Mental Health Symptoms Associated with Sexualized Drug Use (Chemsex) among Men Who Have Sex with Men: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Research Question
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Coding of Studies
3. Results
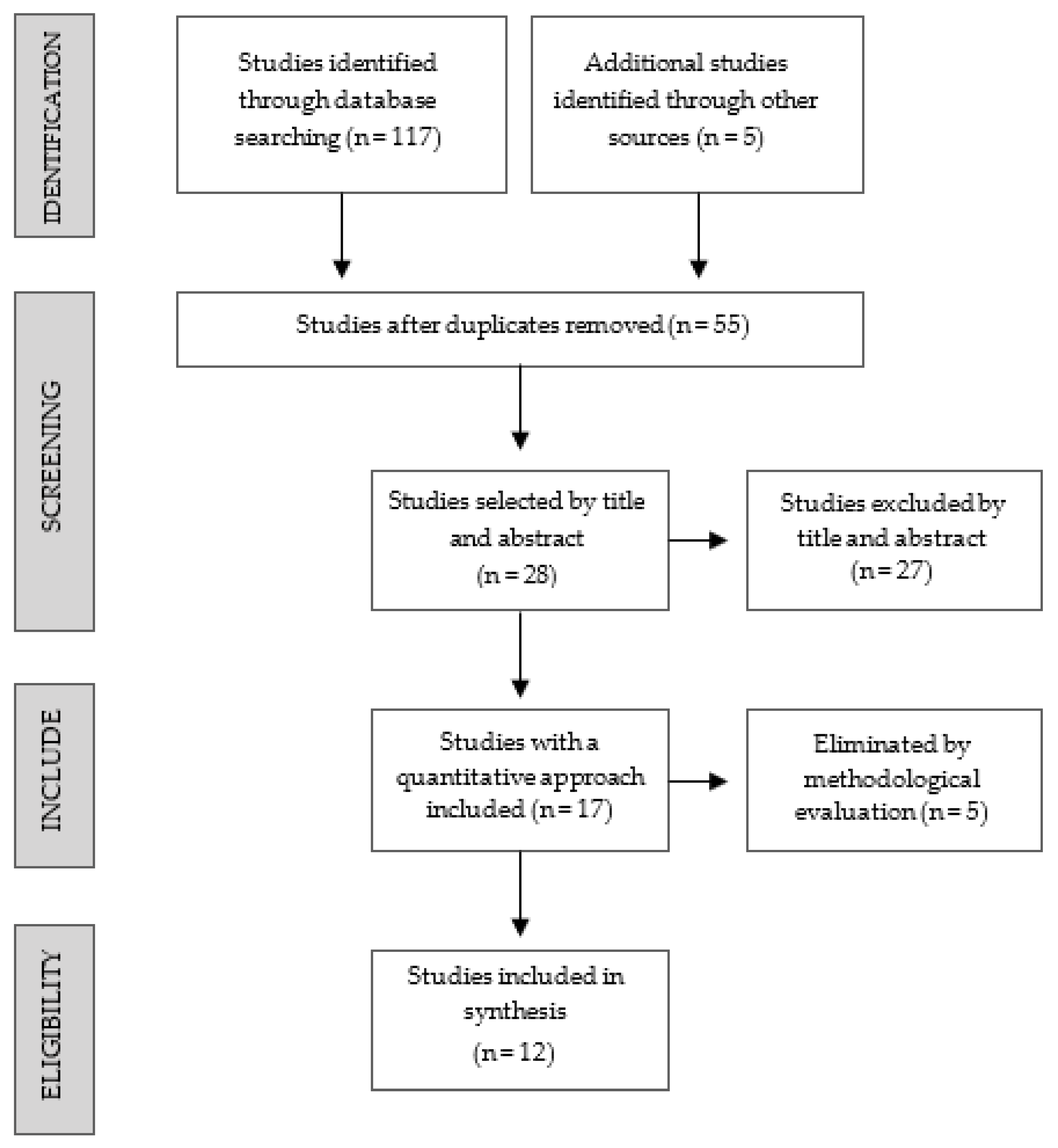
3.1. Study Selection
3.2. Prevalence and Type of Drug Use in Chemsex
3.3. Assessment Techniques
3.4. Mental Health
3.5. Relationship between Non-Intravenous Drug Use and Mental Health
3.6. Relationship between Intravenous Drug Use and Mental Health
3.7. Absence of Relationship between Drugs and Mental Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maxwell, S.; Shahmanesh, M.; Gafos, M. Chemsex behaviours among men who have sex with men: A systematic review of the literature. Int. J. Drug Policy 2019, 63, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Tomkins, A.; George, R.; Kliner, M. Sexualised drug taking among men who have sex with men: A systematic review. Perspect. Public Health 2019, 139, 23–33. [Google Scholar] [CrossRef]
- Lafortune, D.; Blais, M.; Miller, G.; Dion, L.; Lalonde, F.; Dargis, L. Psychological and Interpersonal Factors Associated with Sexualized Drug Use Among Men Who Have Sex with Men: A Mixed-Methods Systematic Review. Arch. Sex. Behav. 2021, 50, 427–460. [Google Scholar] [CrossRef]
- Bourne, A.; Reid, D.; Hickson, F.; Torres Rueda, S.; Weatherburn, P. The Chemsex Study: Drug Use in Sexual Settings among Gay and Bisexual Men in Lambeth, Southwark and Lewisham; Sigma Research, London School of Hygiene & Tropical Medicine: London, UK, 2014; Available online: https://researchonline.lshtm.ac.uk/id/eprint/2197245/ (accessed on 3 August 2021).
