Opportunities and Barriers of Telemedicine in Rheumatology: A Participatory, Mixed-Methods Study
Abstract
:1. Introduction
“[T]he practice of medicine over a distance, in which interventions, diagnoses, therapeutic decisions, and subsequent treatment recommendations are based on patient data, documents and other information transmitted through telecommunication systems” [12].
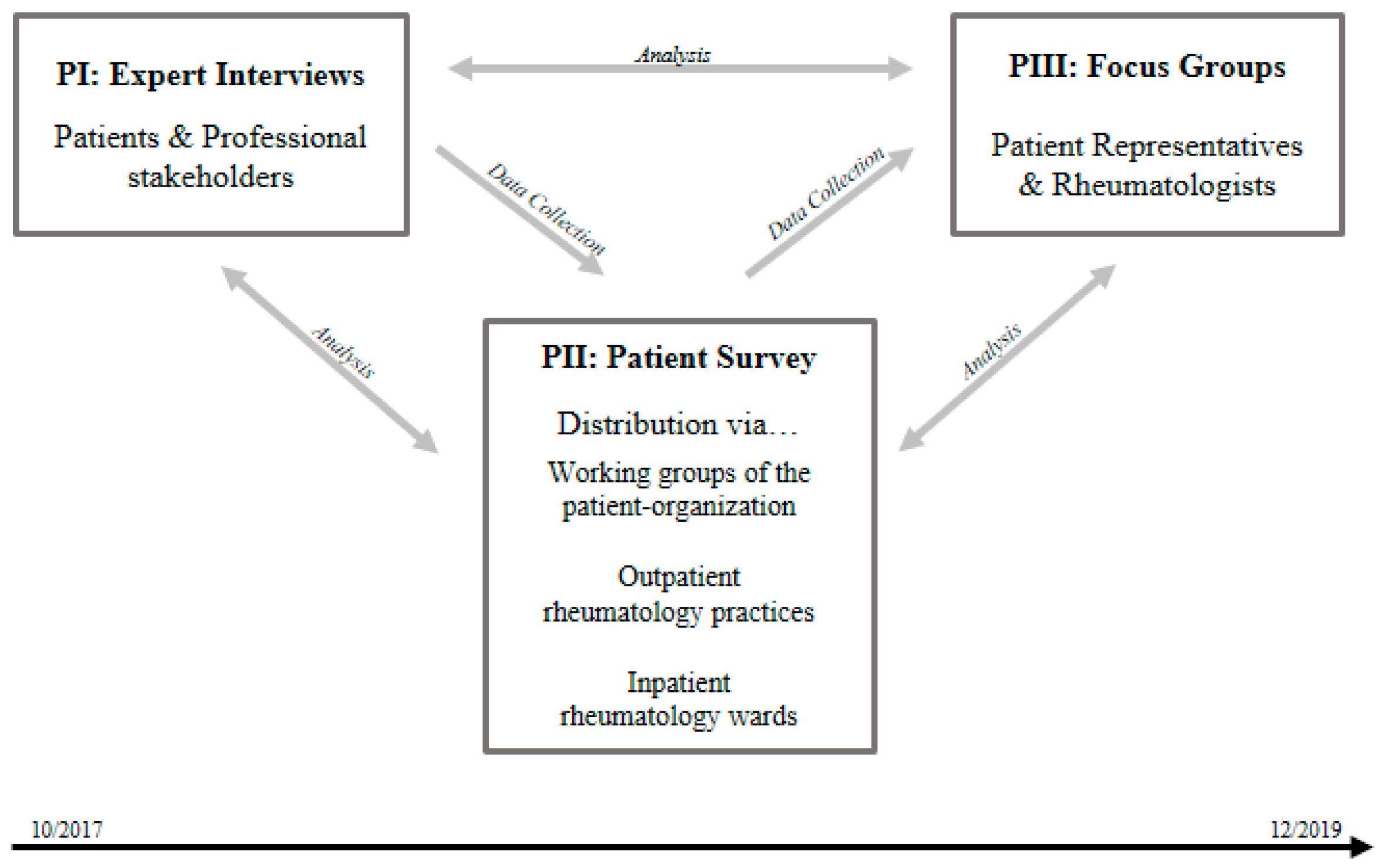
2. Materials and Methods
2.1. Study Design
2.2. Expert Interviews
2.3. Patient Survey
2.4. Focus Groups
2.5. Qualitative Content Analysis
3. Results
3.1. Expert Interviews
3.1.1. Conceptualization of Telemedicine
“Telemedicine is comparable to the word digitalization. Everything and nothing. I think telemedicine starts where there is internet access. And I would understand telemedicine as using the technical conditions that we have as efficiently as possible for the benefit of all. And for me, telemedicine is not only the internet access in the medical practice, but also not necessarily the utmost... In other words, performing surgery between two hospitals via a monitor. It’s more about using platforms like internet consultations, especially nowadays. So that, the insured also have the opportunity to work with a technical system. In other words, that smartphones are used appropriately. That’s how I would actually define telemedicine—well, I think this is somehow wrong. Because telemedicine covers a whole lot of things. And I would say that if you put it very simply, you could actually start telemedicine with the electronic