Health Literacy, Health Behaviors, and Body Mass Index Impacts on Quality of Life: Cross-Sectional Study of University Students in Surabaya, Indonesia
Abstract
1. Introduction
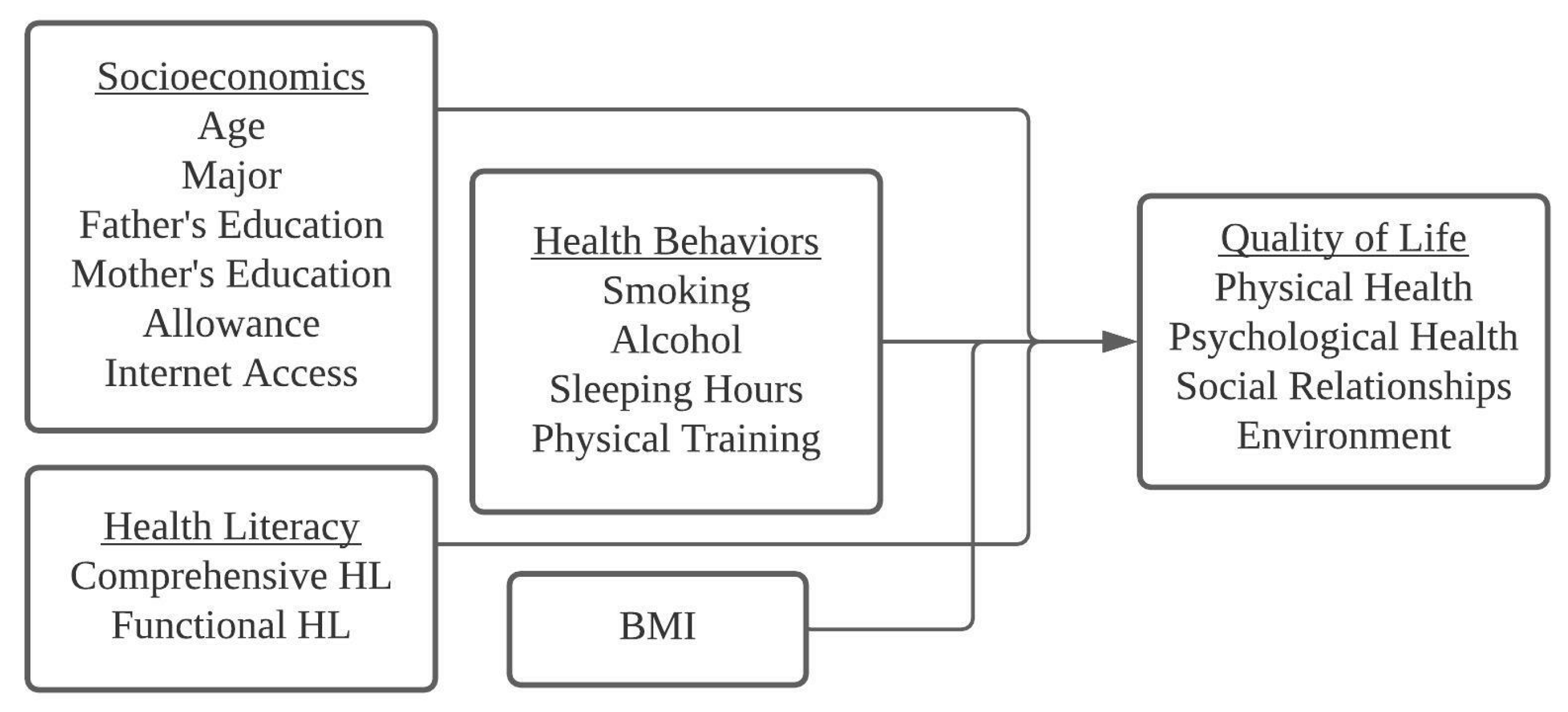
2. Materials and Methods
2.1. Description of Study Design, Population, and Sample
2.2. Measures
2.2.1. Quality of Life
2.2.2. Comprehensive Health Literacy (CHL)
2.2.3. Functional Health Literacy (FHL)
2.2.4. Health Behaviors
2.2.5. Body Mass Index (BMI)
2.2.6. Socioeconomic Determinants
2.3. Statistical Analysis
3. Results
3.1. Respondent Characteristics
3.2. QOL Association with Socioeconomic Determinants, CHL, FHL, HBs, and BMI
3.3. Multivariate Generalized Linear Models of the Four Domains of QOL with Socioeconomic Determinants, HBs, BMI, and CHL
3.4. Multivariate Generalized Linear Models of the Four Domains of QOL with Socioeconomic Determinants, HBs, BMI, and FHL
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Powers, C.B.; Wisocki, P.A.; Whitbourne, S.K. Age Differences and Correlates of Worrying in Young and Elderly Adults. Gerontologist 1992, 32, 82–88. [Google Scholar] [CrossRef]
- Zhang, L. Thinking of the Academic Burden on Students and Education Reform Mode of Occupation Education; Atlantis Press: Beijing, China, 2016; pp. 605–609. [Google Scholar] [CrossRef][Green Version]
- Christie, H.; Tett, L.; Cree, V.E.; Hounsell, J.; McCune, V. “A real rollercoaster of confidence and emotions”: Learning to be a university student. Stud. High. Educ. 2008, 33, 567–581. [Google Scholar] [CrossRef]
- Bernier, A.; Larose, S.; Whipple, N. Leaving home for college: A potentially stressful event for adolescents with preoccupied attachment patterns. Attach. Hum. Dev. 2005, 7, 171–185. [Google Scholar] [CrossRef]
- Tett, L.; Cree, V.E.; Christie, H. From further to higher education: Transition as an on-going process. High. Educ. 2017, 73, 389–406. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Hetrick, S.E.; Parker, A.G. The impact of stress on students in secondary school and higher education. Int. J. Adolesc. Youth 2020, 25, 104–112. [Google Scholar] [CrossRef]
- Taylor, D.J.; Bramoweth, A.D.; Grieser, E.A.; Tatum, J.I.; Roane, B.M. Epidemiology of Insomnia in College Students: Relationship With Mental Health, Quality of Life, and Substance Use Difficulties. Behav. Ther. 2013, 44, 339–348. [Google Scholar] [CrossRef]
- Weidner, G.; Kohlmann, C.W.; Dotzauer, E.; Burns, L.R. The effects of academic stress on health behaviors in young adults. Anxiety Stress Coping 1996, 9, 123–133. [Google Scholar] [CrossRef]
- Brandão, M.P.; Pimentel, F.L.; Cardoso, M.F. Impact of academic exposure on health status of university students. Rev. Saude Publica 2011, 45, 49–58. [Google Scholar] [CrossRef]
- Ribeiro, Í.J.S.; Pereira, R.; Freire, I.V.; de Oliveira, B.G.; Casotti, C.A.; Boery, E.N. Stress and Quality of Life Among University Students: A Systematic Literature Review. Health Prof. Educ. 2018, 4, 70–77. [Google Scholar] [CrossRef]
- Lageborn, C.T.; Ljung, R.; Vaez, M.; Dahlin, M. Ongoing university studies and the risk of suicide: A register-based nationwide cohort study of 5 million young and middle-aged individuals in Sweden, 1993–2011. BMJ Open 2017, 7, 14264. [Google Scholar] [CrossRef]
- WHO WHOQOL—Measuring Quality of Life|The World Health Organization. Available online: https://www.who.int/tools/whoqol (accessed on 16 September 2021).
