 67.62 ± 12.49 | 44.97 ± 7.91 | 17.29 *** | 60.39 ± 8.81 | 44.29 ± 7.17 | 13.64 *** |
| Social interaction | 6.63 ± 2.19 | 8.09 ± 2.09 | −5.31 *** | 7.57 ± 1.80 | 9.34 ± 1.60 | −7.10 *** |
| Subjected support | 18.85 ± 2.54 | 33.02 ± 112.12 | −1.48 | 25.52 ± 70.02 | 36.53 ± 121.22 | −0.76 |
| Instrumental support | 9.85 ± 3.23 | 11.47 ± 1.78 | −4.97 *** | 9.07 ± 3.81 | 11.45 ± 1.22 | −5.74 *** |
| Impulsivity | 12.62 ± 6.38 | 9.69 ± 4.07 | 4.37 *** | 11.16 ± 4.87 | 9.70 ± 4.65 | 2.09 * |
| Mental disorder | 80.29 *** | 10.686 *** | ||||
| Yes | 57 (52.8) | 4 (2.9) | 10 (10.9) | 0 (0.0) | ||
| No | 51 (47.2) | 133 (97.1) | 82 (89.1) | 93 (100.0) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, L.; Zhang, J.; Lamis, D.A.; Wang, Y. Risk Assessment on Suicide Death and Attempt among Chinese Rural Youths Aged 15–34 Years. Int. J. Environ. Res. Public Health 2021, 18, 13362. https://doi.org/10.3390/ijerph182413362
Sun L, Zhang J, Lamis DA, Wang Y. Risk Assessment on Suicide Death and Attempt among Chinese Rural Youths Aged 15–34 Years. International Journal of Environmental Research and Public Health. 2021; 18(24):13362. https://doi.org/10.3390/ijerph182413362
Chicago/Turabian StyleSun, Long, Jie Zhang, Dorian A. Lamis, and Yifan Wang. 2021. "Risk Assessment on Suicide Death and Attempt among Chinese Rural Youths Aged 15–34 Years" International Journal of Environmental Research and Public Health 18, no. 24: 13362. https://doi.org/10.3390/ijerph182413362
APA StyleSun, L., Zhang, J., Lamis, D. A., & Wang, Y. (2021). Risk Assessment on Suicide Death and Attempt among Chinese Rural Youths Aged 15–34 Years. International Journal of Environmental Research and Public Health, 18(24), 13362. https://doi.org/10.3390/ijerph182413362