medical letter. This has nothing whatsoever to do with the patient himself, but people send things back and forth to each other without using paper. So I would actually say: Telemedicine is everything and nothing, but it definitely starts with the internet connection.” (Interview 17, Professional Stakeholder: Health insurance representative, Pos. 19)
3.1.2. Patients’ Perspectives
“No, I think it’s important. I have to have my doctor right in front of me and he has to have me. Otherwise, a lot of things get lost… for example the way we deal with and trust each other.” (Interview 14, Patient, Pos. 110)
“But I do think that telemedicine is a good thing. You live far away and then suddenly there’s something. For example, in my case here. I got a little thing with the skin. (…) By that it is possible to quickly ask someone competent. ‘My God, I actually have to go there tomorrow and now all the joints are swollen and so on’. The rheumatologist would know what to do. He can give you a quick hint: ‘Do this or that or this’. So you don’t have to go 30 km, wait four hours and then go back 30 km.” (Interview 4, Patient, Pos. 125)
“With [name of a video conference service] and the whole thing- Who of the old people up there in Mecklenburg [dense populated region in Germany] or so has the technical equipment? I always ask myself.” (Interview 4, Patient, Pos. 125)
“As I said, I see the issue that you can no longer control who gets hold of certain data and what they do with it. (...) Suddenly people find out things, who should not have access to this information. And that’s really just the tip of it, because you can’t imagine what could be done with such data there.” (Interview 2, Patient, Pos. 302)