- The WHOQOL Group Whoqol-Bref: Introduction, Administration, Scoring and Generic Version of the Assessment. Program. Ment. Health 1996, 16, 10–13.
- Memon, A.B.; Rahman, A.A.U.; Channar, K.A.; Zafar, M.S.; Kumar, N. Assessing the Quality of Life of Oral Submucous Fibrosis Patients: A Cross-Sectional Study Using the WHOQOL-BREF Tool. Int. J. Environ. Res. Public Health 2021, 18, 9498. [Google Scholar] [CrossRef]
- Wang, K.-T.; Fu, S.-H.; Hsieh, P.-L.; Lin, Y.-L.; Yang, S.-Y. Investigating the Relationship between Media Usage, Depression, and Quality of Life among Older Adults. Healthcare 2021, 9, 1154. [Google Scholar] [CrossRef]
- Hargreaves, S.M.; Nakano, E.Y.; Han, H.; Raposo, A.; Ariza-Montes, A.; Vega-Muñoz, A.; Zandonadi, R.P. Quality of life of brazilian vegetarians measured by the whoqol-bref: Influence of type of diet, motivation and sociodemographic data. Nutrients 2021, 13, 2648. [Google Scholar] [CrossRef]
- Kotarska, K.; Nowak, M.A.; Nowak, L.; Król, P.; Sochacki, A.; Sygit, K.; Sygit, M. Physical activity and quality of life of university students, their parents and grandparents in poland—selected determinants. Int. J. Environ. Res. Public Health 2021, 18, 3871. [Google Scholar] [CrossRef]
- Harsch, S.; Jawid, A.; Jawid, M.E.; Nunes, L.S.; Sahrai, D.; Bittlingmayer, U.H. The relationship of health literacy, wellbeing and religious beliefs in neglected and unequal contexts—Results of a survey study in central Afghanistan. Health Promot. J. Aust. 2021, 32, 80–87. [Google Scholar] [CrossRef]
- Sirisuwan, P.; Phimha, S.; Banchonhattakit, P. Active Aging, Health Literacy, and Quality of Life among Elderly in the Northeast of Thailand. Indian J. Forensic Med. Toxicol. 2021, 15, 2645–2650. [Google Scholar] [CrossRef]
- Zarcadoolas, C.; Pleasant, A.; Greer, D.S. Understanding health literacy: An expanded model. Health Promot. Int. 2005, 20, 195–203. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Nutbeam, D. Health promotion glossary. Health Promot. 1986, 1, 113–127. [Google Scholar] [CrossRef]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Short, S.E.; Mollborn, S. Social determinants and health behaviors: Conceptual frames and empirical advances. Curr. Opin. Psychol. 2015, 5, 78–84. [Google Scholar] [CrossRef]
- Toghianifar, N.; Najafian, J.; Pooya, A.; Rabiei, K.; Eshrati, B.; Anaraki, J.; Sarrafzadegan, N. Association of smoking status with quality of life in a cross-sectional population-based sample of iranian adults: Isfahan healthy heart program. Asia-Pac. J. Public Health 2012, 24, 786–794. [Google Scholar] [CrossRef]
- de Campos Moreira, T.; Figueiró, L.R.; Fernandes, S.; Ferigolo, M.; Barros, H.M.T.; Dias, I.R.; Justo, F.M. Quality of life of users of psychoactive substances, relatives, and non-users assessed using the WHOQOL-BREF. Ciênc. Saúde Coletiva 2013, 18, 1953–1962. [Google Scholar]
- Strandberg, A.Y.; Strandberg, T.E.; Pitkälä, K.; Salomaa, V.V.; Tilvis, R.S.; Miettinen, T.A. The effect of smoking in midlife on health-related quality of life in old age: A 26-year prospective study. Arch. Intern. Med. 2008, 168, 1968–1974. [Google Scholar] [CrossRef]
- Zillich, A.J.; Ryan, M.; Adams, A.; Yeager, B.; Farris, K. Effectiveness of a pharmacist-based smoking-cessation program and its impact on quality of life. Pharmacotherapy 2002, 22, 759–765. [Google Scholar] [CrossRef]
- Torres, G.C.S.; Paragas, E.D. Social determinants associated with the quality of life of baccalaureate nursing students: A cross-sectional study. Nurs. Forum. 2019, 54, 137–143. [Google Scholar] [CrossRef]
- Zhang, Y.; Qu, B.; Lun, S.; Wang, D.; Guo, Y.; Liu, J. Quality of Life of Medical Students in China: A Study Using the WHOQOL-BREF. PLoS ONE 2012, 7, e49714. [Google Scholar] [CrossRef]
- Çiçek, G. Quality of Life and Physical Activity among University Students. Univers. J. Educ. Res. 2018, 6, 1141–1148. [Google Scholar] [CrossRef]
- Stenholm, S.; Head, J.; Aalto, V.; Kivimäki, M.; Kawachi, I.; Zins, M.; Goldberg, M.; Platts, L.G.; Zaninotto, P.; Magnusson Hanson, L.L.; et al. Body mass index as a predictor of healthy and disease-free life expectancy between ages 50 and 75: A multicohort study. Int. J. Obes. 2017, 41, 769. [Google Scholar] [CrossRef]
- Aune, D.; Sen, A.; Prasad, M.; Norat, T.; Janszky, I.; Tonstad, S.; Romundstad, P.; Vatten, L.J. BMI and all cause mortality: Systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ 2016, 353. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Hung, C.-K.; Chang, Y.-Y.; Tai, C.-M.; Lin, J.-T.; Wang, J.-D. Health-related Quality of Life in Adult Patients with Morbid Obesity Coming for Bariatric Surgery. Obes. Surg. 2008, 20, 1121–1127. [Google Scholar] [CrossRef]
- Serinolli, M.I.; Novaretti, M.C.Z. A cross-sectional study of sociodemographic factors and their influence on quality of life in medical students at Sao Paulo, Brazil. PLoS ONE 2017, 12, 1–13. [Google Scholar] [CrossRef]
- Taylor, V.H.; Forhan, M.; Vigod, S.N.; McIntyre, R.S.; Morrison, K.M. The impact of obesity on quality of life. Best Pract. Res. Clin. Endocrinol. Metab. 2013, 27, 139–146. [Google Scholar] [CrossRef]