- Glynn, R.W.; Byrne, N.; O’Dea, S.; Shanley, A.; Codd, M.; Keenan, E.; Ward, M.; Igoe, D.; Clarke, S. Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin, Ireland. Int. J. Drug Policy 2018, 52, 9–15. [Google Scholar] [CrossRef]
- Hegazi, A.; Lee, M.J.; Whittaker, W.; Green, S.; Simms, R.; Cutts, R.; Nagington, M.; Nathan, B.; Pakianathan, M.R. Chemsex and the city: Sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. Int. J. STD AIDS 2017, 28, 362–366. [Google Scholar] [CrossRef]
- Macfarlane, A. Sex, drugs and self-control: Why chemsex is fast becoming a public health concern. J. Fam. Plann. Reprod. Health Care 2016, 42, 291–294. [Google Scholar] [CrossRef] [Green Version]
- Power, J.; Mikołajczak, G.; Bourne, A.; Brown, G.; Leonard, W.; Lyons, A.; Dowsett, G.W.; Lucke, J. Sex, drugs and social connectedness: Wellbeing among HIV-positive gay and bisexual men who use party-and-play drugs. Sex. Health 2018, 15, 135–143. [Google Scholar] [CrossRef]
- Hurley, M.; Prestage, G. Intensive sex partying amongst gay men in Sydney. Cult. Health Sex. 2009, 11, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Fernández Dávila, P. “Sesión de sexo, morbo y vicio”: Una aproximación holística para entender la aparición del fenómeno ChemSex entre hombres gais, bisexuales y otros hombres que tienen sexo con hombres en España. Rev. Multidiscip. Sida 2016, 4, 41–65. [Google Scholar]
- Hout, M.C.V.; Crowley, D.; O’Dea, S.; Clarke, S. Chasing the rainbow: Pleasure, sex-based sociality and consumerism in navigating and exiting the Irish Chemsex scene. Cult. Health Sex. 2019, 21, 1074–1086. [Google Scholar] [CrossRef]
- Ahmed, A.-K.; Weatherburn, P.; Reid, D.; Hickson, F.; Torres-Rueda, S.; Steinberg, P.; Bourne, A. Social norms related to combining drugs and sex (“chemsex”) among gay men in South London. Int. J. Drug Policy 2016, 38, 29–35. [Google Scholar] [CrossRef]
- Blomquist, P.B.; Mohammed, H.; Mikhail, A.; Weatherburn, P.; Reid, D.; Wayal, S.; Hughes, G.; Mercer, C.H. Characteristics and sexual health service use of MSM engaging in chemsex: Results from a large online survey in England. Sex. Transm. Infect. 2020, 96, 590–595. [Google Scholar] [CrossRef] [Green Version]
- Sewell, J.; Miltz, A.; Lampe, F.C.; Cambiano, V.; Speakman, A.; Phillips, A.N.; Stuart, D.; Gilson, R.; Asboe, D.; Nwokolo, N.; et al. Poly drug use, chemsex drug use, and associations with sexual risk behaviour in HIV-negative men who have sex with men attending sexual health clinics. Int. J. Drug Policy 2017, 43, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Guerras, J.-M.; Hoyos Miller, J.; Agustí, C.; Chanos, S.; Pichon, F.; Kuske, M.; Cigan, B.; Fuertes, R.; Stefanescu, R.; Ooms, L.; et al. Association of Sexualized Drug Use Patterns with HIV/STI Transmission Risk in an Internet Sample of Men Who Have Sex with Men from Seven European Countries. Arch. Sex. Behav. 2021, 50, 461–477. [Google Scholar] [CrossRef] [PubMed]
- Stuart, D. Chemsex: Origins of the word, a history of the phenomenon and a respect to the culture. Drugs Alcohol Today 2019, 19, 3–10. [Google Scholar] [CrossRef]
- Deimel, D.; Stoever, H.; Hoesselbarth, S.; Dichtl, A.; Graf, N.; Gebhardt, V. Drug use and health behaviour among German men who have sex with men: Results of a qualitative, multi-centre study. Harm. Reduct. J. 2016, 13, 36. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Tenga, T.; Lu, H.; Zhao, Y.; Liu, H.; Yin, L.; Sun, Z.; He, X.; Qian, H.-Z.; Ruan, Y.; et al. Poppers use and risky sexual behaviors among men who have sex with men in Beijing, China. Drug Alcohol Depend. 2016, 160, 42–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bourne, A.; Reid, D.; Hickson, F.; Torres-Rueda, S.; Weatherburn, P. Illicit drug use in sexual settings (‘chemsex’) and HIV/STI transmission risk behaviour among gay men in South London: Findings from a qualitative study. Sex. Transm. Infect. 2015, 91, 564–568. [Google Scholar] [CrossRef]
- Rana, S.; Macdonald, N.; French, P.; Jarman, J.; Patel, S.; Portman, M.; Suchak, T.; Sullivan, A.; White, J.; Crook, P. Enhanced surveillance of syphilis cases among men who have sex with men in London, October 2016–January 2017. Int. J. STD AIDS 2019, 30, 422–429. [Google Scholar] [CrossRef]
- Santoro, P.; Rodríguez, R.; Morales, P.; Morano, A.; Morán, M. One “chemsex” or many? Types of chemsex sessions among gay and other men who have sex with men in Madrid, Spain: Findings from a qualitative study. Int. J. Drug Policy 2020, 82, 102790. [Google Scholar] [CrossRef]
- Brogan, N.; Paquette, D.M.; Lachowsky, N.J.; Blais, M.; Brennan, D.J.; Hart, T.A.; Adam, B. Canadian results from the European Men-who-have-sex-with-men Internet survey (EMIS-2017). Can. Commun. Dis. Rep. Releve Mal. Transm. Au Can. 2019, 45, 271–282. [Google Scholar] [CrossRef]
