Accept Anxiety to Improve Sleep: The Impact of the COVID-19 Lockdown on the Relationships between Mindfulness, Distress, and Sleep Quality
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Materials
2.3. Data Analysis
3. Results
3.1. Effects of Lockdown
3.2. From Lockdown to Sleep Problems through Mindfulness and Distress
3.3. The Effects of Mindfulness Depend on Acceptance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Morin, C.M.; Bjorvatn, B.; Chung, F.; Holzinger, B.; Partinen, M.; Penzel, T.; Ivers, H.; Wing, Y.K.; Chan, N.Y.; Merikanto, I.; et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: An international collaborative study. Sleep Med. 2021, 87, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Salfi, F.; D’Atri, A.; Tempesta, D.; Ferrara, M. Sleeping under the waves: A longitudinal study across the contagion peaks of the COVID-19 pandemic in Italy. J. Sleep Res. 2021, 30, e13313. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Ozamiz-Etxebarria, N.; Idoiaga Mondragon, N.; Dosil Santamaría, M.; Picaza Gorrotxategi, M. Psychological Symptoms during the Two Stages of Lockdown in Response to the COVID-19 Outbreak: An Investigation in a Sample of Citizens in Northern Spain. Front. Psychol. 2020, 11, 1491. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion Books: New York, NY, USA, 1994. [Google Scholar]
- Howell, A.J.; Digdon, N.L.; Buro, K.; Sheptycki, A.R. Relations among mindfulness, well-being, and sleep. Personal. Individ. Differ. 2008, 45, 773–777. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef] [Green Version]
- Mayer, B.; Polak, M.G.; Remmerswaal, D. Mindfulness, Interpretation Bias, and Levels of Anxiety and Depression: Two Mediation Studies. Mindfulness 2019, 10, 55–65. [Google Scholar] [CrossRef] [Green Version]
- Ong, J.C.; Moore, C. What do we really know about mindfulness and sleep health? Curr. Opin. Psychol. 2020, 34, 18–22. [Google Scholar] [CrossRef]
- Zheng, M.X.; Masters-Waage, T.C.; Yao, J.; Lu, Y.; Tan, N.; Narayanan, J. Stay Mindful and Carry on: Mindfulness Neutralizes COVID-19 Stressors on Work Engagement via Sleep Duration. Front. Psychol. 2020, 11, 610156. [Google Scholar] [CrossRef]
- Simione, L.; Raffone, A.; Mirolli, M. Stress as the Missing Link between Mindfulness, Sleep Quality, and Well-being: A Cross-sectional Study. Mindfulness 2020, 11, 439–451. [Google Scholar] [CrossRef]