- Toçi, E.; Burazeri, G.; Kamberi, H.; Toçi, D.; Roshi, E.; Jerliu, N.; Bregu, A.; Brand, H. Health literacy and body mass index: A population-based study in a South-Eastern European country. J. Public Health 2021, 43, 123–130. [Google Scholar] [CrossRef]
- Adewole, K.O.; Ogunfowokan, A.A.; Olodu, M. Influence of health literacy on health promoting behaviour of adolescents with and without obesity. Int. J. Afr. Nurs. Sci. 2021, 15, 100342. [Google Scholar] [CrossRef]
- Cruz, L.N.; Polanczyk, C.A.; Camey, S.A.; Hoffmann, J.F.; Fleck, M.P. Quality of life in Brazil: Normative values for the Whoqol-bref in a southern general population sample. Qual. Life Res. 2011, 20, 1123–1129. [Google Scholar] [CrossRef]
- Lodhi, F.S.; Montazeri, A.; Nedjat, S.; Mahmoodi, M.; Farooq, U.; Yaseri, M.; Kasaeian, A.; Holakouie-Naieni, K. Assessing the quality of life among Pakistani general population and their associated factors by using the World Health Organization’s quality of life instrument (WHOQOL-BREF): A population based cross-sectional study. Health Qual. Life Outcomes 2019, 17. [Google Scholar] [CrossRef]
- Baumann, M.; Chau, K.; Kabuth, B.; Chau, N. Association between health-related quality of life and being an immigrant among adolescents, and the role of socioeconomic and health-related difficulties. Int. J. Environ. Res. Public Health 2014, 11, 1694–1714. [Google Scholar] [CrossRef]
- Chattu, V.K.; Sahu, P.K.; Seedial, N.; Seecharan, G.; Seepersad, A.; Seunarine, M.; Sieunarine, S.; Seymour, K.; Simboo, S.; Singh, A. An Exploratory Study of Quality of Life and Its Relationship with Academic Performance among Students in Medical and other Health Professions. Med. Sci. 2020, 8, 23. [Google Scholar] [CrossRef]
- Dučinskienė, D.; Kalėdienė, R.; Petrauskienė, J. Quality of life among Lithuanian university students. Acta Med. Lituan. 2003, 10, 76–81. [Google Scholar]
- Ameer, M.H.; Khalid, N.; Asghar, S. Quality of life and its determinants in students of medical and non-medical education. Int. J. Community Med. Public Health 2020, 7, 1664. [Google Scholar] [CrossRef]
- Surabaya, U.N. Overview of Surabaya State University. Available online: https://en.unesa.ac.id/page/tentang-unesa/selayang-pandang (accessed on 16 September 2021).
- PD Dikti Indonesia Surabaya State University Information Page. Available online: https://pddikti.kemdikbud.go.id/data_pt/Q0IxMTU0QjQtMTBCQS00NzEyLUI5MTYtMzYwNTFCQTdDMzJG (accessed on 16 September 2021).
- The WHOQOL Group WHO Quality of Life Scale (WHOQOL). Psychol. Med. 1998, 28, 551–558.
- Pelikan, J.M.; Röthlin, F.; Ganahl, K. Measuring Comprehensive Health Literacy in General Populations: Validation of Instrument, Indices and Scales of the HLS-EU Study; Ludwig Boltzmann Institute Health Promotion Research: Vienna, Austria, 2014. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Nolasco, A.; Barona, C.; Tamayo-Fonseca, N.; Irles, M.Á.; Más, R.; Tuells, J.; Pereyra-Zamora, P. Health literacy: Psychometric behaviour of the HLS-EU-Q16 questionnaire. Gac. Sanit. 2020, 34, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Dsouza, J.P.; Van Den Broucke, S.; Pattanshetty, S. Validity and reliability of the Indian version of the HLS-EU-Q16 questionnaire. Int. J. Environ. Res. Public Health 2021, 18, 495. [Google Scholar] [CrossRef]
- Rouquette, A.; Nadot, T.; Labitrie, P.; Van den Broucke, S.; Mancini, J.; Rigal, L.; Ringa, V. Validity and measurement invariance across sex, age, and education level of the French short versions of the European Health Literacy Survey Questionnaire. PLoS ONE 2018, 13, e0208091. [Google Scholar] [CrossRef]
- Gustafsdottir, S.S.; Sigurdardottir, A.K.; Arnadottir, S.A.; Heimisson, G.T.; Mårtensson, L. Translation and cross-cultural adaptation of the European Health Literacy Survey Questionnaire, HLS-EU-Q16: The Icelandic version. BMC Public Health 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick assessment of literacy in primary care: The newest vital sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.P.; Leenaars, K.E.F.; Rowlands, G.; Weiss, B.D.; Maat, H.P.; Essink-Bot, M.L. International application of health literacy measures: Adaptation and validation of the newest vital sign in The Netherlands. Patient Educ. Couns. 2014, 97, 403–409. [Google Scholar] [CrossRef]
- Kogure, T.; Sumitani, M.; Suka, M.; Ishikawa, H.; Odajima, T.; Igarashi, A.; Kusama, M.; Okamoto, M.; Sugimori, H.; Kawahara, K. Validity and reliability of the Japanese version of the newest vital sign: A preliminary study. PLoS ONE 2014, 9, e94582. [Google Scholar] [CrossRef]
- Zotti, P.; Cocchi, S.; Polesel, J.; Cipolat Mis, C.; Bragatto, D.; Cavuto, S.; Conficconi, A.; Costanzo, C.; De Giorgi, M.; Drace, C.A.; et al. Cross-cultural validation of health literacy measurement tools in Italian oncology patients. BMC Health Serv. Res. 2017, 17, 1–7. [Google Scholar] [CrossRef]
- Tseng, H.M.; Liao, S.F.; Wen, Y.P.; Chuang, Y.J. Adaptation and validation of a measure of health literacy in Taiwan: The Newest Vital Sign. Biomed. J. 2018, 41, 273–278. [Google Scholar] [CrossRef]
- Institute of Epidemiology & Health Care. Available online: https://www.ucl.ac.uk/epidemiology-health-care/research/behavioural-science-and-health/research/psychobiology/international-health-and-behaviour (accessed on 21 September 2021).