- Moyle, L.; Dymock, A.; Aldridge, A.; Mechen, B. Pharmacosex: Reimagining sex, drugs and enhancement. Int. J. Drug Policy 2020, 86, 102943. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7773803/ (accessed on 25 May 2021). [CrossRef]
- Schmidt, A.J.; Bourne, A.; Weatherburn, P.; Reid, D.; Marcus, U.; Hickson, F. Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). Int. J. Drug Policy 2016, 38, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Edmundson, C.; Heinsbroek, E.; Glass, R.; Hope, V.; Mohammed, H.; White, M.; Desai, M. Sexualised drug use in the United Kingdom (UK): A review of the literature. Int. J. Drug Policy 2018, 55, 131–148. [Google Scholar] [CrossRef]
- Evers, Y.J.; Geraets, J.J.H.; Van Liere, G.A.F.S.; Hoebe, C.J.P.A.; Dukers-Muijrers, N.H.T.M. Attitude and beliefs about the social environment associated with chemsex among MSM visiting STI clinics in the Netherlands: An observational study. PLoS ONE 2020, 15, e0235467. [Google Scholar] [CrossRef]
- Pufall, E.L.; Kall, M.; Shahmanesh, M.; Nardone, A.; Gilson, R.; Delpech, V.; Ward, H. Positive Voices study group Sexualized drug use (‘chemsex’) and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Med. 2018, 19, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.; Gafos, M.; Moncrieff, M.; Shahmanesh, M.; Stirrup, O. Pre-exposure prophylaxis use among men who have sex with men who have experienced problematic chemsex. Int. J. STD AIDS 2020, 31, 474–480. [Google Scholar] [CrossRef]
- Evers, Y.J.; Van Liere, G.A.F.S.; Hoebe, C.J.P.A.; Dukers-Muijrers, N.H.T.M. Chemsex among men who have sex with men living outside major cities and associations with sexually transmitted infections: A cross-sectional study in the Netherlands. PLoS ONE 2019, 14, e0216732. [Google Scholar] [CrossRef]
- Torres, T.S.; Bastos, L.S.; Kamel, L.; Bezerra, D.R.B.; Fernandes, N.M.; Moreira, R.I.; Garner, A.; Veloso, V.G.; Grinsztejn, B.; De Boni, R.B. Do men who have sex with men who report alcohol and illicit drug use before/during sex (chemsex) present moderate/high risk for substance use disorders? Drug Alcohol Depend. 2020, 209, 107908. [Google Scholar] [CrossRef] [PubMed]
- Stevens, O.; Moncrieff, M.; Gafos, M. Chemsex-related drug use and its association with health outcomes in men who have sex with men: A cross-sectional analysis of Antidote clinic service data. Sex. Transm. Infect. 2020, 96, 124–130. [Google Scholar] [CrossRef]
- Chen, G.-L.; Lin, S.-Y.; Lo, H.-Y.; Wu, H.-C.; Lin, Y.-M.; Chen, T.-C.; Chu, S.-Y.S.; Lee, W.-C.; Chen, Y.-H.; Lu, P.-L. Clinical impact of recreational drug use among people living with HIV in southern Taiwan. J. Microbiol. Immunol. Infect. 2021, 54, 952–962. [Google Scholar] [CrossRef]
- Achterbergh, R.C.A.; Drückler, S.; van Rooijen, M.S.; van Aar, F.; Slurink, I.a.L.; de Vries, H.J.C.; Boyd, A. Sex, drugs, and sexually transmitted infections: A latent class analysis among men who have sex with men in Amsterdam and surrounding urban regions, the Netherlands. Drug Alcohol Depend. 2020, 206, 107526. [Google Scholar] [CrossRef] [PubMed]
- González-Baeza, A.; Dolengevich-Segal, H.; Pérez-Valero, I.; Cabello, A.; Téllez, M.J.; Sanz, J.; Pérez-Latorre, L.; Bernardino, J.I.; Troya, J.; De La Fuente, S.; et al. Sexualized Drug Use (Chemsex) Is Associated with High-Risk Sexual Behaviors and Sexually Transmitted Infections in HIV-Positive Men Who Have Sex with Men: Data from the U-SEX GESIDA 9416 Study. AIDS Patient Care STDs 2018, 32, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Losilla Rodríguez, B.; López-Zúñiga, M.; Espadafor-López, B.; López-Ruz, M. Study of ChemSex in HIV positive and negative homosexual patients. Actual. Med. 2019, 104, 24–30. [Google Scholar] [CrossRef]
- Ottaway, Z.; Finnerty, F.; Buckingham, T.; Richardson, D. Increasing rates of reported chemsex/sexualised recreational drug use in men who have sex with men attending for postexposure prophylaxis for sexual exposure. Sex. Transm. Infect. 2017, 93, 31. [Google Scholar] [CrossRef]
- Howarth, A.; Apea, V.; Michie, S.; Morris, S.; Sachikonye, M.; Mercer, C.; Evans, A.; Delpech, V.; Sabin, C.; Burns, F. The association between use of chemsex drugs and HIV clinic attendance among gay and bisexual men living with HIV in London. HIV Med. 2021, 22, 641–649. [Google Scholar] [CrossRef]
- Arends, R.M.; van den Heuvel, T.J.; Foeken-Verwoert, E.G.J.; Grintjes, K.J.T.; Keizer, H.J.G.; Schene, A.H.; van der Ven, A.J.A.M.; Schellekens, A.F.A. Sex, Drugs, and Impulse Regulation: A Perspective on Reducing Transmission Risk Behavior and Improving Mental Health Among MSM Living With HIV. Front. Psychol. 2020, 11, 1005. [Google Scholar] [CrossRef]
