General and COVID-19-Related Mortality by Pre-Existing Chronic Conditions and Care Setting during 2020 in Emilia-Romagna Region, Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Mortality Data and Population Denominators
2.3. Classification of Chronic Conditions and Care Setting
2.3.1. Selection of Chronic Conditions
2.3.2. Care Setting
2.4. Statistical Analysis
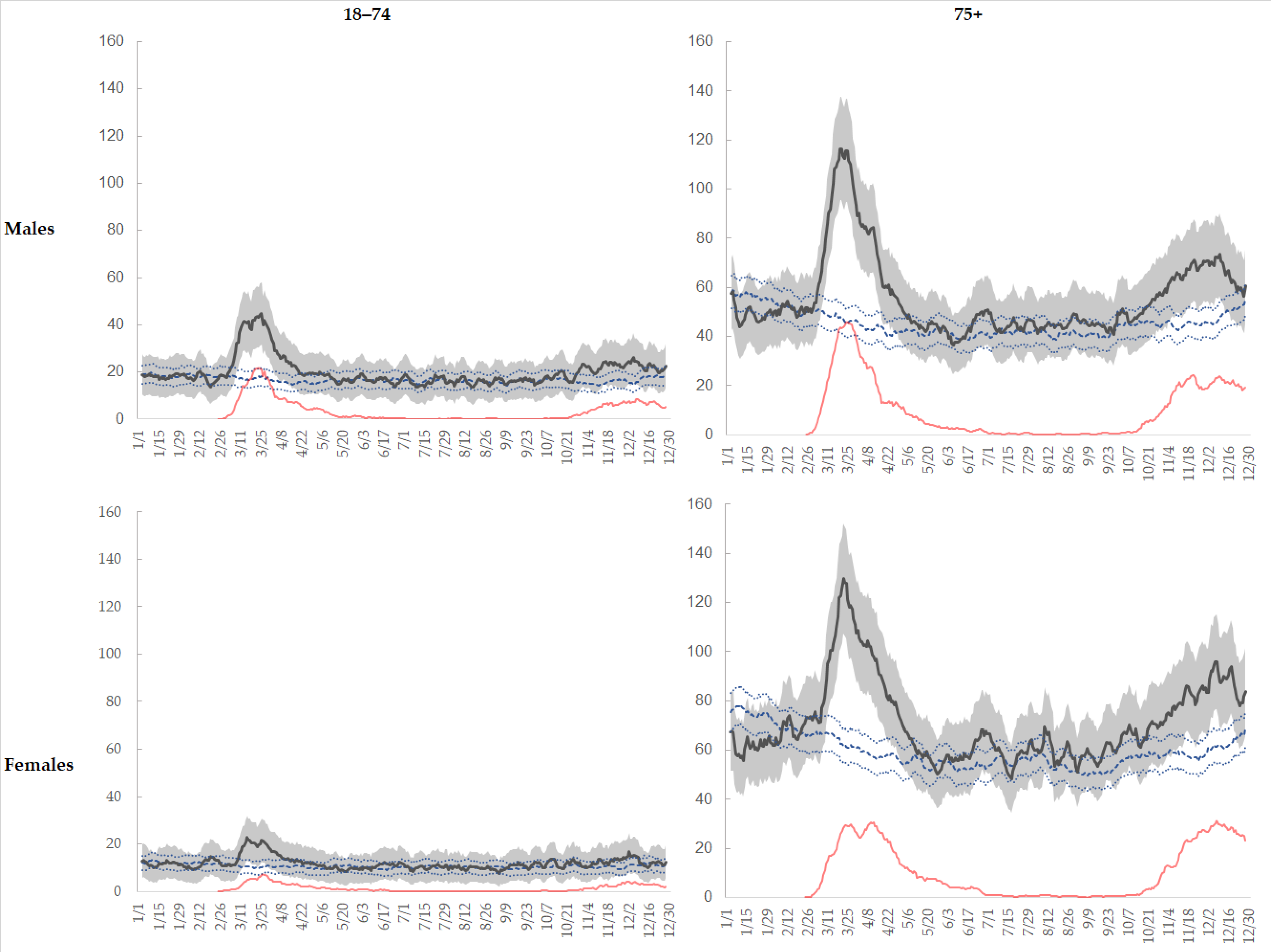
- absolute daily number of overall and COVID-19 deaths, comparing 2020 and 2015–2019 mean, by sex and age group;
- relative frequencies of 2020 deaths by sex, age group (18–74, 75+), period, pre-existent chronic conditions, and care setting;
- mortality excesses (observed minus expected) and number of COVID-19 deaths, by sex, age group and period;
- estimates of Mortality Rate Ratios (MRR: exp(β1)) and 95% confidence intervals, through Poisson models, comparing deaths (Y) counted in 2020 with those counted in 2015–2019 (X1 = dummy for period: [2016–2019 = 0, 2020 = 1]), adjusted for age (five- year classes: vector [X2]), by sex, age group, care setting (stratifying variables). Population at 1 January of each of the six years was included in models as offset (P):