- Drake, C.L.; Pillai, V.; Roth, T. Stress and Sleep Reactivity: A Prospective Investigation of the Stress-Diathesis Model of Insomnia. Sleep 2014, 37, 1295–1304. [Google Scholar] [CrossRef] [Green Version]
- Ong, J.C.; Ulmer, C.S.; Manber, R. Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia. Behav. Res. Ther. 2012, 50, 651–660. [Google Scholar] [CrossRef] [Green Version]
- Sauer, S.; Walach, H.; Schmidt, S.; Hinterberger, T.; Lynch, S.; Büssing, A.; Kohls, N. Assessment of Mindfulness: Review on State of the Art. Mindfulness 2013, 4, 3–17. [Google Scholar] [CrossRef]
- Carpenter, J.K.; Conroy, K.; Gomez, A.F.; Curren, L.C.; Hofmann, S.G. The relationship between trait mindfulness and affective symptoms: A meta-analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clin. Psychol. Rev. 2019, 74, 101785. [Google Scholar] [CrossRef]
- Lindsay, E.K.; Creswell, J.D. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clin. Psychol. Rev. 2017, 51, 48–59. [Google Scholar] [CrossRef] [Green Version]
- Simione, L.; Raffone, A.; Mirolli, M. Acceptance, and Not Its Interaction with Attention Monitoring, Increases Psychological Well-Being: Testing the Monitor and Acceptance Theory of Mindfulness. Mindfulness 2021, 12, 1398–1411. [Google Scholar] [CrossRef]
- Giovannini, C.; Giromini, L.; Bonalume, L.; Tagini, A.; Lang, M.; Amadei, G. The Italian Five Facet Mindfulness Questionnaire: A Contribution to its Validity and Reliability. J. Psychopathol. Behav. Assess 2014, 36, 415–423. [Google Scholar] [CrossRef]
- Iani, L.; Lauriola, M.; Costantini, M. A confirmatory bifactor analysis of the hospital anxiety and depression scale in an Italian community sample. Health Qual. Life Outcomes 2014, 12, 84. [Google Scholar] [CrossRef] [PubMed]
- Natale, V.; Fabbri, M.; Tonetti, L.; Martoni, M. Psychometric goodness of the Mini Sleep Questionnaire. Psychiatry Clin. Neurosci. 2014, 68, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, M.; Beracci, A.; Martoni, M.; Meneo, D.; Tonetti, L.; Natale, V. Measuring Subjective Sleep Quality: A Review. Int. J. Environ. Res. Public Health 2021, 18, 1082. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Fabbri, M.; Natale, V.; Prat, G. Sleep Beliefs Scale (SBS) and circadian typology. J. Sleep Res. 2006, 15, 125–132. [Google Scholar] [CrossRef]
- Natale, V.; Esposito, M.J.; Martoni, M.; Fabbri, M. Validity of the reduced version of the Morningness-Eveningness Questionnaire. Sleep Biol. Rhythm. 2006, 4, 72–74. [Google Scholar] [CrossRef]
