Scoping Review of Intervention Strategies for Improving Coverage and Uptake of Maternal Nutrition Services in Southeast Asia
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Question
2.2. Information Sources and Search Strategy
2.3. Eligibility Criteria
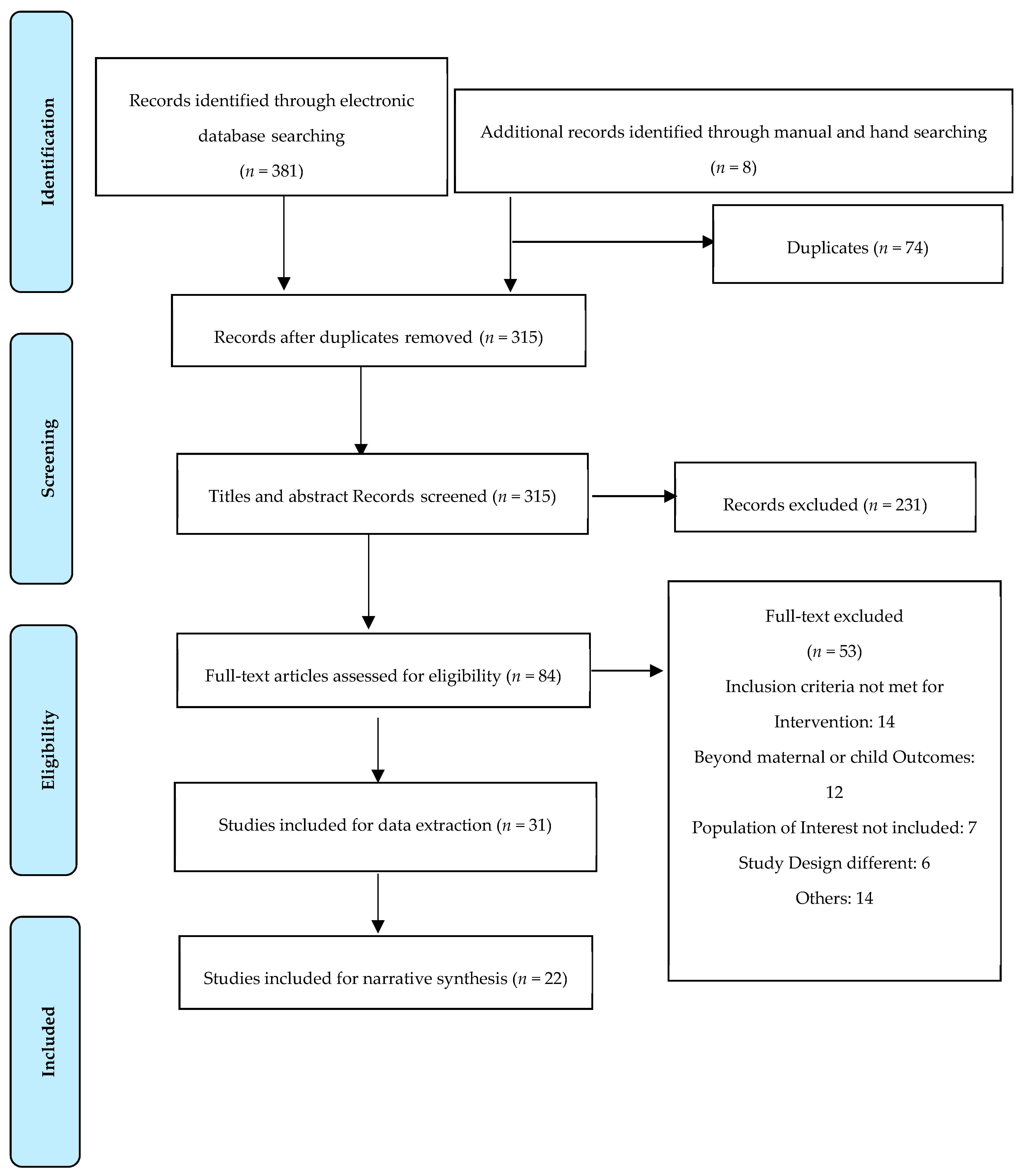
2.4. Study-Selection Process
2.5. Data-Extraction Process
2.6. Collating, Summarizing, and Reporting the Results
3. Results
3.1. Quality Appraisal
3.2. Characteristics of Included Articles
3.3. Summary of Interventions
- Micronutrient supplementation (IFA, calcium, and multiple micronutrients)
- b.
- Nutrition education and counselling
- c.
- Balanced energy-protein supplementation
- d.