- Bohn, A.; Sander, D.; Köhler, T.; Hees, N.; Oswald, F.; Scherbaum, N.; Deimel, D.; Schecke, H. Chemsex and Mental Health of Men Who Have Sex With Men in Germany. Front. Psychiatry 2020, 11, 1100. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7672155/ (accessed on 25 May 2021). [CrossRef]
- Fletcher, J.B.; Clark, K.A.; Reback, C.J. Depression and HIV transmission risk among methamphetamine-using men who have sex with men. Addict. Res. Theory 2021, 29, 263–270. [Google Scholar] [CrossRef]
- Tan, R.K.J.; O’Hara, C.A.; Koh, W.L.; Le, D.; Tan, A.; Tyler, A.; Tan, C.; Kwok, C.; Banerjee, S.; Wong, M.L. Social capital and chemsex initiation in young gay, bisexual, and other men who have sex with men: The pink carpet Y cohort study. Subst. Abuse Treat. Prev. Policy 2021, 16, 18. [Google Scholar] [CrossRef]
- Hylton, E.; Wirtz, A.L.; Zelaya, C.E.; Latkin, C.; Peryshkina, A.; Mogilnyi, V.; Dzhigun, P.; Kostetskaya, I.; Galai, N.; Beyrer, C. Sexual Identity, Stigma, and Depression: The Role of the “Anti-gay Propaganda Law” in Mental Health among Men Who Have Sex with Men in Moscow, Russia. J. Urban Health Bull. N. Y. Acad. Med. 2017, 94, 319–329. [Google Scholar] [CrossRef]
- Mays, V.M.; Cochran, S.D. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. Am. J. Public Health 2001, 91, 1869–1876. [Google Scholar] [CrossRef] [PubMed]
- Meyer, I.H. Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef]
- Teasdale, B.; Bradley-Engen, M. Adolescent Same-Sex Attraction and Mental Health: The Role of Stress and Support. J. Homosex. 2010, 57, 287–309. [Google Scholar] [CrossRef] [PubMed]
- Burton, C.M.; Marshal, M.P.; Chisolm, D.J.; Sucato, G.S.; Friedman, M.S. Sexual minority-related victimization as a mediator of mental health disparities in sexual minority youth: A longitudinal analysis. J. Youth Adolesc. 2013, 42, 394–402. [Google Scholar] [CrossRef] [Green Version]
- Poteat, V.P.; Mereish, E.H.; DiGiovanni, C.D.; Koenig, B.W. The effects of general and homophobic victimization on adolescents’ psychosocial and educational concerns: The importance of intersecting identities and parent support. J. Couns. Psychol. 2011, 58, 597–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, S.T.; Fish, J.N. Mental Health in Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth. Annu. Rev. Clin. Psychol. 2016, 12, 465–487. [Google Scholar] [CrossRef] [Green Version]
- Katz-Wise, S.L.; Hyde, J.S. Victimization experiences of lesbian, gay, and bisexual individuals: A meta-analysis. J. Sex Res. 2012, 49, 142–167. [Google Scholar] [CrossRef]
- McConnell, E.A.; Janulis, P.; Phillips, G.; Truong, R.; Birkett, M. Multiple Minority Stress and LGBT Community Resilience among Sexual Minority Men. Psychol. Sex. Orientat. Gend. Divers. 2018, 5, 1–12. [Google Scholar] [CrossRef]
- Sattler, F.A.; Wagner, U.; Christiansen, H. Effects of Minority Stress, Group-Level Coping, and Social Support on Mental Health of German Gay Men. PLoS ONE 2016, 11, e0150562. [Google Scholar] [CrossRef]
- Sun, S.; Pachankis, J.E.; Li, X.; Operario, D. Addressing Minority Stress and Mental Health among Men Who Have Sex with Men (MSM) in China. Curr. HIV/AIDS Rep. 2020, 17, 35–62. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Cooper, C.; Rogers, M.; Bethel, A.; Briscoe, S.; Lowe, J. A mapping review of the literature on UK-focused health and social care databases. Health Inf. Libr. J. 2015, 32, 5–22. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Tufanaru, C.; Aromataris, E. JBI’s systematic reviews: Data extraction and synthesis. Am. J. Nurs. 2014, 114, 49–54. [Google Scholar] [CrossRef]
- Nimbi, F.M.; Rosati, F.; Esposito, R.M.; Stuart, D.; Simonelli, C.; Tambelli, R. Chemsex in Italy: Experiences of Men Who Have Sex With Men Consuming Illicit Drugs to Enhance and Prolong Their Sexual Activity. J. Sex. Med. 2020, 17, 1875–1884. [Google Scholar] [CrossRef] [PubMed]
- Vaccher, S.J.; Hammoud, M.A.; Bourne, A.; Lea, T.; Haire, B.G.; Holt, M.; Saxton, P.; Mackie, B.; Badge, J.; Jin, F.; et al. Prevalence, frequency, and motivations for alkyl nitrite use among gay, bisexual and other men who have sex with men in Australia. Int. J. Drug Policy 2020, 76, 102659. [Google Scholar] [CrossRef] [PubMed]
- Batisse, A.; Peyrière, H.; Eiden, C.; Courné, M.-A.; Djezzar, S. Usage de psychostimulants dans un contexte sexuel: Analyse des cas rapportés au Réseau français des centres d’addictovigilance. Évaluation des risques liés à la pratique du SLAM. Therapies 2016, 71, 447–455. [Google Scholar] [CrossRef]