- Tehseen, S.; Ramayah, T.; Sajilan, S. Testing and Controlling for Common Method Variance: A Review of Available Methods. J. Manag. Sci. 2017, 4, 146–175. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [Green Version]
- Lai, K. Estimating Standardized SEM Parameters Given Nonnormal Data and Incorrect Model: Methods and Comparison. Struct. Equ. Model. 2018, 25, 600–620. [Google Scholar] [CrossRef]
- Hu, L.-T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Tomlinson, E.R.; Yousaf, O.; Vittersø, A.D.; Jones, L. Dispositional Mindfulness and Psychological Health: A Systematic Review. Mindfulness 2018, 9, 23–43. [Google Scholar] [CrossRef] [Green Version]
- Sedlmeier, P.; Loße, C.; Quasten, L.C. Psychological Effects of Meditation for Healthy Practitioners: An Update. Mindfulness 2018, 9, 371–387. [Google Scholar] [CrossRef]
- Linton, S.J.; Kecklund, G.; Franklin, K.A.; Leissner, L.C.; Sivertsen, B.; Lindberg, E.; Svensson, A.C.; Hansson, S.O.; Sundin, Ö.; Hetta, J.; et al. The effect of the work environment on future sleep disturbances: A systematic review. Sleep Med. Rev. 2015, 23, 10–19. [Google Scholar] [CrossRef]
- Lau, W.K.W.; Leung, M.-K.; Wing, Y.-K.; Lee, T.M.C. Potential Mechanisms of Mindfulness in Improving Sleep and Distress. Mindfulness 2018, 9, 547–555. [Google Scholar] [CrossRef] [Green Version]
- Cash, M.; Whittingham, K. What Facets of Mindfulness Contribute to Psychological Well-being and Depressive, Anxious, and Stress-related Symptomatology? Mindfulness 2010, 1, 177–182. [Google Scholar] [CrossRef]
- Shallcross, A.J. Waking up to the problem of sleep: Can mindfulness help? A review of theory and evidence for the effects of mindfulness for sleep. Curr. Opin. Psychol. 2019, 13, 37–41. [Google Scholar] [CrossRef]
- Paul, N.A.; Stanton, S.J.; Greeson, J.M.; Smoski, M.J.; Wang, L. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Soc. Cogn. Affect. Neurosci. 2013, 8, 56–64. [Google Scholar] [CrossRef] [Green Version]
- Chen, F.; Bollen, K.A.; Paxton, P.; Curran, P.J.; Kirby, J.B. Improper Solutions in Structural Equation Models: Causes, Consequences, and Strategies. Sociol. Methods Res. 2001, 29, 468–508. [Google Scholar] [CrossRef]