- Barriers affecting coverage, uptake, and compliance of program delivery
4. Discussion
4.1. Effect of Home Visits by CHW on Compliance with Nutrition Interventions
4.2. Effects of Nutrition Education and Counselling on Compliance and Uptake of Nutrition Services or Intervention
4.3. Effects of Food or Cash Transfer on Compliance and Uptake of Nutrition Services
4.4. Effect of Community-Level Events, Social Marketing Campaigns or Group Sessions on Compliance and Uptake of Nutrition Services
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Ahmed, T.; Hossain, M.; Sanin, K.I. Global Burden of Maternal and Child Undernutrition and Micronutrient Deficiencies. Ann. Nutr. Metab. 2012, 61 (Suppl. S1), 8–17. [Google Scholar] [CrossRef]
- Christian, P.; Smith, E.R.; Zaidi, A. Addressing inequities in the global burden of maternal undernutrition: The role of target-ing. BMJ Glob. Health 2020, 5, e002186. [Google Scholar] [CrossRef]
- Development Initiatives. Global Nutrition Report 2017: Nourishing the SDGs; Development Initiatives: Bristol, UK, 2017. [Google Scholar]
- Directorate of Community Nutrition, Ministry of Health. Atmarita: Nutrition problems in Indonesia. In Proceedings of the Integrated International Seminar and Workshop on Lifestyle-Related Diseases 2005, Yogyakarta, Indonesia, 19–20 March 2005. [Google Scholar]
- Swaminathan, S.; Hemalatha, R.; Pandey, A.; Kassebaum, N.J.; Laxmaiah, A.; Longvah, T.; Lodha, R.; Ramji, S.; Kumar, G.A.; Afshin, A.; et al. The burden of child and maternal malnutrition and trends in its indicators in the states of India: The Global Burden of Disease Study 1990–2017. Lancet Child Adolesc. Health 2019, 3, 855–870. [Google Scholar] [CrossRef]
- Bellizzi, S.; Pichierri, G.; Napodano, C.M.P.; Salaris, P.; Fiamma, M.; Fozza, C.; Cegolon, L. Iron deficiency anaemia and low BMI among adolescent girls in India: The transition from 2005 to 2015. Public Health Nutr. 2021, 24, 1577–1582. [Google Scholar] [CrossRef]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Kumera, G.; Gedle, D.; Alebel, A.; Feyera, F.; Eshetie, S. Undernutrition and its association with socio-demographic, anemia and intestinal parasitic infection among pregnant women attending antenatal care at the University of Gondar Hospital, Northwest Ethiopia. Matern. Health Neonatol. Perinatol. 2018, 4, 18. [Google Scholar] [CrossRef] [PubMed]
- Dadi, A.F.; Desyibelew, H.D. Undernutrition and its associated factors among pregnant mothers in Gondar town, Northwest Ethiopia. PLoS ONE 2019, 14, e0215305. [Google Scholar] [CrossRef] [PubMed]
- Endalifer, M.; Tewabe, M.; Adar, A. Undernutrition and associated factors among pregnant women attending ANC follow up in Alamata general hospital, Northern Region, Ethiopia, 2017. J. Nutr. Health Food Eng. 2019, 9, 70–78. [Google Scholar]
- Bhutta, Z.A.; Gupta, I.; De’Silva, H.; Manandhar, D.; Awasthi, S.; Hossain, S.M.M.; Salam, M.A. Maternal and child health: Is South Asia ready for change? BMJ 2004, 328, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Perez-Escamilla, R.; Bermudez, O.; Buccini, G.S.; Kumanyika, S.; Lutter, C.K.; Monsivais, P.; Victora, C. Nutrition disparities and the global burden of malnutrition. BMJ 2018, 361, k2252. [Google Scholar] [CrossRef]
- Goudet, S.; Murira, Z.; Torlesse, H.; Hatchard, J.; Busch-Hallen, J. Effectiveness of programme approaches to improve the cover-age of maternal nutrition interventions in South Asia. Matern. Child Nutr. 2018, 14 (Suppl. S4), e12699. [Google Scholar] [CrossRef] [PubMed]
- Blencowe, H.; Krasevec, J.; de Onis, M.; Black, R.E.; An, X.; Stevens, G.A.; Borghi, E.; Hayashi, C.; Estevez, D.; Cegolon, L.; et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Health 2019, 7, e849–e860. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRIS-MA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute. Critical Appraisal Tools. Available online: https://joannabriggs.org/critical-appraisal-tools (accessed on 15 November 2019).
- Bhutta, Z.A.; Rizvi, A.; Raza, F.; Hotwani, S.; Zaidi, S.; Hossain, S.M.; Soofi, S.; Bhutta, S. A Comparative Evaluation of Multiple Micronutrient and Iron–Folic Acid Supplementation during Pregnancy in Pakistan: Impact on Pregnancy Outcomes. Food Nutr. Bull. 2009, 30, S496–S505. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Utomo, B.; Hidayat, A.; Subarkah, K. Preventing low birthweight through maternal multiple micro-nutrient supplementation: A cluster-randomized, controlled trial in Indramayu, West Java. Food Nutr. Bull. 2009, 30 (Suppl. S4), S488–S495. [Google Scholar] [CrossRef]
- Rah, J.H.; de Pee, S.; Halati, S.; Parveen, M.; Mehjabeen, S.S.; Steiger, G.; Bloem, M.W.; Kraemer, K. Provision of Micronutrient Powder in Response to the Cyclone Sidr Emergency in Bangladesh: Cross-Sectional Assessment at the end of the Intervention. Food Nutr. Bull. 2011, 32, 277–285. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Lowe, A.; Vir, S.; Kumar, S.; Mohanraj, R.; Chaturvedi, A.; Noznesky, E.A.; Martorell, R.; Mason, J.B. Public health interventions, barriers, and opportunities for improving maternal nutrition in India. Food Nutr. Bull. 2012, 33 (Suppl. S1), S71–S92. [Google Scholar] [CrossRef]
- Noznesky, E.A.; Ramakrishnan, U.; Martorell, R. A Situation Analysis of Public Health Interventions, Barriers, and Opportunities for Improving Maternal Nutrition in Bihar, India. Food Nutr. Bull. 2012, 33, S93–S103. [Google Scholar] [CrossRef]
- Nisar, Y.B.; Dibley, M.J. Earlier initiation and use of a greater number of iron-folic acid supplements during pregnancy pre-vents early neonatal deaths in Nepal and Pakistan. PLoS ONE 2014, 9, e112446. [Google Scholar] [CrossRef] [PubMed]
- Vir, S.C.; Kalita, A.; Mondal, S.; Malik, R. Impact of community-based mitanin programme on undernutrition in rural Chhattisgarh State, India. Food Nutr. Bull. 2014, 35, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Gernand, A.D.; Schulze, K.J.; Nanayakkara-Bind, A.; Arguello, M.; Shamim, A.A.; Ali, H.; Wu, L.; West, K.P., Jr.; Christian, P. Effects of prenatal multiple micronutrient supplementation on fetal growth factors: A cluster-randomized, controlled trial in rural Bangladesh. PLoS ONE 2015, 10, e0137269. [Google Scholar] [CrossRef]