- Wardle, J.; Steptoe, A. The European health and behaviour survey: Rationale, methods and initial results from the United Kingdom. Soc. Sci. Med. 1991, 33, 925–936. [Google Scholar] [CrossRef]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J. Clin. Sleep Med. 2015, 11, 591–592. [Google Scholar] [CrossRef]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef] [PubMed]
- WHO BMI-for-Age (5–19 Years). Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 16 April 2021).
- Europe, W. WHO/Europe|Nutrition—Body Mass Index—BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 24 September 2021).
- Prihanto, J.B.; Nurhayati, F.; Wahjuni, E.S.; Matsuyama, R.; Tsunematsu, M.; Kakehashi, M. Health Literacy and Health Behavior: Associated Factors in Surabaya High School Students, Indonesia. Int. J. Environ. Res. Public Health 2021, 18, 8111. [Google Scholar] [CrossRef]
- Zheng, M.; Jin, H.; Shi, N.; Duan, C.; Wang, D.; Yu, X.; Li, X. The relationship between health literacy and quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2018, 16, 201. [Google Scholar] [CrossRef]
- Panagioti, M.; Skevington, S.M.; Hann, M.; Howells, K.; Blakemore, A.; Reeves, D.; Bower, P. Effect of health literacy on the quality of life of older patients with long-term conditions: A large cohort study in UK general practice. Qual. Life Res. 2018, 27, 1257–1268. [Google Scholar] [CrossRef] [PubMed]
- Islakhiyah; Kristina, S.A.; Endarti, D.; Nurhasanah, R.H. Quality of life and associated factors among students in Jambi province, Indonesia. Int. J. Pharm. Res. 2020, 12, 48–54. [Google Scholar] [CrossRef]
- Veiga, S.; Serrão, C. Health Literacy of a Sample of Portuguese Elderly. Appl. Res. Health Soc. Sci. Interface Interact. 2017, 13, 14–26. [Google Scholar] [CrossRef][Green Version]
- Tikhomirova, T.; Malykh, A.; Malykh, S. Predicting Academic Achievement with Cognitive Abilities: Cross-Sectional Study across School Education. Behav. Sci. 2020, 10, 158. [Google Scholar] [CrossRef]
- Olchik, M.R.; Ayres, A.; Ghisi, M.; Schuh, A.F.S.; Rieder, C.R.M. The impact of cognitive performance on quality of life in individualswith Parkinson’s disease. Dement. Neuropsychol. 2016, 10, 303. [Google Scholar] [CrossRef]
- Shareef, M.A.; Alamodi, A.A.; Al-Khateeb, A.A.; Abudan, Z.; Alkhani, M.A.; Zebian, S.I.; Qannita, A.S.; Tabrizi, M.J. The interplay between academic performance and quality of life among preclinical students Career choice, professional education and development. BMC Med. Educ. 2015, 15, 193. [Google Scholar] [CrossRef]
- Malibary, H.; Zagzoog, M.M.; Banjari, M.A.; Bamashmous, R.O.; Omer, A.R. Quality of Life (QoL) among medical students in Saudi Arabia: A study using the WHOQOL-BREF instrument. BMC Med. Educ. 2019, 19, 344. [Google Scholar] [CrossRef] [PubMed]
- Chazan, A.C.S.; Campos, M.R.; Portugal, F.B. Quality of life of medical students at the State University of Rio de Janeiro (UERJ), measured using Whoqol-bref: A multivariate analysis. Cien. Saude Colet. 2015, 20, 547–556. [Google Scholar] [CrossRef]
- Ali, O.; Salam, Z.; Saeed, T.; Sethi, M.R.; Irfan, M. Quality of life of medical and dental students of peshawar. J. Postgrad. Med. Inst. 2018, 32, 191–192. [Google Scholar]
- Pagnin, D.; de Queiroz, V. Influence of burnout and sleep difficulties on the quality of life among medical students. Springerplus 2015, 4, 676. [Google Scholar] [CrossRef] [PubMed]
- Naseem, S.; Orooj, F.; Ghazanfar, H.; Ghazanfar, A. Quality of life of Pakistani medical students studying in a private institution. J. Pak. Med. Assoc. 2016, 66, 579–583. [Google Scholar]
- Cauffman, E.; Shulman, E.P.; Steinberg, L.; Claus, E.; Banich, M.T.; Graham, S.; Woolard, J. Age Differences in Affective Decision Making as Indexed by Performance on the Iowa Gambling Task. Dev. Psychol. 2010, 46, 193–207. [Google Scholar] [CrossRef] [PubMed]
- Asghari, A.; Mohammadi, F.; Kamrava, S.K.; Jalessi, M.; Farhadi, M. Evaluation of quality of life in patients with obstructive sleep apnea. Eur. Arch. Otorhinolaryngol. 2013, 270, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- Sarwer, D.B.; Polonsky, H.M. The Psychosocial Burden of Obesity. Endocrinol. Metab. Clin. N. Am. 2016, 45, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Yoosuf, S.; Gupta, G.; Bhargava, R.; Kumar, N.; Ranjan, P.; Pandey, R.M.; Pandey, S.; Vikram, N.K. Magnitude of psychiatric comorbidity in patients with obesity in Northern Indian population. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102270. [Google Scholar] [CrossRef]