- Card, K.G.; Armstrong, H.L.; Wang, L.; Bacani, N.; Moore, D.M.; Roth, E.A.; Hogg, R.S.; Lachowsky, N.J. Escape expectancies and sexualized substance use among gay, bisexual, and other men who have sex with men. AIDS Care 2019, 1–9. [Google Scholar] [CrossRef]
- Demant, D.; Oviedo-Trespalacios, O. Harmless? A hierarchical analysis of poppers use correlates among young gay and bisexual men. Drug Alcohol Rev. 2019, 38, 465–472. [Google Scholar] [CrossRef]
- Dolengevich-Segal, H.; Gonzalez-Baeza, A.; Valencia, J.; Valencia-Ortega, E.; Cabello, A.; Tellez-Molina, M.J.; Perez-Elias, M.J.; Serrano, R.; Perez-Latorre, L.; Martin-Carbonero, L.; et al. Drug-related and psychopathological symptoms in HIV-positive men who have sex with men who inject drugs during sex (slamsex): Data from the U-SEX GESIDA 9416 Study. PLoS ONE 2019, 14, e0220272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hammoud, M.A.; Bourne, A.; Maher, L.; Jin, F.; Haire, B.; Lea, T.; Degenhardt, L.; Grierson, J.; Prestage, G. Intensive sex partying with gamma-hydroxybutyrate: Factors associated with using gamma-hydroxybutyrate for chemsex among Australian gay and bisexual men—Results from the Flux Study. Sex. Health 2017, 15, 123–134. [Google Scholar] [CrossRef]
- Hibbert, M.P.; Brett, C.E.; Porcellato, L.A.; Hope, V.D. Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex. Transm. Infect. 2019, 95, 342–350. [Google Scholar] [CrossRef]
- Nöstlinger, C.; Reyniers, T.; Smekens, T.; Apers, H.; Laga, M.; Wouters, K.; Vuylsteke, B. Drug use, depression and sexual risk behaviour: A syndemic among early pre-exposure prophylaxis (PrEP) adopters in Belgium? AIDS Care 2020, 32, 57–64. [Google Scholar] [CrossRef]
- Schecke, H.; Lea, T.; Bohn, A.; Köhler, T.; Sander, D.; Scherbaum, N.; Deimel, D. Crystal Methamphetamine Use in Sexual Settings Among German Men Who Have Sex With Men. Front. Psychiatry 2019, 10, 886. Available online: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00886/full (accessed on 28 May 2020). [CrossRef]
- Trouiller, P.; Velter, A.; Saboni, L.; Sommen, C.; Sauvage, C.; Vaux, S.; Barin, F.; Chevaliez, S.; Lot, F.; Jauffret-Roustide, M. Injecting drug use during sex (known as “slamming”) among men who have sex with men: Results from a time-location sampling survey conducted in five cities, France. Int. J. Drug Policy 2020, 79, 102703. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Pers. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Israel, T. Development and validation of a psychological sense of LGBT Community Scale. J. Community Psychol. 2012, 40, 573–587. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Williams, J.B.; Kroenke, K.; Linzer, M.; deGruy, F.V.; Hahn, S.R.; Brody, D.; Johnson, J.G. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994, 272, 1749–1756. [Google Scholar] [CrossRef]
- Levis, B.; Benedetti, A.; Thombs, B.D. DEPRESsion Screening Data (DEPRESSD) Collaboration Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, l1476. [Google Scholar] [CrossRef] [Green Version]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addict. Abingdon Engl. 1993, 88, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Berner, M.M.; Kriston, L.; Bentele, M.; Härter, M. The alcohol use disorders identification test for detecting at-risk drinking: A systematic review and meta-analysis. J. Stud. Alcohol Drugs 2007, 68, 461–473. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.; Shield, K.; Monteiro, M.; Rehm, J. Facilitating Screening and Brief Interventions in Primary Care: A Systematic Review and Meta-Analysis of the AUDIT as an Indicator of Alcohol Use Disorders. Alcohol. Clin. Exp. Res. 2019, 43, 2028–2037. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef] [Green Version]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Keogh, P.; Reid, D.; Bourne, A.; Weatherburn, P.; Hickson, F.; Jessup, K.; Hammond, G. Wasted Opportunities: Problematic Alcohol and Drug Use among Gay Men and Bisexual Men; Sigma Research: London, UK, 2009; ISBN 1-872956-97-1. [Google Scholar]
- Hampel, B.; Kusejko, K.; Kouyos, R.D.; Böni, J.; Flepp, M.; Stöckle, M.; Conen, A.; Béguelin, C.; Künzler-Heule, P.; Nicca, D.; et al. Chemsex drugs on the rise: A longitudinal analysis of the Swiss HIV Cohort Study from 2007 to 2017. HIV Med. 2020, 21, 228–239. [Google Scholar] [CrossRef]
- Dolengevich-Segal, H.; Rodríguez-Salgado, B.; Gómez-Arnau, J.; Sánchez-Mateos, D. Severe Psychosis, Drug Dependence, and Hepatitis C Related to Slamming Mephedrone. Case Rep. Psychiatry 2016, 2016, 8379562. [Google Scholar] [CrossRef] [Green Version]