- Memon, Z.A.; Khan, G.N.; Soofi, S.B.; Baig, I.Y.; Bhutta, Z.A. Impact of a community-based perinatal and newborn preventive care package on perinatal and neonatal mortality in a remote mountainous district in Northern Pakistan. BMC Pregnancy Childbirth 2015, 15, 106. [Google Scholar] [CrossRef] [PubMed]
- Sablok, A.; Batra, A.; Thariani, K.; Batra, A.; Bharti, R.; Aggarwal, A.R.; Kabi, B.; Chellani, H. Supplementation of vitamin D in pregnancy and its correlation with feto-maternal outcome. Clin. Endocrinol. 2015, 83, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Kosec, K.; Avula, R.; Holtemeyer, B.; Tyagi, P.; Hausladen, S.; Menon, P. Predictors of essential health and nutrition service delivery in Bihar, India: Results from household and frontline worker surveys. Glob. Health Sci. Pract. 2015, 3, 255–273. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jolly, S.P.; Rahman, M.; Afsana, K.; Yunus, F.M.; Chowdhury, A.M.R. Evaluation of Maternal Health Service Indicators in Urban Slum of Bangladesh. PLoS ONE 2016, 11, e0162825. [Google Scholar] [CrossRef]
- Kadiyala, S.; Morgan, E.H.; Cyriac, S.; Margolies, A.; Roopnaraine, T. Adapting Agriculture Platforms for Nutrition: A Case Study of a Participatory, Video-Based Agricultural Extension Platform in India. PLoS ONE 2016, 11, e0164002. [Google Scholar] [CrossRef]
- Mridha, M.K.; Matias, S.L.; Chaparro, C.M.; Paul, R.R.; Hussain, S.; Vosti, S.A.; Harding, K.L.; Cummins, J.R.; Day, L.T.; Saha, S.L.; et al. Lipid-based nutrient supplements for pregnant women reduce newborn stunting in a cluster-randomized controlled effectiveness trial in Bangladesh. Am. J. Clin. Nutr. 2016, 103, 236–249. [Google Scholar] [CrossRef]
- Rahman, M.; Yunus, F.M.; Shah, R.; Jhohura, F.T.; Mistry, S.K.; Quayyum, T.; Aktar, B.; Afsana, K. A Controlled Before-and-After Perspective on the Improving Maternal, Neonatal, and Child Survival Program in Rural Bangladesh: An Impact Analysis. PLoS ONE 2016, 11, e0161647. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Sanghvi, T.; Kim, S.S.; Tran, L.M.; Afsana, K.; Mahmud, Z.; Aktar, B.; Menon, P. Factors influencing maternal nutrition practices in a large scale maternal, newborn and child health program in Bangladesh. PLoS ONE 2017, 12, e0179873. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.H.; Kim, S.S.; Sanghvi, T.; Mahmud, Z.; Tran, L.M.; Shabnam, S.; Aktar, B.; Haque, R.; Afsana, K.; Frongillo, E.A.; et al. Integrating Nutrition Interventions into an Existing Maternal, Neonatal, and Child Health Program Increased Maternal Dietary Diversity, Micronutrient Intake, and Exclusive Breastfeeding Practices in Bangladesh: Results of a Cluster-Randomized Program Evaluation. J. Nutr. 2017, 147, 2326–2337. [Google Scholar] [CrossRef]
- Raghunathan, K.; Chakrabarti, S.; Avula, R.; Kim, S.S. Can conditional cash transfers improve the uptake of nutrition interventions and household food security? Evidence from Odisha’s Mamata scheme. PLoS ONE 2017, 12, e0188952. [Google Scholar] [CrossRef] [PubMed]
- Dewey, K.G.; Mridha, M.K.; Matias, S.L.; Arnold, C.D.; Cummins, J.R.; Khan, S.A.; Maalouf-Manasseh, Z.; Siddiqui, Z.; Ullah, B.; Vosti, S.A. Lipid-based nutrient supplementation in the first 1000 d improves child growth in Bangladesh: A cluster-randomized effectiveness trial. Am. J. Clin. Nutr. 2017, 105, 944–957. [Google Scholar] [CrossRef]
- Nair, N.; Tripathy, P.; Sachdev, H.S.; Pradhan, H.; Bhattacharyya, S.; Gope, R.; Gagrai, S.; Rath, S.; Rath, S.; Sinha, R.; et al. Effect of participatory women’s groups and counselling through home visits on children’s linear growth in rural eastern India (CARING trial): A cluster-randomised controlled trial. Lancet Glob. Health 2017, 5, e1004–e1016. [Google Scholar] [CrossRef]
- Harris-Fry, H.; Paudel, P.; Harrisson, T.; Shrestha, N.; Jha, S.; Beard, B.J.; Copas, A.; Shrestha, B.P.; Manandhar, D.S.; Costello, A.M.D.L.; et al. Participatory Women’s Groups with Cash Transfers Can Increase Dietary Diversity and Micronutrient Adequacy during Pregnancy, whereas Women’s Groups with Food Transfers Can Increase Equity in Intrahousehold Energy Allocation. J. Nutr. 2018, 148, 1472–1483. [Google Scholar] [CrossRef] [PubMed]
- Hashmi, A.H.; Paw, M.K.; Nosten, S.; Darakamon, M.C.; Gilder, M.E.; Charunwatthana, P.; Carrara, V.I.; Wickramasinghe, K.; Angkurawaranon, C.; Plugge, E.; et al. ‘Because the baby asks for it’: A mixed-methods study on local perceptions toward nutrition during pregnancy among marginalised migrant women along the Myanmar–Thailand border. Glob. Health Action 2018, 11, 1473104. [Google Scholar] [CrossRef] [PubMed]
- Khanam, F.; Hossain, B.; Mistry, S.K.; Mitra, D.K.; Raza, W.A.; Rifat, M.; Afsana, K.; Rahman, M. The association between daily 500 mg calcium supplementation and lower pregnancy-induced hypertension risk in Bangladesh. BMC Pregnancy Childbirth 2018, 18, 406. [Google Scholar] [CrossRef]
- Saville, N.M.; Shrestha, B.P.; Style, S.; Harris-Fry, H.; Beard, B.J.; Sen, A.; Jha, S.; Rai, A.; Paudel, V.; Sah, R. Impact on birth weight and child growth of Participatory Learning and Action women’s groups with and without transfers of food or cash during pregnancy: Findings of the low birth weight South Asia cluster-randomised controlled trial (LBWSAT) in Nepal. PLoS ONE 2018, 13, e0194064. [Google Scholar] [CrossRef]
- More, N.S.; Waingankar, A.; Ramani, S.; Chanani, S.; D’Souza, V.; Pantvaidya, S.; Fernandez, A.; Jayaraman, A. Community-Based Management of Acute Malnutrition to Reduce Wasting in Urban Informal Settlements of Mumbai, India: A Mixed-Methods Evaluation. Glob. Health Sci. Pract. 2018, 6, 103–127. [Google Scholar] [CrossRef]