i,jµl = exp (i,jβ1l * x1 + [i,jβ2l]*[x2])*Pi,j;i: sex, j: age class
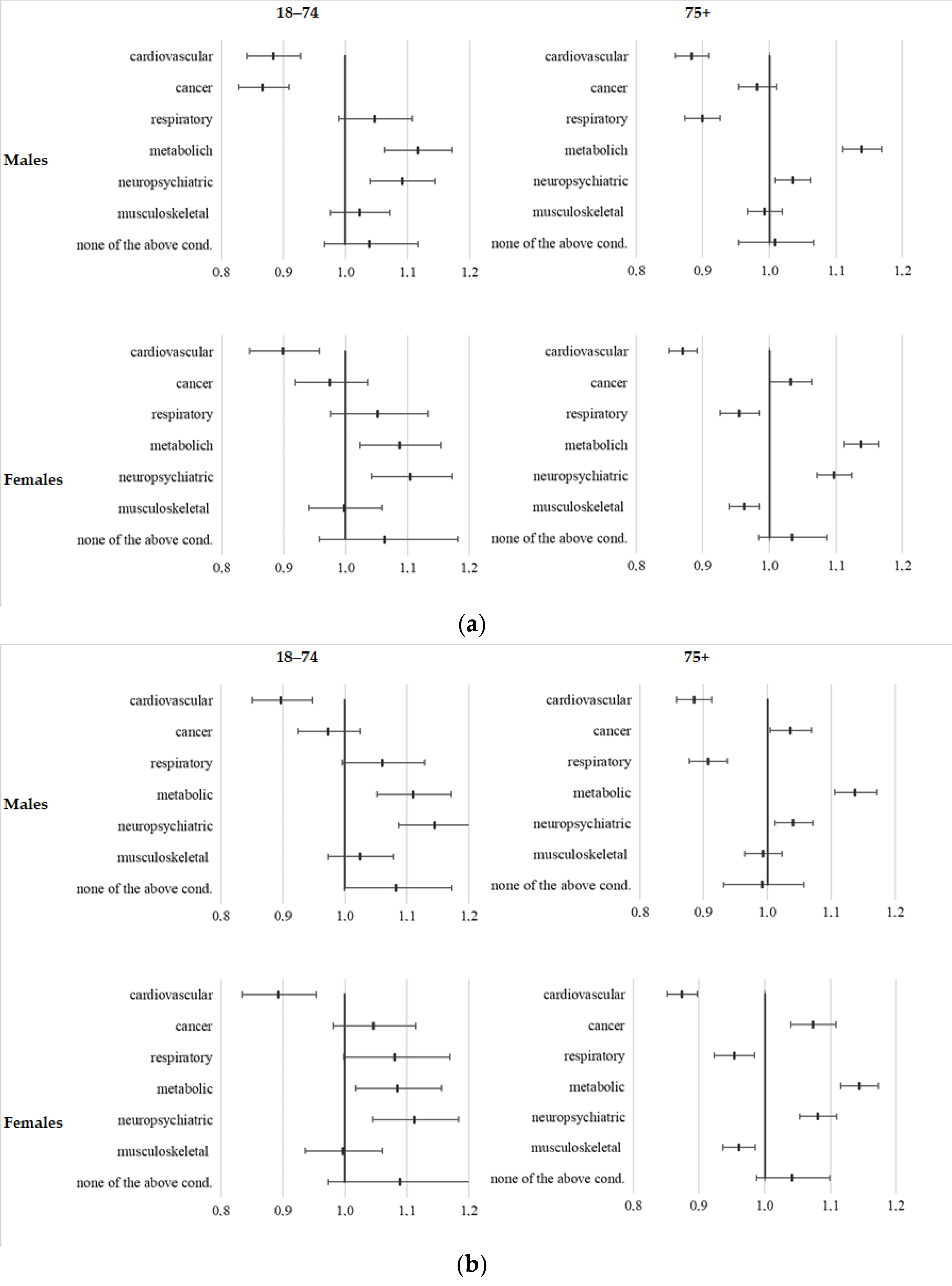
- estimates of Prevalence Ratios (PR: exp(βd)) and 95% confidence intervals, through log-binomial models and their coefficients in explaining probability (p) of dying in 2020 (Y: death in 2020) by means of dichotomous variables (Xd) indicating pre-existing chronic conditions (d), adjusted for age (five years class: vector [X8]), by sex, age group (stratifying variables):
3. Results
3.1. Deaths in Emilia-Romagna Region
3.2. Mortality Figures
3.3. Prevalence of Chronic Pre-Existent Conditions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Istat. Demographic Balance for the Year 2020; Istituto Italiano di Statistica. 2021. Available online: http://demo.istat.it/bilmens/index.php?anno=2020&lingua=eng (accessed on 5 June 2021).
- JHU. Mortality Analyses; John Hopkins University & Medicine. 2021. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 4 June 2021).
- Eurostat. Excess Mortality—Statistics. 2021. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Excess_mortality_-_statistics (accessed on 10 June 2021).
- ISS. Impatto dell’Epidemia COVID-19 Sulla Mortalità Totale della Popolazione Residente, anno. 2020. Available online: https://www.istat.it/it/files/2021/03/Report_ISS_Istat_2020_5_marzo.pdf (accessed on 4 June 2021).
- Fabiani, M.; Onder, G.; Boros, S.; Spuri, M.; Minelli, G.; Urdiales, A.M.; Andrianou, X.; Riccardo, F.; Del Manso, M.; Petrone, D.; et al. Case Fatality Rate of SARS-CoV-2 Infection at Regional Level and across Different Phases of the Epidemic in Italy. Version of 20 January 2021; Rapporto ISS COVID-19 2021; n. 1/2021. Available online: https://www.iss.it/rapporti-covid-19/-/asset_publisher/btw1J82wtYzH/content/rapporto-isscovid-19-il-case-fatality-rate-dell-infezione-sars-cov-2-a-livello-regionale-e-attraverso-le-differenti-fasi-dell-epidemia-in-italia.-versione-del-20-gennaio-2021 (accessed on 11 November 2021).