- Gomes, E.; Bastos, T.; Probst, M.; Ribeiro, J.C.; Silva, G.; Corredeira, R. Quality of life and physical activity levels in outpatients with schizophrenia. Rev. Bras. Psiquiatr. 2016, 38, 157–160. [Google Scholar] [CrossRef]
- Wong, F.Y.; Yang, L.; Yuen, J.W.M.; Chang, K.K.P.; Wong, F.K.Y. Assessing quality of life using WHOQOL-BREF: A cross-sectional study on the association between quality of life and neighborhood environmental satisfaction, and the mediating effect of health-related behaviors. BMC Public Health 2018, 18, 113. [Google Scholar] [CrossRef] [PubMed]
| Variables | Female | Male | Total | Stat. Value | p-Value |
|---|---|---|---|---|---|
| Socioeconomics | |||||
| Age (Mean, Sd) | 19.78 (0.920) | 19.87 (0.945) | 19.81 (0.929) | −1.189 | 0.235 1 |
| Academic Performance (Mean, Sd) | 3.43 (0.216) | 3.38 (0.220) | 3.41 (0.219) | −3.890 | 0.000 1 |
| Major | 7.056 | 0.008 2 | |||
| Non-Education | 264 (42.24%) | 157 (51.48%) | 421 (45.27%) | ||
| Education | 361 (57.76%) | 148 (48.52%) | 509 (54.73%) | ||
| Father’s Education | 24.836 | 0.000 2 | |||
| Elementary and Below | 83 (13.28%) | 26 (8.52%) | 109 (11.72%) | ||
| Junior and Senior High | 391 (62.56%) | 158 (51.80%) | 549 (59.03%) | ||
| University and Postgraduate | 151 (24.16%) | 121 (39.67%) | 272 (29.25%) | ||
| Mother’s Education | 8.02 | 0.018 2 | |||
| Elementary and Below | 82 (13.12%) | 40 (13.11%) | 122 (13.12%) | ||
| Junior and Senior High | 382 (61.12%) | 160 (52.46%) | 542 (58.28%) | ||
| University and Postgraduate | 161 (25.76%) | 105 (34.43%) | 266 (28.60%) | ||
| Allowance | 8.927 | 0.012 2 | |||
| Low | 69 (11.04%) | 54 (17.70%) | 123 (13.23%) | ||
| Medium | 227 (36.32%) | 112 (36.72%) | 339 (36.45%) | ||
| High | 329 (52.64%) | 139 (45.57%) | 468 (50.32%) | ||
| Internet Access | 5.555 | 0.135 2 | |||
| No Private Internet | 147 (23.52%) | 56 (18.36%) | 203 (21.83%) | ||
| <10 giga | 164 (26.24%) | 72 (23.61%) | 236 (25.38%) | ||
| >10 giga, <Unlimited | 149 (23.84%) | 87 (28.52%) | 236 (25.38%) | ||
| Unlimited | 329 (52.64%) | 139 (45.57%) | 255 (27.42%) | ||
| Health Literacy | |||||
| CHL | 0.217 | 0.897 2 | |||
| Inadequate | 33 (5.28%) | 14 (4.59%) | 47 (5.05%) | ||
| Problematic | 167 (26.72%) | 81 (26.56%) | 248 (26.67%) | ||
| Sufficient | 425 (68.00%) | 210 (68.85%) | 635 (68.28%) | ||
| FHL | 13.129 | 0.001 2 | |||
| Limited | 255 (40.80%) | 162 (53.11%) | 417 (44.84%) | ||
| Marginal | 248 (39.68%) | 101 (33.11%) | 349 (37.53%) | ||
| Average | 122 (19.52%) | 42 (13.77%) | 164 (17.63%) | ||
| Health Behaviors | |||||
| Smoking | 78.714 | 0.000 2 | |||
| No | 618 (98.88%) | 257 (84.26%) | 875 (94.10%) | ||
| Yes | 7 (1.12%) | 48 (15.74%) | 55 (5.90%) | ||
| Alcohol | 18.342 | 0.000 2 | |||
| No | 593 (94.88%) | 265 (86.89%) | 858 (92.30%) | ||
| Yes | 32 (5.12%) | 40 (13.11%) | 72 (7.70%) | ||
| Sleeping Hour | 0.213 | 0.649 2 | |||
| Less | 348 (55.68%) | 165 (54.10%) | 504 (54.20%) | ||
| Enough | 277 (44.32%) | 140 (45.90%) | 426 (45.80%) | ||
| Physical exercise | 28.963 | 0.000 2 | |||
| No | 296 (47.36%) | 88 (28.85%) | 384 (41.30%) | ||
| Yes | 329 (52.64%) | 217 (71.15%) | 546 (58.70%) | ||
| Health Outcome | |||||
| BMI | 16.637 | 0.000 2 | |||
| Underweight | 159 (25.44%) | 45 (14.75%) | 204 (21.90%) | ||
| Normal Weight | 358 (57.28%) | 185 (60.66%) | 543 (58.40%) | ||
| Obese | 108 (17.28%) | 75 (24.59%) | 183 (19.70%) | ||
| Quality of Life | |||||
| Physical Health (Mean, Sd) | 57.02 (10.86) | 56.97 (11.31) | 57.00 (11.01) | −0.407 | 0.684 1 |
| Psychological Health (Mean, Sd) | 62.56 (10.91) | 62.37 (13.06) | 62.50 (11.65) | −0.180 | 0.857 1 |
| Social Relationships (Mean, Sd) | 61.80 (16.82) | 62.99 (16.86) | 62.19 (16.83) | −0.654 | 0.513 1 |
| Environmental Health (Mean, Sd) | 64.11 (11.89) | 63.71 (12.93) | 63.98 (12.23) | −0.218 | 0.828 1 |
| Variables | Physical Health | Psychological Health | Social Relationship | Environmental Health | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (Sd) | p-Value (Statistics) | Mean (Sd) | p-Value (Statistics) | Mean (Sd) | p-Value (Statistics) | Mean (Sd) | p-Value (Statistics) | |
| Socioeconomics | ||||||||
| Age | - | 0.016 1 (0.079) | - | 0.277 1 (0.036) | - | 0.128 1 (0.050) | - | 0.003 1 (0.096) |
| Gender | 0.684 2 (−0.407) | 0.857 2 (−0.180) | 0.513 2 (−0.654) | 0.828 2 (−0.218) | ||||
| Female | 57.02 (10.86) | 62.56 (10.91) | 61.80 (16.82) | 64.11 (11.89) | ||||
| Male | 56.97 (11.31) | 62.37 (13.06) | 62.99 (16.86) | 63.71 (12.93) | ||||
| Academic Performance | - | 0.009 1 (0.086) | - | 0.001 1 (0.108) | - | 0.040 1 (0.067) | - | 0.005 1 (0.092) |