- Stevens, A.; Gilder, M.; Moo, P.; Hashmi, A.; Toe, S.; Doh, B.; Nosten, S.; Chotivanich, K.; Somerset, S.; Mcgready, R. Folate supplementation to prevent birth abnormalities: Evaluating a community-based participatory action plan for refugees and migrant workers on the Thailand-Myanmar border. Public Health 2018, 161, 83–89. [Google Scholar] [CrossRef]
- Stevens, B.; Watt, K.; Brimbecombe, J.; Clough, A.; Judd, J.A.; Lindsay, D. A village-matched evaluation of providing a local supplemental food during pregnancy in rural Bangladesh: A preliminary study. BMC Pregnancy Childbirth 2018, 18, 286. [Google Scholar] [CrossRef]
- Svefors, P.; Selling, K.E.; Shaheen, R.; Khan, A.I.; Persson, L.Å.; Lindholm, L. Cost-effectiveness of prenatal food and micronutrient interventions on under-five mortality and stunting: Analysis of data from the MINIMat randomized trial, Bangladesh. PLoS ONE 2018, 13, e0191260. [Google Scholar] [CrossRef]
- Wendt, A.S.; Stephenson, R.; Young, M.F.; Verma, P.; Srikantiah, S.; Webb-Girard, A.; Hogue, C.J.; Ramakrishnan, U.; Martorell, R. Identifying bottlenecks in the iron and folic acid supply chain in Bihar, India: A mixed-methods study. BMC Health Serv. Res. 2018, 18, 281. [Google Scholar] [CrossRef] [PubMed]
- Pavithra, G.; Kumar, S.G.; Roy, G. Effectiveness of a community-based intervention on nutrition education of mothers of mal-nourished children in a rural coastal area of South India. Indian J. Public Health 2019, 63, 4. [Google Scholar]
- Dhaded, S.M.; Hambidge, K.M.; Ali, S.A.; Somannavar, M.; Saleem, S.; Pasha, O.; Khan, U.; Herekar, V.; Vernekar, S.; Kumar, Y.S. Preconception nutrition intervention improved birth length and reduced stunting and wasting in newborns in South Asia: The Women First Randomized Controlled Trial. PLoS ONE 2020, 15, e0218960. [Google Scholar] [CrossRef] [PubMed]
- WHO: E-Library of Evidence for Nutrition Actions (eLENA). Balanced Energy and Protein Supplementation during Pregnancy. 2019. Available online: http://www.who.int/elena/titles/energy_protein_pregnancy/en/ (accessed on 22 February 2020).
- WHO: E-Library of Evidence for Nutrition Actions (eLENA). Daily Iron and Folic Acid Supplementation during Pregnancy. 2019. Available online: http://www.who.int/elena/titles/daily_iron_pregnancy/en/ (accessed on 22 February 2020).
- Kumar, A.; Kaur, S. Calcium: A Nutrient in Pregnancy. J. Obstet. Gynecol. India 2017, 67, 313–318. [Google Scholar] [CrossRef]
- Sanghvi, T.G.; Harvey, P.W.; Wainwright, E. Maternal iron–folic acid supplementation programs: Evidence of impact and implementation. Food Nutr. Bull. 2010, 31 (Suppl. S2), S100–S107. [Google Scholar] [CrossRef]
- Mason, J.B.; Saldanha, L.S.; Ramakrishnan, U.; Lowe, A.; Noznesky, E.A.; Girard, A.W.; McFarland, D.A.; Martorell, R. Opportunities for Improving Maternal Nutrition and Birth Outcomes: Synthesis of Country Experiences. Food Nutr. Bull. 2012, 33, S104–S137. [Google Scholar] [CrossRef]
- Edmond, K.M.; Yousufi, K.; Anwari, Z.; Sadat, S.M.; Staniczai, S.M.; Higgins-Steele, A.; Bellows, A.L.; Smith, E.R. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Med. 2018, 16, 106. [Google Scholar] [CrossRef]
- Girard, A.W.; Olude, O. Nutrition Education and Counselling Provided during Pregnancy: Effects on Maternal, Neonatal and Child Health Outcomes. Paediatr. Périnat. Epidemiol. 2012, 26, 191–204. [Google Scholar] [CrossRef]
- Garg, A.; Kashyap, S. Effect of counseling on nutritional status during pregnancy. Indian J. Pediatr. 2006, 73, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Barros, F.C.; Assunção, M.C.; Restrepo-Méndez, M.C.; Matijasevich, A.; Martorell, R. Scaling up maternal nutrition programs to improve birth outcomes: A review of implementation issues. Food Nutr. Bull. 2012, 33 (Suppl. S1), S6–S26. [Google Scholar] [CrossRef]
- Vaivada, T.; Gaffey, M.F.; Das, J.K.; Bhutta, Z.A. Evidence-based interventions for improvement of maternal and child nutrition in low-income settings: What’s new? Curr. Opin Clin. Nutr. Metab. Care 2017, 20, 204–210. [Google Scholar] [CrossRef]
- Alam, A.; Rasheed, S.; Khan, N.U.; Sharmin, T.; Huda, T.M.; Arifeen, S.E.; Dibley, M.J. How can formative research inform the design of an iron-folic acid supplementation intervention starting in first trimester of pregnancy in Bangladesh? BMC Public Health 2015, 15, 374. [Google Scholar] [CrossRef]
- Gope, R.K.; Tripathy, P.; Prasad, V.; Pradhan, H.; Sinha, R.K.; Panda, R.; Chowdhury, J.; Murugan, G.; Roy, S.; De, M.; et al. Effects of participatory learning and action with women’s groups, counselling through home visits and crèches on undernutrition among children under three years in eastern India: A quasi-experimental study. BMC Public Health 2019, 19, 962. [Google Scholar] [CrossRef]
- Rivera, J.A.; Sotres-Alvarez, D.; Habicht, J.-P.; Shamah, T.; Villalpando, S. Impact of the Mexican program for education, health, and nutrition (Progresa) on rates of growth and anemia in infants and young children: A randomized effectiveness study. JAMA 2004, 291, 2563–2570. [Google Scholar] [CrossRef] [PubMed]
- Olney, D.K.; Leroy, J.L.; Bliznashka, L.; Ruel, M. PROCOMIDA, a Food-Assisted Maternal and Child Health and Nutrition Program, Reduces Child Stunting in Guatemala: A Cluster-Randomized Controlled Intervention Trial. J. Nutr. 2018, 148, 1493–1505. [Google Scholar] [CrossRef]
- Leroy, J.L.; Olney, D.; Ruel, M. Tubaramure, a Food-Assisted Integrated Health and Nutrition Program, Reduces Child Stunting in Burundi: A Cluster-Randomized Controlled Intervention Trial. J. Nutr. 2018, 148, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Olaniran, A.; Madaj, B.; Bar-Zev, S.; van den Broek, N. The roles of community health workers who provide maternal and new-born health services: Case studies from Africa and Asia. BMJ Glob. Health 2019, 4, e001388. [Google Scholar] [CrossRef]