- Salmaso, S.; Zambri, F.; Renzi, M.; Giusti, A. Interrupting the chains of transmission of COVID-19 in Italy: Survey among the Prevention Departments. Epidemiol. Prev. 2020, 44 (Suppl. 2), 33–41. [Google Scholar]
- Pompili, E.C.D.; Cigliano, F.; Dalmasso, M.; Pasqualini, O.; Amprino, V.; Castella, A.; Gallone, A.; Greco, G.; Procopio, E.; Audisio, L.; et al. Organizzazione e Sviluppo di un Modello Drive-through per l’Esecuzione di Tamponi in Risposta alla Pandemia di COVID-19: l’Esperienza di una Azienda Sanitaria Locale nel Nord Italia. 2020. Available online: https://repo.epiprev.it/index.php/download/organizzazione-e-sviluppo-di-un-modello-drive-through-per-lesecuzione-di-tamponi-in-risposta-alla-pandemia-di-covid-19-lesperienza-di-una-azienda-sanitaria-locale-nel-nord-italia/ (accessed on 11 November 2021).
- Gude-Sampedro, F.; Fernández-Merino, C.; Ferreiro, L.; Lado-Baleato, Ó.; Espasandín-Domínguez, J.; Hervada, X.; Cadarso, C.M.; Valdés, L. Development and validation of a prognostic model based on comorbidities to predict COVID-19 severity: A population-based study. Int. J. Epidemiol. 2020, 50, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, L.; Vanacore, N.; Donfrancesco, C.; Noce, C.L.; Canevelli, M.; Punzo, O.; Raparelli, V.; Pezzotti, P.; Riccardo, F.; Bella, A.; et al. Clinical Characteristics of Hospitalized Individuals Dying With COVID-19 by Age Group in Italy. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 1796–1800. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.O.; Gale, C.P.; Kontopantelis, E.; Doran, T.; de Belder, M.; Asaria, M.; Luscher, T.; Wu, J.; Rashid, M.; Stephenson, C.; et al. Sex Differences in Mortality Rates and Underlying Conditions for COVID-19 Deaths in England and Wales. Mayo Clin. Proc. 2020, 95, 2110–2124. [Google Scholar] [CrossRef] [PubMed]
- Atkins, J.L.; Masoli, J.A.H.; Delgado, J.; Pilling, L.C.; Kuo, C.-L.; Kuchel, G.A.; Melzer, D. Preexisting Comorbidities Predicting COVID-19 and Mortality in the UK Biobank Community Cohort. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2020, 75, 2224–2230. [Google Scholar] [CrossRef] [PubMed]
- De Lusignan, S.; Joy, M.; Oke, J.; McGagh, D.; Nicholson, B.; Sheppard, J.; Akinyemi, O.; Amirthalingam, G.; Brown, K.; Byford, R. Disparities in the excess risk of mortality in the first wave of COVID-19: Cross sectional study of the English sentinel network. J. Infect. 2020, 81, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Noor, F.M.; Islam, M.M. Prevalence and Associated Risk Factors of Mortality Among COVID-19 Patients: A Meta-Analysis. J. Community Health 2020, 45, 1270–1282. [Google Scholar] [CrossRef]
- Palmieri, L.; Palmer, K.; Noce, C.L.; Meli, P.; Giuliano, M.; Floridia, M.; de Bella, M.T.; Piccioli, A.; Brusaferro, S.; Onder, G. Differences in the clinical characteristics of COVID-19 patients who died in hospital during different phases of the pandemic: National data from Italy. Aging Clin. Exp. Res. 2020, 33, 193–199. [Google Scholar] [CrossRef]