- Pan, H.; Liu, S.; Miao, D.; Yuan, Y. Sample Size Determination for Mediation Analysis of Longitudinal Data. BMC Med. Res. Methodol. 2018, 18, 32. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Cardaciotto, L.; Herbert, J.D.; Forman, E.M.; Moitra, E.; Farrow, V. The Assessment of Present-Moment Awareness and Acceptance: The Philadelphia Mindfulness Scale. Assessment 2008, 15, 204–223. [Google Scholar] [CrossRef] [Green Version]
- Hadash, Y.; Bernstein, A. Behavioral assessment of mindfulness: Defining features, organizing framework, and review of emerging methods. Curr. Opin. Psychol. 2019, 28, 229–237. [Google Scholar] [CrossRef] [Green Version]
| Time 0 | Time 1 | |||||||
|---|---|---|---|---|---|---|---|---|
| Scale | Variable | Cronbach’s α | M | SD | M | SD | F(1,37) | η2p |
| FFMQ | Observing | 0.79 | 27.36 | 6.7 | 29.74 | 4.56 | 6.51 * | 0.15 |
| Non-judging | 0.80 | 27.18 | 5.4 | 22.49 | 5.57 | 16.56 ** | 0.31 | |
| Non-reacting | 0.71 | 21.49 | 4.4 | 22.36 | 3.54 | 1.57 | 0.04 | |
| FFMQ tot | 0.86 | 131.03 | 16.72 | 123.13 | 11.38 | 6.96 * | 0.16 | |
| HADS | Anxiety | 0.76 | 9.31 | 2.91 | 9.77 | 3.19 | 0.90 | 0.02 |
| Depression | 0.82 | 8.13 | 1.96 | 9.13 | 2.41 | 7.26 * | 0.16 | |
| HADS tot | 0.86 | 17.44 | 4.12 | 18.90 | 4.68 | 4.43 * | 0.11 | |
| MSQ | Sleep | 0.75 | 14.26 | 6.05 | 15.74 | 6.04 | 4.58 * | 0.11 |
| Wake | 0.84 | 13.10 | 5.16 | 13.28 | 5.52 | 0.05 | 0.01 | |
| MSQ tot | 0.85 | 27.36 | 10.18 | 29.03 | 10.71 | 1.72 | 0.04 | |
| rMEQ | rMEQ tot | 0.51 | 14.74 | 3.53 | 14.13 | 3.81 | 1.21 | 0.03 |
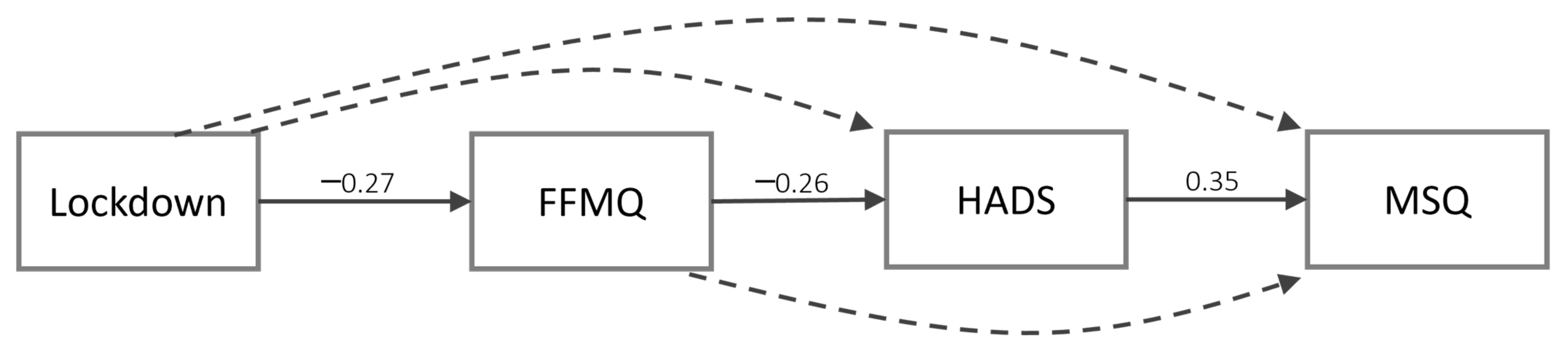
| Path | b | CIlower | CIupper | SE | β | ||
|---|---|---|---|---|---|---|---|
| Lockdown | → | FFMQ | −7.88 * | −14.95 | −1.42 | 3.45 | −0.27 |
| Lockdown | → | HADS | 0.85 | −1.01 | 2.82 | 0.97 | 0.10 |
| Lockdown | → | MSQ | 0.13 | −3.99 | 4.53 | 2.20 | 0.01 |
| FFMQ | → | HADS | −0.08 * | −0.15 | −0.01 | 0.04 | −0.26 |
| HADS | → | MSQ | 0.82 * | 0.16 | 1.32 | 0.29 | 0.35 |
| FFMQ | → | MSQ | −0.04 | −0.18 | 0.17 | 0.08 | −0.05 |
| Path | b | CIlower | CIupper | SE | β | ||
|---|---|---|---|---|---|---|---|
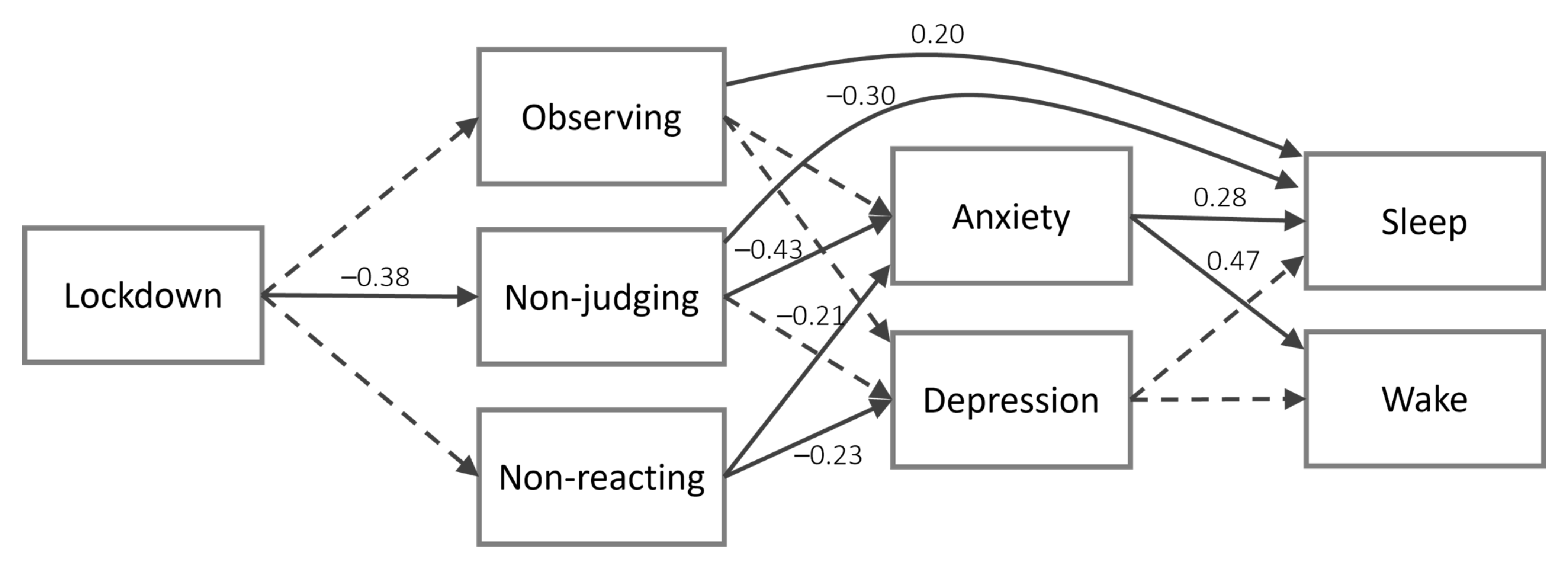
| Lockdown | → | Sleep | −0.74 | −3.44 | 2.06 | 1.43 | −0.06 |
| Lockdown | → | Wake | −1.03 | −3.19 | 0.95 | 1.03 | −0.10 |
| Lockdown | → | Anxiety | −0.42 | −1.65 | 0.81 | 0.61 | −0.07 |
| Lockdown | → | Depression | 0.76 | −0.22 | 1.66 | 0.49 | 0.17 |
| Lockdown | → | Observing | 2.19 | −0.42 | 4.65 | 1.26 | 0.19 |
| Lockdown | → | Non-judging | −4.69 ** | −7.06 | −2.23 | 1.24 | −0.38 |
| Lockdown | → | Non-reacting | 0.76 | −1.30 | 2.61 | 0.99 | 0.09 |