| Major | 0.099 2 (−1.648) | 0.002 2 (−3.101) | 0.028 2 (−2.203) | 0.002 2 (−3.050) | ||||
| Non-Education | 56.26 (11.70) | 60.94 (12.09) | 60.24 (16.59) 2 | 63.07 (12.85) | ||||
| Education | 55.14 (19.00) | 59.78 (25.00) | 58.65 (19.00) | 61.84 (25.00) | ||||
| Father’s Education | 0.159 3 (3.683) | 0.490 3 (1.426) | 0.679 3 (0.774) | 0.002 3 (12.663) | ||||
| Elementary and Below | 55.65 (10.98) | 62.62 (9.94) | 60.68 (17.34) | 61.19 (12.47) | ||||
| Junior and Senior High | 56.77 (10.87) | 62.14 (11.96) | 62.17 (16.75) | 63.72 (11.80) | ||||
| University and Postgraduate | 58.02 (11.24) | 63.16 (11.66) | 62.84 (16.81) | 65.62 (12.79) | ||||
| Mother’s Education | 0.824 3 (0.386) | 0.644 3 (0.881) | 0.983 3 (0.034) | 0.071 3 (5.285) | ||||
| Elementary and Below | 56.43 (12.17) | 61.71 (11.59) | 62.69 (17.82) | 62.96 (13.40) | ||||
| Junior and Senior High | 57.04 (10.57) | 62.41 (11.56) | 62.01 (16.56) | 63.41 (11.82) | ||||
| University and Postgraduate | 57.18 (11.35) | 63.04 (11.89) | 62.32 (16.97) | 65.61 (12.40) | ||||
| Allowance | 0.517 3 (1.318) | 0.056 3 (5.750) | 0.290 3 (2.478) | 0.000 3 (18.204) | ||||
| Low | 56.06 (11.51) | 60.71 (12.48) | 60.39 (19.33) | 62.98 (13.89) | ||||
| Medium | 56.60 (10.70) | 62.07 (11.10) | 61.72 (16.47) | 62.23 (11.21) | ||||
| High | 57.54 (11.08) | 63.27 (11.78) | 63.00 (16.37) | 65.51 (12.31) | ||||
| Internet Access | 0.247 3 (4.141) | 0.367 3 (3.163) | 0.144 3 (5.415) | 0.006 3 (12.446) | ||||
| No Private Internet | 57.76 (11.50) | 63.04 (12.14) | 62.29 (19.48) | 65.79 (14.22) | ||||
| <10 giga | 55.77 (10.66) | 62.30 (10.86) | 63.15 (15.92) | 62.17 (11.19) | ||||
| >10 giga, <Unlimited | 57.82 (11.63) | 61.61 (12.32) | 60.14 (16.08) | 63.49 (11.96) | ||||
| Unlimited | 56.78 (10.24) | 63.07 (11.34) | 63.12 (15.96) | 64.66 (11.49) | ||||
| Health Literacy | ||||||||
| FHL | 0.000 3 (15.497) | 0.140 3 (3.929) | 0.018 3 (8.085) | 0.214 3 (3.087) | ||||
| Limited | 58.49 (11.05) | 63.11 (11.99) | 63.73 (16.36) | 64.63 (12.21) | ||||
| Marginal | 55.69 (10.68) | 62.36 (10.75) | 61.79 (16.47) | 63.53 (11.67) | ||||
| Average | 56.01 (11.16) | 61.21 (12.56) | 59.12 (18.33) | 63.27 (13.42) | ||||
| CHL | 0.000 3 (21.367) | 0.000 3 (25.717) | 0.000 3 (15.947) | 0.000 3 (43.464) | ||||
| Inadequate | 50.64 (12.18) | 56.96 (12.34) | 55.36 (19.41) | 55.28 (15.12) | ||||
| Problematic | 55.82 (11.04) | 60.24 (11.80) | 59.43 (16.67) | 61.21 (11.74) | ||||
| Sufficient | 57.93 (10.71) | 63.79 (11.30) | 63.77 (16.44) | 65.70 (11.72) | ||||
| Health Behaviors | ||||||||
| Smoking | 0.050 2 (−1.962) | 0.764 2 (−0.300) | 0.734 2 (−0.340) | 0.630 2 (−0.482) | ||||
| No | 57.15 (10.97) | 62.45 (11.72) | 62.23 (16.90) | 63.98 (12.20) | ||||
| Yes | 54.60 (11.39) | 63.24 (10.53) | 61.55 (15.80) | 63.89 (12.79) | ||||
| Alcohol | 0.829 2 (−0.216) | 0.761 2 (−0.304) | 0.819 2 (−0.229) | 0.898 2 (−0.129) | ||||
| No | 57.04 (11.13) | 62.53 (11.70) | 62.22 (16.83) | 63.98 (12.34) | ||||
| Yes | 56.54 (9.43) | 62.04 (11.11) | 61.78 (16.90) | 64.01 (10.98) | ||||
| Sleep | 0.047 2 (−1.987) | 0.293 2 (−1.053) | 0.476 2 (−0.712) | 0.745 2 (−0.325) | ||||
| Not Enough | 56.43 (10.81) | 62.23 (11.22) | 62.44 (16.68) | 63.94 (12.51) | ||||
| Enough | 57.70 (11.21) | 62.82 (12.17) | 61.88 (17.03) | 64.02 (11.90) | ||||
| Physical exercise | 0.092 2 (−1.686) | 0.131 2 (−1.511) | 0.000 2 (−3.886) | 0.001 2 (−3.324) | ||||
| No | 56.27 (10.62) | 61.74 (11.27) | 59.70 (16.11) | 62.38 (11.68) | ||||
| Yes | 57.51 (11.24) | 63.03 (11.90) | 63.94 (17.12) | 65.10 (12.50) | ||||
| Health Outcome | ||||||||
| BMI | 0.386 3 (1.902) | 0.000 3 (23.293) | 0.039 3 (6.487) | 0.327 3 (2.233) | ||||
| Underweight | 57.00 (10.76) | 62.85 (10.41) | 61.84 (15.14) | 63.21 (11.83) | ||||
| Normal Weight | 57.26 (11.06) | 63.51 (11.60) | 63.10 (17.29) | 64.37 (12.23) | ||||
| Obese | 56.24 (11.11) | 59.09 (12.51) | 59.89 (17.09) | 63.68 (12.71) | ||||
| Variables | Physical Health QOL | Psychological Health QOL | Social Relationship QOL | Environmental Health QOL | ||||
|---|---|---|---|---|---|---|---|---|
| Exp β (95% CI) | p-Value | Exp β (95% CI) | p-Value | Exp β (95% CI) | p-Value | Exp β (95% CI) | p-Value | |
| Socioeconomics | ||||||||
| Gender | ||||||||
| Female | 0.996 (0.967–1.025) | 0.772 | 0.995 (0.967–1.023) | 0.733 | 0.978 (0.935–1.022) | 0.264 | 1.014 (0.986–1.043) | 0.326 |
| Male | ref. | ref. | ref. | ref. | ||||
| Age | 1.011 (0.998–1.025) | 0.107 | 1.003 (0.989–1.016) | 0.695 | 1.011 (0.990–1.032) | 0.242 | 1.012 (0.999–1.026) | 0.079 |