- Kaeuffer, C.; Le Hyaric, C.; Fabacher, T.; Mootien, J.; Dervieux, B.; Ruch, Y.; Hugerot, A.; Zhu, Y.-J.; Pointurier, V.; Clere-Jehl, R.; et al. Clinical characteristics and risk factors associated with severe COVID-19: Prospective analysis of 1,045 hospitalised cases in North-Eastern France, March 2020. Eurosurveillance 2020, 25, 2000895. [Google Scholar] [CrossRef] [PubMed]
- Di Girolamo, C.; Bartolini, L.; Caranci, N.; Moro, M.L. Socioeconomic inequalities in overall and COVID-19 mortality during the first outbreak peak in Emilia-Romagna Region (Northern Italy). Epidemiol. Prev. 2020, 44 (Suppl. 2), 288–296. [Google Scholar] [PubMed]
- Ballotari, P.; Guarda, L.; Giacomazzi, E.; Ceruti, A.; Gatti, L.; Ricci, P. Excess mortality risk in nursing care homes before and during the COVID-19 outbreak in Mantua and Cremona provinces (Lombardy Region, Northern Italy). Epidemiol. Prev. 2020, 44 (Suppl. 2), 282–287. [Google Scholar] [PubMed]
- Fortuna, D.; Berti, E.; Moro, M.L. Multimorbidity epidemiology and health care utilization through combined healthcare administrative databases. Epidemiol. Prev. 2021, 45, 62–71. [Google Scholar] [PubMed]
- Spadea, T.; Di Girolamo, C.; Landriscina, T.; Leoni, O.; Forni, S.; Colais, P.; Fanizza, C.; Allotta, A.; Onorati, R.; Gnavi, R.; et al. Indirect impact of Covid-19 on hospital care pathways in Italy. Sci. Rep. 2021, 11, 21526. [Google Scholar] [CrossRef] [PubMed]
- Istat-Iss. Impatto dell’Epidemia COVID-19 Sulla Mortalità Totale della Popolazione Residente. Anno 2020 e gennaio-aprile 2021. Istituto Nazione di Statistica. Available online: https://www.istat.it/it/files//2021/06/Report_ISS_Istat_2021_10_giugno.pdf (accessed on 11 November 2021).
- Richards, N.R.J. Can Dying at Home during COVID-19 still Be Indicator of ‘quality of death’? 2021. Available online: https://policyscotland.gla.ac.uk/can-dying-at-home-during-covid-19-still-be-an-indicator-of-quality-of-death/ (accessed on 11 November 2021).
- Raleigh, V. Invisible Deaths: Understanding Why Deaths at Home Increased during the Covid-19 Pandemic. 2021. Available online: https://www.kingsfund.org.uk/blog/2021/06/understanding-why-deaths-home-increased-covid-19-pandemic (accessed on 11 November 2021).
- Graham, N.; Junghans, C.; Downes, R.; Sendall, C.; Lai, H.; McKirdy, A.; Elliott, P.; Howard, R.; Wingfield, D.; Priestman, M.; et al. SARS-CoV-2 infection, clinical features and outcome of COVID-19 in United Kingdom nursing homes. J. Infect. 2020, 81, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Istat. Luogo del Decesso, Marzo-Aprile. 2020. Available online: https://www.istat.it/it/files//2021/04/CauseMortePrima_PandemiaCard4.pdf (accessed on 11 November 2021).
- Burki, T. England and Wales see 20,000 excess deaths in care homes. Lancet 2020, 395, 1602. [Google Scholar] [CrossRef]