- Lev-Ran, S.; Roerecke, M.; Le Foll, B.; George, T.P.; McKenzie, K.; Rehm, J. The association between cannabis use and depression: A systematic review and meta-analysis of longitudinal studies. Psychol. Med. 2014, 44, 797–810. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Chen, X.; Lam, E.H.K.; Li, J.; Kahler, C.W.; Lau, J.T.F. The Moderating Role of Social Support on the Relationship Between Anxiety, Stigma, and Intention to Use Illicit Drugs Among HIV-Positive Men Who Have Sex with Men. AIDS Behav. 2020, 24, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Hellem, T.L. A Review of Methamphetamine Dependence and Withdrawal Treatment: A Focus on Anxiety Outcomes. J. Subst. Abuse Treat. 2016, 71, 16–22. [Google Scholar] [CrossRef]
- van Noorden, M.S.; Kamal, R.; de Jong, C.A.J.; Vergouwen, A.C.M.T.; Zitman, F.G. Gamma-hydroxybutyric acid (GHB) dependence and the GHB withdrawal syndrome: Diagnosis and treatment. Ned. Tijdschr. Geneeskd. 2010, 154, A1286. [Google Scholar] [PubMed]
- Coyle, R.M.; Lampe, F.C.; Miltz, A.R.; Sewell, J.; Anderson, J.; Apea, V.; Collins, S.; Dhairyawan, R.; Johnson, A.M.; Lascar, M.; et al. Associations of depression and anxiety symptoms with sexual behaviour in women and heterosexual men attending sexual health clinics: A cross-sectional study. Sex. Transm. Infect. 2019, 95, 254–261. [Google Scholar] [CrossRef] [Green Version]
- Foley, J.D.; Vanable, P.A.; Brown, L.K.; Carey, M.P.; DiClemente, R.J.; Romer, D.; Valois, R.F. Depressive Symptoms as a Longitudinal Predictor of Sexual Risk Behaviors among African American Adolescents. Health Psychol. 2019, 38, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Miltz, A.R.; Rodger, A.J.; Sewell, J.; Speakman, A.; Phillips, A.N.; Sherr, L.; Gilson, R.J.; Asboe, D.; Nwokolo, N.C.; Clarke, A.; et al. Clinically significant depressive symptoms and sexual behaviour among men who have sex with men. BJPsych Open 2017, 3, 127–137. [Google Scholar] [CrossRef] [Green Version]
- Rimes, K.A.; Ion, D.; Wingrove, J.; Carter, B. Sexual orientation differences in psychological treatment outcomes for depression and anxiety: National cohort study. J. Consult. Clin. Psychol. 2019, 87, 577–589. [Google Scholar] [CrossRef] [Green Version]
- Semlyen, J.; King, M.; Varney, J.; Hagger-Johnson, G. Sexual orientation and symptoms of common mental disorder or low wellbeing: Combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 2016, 16, 67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneeberger, A.R.; Dietl, M.F.; Muenzenmaier, K.H.; Huber, C.G.; Lang, U.E. Stressful childhood experiences and health outcomes in sexual minority populations: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1427–1445. [Google Scholar] [CrossRef]
- Hibbert, M.P.; Germain, J.S.; Brett, C.E.; Van Hout, M.-C.; Hope, V.D.; Porcellato, L.A. Service provision and barriers to care for men who have sex with men engaging in chemsex and sexualised drug use in England. Int. J. Drug Policy 2021, 92, 103090. [Google Scholar] [CrossRef]
- Pienaar, K.; Murphy, D.A.; Race, K.; Lea, T. Problematising LGBTIQ drug use, governing sexuality and gender: A critical analysis of LGBTIQ health policy in Australia. Int. J. Drug Policy 2018, 55, 187–194. [Google Scholar] [CrossRef]
- Race, K. Thinking with pleasure: Experimenting with drugs and drug research. Int. J. Drug Policy 2017, 49, 144–149. [Google Scholar] [CrossRef]
- Weatherburn, P.; Hickson, F.; Reid, D.; Torres-Rueda, S.; Bourne, A. Motivations and values associated with combining sex and illicit drugs (‘chemsex’) among gay men in South London: Findings from a qualitative study. Sex. Transm. Infect. 2017, 93, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Stuart, A.L.; Pasco, J.A.; Jacka, F.N.; Brennan, S.L.; Berk, M.; Williams, L.J. Comparison of self-report and structured clinical interview in the identification of depression. Compr. Psychiatry 2014, 55, 866–869. [Google Scholar] [CrossRef] [PubMed]
- Verdejo-García, A.; Bechara, A.; Recknor, E.C.; Pérez-García, M. Executive dysfunction in substance dependent individuals during drug use and abstinence: An examination of the behavioral, cognitive and emotional correlates of addiction. J. Int. Neuropsychol. Soc. 2006, 12, 405–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Population | Intervention | Outcome |
|---|---|---|
| Men who have sex with men | Sexualized drug | Psychological disorders |
| (MSM) Gay man/men Bisexual man/men Homosexual man/men | Sexualized drug use Sexualized substance Slamsex Party and play Chemsex Mephedrone Cathinones N-methyl-3,4-methylenedioxyamphetamine MDMA GHB Gamma hydroxybutyrate Gamma hydroxybutyric acid Ketamine Cocaine Poppers Methamphetamine Viagra | Psychiatric disease Mental disorders Mental health Mental health symptoms Mental health outcomes Psychological wellbeing Anxiety Depression Addictive Behavior |