3.1.3. Professional Stakeholders’ Perspectives
“Well, at the end of the day, I consider it as something supportive. It cannot replace the direct contact, the complete direct contact between doctor and patient, it neither can nor should. Because I think I also have to touch, I also have to see personally in front of me, without that it doesn’t work.” (Interview 10, Professional stakeholder: Rheumatologist, Pos. 93)
“It is a paradox, that patients who would be most affected by it [telemedicine], patients who live far away from the city, (...) still have white spots in their surroundings, for example areas, residential areas where ISDN is available. They don’t even have DSL 2000, they don’t have anything. And it doesn’t matter whether they want to or not, they simply can’t hold a video conference.” (Interview 22, Professional stakeholder: General practitioner, Pos. 40)
“And I can’t bill that at all in the S[ocial] H[ealth] I[nsurance] system, so it’s a hobby that I do. But I do have hobbies. Most of my colleagues have hobbies, they know what they can do in their free time. You can’t. You can’t do hobby activities at work. That is not possible. And that’s just telemedicine, unfortunately, that falls into it.” (Interview 28, Professional stakeholder: General Practitioner, Pos. 45)
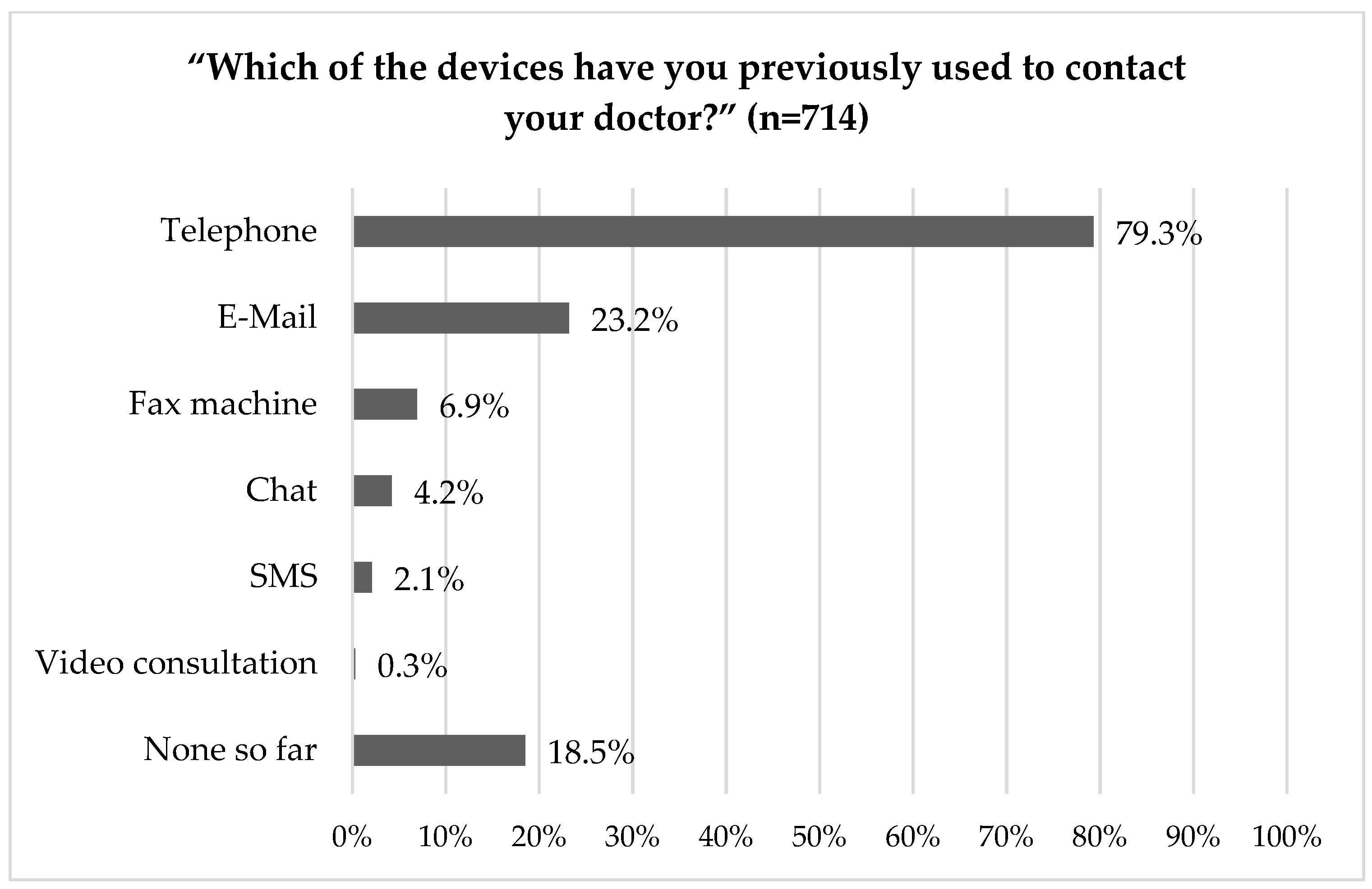
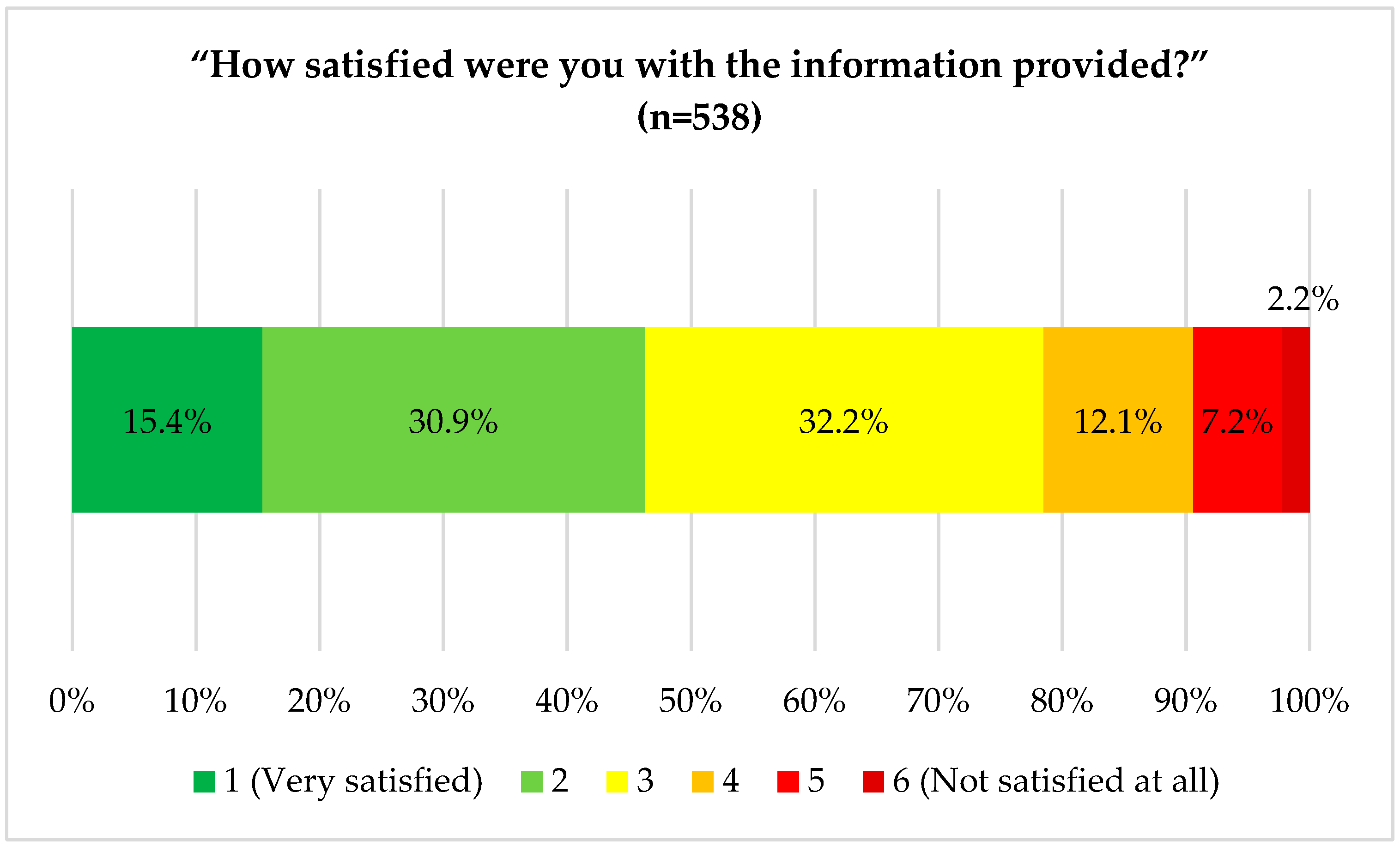