- Nemani, K.; Li, C.; Olfson, M.; Blessing, E.M.; Razavian, N.; Chen, J.; Petkova, E.; Goff, D.C. Association of Psychiatric Disorders With Mortality Among Patients With COVID-19. JAMA Psychiatry 2021, 78, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, N. Epilepsy and COVID-19: Updated evidence and narrative review. Epilepsy. Behav. 2021, 116, 107785. [Google Scholar] [CrossRef] [PubMed]
- Mangone, L.; Gioia, F.; Mancuso, P.; Bisceglia, I.; Ottone, M.; Vicentini, M.; Pinto, C.; Giorgi Rossi, P. Cumulative COVID-19 incidence, mortality and prognosis in cancer survivors: A population-based study in Reggio Emilia, Northern Italy. Int. J. Cancer 2021, 149, 820–826. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Wang, L.; Ye, J.; Gu, Z.; Wang, S.; Xia, J.; Xie, Y.; Li, Q.; Xu, R.; Lin, N. Predictors of mortality in patients with coronavirus disease 2019: A systematic review and meta-analysis. BMC Infect. Dis. 2021, 21, 663. [Google Scholar] [CrossRef] [PubMed]
- Trifirò, G.; Massari, M.; Da Cas, R.; Ippolito, F.M.; Sultana, J.; Crisafulli, S.; Rossi, P.G.; Marino, M.; Zorzi, M.; Bovo, E.; et al. Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Death in Patients Hospitalised with COVID-19: A Retrospective Italian Cohort Study of 43,000 Patients. Drug Saf. 2020, 43, 1297–1308. [Google Scholar] [CrossRef] [PubMed]
| Males | Females | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs. Deaths (OBS) | OBS-Expected (ΔOE) | ΔOE/Expected % | COVID-19 Deaths (COV) | COV/ ΔOE % | Obs. Deaths (OBS) | OBS-Expected (ΔOE) | ΔOE/Expected % | COVID-19 Deaths (COV) | COV/ ΔOE % | |||
| Period age-group | January–February | 18–74 | 1078 | −16 | −1.5 | 0 | 0.0 | 698 | −18 | −2.5 | 0 | 0.0 |
| 75+ | 3021 | −197 | −6.1 | 2 | −1.0 | 3898 | −379 | −8.9 | 1 | −0.3 | ||
| Tot. | 4099 | −213 | −4.9 | 2 | −0.9 | 4596 | −398 | −8.0 | 1 | −0.3 | ||
| March–May | 18–74 | 2358 | 836 | 54.9 | 693 | 82.9 | 1256 | 291 | 30.2 | 245 | 84.2 | |
| 75+ | 6422 | 2337 | 57.2 | 1717 | 73.5 | 7753 | 2295 | 42.0 | 1572 | 68.5 | ||
| Tot. | 8780 | 3173 | 56.6 | 2410 | 75.9 | 9009 | 2586 | 40.3 | 1817 | 70.3 | ||
| June–September | 18–74 | 1983 | 1 | 0.1 | 35 | 3500 | 1264 | 30 | 2.4 | 16 | 54.1 | |
| 75+ | 5410 | 398 | 7.9 | 101 | 25.4 | 7209 | 657 | 10.0 | 165 | 25.1 | ||
| Tot. | 7393 | 399 | 5.7 | 136 | 34.1 | 8473 | 687 | 8.8 | 181 | 26.4 | ||
| October–December | 18–74 | 1923 | 398 | 26.1 | 388 | 97.5 | 1127 | 148 | 15.2 | 163 | 109.8 | |
| 75+ | 5578 | 1294 | 30.2 | 1330 | 102.8 | 7184 | 1701 | 31.0 | 1527 | 89.8 | ||
| Tot. | 7501 | 1692 | 29.1 | 1718 | 101.5 | 8311 | 1849 | 28.6 | 1690 | 91.4 | ||
| Age-class | 18–74 | 7342 | 1219 | 19.9 | 1116 | 91.6 | 4345 | 451 | 11.6 | 424 | 94.1 | |
| 75+ | 20,431 | 3833 | 23.1 | 3150 | 82.2 | 26,044 | 4273 | 19.6 | 3265 | 76.4 | ||
| Total | 27,773 | 5051 | 22.2 | 4266 | 84.5 | 30,389 | 4724 | 18.4 | 3689 | 78.1 | ||
| Care Setting | General Mortality | Not COVID-19 Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 18–74 | 75+ | 18–74 | 75+ | ||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| Male | Hospital (excluding long-term hospitalizations) | 1.25 | (1.21–1.30) | 1.20 | (1.17–1.22) | 0.98 | (0.95–1.00) | 0.89 | (0.87–0.91) |