| Author and Year | Study | Title | Year of Study | Journal | Country | Objective | Study Design | n (Age) |
|---|---|---|---|---|---|---|---|---|
| (Batisse et al., 2016) [59] | - | Use of psychostimulants in a sexual context: Analysis of cases reported to the French network of Addictovigilance Centers | 2016 | Therapies | France | Estimate prevalence of psychiatric disorders, intoxication, dependence and substance abuse in people who practice slamsex. | Cross-sectional | 51 (Mean = 40) |
| (Brogan et al., 2019) [22] | Canadian EMIS-2017 | Canadian results from the European Men-who-have-sex-with-men Internet survey (EMIS-2017) | 2019 | Canada Communicable Disease Report | Canada | Assess needs related to sexually transmitted infections of gays, bisexuals, and other men who have sex with men. | Cross-sectional | 5165 (Median = 36) |
| (Card et al., 2019) [60] | Momentum Health Study | Escape expectancies and sexualized substance use among gay, bisexual, and other men who have sex with men | 2019 | AIDS care | Canada | Examine how McKirnan’s Cognitive Escape Theory (CES) is related to the use of sexualized substances. | Cross-sectional | 774 (Range = 25–47) |
| (Demant & Oviedo-Trespalacios, 2019) [61] | - | Harmless? A hierarchical analysis of poppers use correlates among young gay and bisexual men | 2019 | Drug and Alcohol Review | Australia | Examine recent poppers use patterns with personal characteristics, other substance use, as well as mental and psychosocial health. | Cross-sectional | 836 (Mean = 23.4) |
| (Dolengevich-Segal et al., 2019) [62] | U-SEX GESIDA 9416 study | Drug-related and psychopathological symptoms in HIV-positive men who have sex with men who inject drugs during sex (slamsex): Data from the U-SEX GESIDA 9416 Study | 2019 | Plos One | Spain | Describe the physical and psychopathological symptoms of sexualized intravenous drug use (slamsex). | Cross-sectional | 742 (Range = 33–44) |
| (Hammoud et al., 2017) [63] | Following Lives Undergoing Change (Flux) Study | Intensive sex partying with gamma-hydroxybutyrate: factors associated with using gamma-hydroxybutyrate for chemsex among Australian gay and bisexual men—results from the Flux Study | 2017 | Sexual Health | Australia | To study factors associated with the use of GHB and its relationship with sex: risk behavior, contexts, consequences and motivations for its use. | Prospective observational | 3190 (Mean = 35) |
| (Hibbert et al., 2019) [64] | - | Psychosocial and sexual characteristics associated with sexualized drug use and chemsex among men who have sex with men (MSM) in the UK | 2019 | Sexually Transmitted Infections | United Kingdom | To study psychosocial and sexual patterns of the use of sexualized drugs in men who have a relationship with other men. | Cross-sectional | 3676 (Mean = 30.7) |
| (Nöstlinger et al., 2020) [65] | Be-PrEP-ared | Drug use, depression and sexual risk behavior: a syndemic among early pre-exposure prophylaxis (PrEP) adopters in Belgium? | 2020 | AIDS Care | Belgium | To assess the interaction of drug use and depression with risky sexual behavior. | Longitudinal, prospective cohort study | Baseline (200), M9 (186) and M18 (179) (Range = 22–70) |
| (Schecke et al., 2019) [66] | German Chemsex Survey | Crystal Methamphetamine use in sexual settings among German men who have sex with men | 2019 | Frontiers in Psychiatry | Germany | To study the use of methamphetamine in sexual settings and its association with the acquisition and transmission of sexually transmitted infections. | Cross-sectional | 1050 (Mean = 34.5) |
| (Sewell et al., 2017) [14] | AURAH | Poly drug use, chemsex drug use, and associations with sexual risk behavior in HIV-negative men who have sex with men attending sexual health clinics | 2017 | International Journal of Drug Policy | England | To assess prevalence of multiple drug use and chemsex practice and its association with risky sexual behavior. | Cross-sectional | 1484 (Median = 31.5) |
| (Trouiller et al., 2020) [67] | PREVAGAY 2015 bio-behavioural survey | Injecting drug use during sex (known as “slamming”) among men who have sex with men: Results from a time-location sampling survey conducted in five cities, France | 2020 | International Journal of Drug Policy | France | Estimate prevalence of men who practice slamsex and identify factors associated with this practice. | Cross-sectional | 2610 (Range = 28.7 –43) |