| Academic Performance | 1.062 (1.002–1.126) | 0.040 | 1.080 (1.019–1.144) | 0.009 | 1.045 (0.956–1.142) | 0.268 | 1.064 (1.004–1.127) | 0.039 |
| Major | ||||||||
| Non-Education | 0.984 (0.960–1.010) | 0.226 | 0.964 (0.940–0.988) | 0.003 | 0.959 (0.922–0.997) | 0.021 | 0.985 (0.961–1.010) | 0.229 |
| Education | ref. | ref. | ref. | ref. | ||||
| Father’s Education | ||||||||
| Elementary and Below | 0.975 (0.927–1.025) | 0.333 | 1.013 (0.964–1.065) | 0.565 | 0.979 (0.907–1.057) | 0.550 | 0.962 (0.916–1.011) | 0.106 |
| Junior and Senior High | 0.981 (0.952–1.012) | 0.219 | 0.989 (0.960–1.018) | 0.436 | 0.992 (0.947–1.038) | 0.695 | 0.988 (0.959–1.017) | 0.380 |
| University and Postgraduate | ref. | ref. | ref. | ref. | ||||
| Mother’s Education | ||||||||
| Elementary and Below | 0.986 (0.939–1.034) | 0.579 | 0.958 (0.914–1.005) | 0.078 | 1.004 (0.934–1.081) | 0.904 | 0.966 (0.922–1.013) | 0.148 |
| Junior and Senior High | 1.002 (0.972–1.032) | 0.909 | 0.990 (0.962–1.020) | 0.506 | 1.003 (0.958–1.049) | 0.904 | 0.974 (0.946–1.003) | 0.053 |
| University and Postgraduate | ref. | ref. | ref. | ref. | ||||
| Allowance | ||||||||
| Low | 0.996 (0.957–1.037) | 0.841 | 0.971 (0.933–1.009) | 0.151 | 0.963 (0.907–1.023) | 0.226 | 0.980 (0.943–1.019) | 0.309 |
| Medium | 0.987 (0.961–1.015) | 0.340 | 0.981 (0.955–1.008) | 0.132 | 0.978 (0.938–1.019) | 0.232 | 0.952 (0.927–0.978) | 0.000 |
| High | ref. | ref. | ref. | ref. | ||||
| Internet Access | ||||||||
| No Private Internet | 1.021 (0.985–1.058) | 0.244 | 1.006 (0.972–1.042) | 0.723 | 0.994 (0.941–1.049) | 0.804 | 1.025 (0.990–1.061) | 0.163 |
| <10 giga | 0.992 (0.959–1.027) | 0.647 | 0.999 (0.966–1.034) | 0.968 | 1.020 (0.968–1.075) | 0.390 | 0.976 (0.944–1.009) | 0.126 |
| >10 giga, <Unlimited | 1.019 (0.984–1.055) | 0.280 | 0.982 (0.949–1.016) | 0.273 | 0.958 (0.909–1.011) | 0.080 | 0.985 (0.952–1.019) | 0.364 |
| Unlimited | ref. | ref. | ref. | ref. | ||||
| Health Outcome | ||||||||
| BMI | ||||||||
| Underweight | 1.018 (0.979–1.059) | 0.361 | 1.065 (1.024–1.107) | 0.001 | 1.039 (0.979–1.103) | 0.165 | 0.997 (0.959–1.036) | 0.869 |
| Normal Weight | 1.018 (0.985–1.051) | 0.290 | 1.071 (1.037–1.106) | 0.000 | 1.050 (0.999–1.103) | 0.048 | 1.010 (0.979–1.043) | 0.520 |
| Obese | ref. | ref. | ref. | ref. | ||||
| Health Behaviors | ||||||||
| Smoking | ||||||||
| No | 1.052 (0.993–1.113) | 0.094 | 0.992 (0.938–1.049) | 0.763 | 1.038 (0.950–1.132) | 0.336 | 1.008 (0.953–1.066) | 0.768 |
| Yes | ref. | ref. | ref. | ref. | ||||
| Alcohol | ||||||||
| No | 1.001 (0.953–1.051) | 0.965 | 1.005 (0.958–1.054) | 0.829 | 1.003 (0.931–1.079) | 0.931 | 1.001 (0.954–1.049) | 0.971 |
| Yes | ref. | ref. | ref. | ref. | ||||
| Sleep | ||||||||
| Not Enough | 0.987 (0.962–1.012) | 0.296 | 0.998 (0.973–1.023) | 0.870 | 1.016 (0.977–1.056) | 0.376 | 1.001 (0.977–1.026) | 0.926 |
| Enough | ref. | ref. | ref. | ref. | ||||
| Physical exercise | ||||||||
| No | 0.983 (0.958–1.009) | 0.199 | 0.981 (0.956–1.006) | 0.120 | 0.940 (0.903–0.978) | 0.001 | 0.959 (0.935–0.984) | 0.001 |
| Yes | ref. | ref. | ref. | ref. | ||||
| Health Literacy | ||||||||
| CHL | ||||||||
| Inadequate | 0.878 (0.828–0.931) | 0.000 | 0.900 (0.850–0.954) | 0.001 | 0.874 (0.800–0.956) | 0.008 | 0.854 (0.807–0.904) | 0.000 |
| Problematic | 0.965 (0.938–0.994) | 0.015 | 0.950 (0.924–0.977) | 0.000 | 0.934 (0.894–0.976) | 0.001 | 0.937 (0.911–0.963) | 0.000 |
| Sufficient | ref. | ref. | ref. | ref. | ||||
| Variables | Physical Health QOL | Psychological Health QOL | Social Relationship QOL | Environmental Health QOL | ||||
|---|---|---|---|---|---|---|---|---|
| Exp β (95% CI) | p-Value | Exp β (95% CI) | p-Value | Exp β (95% CI) | p-Value | Exp β (95% CI) | p-Value | |
| Socioeconomics | ||||||||
| Gender | ||||||||
| Female | 1.000 (0.971–1.029) | 0.979 | 0.997 (0.969–1.026) | 0.865 | 0.981 (0.939–1.026) | 0.358 | 1.017 (0.988–1.047) | 0.248 |
| Male | ref. | ref. | ref. | ref. | ||||
| Age | 1.010 (0.996–1.023) | 0.183 | 1.001 (0.988–1.015) | 0.840 | 1.008 (0.987–1.029) | 0.386 | 1.011 (0.997–1.024) | 0.137 |
| Academic Performance | 1.078 (1.017–1.144) | 0.010 | 1.088 (1.026–1.153) | 0.005 | 1.054 (0.964–1.152) | 0.200 | 1.076 (1.015–1.141) | 0.017 |
| Major | ||||||||
| Non-Education | 0.985 (0.960–1.011) | 0.249 | 0.962 (0.938–0.986) | 0.002 | 0.956 (0.919–0.994) | 0.013 | 0.983 (0.958–1.008) | 0.170 |
| Education | ref. | ref. | ref. | ref. | ||||
| Father’s Education | ||||||||
| Elementary and Below | 0.950 (0.903–0.999) | 0.042 | 0.994 (0.945–1.045) | 0.778 | 0.951 (0.882–1.027) | 0.162 | 0.938 (0.892–0.986) | 0.007 |