| Observing | → | Anxiety | 0.01 | −0.11 | 0.12 | 0.06 | 0.03 |
| Non-judging | → | Anxiety | −0.21 ** | −0.33 | −0.10 | 0.06 | −0.43 |
| Non-reacting | → | Anxiety | −0.15 * | −0.28 | −0.01 | 0.07 | −0.21 |
| Observing | → | Depression | −0.01 | −0.13 | 0.08 | 0.05 | −0.04 |
| Non-judging | → | Depression | −0.07 | −0.16 | 0.03 | 0.05 | −0.19 |
| Non-reacting | → | Depression | −0.12 * | −0.26 | −0.01 | 0.07 | −0.23 |
| Observing | → | Sleep | 0.21 * | 0.04 | 0.47 | 0.11 | 0.20 |
| Non-judging | → | Sleep | −0.29 * | −0.61 | −0.02 | 0.14 | −0.30 |
| Non-reacting | → | Sleep | 0.19 | −0.15 | 0.61 | 0.19 | 0.14 |
| Observing | → | Wake | 0.12 | −0.05 | 0.33 | 0.09 | 0.13 |
| Non-judging | → | Wake | −0.11 | −0.35 | 0.10 | 0.11 | −0.12 |
| Non-reacting | → | Wake | 0.04 | −0.32 | 0.39 | 0.18 | 0.04 |
| Anxiety | → | Sleep | 0.55 * | 0.08 | 1.13 | 0.27 | 0.28 |
| Depression | → | Sleep | −0.03 | −0.74 | 0.60 | 0.35 | −0.01 |
| Anxiety | → | Wake | 0.81 * | 0.40 | 1.16 | 0.20 | 0.47 |
| Depression | → | Wake | −0.05 | −0.57 | 0.47 | 0.26 | −0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirolli, M.; Simione, L.; Martoni, M.; Fabbri, M. Accept Anxiety to Improve Sleep: The Impact of the COVID-19 Lockdown on the Relationships between Mindfulness, Distress, and Sleep Quality. Int. J. Environ. Res. Public Health 2021, 18, 13149. https://doi.org/10.3390/ijerph182413149
Mirolli M, Simione L, Martoni M, Fabbri M. Accept Anxiety to Improve Sleep: The Impact of the COVID-19 Lockdown on the Relationships between Mindfulness, Distress, and Sleep Quality. International Journal of Environmental Research and Public Health. 2021; 18(24):13149. https://doi.org/10.3390/ijerph182413149
Chicago/Turabian StyleMirolli, Marco, Luca Simione, Monica Martoni, and Marco Fabbri. 2021. "Accept Anxiety to Improve Sleep: The Impact of the COVID-19 Lockdown on the Relationships between Mindfulness, Distress, and Sleep Quality" International Journal of Environmental Research and Public Health 18, no. 24: 13149. https://doi.org/10.3390/ijerph182413149
APA StyleMirolli, M., Simione, L., Martoni, M., & Fabbri, M. (2021). Accept Anxiety to Improve Sleep: The Impact of the COVID-19 Lockdown on the Relationships between Mindfulness, Distress, and Sleep Quality. International Journal of Environmental Research and Public Health, 18(24), 13149. https://doi.org/10.3390/ijerph182413149