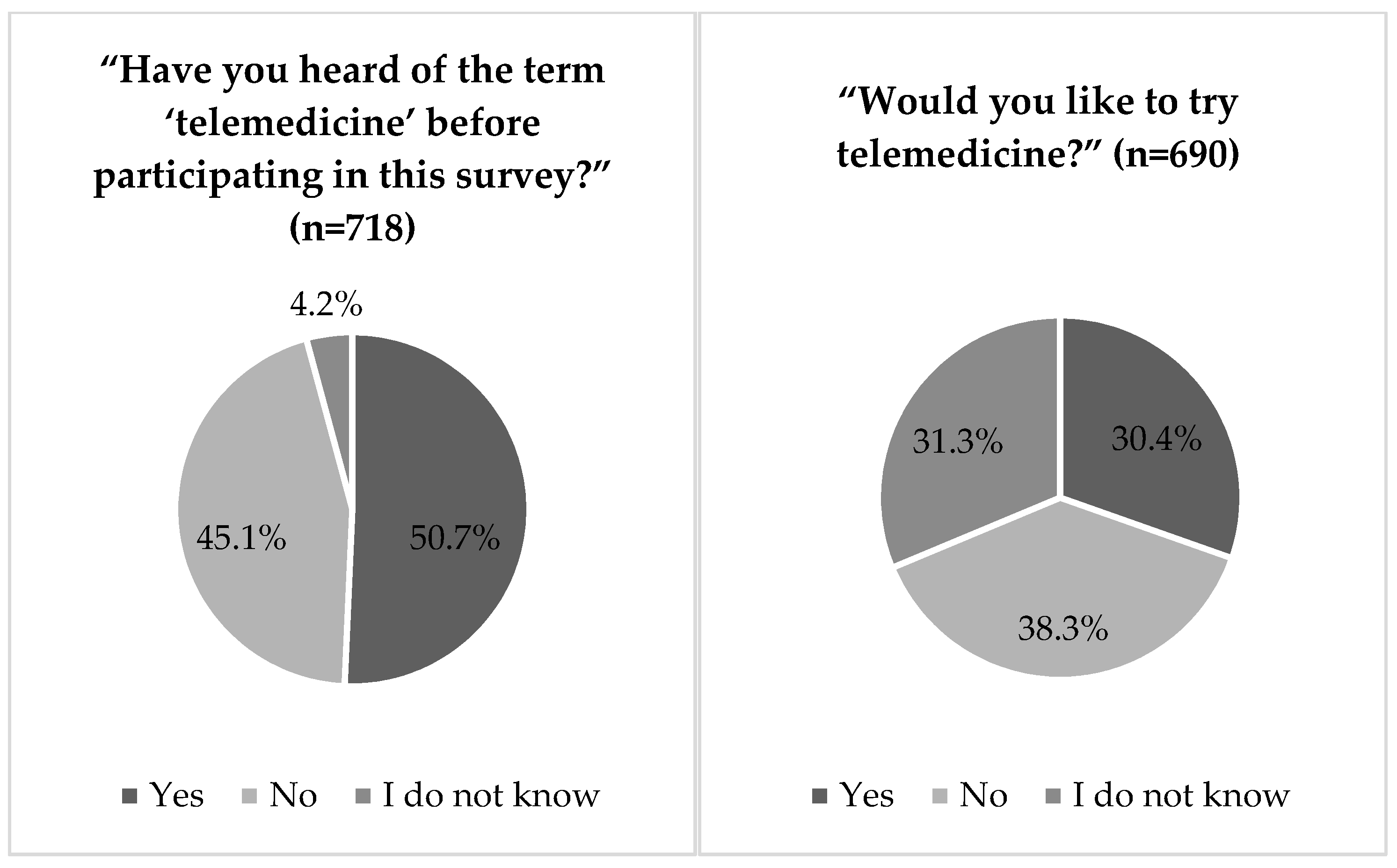
3.2. Patient Survey
3.2.1. Technology Use in Health Care
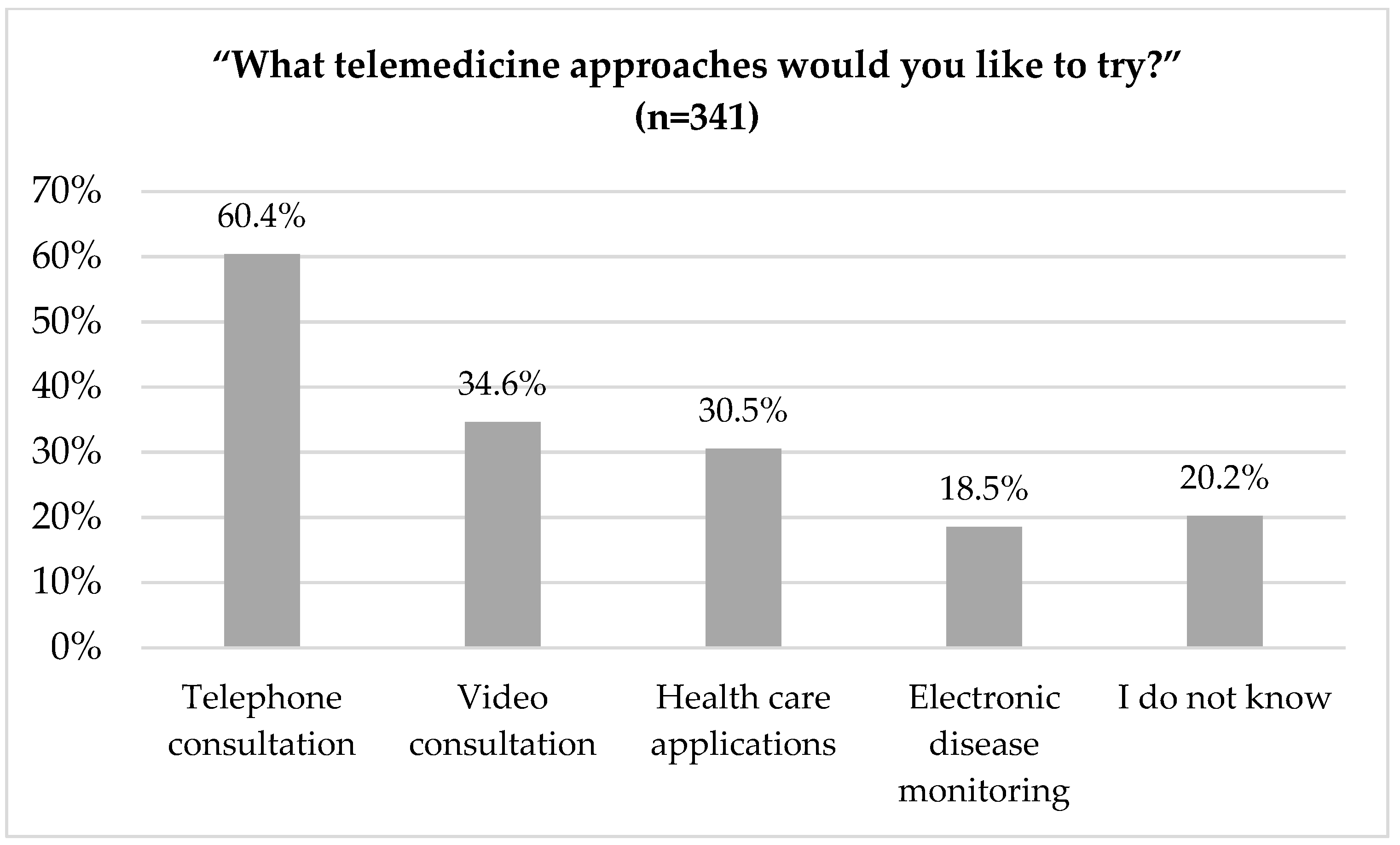
3.2.2. Telemedicine
3.3. Focus Groups
“Discussant: Well, personal contact with the doctor is important. And not taking a picture and sending it somewhere. For me, personal contact is most important. Interviewer: And personal contact means you want to be in the same room with the doctor? Discussant: Yes.” (Focus group 2, Patient representative, Pos. 174)
“Then I also imagine an overload for the doctor. Because he now also has patients who he doesn’t know. That would be irresponsible, because he doesn’t see the whole person and so on. I don’t want to imagine that at all. So at the very most, if you are under a doctor’s care and he knows you, you may then also ask a question by phone or by video or by telemedicine. For a doctor who has never seen me or so, I would not actually agree with that. (Focus group 2, Patient representative, Pos. 178)
“I’m interested in the organizational side of things. When I make a phone call now, where do I actually end up? Is it a doctor who has office hours there, who only does telemedicine? Because when I arrive at my doctor’s office, he doesn’t have any time, he has to see his patients. He can’t focus on me. I do not see it.” (Focus group 2, Patient representative, Pos. 116)
“Perhaps telemedicine can then be seen more or less as a digital safety or support network, so to speak. We as physicians are more or less automatically notified of potential problems thus we can react as promptly as possible in the consultation.” (Focus group 1, Rheumatologists Pos. 40)