| Junior and Senior High | 0.974 (0.945–1.004) | 0.083 | 0.980 (0.951–1.010) | 0.176 | 0.978 (0.934–1.024) | 0.303 | 0.978 (0.949–1.007) | 0.113 |
| University and Postgraduate | ref. | ref. | ref. | ref. | ||||
| Mother’s Education | ||||||||
| Elementary and Below | 0.991 (0.945–1.041) | 0.736 | 0.965 (0.920–1.012) | 0.128 | 1.013 (0.941–1.090) | 0.712 | 0.974 (0.929–1.022) | 0.266 |
| Junior and Senior High | 0.999 (0.969–1.029) | 0.928 | 0.988 (0.959–1.018) | 0.414 | 1.000 (0.956–1.047) | 0.986 | 0.970 (0.942–0.999) | 0.030 |
| University and Postgraduate | ref. | ref. | ref. | ref. | ||||
| Allowance | ||||||||
| Low | 0.983 (0.945–1.023) | 0.384 | 0.962 (0.925–1.001) | 0.065 | 0.951 (0.896–1.011) | 0.114 | 0.970 (0.933–1.009) | 0.142 |
| Medium | 0.986 (0.960–1.014) | 0.307 | 0.981 (0.955–1.007) | 0.126 | 0.978 (0.938–1.019) | 0.232 | 0.952 (0.927–0.978) | 0.000 |
| High | ref. | ref. | ref. | ref. | ||||
| Internet Access | ||||||||
| No Private Internet | 1.016 (0.980–1.053) | 0.373 | 1.004 (0.969–1.040) | 0.814 | 0.995 (0.942–1.050) | 0.839 | 1.023 (0.987–1.059) | 0.225 |
| <10 giga | 0.988 (0.955–1.023) | 0.474 | 0.994 (0.961–1.028) | 0.690 | 1.015 (0.963–1.070) | 0.517 | 0.968 (0.935–1.001) | 0.042 |
| >10 giga, <Unlimited | 1.013 (0.978–1.049) | 0.476 | 0.978 (0.945–1.012) | 0.190 | 0.955 (0.906–1.008) | 0.061 | 0.978 (0.945–1.013) | 0.195 |
| Unlimited | ref. | ref. | ref. | ref. | ||||
| Health Outcome | ||||||||
| BMI | ||||||||
| Underweight | 1.018 (0.978–1.059) | 0.375 | 1.065 (1.024–1.108) | 0.001 | 1.038 (0.977–1.102) | 0.171 | 0.998 (0.960–1.038) | 0.915 |
| Normal Weight | 1.019 (0.986–1.053) | 0.267 | 1.074 (1.040–1.109) | 0.000 | 1.054 (1.002–1.107) | 0.032 | 1.014 (0.982–1.047) | 0.399 |
| Obese | ref. | ref. | ref. | ref. | ||||
| Health Behaviors | ||||||||
| Smoking | ||||||||
| No | 1.045 (0.987–1.107) | 0.138 | 0.982 (0.928–1.039) | 0.492 | 1.025 (0.939–1.118) | 0.525 | 0.992 (0.937–1.050) | 0.785 |
| Yes | ref. | ref. | ref. | ref. | ||||
| Alcohol | ||||||||
| No | 1.012 (0.963–1.063) | 0.624 | 1.012 (0.964–1.063) | 0.600 | 1.018 (0.944–1.097) | 0.611 | 1.010 (0.962–1.061) | 0.664 |
| Yes | ref. | ref. | ref. | ref. | ||||
| Sleep | ||||||||
| Not Enough | 0.990 (0.964–1.015) | 0.410 | 0.998 (0.973–1.024) | 0.889 | 1.019 (0.980–1.059) | 0.311 | 1.002 (0.977–1.027) | 0.892 |
| Enough | ref. | ref. | ref. | ref. | ||||
| Physical exercise | ||||||||
| No | 0.990 (0.964–1.016) | 0.437 | 0.986 (0.961–1.012) | 0.270 | 0.948 (0.911–0.986) | 0.004 | 0.964 (0.940–0.990) | 0.006 |
| Yes | ref. | ref. | ref. | ref. | ||||
| Health Literacy | ||||||||
| FHL | ||||||||
| Limited | 1.048 (1.010–1.086) | 0.011 | 1.032 (0.996–1.069) | 0.094 | 1.075 (1.017–1.135) | 0.009 | 1.022 (0.986–1.059) | 0.249 |
| Marginal | 0.994 (0.959–1.031) | 0.761 | 1.017 (0.981–1.054) | 0.362 | 1.039 (0.983–1.098) | 0.168 | 1.001 (0.966–1.038) | 0.940 |
| Average | ref. | - | ref. | - | ref. | - | ref. | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prihanto, J.B.; Wahjuni, E.S.; Nurhayati, F.; Matsuyama, R.; Tsunematsu, M.; Kakehashi, M. Health Literacy, Health Behaviors, and Body Mass Index Impacts on Quality of Life: Cross-Sectional Study of University Students in Surabaya, Indonesia. Int. J. Environ. Res. Public Health 2021, 18, 13132. https://doi.org/10.3390/ijerph182413132
Prihanto JB, Wahjuni ES, Nurhayati F, Matsuyama R, Tsunematsu M, Kakehashi M. Health Literacy, Health Behaviors, and Body Mass Index Impacts on Quality of Life: Cross-Sectional Study of University Students in Surabaya, Indonesia. International Journal of Environmental Research and Public Health. 2021; 18(24):13132. https://doi.org/10.3390/ijerph182413132
Chicago/Turabian StylePrihanto, Junaidi Budi, Endang Sri Wahjuni, Faridha Nurhayati, Ryota Matsuyama, Miwako Tsunematsu, and Masayuki Kakehashi. 2021. "Health Literacy, Health Behaviors, and Body Mass Index Impacts on Quality of Life: Cross-Sectional Study of University Students in Surabaya, Indonesia" International Journal of Environmental Research and Public Health 18, no. 24: 13132. https://doi.org/10.3390/ijerph182413132
APA StylePrihanto, J. B., Wahjuni, E. S., Nurhayati, F., Matsuyama, R., Tsunematsu, M., & Kakehashi, M. (2021). Health Literacy, Health Behaviors, and Body Mass Index Impacts on Quality of Life: Cross-Sectional Study of University Students in Surabaya, Indonesia. International Journal of Environmental Research and Public Health, 18(24), 13132. https://doi.org/10.3390/ijerph182413132