- Adah, S.; Ogbonna, C.; Anga, P.; Chingle, M.; Ashikeni, M.; Envuladu, E.; Agaba, C.; Audu, S.; Bupwatda, P.; Zoakah, A.J. The impact of advocacy and community mobilization on the utilization of health services at the Comprehensive Health Centre, Gindiri. Jos J. Med. 2009, 4, 11–13. [Google Scholar] [CrossRef][Green Version]
- Khan, N.C.; Thanh, H.T.K.; Berger, J.; Hoa, P.T.; Quang, N.D.; Smitasiri, S.; Cavalli-Sforza, T. Community mobilization and social marketing to promote weekly iron-folic acid supplementation: A new approach toward controlling anemia among women of reproductive age in Vietnam. Nutr. Rev. 2005, 63 (Suppl. S2), S87–S94. [Google Scholar] [CrossRef]
- Chaparro, C.; Oot, L.; Sethuraman, K. India Nutrition Profile. 2014. Available online: https://www.fantaproject.org/sites/default/files/download/India-Nutrition-Profile-Mar2014.pdf (accessed on 23 February 2020).
| Authors | Study Design | Sample Size | Study Population | Location of the Study | Intervention/ Comparison | Study Outcomes | Delivery Mechanism | Change in Coverage/Uptake |
|---|---|---|---|---|---|---|---|---|
| Bhutta, et al. (2009) [17] | Cluster RCT | I: 1148 C: 1230 | Pregnant women | Pakistan (rural and urban) | I: Multiple micronutrients C: IFA only | Increased maternal monthly weight gain and reduced LBW prevalence in the intervention group; no significant improvement in iron status of women, but the control group had a higher prevalence of subclinical zinc deficiency. | Trained female CHW visited fortnightly | No significant difference in uptake of ANC visits or consumption of IFA tablets |
| Sunawang, et al. (2009) [18] | Cluster RCT | I: 432 C: 411 | Pregnant women | Indonesia | I: Multiple micronutrients C: IFA only | No statistical difference in the birth parameters of child (birth weight, length, head circumference), pregnancy outcome (miscarriage, stillbirth, or neonatal death), or maternal hemoglobin or serum levels of zinc, retinol and ferritin, and urinary iodine. | Field workers of the project visited daily (except Sunday) | High rate of adherence to supplementation (uptake of IFA or MNP) observed in both groups (no statistical difference) due to home visits and monitoring by field workers |
| Rah, et al. (2011) [19] | Cross-sectional assessment in intervention and control areas | I: 358 C: 361 | Lactating mothers | Bangladesh | I: Micronutrient powder + IFA tablets + fortified food ration + social marketing campaign + education sessions C: IFA tablets + fortified food ration | No statistical difference in mean weight, height, BMI, hemoglobin levels, and anemia prevalence between intervention or control group, except proportion of thinness and decreased anemia in women consuming at least 75% sachets, compared to those consuming <75% sachets within the intervention group. | MNP distributors, health and nutrition staff of local NGOs with doctors, midwives, nutritionists, and volunteers | Increased uptake of MNP was reported (compliance) |
| Ramakrishnan, et al. (2012) [20] | Cross-sectional qualitative research | KII: 31 FGD: 35 IDI: 15 | Program officials, health workers (ASHA/ANM/AWW/Doctors) at the central and peripheral level, community leaders, and volunteers. Women 18–45 years. with children ≤3 years. | Tamil Nadu and Uttar Pradesh, India | - | Only 27.6% consumed ≥100 IFA tablets during their most recent pregnancy, 4% took deworming medicine during pregnancy, 20.5% received supplementary food, and 10.9% received nutrition and health education. Barriers were lack of supply of supplements, quality of food, misconceptions concerning intake of certain food products during pregnancy, and in case of take-home ration, sharing of food with the household. | Frontline workers (ASHA, AWW, ANM) | Effective counselling by health workers and targeted media campaigns improve uptake (compliance) |
| Noznesky, et al. (2012) [21] | Qualitative research using KII | KII: 48 | Policy makers, program managers, service providers | Bihar, India | Only 4% consumed deworming pill during their most recent pregnancy, and 0.6% utilized Anganwadi services. Barriers were resource shortages, poverty, lack of awareness, discrimination based on socioeconomic status, as well as policy-related barriers, such as lack of focus on maternal nutrition, knowledge level of the program implementers about maternal undernutrition, and a faulty program management. | Frontline workers (ASHA, AWW, ANM) | Improved essential inputs, management systems, and reduced gender or caste discrimination | |
| Nisar, et al. (2014) [22] | Secondary data analysis: NDHS (2006/2011) and PDHS (2006–07/2012–13) | Pooled NDHS: 8196 mothers Pooled PDHS: 13034 mothers | Mothers | Nepal and Pakistan | I: Any use of IFA or >90 IFA supplements C: No use of IFA | AR of early neonatal deaths was significantly reduced, by 51% in Nepal and 23% in Pakistan, with any use of IFA compared to none. When IFA started at or before the fifth month of pregnancy, the AR of early neonatal mortality was significantly reduced, by 53% in Nepal and 28% in Pakistan, compared to no IFA. When >90 IFA supplements were used and started at or before the fifth month, AR of early neonatal deaths significantly reduced, by 57% in Nepal and 45% in Pakistan. | Public-sector facilities and CHW | Training CHW, making IFA supplements available for free, and increasing demands through awareness-promotion programs |
| Vir, et al. (2014) [23] | Quasi experimental (mixed methods assessment) | I: 1825 C: 1801 | Mothers of children <3 years | Chhattisgarh, India | I *: NSI + Mitanin program C: Only Mitanin program | No significant difference in the nutritional status of children between two groups; more households in the intervention group than in the control group had kitchen gardens (46.6% vs. 32.5%). | Female CHWs (Mitanin) | No significant change in the uptake of IFA tablets but significant improvement in coverage of three ANC visits and ANC within first trimester |