| Community/Long-term Hospital | 0.65 | (0.56–0.75) | 0.73 | (0.69–0.78) | 0.61 | (0.53–0.71) | 0.61 | (0.53–0.71) | |
| Hospice | 0.91 | (0.84–1.00) | 0.95 | (0.89–1.02) | 0.90 | (0.82–0.98) | 0.90 | (0.82–0.98) | |
| Long-term Care Facilities | 1.28 | (1.06–1.55) | 1.28 | (1.20–1.36) | 1.03 | (0.84–1.27) | 1.07 | (1.00–1.15) | |
| Home Care | 2.21 | (1.11–4.37) | 1.36 | (1.00–1.86) | 2.02 | (1.00–4.09) | 1.10 | (0.79–1.54) | |
| None of the above | 1.15 | (1.10–1.20) | 1.21 | (1.18–1.25) | 1.13 | (1.09–1.18) | 1.18 | (1.15–1.21) | |
| Total | 1.15 | (1.12–1.18) | 1.15 | (1.13–1.17) | 0.98 | (0.95–1.00) | 0.97 | (0.96–0.99) | |
| Female | Hospital (excluding long-term hospitalizations) | 1.05 | (1.01–1.11) | 1.13 | (1.11–1.15) | 0.87 | (0.82–0.91) | 0.89 | (0.87–0.91) |
| Community / Long-term Hospital | 0.55 | (0.46–0.67) | 0.72 | (0.68–0.76) | 0.52 | (0.43–0.63) | 0.64 | (0.61–0.68) | |
| Hospice | 1.05 | (0.96–1.14) | 0.97 | (0.90–1.05) | 0.95 | (0.88–1.03) | 1.03 | (0.94–1.12) | |
| Long-term Care Facilities | 1.59 | (1.30–1.93) | 1.35 | (1.30–1.40) | 1.13 | (1.08–1.18) | 1.35 | (1.09–1.66) | |
| Home Care | 0.44 | (0.13–1.43) | 1.36 | (1.08–1.70) | 0.44 | (0.13–1.43) | 1.22 | (0.96–1.54) | |
| None of the above | 1.20 | (1.13–1.27) | 1.28 | (1.25–1.31) | 1.17 | (1.10–1.24) | 1.23 | (1.21–1.26) | |
| Total | 1.07 | (1.04–1.11) | 1.16 | (1.15–1.18) | 0.97 | (0.94–1.00) | 1.02 | (1.00–1.03) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caranci, N.; Di Girolamo, C.; Bartolini, L.; Fortuna, D.; Berti, E.; Sforza, S.; Giorgi Rossi, P.; Moro, M.L. General and COVID-19-Related Mortality by Pre-Existing Chronic Conditions and Care Setting during 2020 in Emilia-Romagna Region, Italy. Int. J. Environ. Res. Public Health 2021, 18, 13224. https://doi.org/10.3390/ijerph182413224
Caranci N, Di Girolamo C, Bartolini L, Fortuna D, Berti E, Sforza S, Giorgi Rossi P, Moro ML. General and COVID-19-Related Mortality by Pre-Existing Chronic Conditions and Care Setting during 2020 in Emilia-Romagna Region, Italy. International Journal of Environmental Research and Public Health. 2021; 18(24):13224. https://doi.org/10.3390/ijerph182413224
Chicago/Turabian StyleCaranci, Nicola, Chiara Di Girolamo, Letizia Bartolini, Daniela Fortuna, Elena Berti, Stefano Sforza, Paolo Giorgi Rossi, and Maria Luisa Moro. 2021. "General and COVID-19-Related Mortality by Pre-Existing Chronic Conditions and Care Setting during 2020 in Emilia-Romagna Region, Italy" International Journal of Environmental Research and Public Health 18, no. 24: 13224. https://doi.org/10.3390/ijerph182413224
APA StyleCaranci, N., Di Girolamo, C., Bartolini, L., Fortuna, D., Berti, E., Sforza, S., Giorgi Rossi, P., & Moro, M. L. (2021). General and COVID-19-Related Mortality by Pre-Existing Chronic Conditions and Care Setting during 2020 in Emilia-Romagna Region, Italy. International Journal of Environmental Research and Public Health, 18(24), 13224. https://doi.org/10.3390/ijerph182413224