“We are all open-minded, but nevertheless the doctors have no time for it... to practice telemedicine in addition to their normal office hours. It only works if retired doctors are brought on board again. So from there, the topic of time savings, I think you have to carefully consider for whom this is a time saving.” (Focus group 1, Rheumatologists, Pos. 26)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sebbag, E.; Felten, R.; Sagez, F.; Sibilia, J.; Devilliers, H.; Arnaud, L. The world-wide burden of musculoskeletal diseases: A systematic analysis of the World Health Organization Burden of Diseases Database. Ann. Rheum. Dis. 2019, 78, 844–848. [Google Scholar] [CrossRef]
- Krusche, M.; Sewerin, P.; Kleyer, A.; Mucke, J.; Vossen, D.; Morf, H. [Specialist training quo vadis?]. Z. Rheumatol. 2019, 78, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Al Maini, M.; Adelowo, F.; Al Saleh, J.; Al Weshahi, Y.; Burmester, G.R.; Cutolo, M.; Flood, J.; March, L.; McDonald-Blumer, H.; Pile, K.; et al. The global challenges and opportunities in the practice of rheumatology: White paper by the World Forum on Rheumatic and Musculoskeletal Diseases. Clin. Rheumatol. 2015, 34, 819–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sørensen, J.; Hetland, M.L. Diagnostic delay in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis: Results from the Danish nationwide DANBIO registry. Ann. Rheum. Dis. 2015, 74, e12. [Google Scholar] [CrossRef] [Green Version]