| Gernand, et al. (2015) [24] | Double-blind, cluster-RCT | I: 264 C: 236 | Pregnant women | Bangladesh (rural) | I: Multiple micronutrient powder C: IFA | No difference in maternal plasma levels of hPL o PGH or cord plasma levels of insulin, IGF-1, or IGFBP-1 between two groups; however, higher cord insulin concentration was in women who were short and higher hPL was found in women carrying female fetuses. | Local field workers visited weekly | High compliance with both MNP and IFA noted in the study |
| Memon β, et al. (2015) [25] | Exploratory quasi-experimental design | I: Pre (n = 322) and Post (n = 316) C: Pre (n = 386) and Post (n = 361) | Pregnant women | Northern Pakistan | I: Community mobilization + education on MNHC through CHC and group sessions + Routine health services C: Routine health services | Improvement in ANC, TT vaccination, institutional delivery rate, cord application, delayed bathing, colostrum feeding, early initiation of breastfeeding (<1 h of birth) (p < 0.001), and reduction in perinatal and neonatal mortality rates (p < 0.05) in the intervention group. | Female health workers and CHW conducted monthly household visits, one-to-one sessions, and video sessions | Increased uptake of ANC visits and care |
| Sablok, et al. (2015) [26] | RCT | I: 120 C: 60 | Pregnant women | Delhi, India | I: Vit D Supplementation C: No supplementation of Vit D | Intervention group had lower incidence of preterm labour (p = 0.02); higher number of newborns to mothers in the control group had lower Vit D levels (<25 nmol/L) (p < 0.001) and lower mean birth weight; and higher proportion of SGA in control group (p = 0.04). | Unclear (Department of Obstetrics and Gynecology, Tertiary hospital, Delhi) | Not reported |
| Kosec, et al. (2015) [27] | Secondary data analysis of DLHS and facility workers Surveys 2012 | 6002 households in 400 villages | Household and frontline workers (ASHA, AWW) | Bihar, India | - | Monetary incentives for AWW are strong predictor of receipt of immunization services (0–2 years) and households receiving general nutrition information. | ASHA and AWW delivering routine services | Incentivizing frontline workers and improving performance increase service uptake by households |
| Jolly, et al. (2016) [28] | Cross-sectional comparative study | I: 607 C: 599 | Married women | Bangladesh (Urban slums) | I: MANOSHI ¶ program C: Without MANOSHI services | Increased odds of improved maternal-health service indicators (4 or more ANC visits, receipt of IFA and TT injection, PNC within 48 h of birth, and institutional delivery rate) in the intervention group (p < 0.05). | Female CHW doing household visits | Uptake of four or more ANC checkups, institutional delivery, skilled assisted delivery, and PNC increased in the intervention group |
| Kadiyala, et al. (2016) [29] | A case study of digital green approach (qualitative assessment) | ** I: IDI: 72 SSI: 73 KII: 6 | SHG members (PLW, CFM, mothers of adolescent girls, and other women); MIL, husbands, FLW, key stakeholders, protagonists, FLPP ⁑ | Odisha, India | I: MIYCN BCC + Digital green approach to agriculture extension | Intervention well received by rural communities and viewed as complementary to routine services; intervention was perceived as a credible source of information related to health and nutrition. | CHWs | Participatory, dialogue-based interventions with women’s groups, as well as video education, improved maternal and childcare services |
| Mridha, et al. (2016) [30] | Researcher-blind, longitudinal, cluster-randomized effectiveness trial | I: 1047 C: 2964 | Pregnant women ≤ 20 gestational weeks | Bangladesh (rural) | I: -Mothers given LNS-PLs C: Mother given IFA | Increased mean birth weight, WAZ, birth length, LAZ, head circumference, HCZ, BMIZ in the children born to mothers in the intervention group | NGO staff | Adherence to IFA was more than the intervention |
| Rahman, et al. (2016) [31] | Quasi-experimental study | I: Pre: 4800; Post: 2400 C: Pre: 2400; Post: 1200 | Mothers and children | Bangladesh (rural) | I: Intensive maternal and newborn care services § C: Essential health care services | Increased number of ANC visits (≥4), skilled birth attendance at dlivery, and PNC visits (≥3 visits); reduction in ANC and PNC complications; mother’s knowledge of breastfeeding initiation and initiation of breastfeeding within an hour of birth increased in the intervention group. | CHW | Uptake of family planning methods, four or more ANC visits improved in the intervention group |
| Nguyen, et al. (2017) [32] | Cross-sectional study | Pregnant women (n = 600); Recently delivered (n = 2000) | Pregnant women and recently delivered | Bangladesh | I: Standard nutrition intervention of nutrition education + IFA + and calcium supplementation + deworming + IYCF counseling | Good nutrition knowledge, women’s self-efficacy, perception of enabling social norms, high husband’s support, early and more prenatal visits, provision of free supplements improve maternal nutrition practices (IFA and calcium intake and diverse diets). | Frontline health workers conducted monthly home visits | Observed increase in the uptake of IFA/calcium tablets and four or more prenatal visits |
| Authors | Study Design | Sample Size | Study Population | Location of the Study | Intervention/ Comparison | Study Outcomes | Delivery Mechanism | Change in Coverage/Uptake |
|---|---|---|---|---|---|---|---|---|
| Nguyen, et al. (2017) [33] | Cluster RCT with cross-sectional baseline (2015) and endline (2016) survey | I: PW: 300 RDW: 1000 C: PW: 300 RDW: 1000 | Pregnant women and recently delivered women | Bangladesh | I: nutrition-focused ¶ MNCH intervention C: standard MNCH intervention | Increase in consumption of IFA and calcium supplements, ≥5 food groups, and most macro and micronutrients; increase in individual food groups consumed among women; increase in EBF by women | Salaried health workers and community health volunteers conducted monthly home visits | Increased probability of early ANC visits and receipt of free iron and calcium tablets in the intervention group |