| (Vaccher et al., 2020) [58] | Prevalence, frequency, and motivations for alkyl nitrite use among gay, bisexual and other men who have sex with men in Australia | 2020 | International Journal of Drug Policy | Australia | To determine the prevalence and frequency of popper use and the factors associated with its use and to examine the motivations for using poppers. | Prospective observational | 3273 (Range = 25–46) |
| Author and Year | Chemsex | Drugs | Cannabis | Poppers | GHB/ GBL | Mephedrone | Speed/ Meth | Ketamine | MDMA | Viagra | Cocaine | Slamming |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Batisse et al. (2016) [59] | 90% | Of those who practice slamming | 11% | 11% | 13% | ** | 8% | 8% | 6% | - | 33% | * 60.78% |
| Brogan et al. (2019) [22] | 5.8% (previous 6 months) | Of the entire sample | 46.6% | - | 7.35% | 0.40% | 6.1 % | - | 8.7% | - | 14% | 3.5% |
| Card et al. (2019) [60] | 11.59% (previous 6 months) | Of the entire sample | - | - | - | - | - | - | - | - | - | - |
| Demant & Oviedo-Trespalacios, (2019) [61] | - | Of the entire sample | - | * 43.8% | - | - | - | - | - | - | - | - |
| Dolengevich-Segal et al. (2019) [62] | 29.11% (previous 12 months) | From chemsex group | - | 78.7% | 71.7% | 69.4% | 29.6% | 36.1% | 48.6% | - | 45.4% | * 15.7% |
| Hammoud et al. (2017) [63] | 16.9% (previous 6 months) | Of the entire sample | 30.0% | 35.1% | * 5.4% | - | 12% | - | 17.7% | 36.4% | - | - |
| Hibbert et al. (2019) [64] | 6% (previous 12 months) | From sexualized drug use sample | 13% | 28% | 3% | 3% | 1% | 2% | 4% | 12% | 10% | - |
| Nöstlinger et al. (2020) [65] | Baseline: 45% (previous 3 months) | Of the entire Sample (baseline) | - | - | 38.5% | 7.5% | 15% | 34.5% | 42.5% | - | 30% | - |
| Schecke et al. (2019) [66] | 12.4% (previous 12 months) | Of those who used methamphetamine | 51.5% | 93.8% | 70.8% | 40.8% | * | 53.8% | 62.3% | 76.2% | 46.9% | - |
| Sewell et al. (2017) [14] | 21.8% (previous 3 months) | Of the entire sample | 21.0% | 32.9% | 12.0% | 19.1% | 6.4% | 8.4% | 13.0% | 17.1% | 19.4% | 2% |
| Trouiller et al. (2020) [67] | 20.8% (previous 12 months) | Of those who practice slamming | - | - | 49% | 55% | 43% | - | - | - | 43% | * 3.1% |
| Vaccher et al. (2020) [58] | 26.3% (previous 6 months) | Of those who used poppers | - | * 45.9% | 16.5% | - | 20% | - | 33.1% | - | 28.4% | - |
| (Batisse et al., 2016) [59] | (Brogan et al., 2019) [22] | (Card et al., 2019) [60] | (Demant & Oviedo-Trespalacios, 2019) [61] | (Dolengevich-Segal et al., 2019) [62] | (Hammoud et al., 2017) [63] | (Hibbert et al., 2019) [64] | (Nöstlinger et al., 2020) [65] | (Schecke et al., 2019) [66] | (Sewell et al., 2017) [14] | (Trouiller et al., 2020) [67] | (Vaccher et al., 2020) [58] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PHQ-4 | * | |||||||||||
| PHQ-9 | * | |||||||||||
| PHQ-15 | * | |||||||||||
| CAGE-4 | * | |||||||||||
| EMS | * | |||||||||||
| HADS | * | |||||||||||
| SSSS | * | |||||||||||
| SAS | * | |||||||||||
| SOS | * | |||||||||||
| ASSIST | * | |||||||||||
| PSOC-LGBT | * | |||||||||||
| DTCQ | * | |||||||||||
| SUMS | * | |||||||||||
| MHC | * | |||||||||||
| K10 | * | * | ||||||||||
| BRS | * | |||||||||||
| MSS | * | |||||||||||
| CISS | * | |||||||||||
| AUDIT-C | * | * | ||||||||||
| SMSE | * | |||||||||||
| GAD-7 | * | * | * | * | ||||||||
| IHS | * | |||||||||||
| OBCS | * | |||||||||||
| UCLA | * | |||||||||||
| SWLS | * | |||||||||||
| RSE | ||||||||||||
| SDS | ||||||||||||
| PC-PTSD | * | |||||||||||
| SF-36 | * | |||||||||||
| GSE | * | |||||||||||
| * | ||||||||||||
| SS | * | |||||||||||
| SPB | * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Íncera-Fernández, D.; Gámez-Guadix, M.; Moreno-Guillén, S. Mental Health Symptoms Associated with Sexualized Drug Use (Chemsex) among Men Who Have Sex with Men: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 13299. https://doi.org/10.3390/ijerph182413299
Íncera-Fernández D, Gámez-Guadix M, Moreno-Guillén S. Mental Health Symptoms Associated with Sexualized Drug Use (Chemsex) among Men Who Have Sex with Men: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(24):13299. https://doi.org/10.3390/ijerph182413299
Chicago/Turabian StyleÍncera-Fernández, Daniel, Manuel Gámez-Guadix, and Santiago Moreno-Guillén. 2021. "Mental Health Symptoms Associated with Sexualized Drug Use (Chemsex) among Men Who Have Sex with Men: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 24: 13299. https://doi.org/10.3390/ijerph182413299
APA StyleÍncera-Fernández, D., Gámez-Guadix, M., & Moreno-Guillén, S. (2021). Mental Health Symptoms Associated with Sexualized Drug Use (Chemsex) among Men Who Have Sex with Men: A Systematic Review. International Journal of Environmental Research and Public Health, 18(24), 13299. https://doi.org/10.3390/ijerph182413299