- Quinn, M.A.; Emery, P. Window of opportunity in early rheumatoid arthritis: Possibility of altering the disease process with early intervention. Clin. Exp. Rheumatol. 2003, 21, S154–S157. [Google Scholar]
- Mitra, A.; Veerakone, R.; Li, K.; Nix, T.; Hashikawa, A.; Mahajan, P. Telemedicine in paediatric emergency care: A systematic review. J. Telemed. Telecare 2021, 1357633X211010106. [Google Scholar] [CrossRef]
- Battineni, G.; Sagaro, G.G.; Chintalapudi, N.; Amenta, F. The Benefits of Telemedicine in Personalized Prevention of Cardiovascular Diseases (CVD): A Systematic Review. J. Pers. Med. 2021, 11, 658. [Google Scholar] [CrossRef]
- da Fonseca, M.H.; Kovaleski, F.; Picinin, C.T.; Pedroso, B.; Rubbo, P. E-Health Practices and Technologies: A Systematic Review from 2014 to 2019. Healthcare (Basel) 2021, 9, 1192. [Google Scholar] [CrossRef]
- May, S.; Jonas, K.; Fehler, G.V.; Zahn, T.; Heinze, M.; Muehlensiepen, F. Challenges in current nursing home care in rural Germany and how they can be reduced by telehealth—An exploratory qualitative pre-post study. BMC Health Serv. Res. 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Labarca, G.; Schmidt, A.; Dreyse, J.; Jorquera, J.; Barbe, F. Telemedicine interventions for CPAP adherence in obstructive sleep apnea patients: Systematic review and meta-analysis. Sleep Med. Rev. 2021, 60, 101543. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.J.; Crichton, M.; Crawford-Williams, F.; Agbejule, O.A.; Yu, K.; Hart, N.H.; de Abreu Alves, F.; Ashbury, F.D.; Eng, L.; Fitch, M.; et al. The efficacy, challenges, and facilitators of telemedicine in post-treatment cancer survivorship care: An overview of systematic reviews. Ann. Oncol. Off. J. Eur. Soc. Oncol. 