| Raghunathan, et al. (2017) [34] | Cross-sectional study | I: 534 C: 627 | Pregnant and lactating women | Odisha, India | I: women who received money under CCT scheme C: women who did not receive money under CCT scheme | Increase in likelihood of pregnancy registration, receiving ANC services (5 pp), and IFA tablets (10 pp) and a decline of 0.84 on the household food insecurity assessment scale | DBT by the government and essential nutrition intervention by AWW and ASHA | CCT scheme increased the coverage of ANC services, IFA consumption, and pregnancy registration |
| Dewey, et al. (2017) [35] | Researcher-blind, longitudinal, cluster-randomized effectiveness trial | α IFA-MNP = 1052; IFA-LNS = 930; LNS-LNS = 1047; Control (IFA) = 982 | Pregnant women at ≤20 gestational age and children | Bangladesh | α I: IFA-MNP: mother given IFA and child given MNP; IFA-LNS: mother given IFA and child LNS; LNS-LNS: mother and child both given LNS; C: IFA-control: mother given IFA and child given nothing | LNS-LNS group had significantly higher LAZ (+0.13 compared with the IFA-MNP group) and head circumference (+0.15 z score compared with the IFA-Control group); stunting prevalence (LAZ < −2) was lower in the LNS-LNS group at 18 months than in the IFA-MNP group (OR: 0.70; 95% CI: 0.53, 0.92), but the difference diminished by 24 months (OR: 0.81; 95% CI: 0.63, 1.04) | NGO staff | Adherence to the interventions was reported but not to other services, which was higher in LNS-LNS and IFA-LNS than LNS-MNP |
| Nair, et al. (2017) [36] | Cluster RCT | I: PW: 2805; Infants: 1460 C: PW: 2952; Infants: 1541 | Pregnant women and infants | Jharkhand and Odisha, India | I: Single home visit during 3rd trimester, monthly home visit to children < 2 years for counseling and growth promotion, 2–3 participatory meetings with local women’s groups | No significant effect on EBF, timely initiation of complementary feeding, morbidity, appropriate home care, or care-seeking during childhood illnesses of the intervention; more pregnant women and children attained MDD, more mothers washed their hands before feeding children, fewer children were underweight at 18 months, and fewer infants died | Community-based incentivized volunteers | No significant change in the uptake of maternal or childcare services |
| Harris-Fry, et al. (2018) [37] | Cluster RCT | I: PLA: 154 PLA + Cash: 283 PLA + food: 218 C: 150 | Pregnant women | Nepal | * I: Women’s groups practicing PLA, PLA women’s groups with a monthly unconditional food transfer, and PLA women’s groups with a monthly unconditional cash transfer; C: usual government services | All of intervention groups had increased consumption of IFA supplements, MUAC measurements, and intrahousehold allocation of some animal-source foods; however, RDEARs between pregnant women and their mothers-in-law were higher in PLA + food arm, and dietary diversity was 0.4 food groups higher in PLA + cash arm than control arm | Government-incentivized female community health volunteers and nutrition mobilizers | Significant uptake of IFA supplements in the intervention groups |
| Hashmi, et al. (2018) [38] | Convergent parallel mixed-method design | Cross sectional survey = 388 PW FGD = 11 women IDI = 4 midwives | Pregnant women | Thailand | - | A high proportion of women had limited knowledge of and poor dietary practices. Sweetened-drink consumption in the last 24 h, as well as being non-teenaged multigravida woman, significantly associated with high BMI compared to normal BMI | - | Proportion of first antenatal care visit higher for the first trimester than in the second or third trimesters |
| Khanam, et al. (2018) [39] | Retrospective cohort design | Case: Women who had PIH Control: Women did not develop PIH | Pregnant women | Bangladesh | I: MNI program | Women who consumed 500 mg/d calcium tablets for more than 6 months during pregnancy had a 45% lower risk of developing hypertension compared to those who consumed less calcium (RR = 0.55, 95% CI = 0.33–0.93 | CHW | No significant difference in the covergae of four or more ANC visits in PIH or non-PIH women |
| Saville, et al. (2018) [40] | Four-arm cluster RCT | I: PLA + food: 2997; PLA +cash: 3065; PLA only: 2448; C: 2426 | Pregnant women | Nepal | I: Arm 1: PLA only Arm 2: PLA + food supplement Arm 3: PLA + cash transfer C: current gov’t program | Compared to the control arm, mean BW significantly higher in the PLA + food arm, by 78.0 g (95% CI 13.9, 142.0) and not in others; no significant difference in any other outcome (WAZ, LAZ, WLZ, HC, maternal BMI, MUAC, and IYCF) | Female community health volunteers + nutrition mobilizers (incentivized) | Enhanced participation in women’s groups increased institutional delivery rate in the intervention group |
| More, et al. (2018) [41] | Mixed-method, quasi-experimental, cross-sectional design | I: 3455 Children C: 2122 Children | Pregnant women and children under age 3 | Mumbai, India | I: growth monitoring of 0–6 years children + home visits and counselling + CBMNT distribution + health camps + referrals + group meetings and events C: routine ICDS services | Prevalence of wasting decreased by 28% (18% to 13%) in intervention areas and by 5% (16.9% to 16%) in comparison areas; children in intervention areas significantly less likely to be malnourished (adjusted odds ratio, 0.81; confidence interval, 0.67 to 0.99) | Frontline health workers | High levels of coverage and lower levels of wasting, particularly severe wasting, in the program intervention areas. |
| Stevens, et al. (2018) [42] | Mixed-method, cross sectional survey and qualitative study design | Pregnant Women: baseline = 371, end line = 307; Local Health Workers: baseline = 100, end line = 79 | Pregnant women and local health workers | Thailand-Myanmar | I: community-based participatory action plan (workshops for health workers + posters in centers + pamphlets distribution + presentations + small group discussions) | No significant improvement in preconception folic acid uptake; however, substantial increase in local healthcare workers’ knowledge | Local health workers (medics, midwives, nurses + ultrasound workers + basic healthcare workers) | No significant uptake of preconception folic acid |
| Stevens, et al. (2018) [43] | Village-matched cluster RCT (3rd phase of a multiphase RCT) | I: 58 C: 29 | Undernourished pregnant women with MUAC of ≤22.1 cm | Northern Bangladesh (rural) | I: nutrition screening + nutrition education + ANC/PNC services + supplements C: nutrition screening + nutrition education + ANC/PNC services | MUAC significantly larger in infants of mothers in the intervention group compared to control group at 6 months (p < 0.05). Mean BW in babies of supplemented mothers (mean: 2.91 kg; SD: 0.19) higher than in babies of mothers in control group (mean: 2.72 kg; SD: 0.13); proportion of LBW babies in the intervention group was much lower (event rate = 0.04) than in the control group (event rate = 0.16). However, none of these differences are statistically significant (p > 0.05), most likely due to small sample size. The intervention reduced the risk of wasting at 6 months by 63.38% (RRR = 0.6338) and of low birth weight by 88.58% (RRR = 0.8858), with NNT of 2.22 and 6.32, respectively. | Female community nutrition volunteers and one male and one female supervisor | Higher registration of women within the first trimester |
| Svefors, et al. (2018) [44] | Factorial randomized trial (Nov 2001 to Feb 2009) | E60Fe: 738, EMMS: 740, E30Fe: 739, U60Fe: 741, UMMS: 741, U30Fe: 741 | Pregnant women | Bangladesh (rural) | I: MINIMat trial of food supplementation ⁑ (E30Fe, E60Fe, EMMS, U30Fe, U60Fe, UMMS) | By incremental U60Fe to EMMS, one disability adjusted life years, averted at a cost of USD 24 | Community volunteers | Not reported |
| Wendt, et al. (2018) [45] | Cross-sectional, observational, mixed-method (Nov 2011 to July 2012) | IDI: 59 (health workers at state, district, block, health sub-centre, and village levels) ANM survey: 340 | Health workers at state, district, block, health sub-centre, and village levels; ANM | Bihar, India | - | 44% of ANM were out of IFA stock. Stock levels and supply-chain practices varied greatly across districts. Specific bottlenecks impacting IFA were forecasting, procurement, storage, disposal, lack of personnel, and few training opportunities for key players in the supply chain | ASHA, AWW, ANM | Not reported |
| Pavithra, et al. (2019) [46] | Community-based intervention study (December 2012 to October 2014) | I: 64 children C: 64 children | 57 mothers and 60 mothers of 64 moderate and severely malnourished children aged 13–60 months in the intervention group and control group, respectively | Puducherry, India (rural) | I: one-to-one communication with mothers concerning their child’s nutritional status and growth monitoring; education and child feeding practices; reinforcement of contents of health education | Awareness level in all domains increased significantly in the intervention group; 81% (52) of malnourished children turned out normal, whereas in the control group, 64% (41) of became normal; statistically significant difference between the mean changes in protein intake among boys (15.34 g to 19.91 g in the intervention group against 13.6 g to 16.24 g in the control group) and girls (15.09 g to 19.57 g in the intervention group against 13.36 g to 16.51 g in the control group), as well as calorie intake among girls (993.86 kcal to 1116.55 kcal in the intervention group against 992.65 kcal to 1078.75 kcal in the control group) between the two groups | Unclear | Not reported |
| Dhaded, et al. (2020) [47] | Secondary analysis; the parent study was an individually randomized, non-masked, multi-site randomized controlled efficacy trial | I: LBM-PC: 1281; LBM-FT: 1277 C: 1280 | Mothers and their children (newborns) | India and Pakistan (rural) | I: Arm 1: received LBM at least 3-months prior to conception; Arm 2: received LBM near the end of the 1st trimester; additional protein-energy supplement was given to women whose BMI was <20 kg/m2 for both Arm 1 & 2 till delivery | LBM-PC associated with a decrease of 44% in stunting, 24% in wasting, and 26% SGA when compared to the control group; the difference between LBM-FT and control group was marginal | Home visitor research assistants | Increased compliance with supplements in the intervention arms (more in the first arm than the second) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurian, K.; Lakiang, T.; Sinha, R.K.; Kathuria, N.; Krishnan, P.; Mehra, D.; Mehra, S.; Sharma, S. Scoping Review of Intervention Strategies for Improving Coverage and Uptake of Maternal Nutrition Services in Southeast Asia. Int. J. Environ. Res. Public Health 2021, 18, 13292. https://doi.org/10.3390/ijerph182413292
Kurian K, Lakiang T, Sinha RK, Kathuria N, Krishnan P, Mehra D, Mehra S, Sharma S. Scoping Review of Intervention Strategies for Improving Coverage and Uptake of Maternal Nutrition Services in Southeast Asia. International Journal of Environmental Research and Public Health. 2021; 18(24):13292. https://doi.org/10.3390/ijerph182413292
Chicago/Turabian StyleKurian, Kauma, Theophilus Lakiang, Rajesh Kumar Sinha, Nishtha Kathuria, Priya Krishnan, Devika Mehra, Sunil Mehra, and Shantanu Sharma. 2021. "Scoping Review of Intervention Strategies for Improving Coverage and Uptake of Maternal Nutrition Services in Southeast Asia" International Journal of Environmental Research and Public Health 18, no. 24: 13292. https://doi.org/10.3390/ijerph182413292
APA StyleKurian, K., Lakiang, T., Sinha, R. K., Kathuria, N., Krishnan, P., Mehra, D., Mehra, S., & Sharma, S. (2021). Scoping Review of Intervention Strategies for Improving Coverage and Uptake of Maternal Nutrition Services in Southeast Asia. International Journal of Environmental Research and Public Health, 18(24), 13292. https://doi.org/10.3390/ijerph182413292