2021, 32, 1552–1570. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Statement on the Ethics of Telemedicine. 2018. Available online: https://www.wma.net/policies-post/wma-statement-on-the-ethics-of-telemedicine/ (accessed on 8 March 2021).
- World Health Organisation. Telemedicine. Opportunities and Developments in Member States. Report on the Second Global Survey on eHealth. Global Observatory for eHealth Series—Volume 2. Available online: https://www.who.int/goe/publications/goe_telemedicine_2010.pdf (accessed on 25 November 2021).
- Snoswell, C.L.; Chelberg, G.; De Guzman, K.R.; Haydon, H.H.; Thomas, E.E.; Caffery, L.J.; Smith, A.C. The clinical effectiveness of telehealth: A systematic review of meta-analyses from 2010 to 2019. J. Telemed. Telecare 2021, 1357633x211022907. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.B.; Frost, L.; Stengaard, C.; Brorholt-Petersen, J.U.; Dodt, K.K.; Søndergaard, H.M.; Terkelsen, C.J. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triaging and treatment of STEMI. Heart (Br. Card. Soc.) 2014, 100, 711–715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koehler, F.; Koehler, K.; Deckwart, O.; Prescher, S.; Wegscheider, K.; Kirwan, B.A.; Winkler, S.; Vettorazzi, E.; Bruch, L.; Oeff, M.; et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): A randomised, controlled, parallel-group, unmasked trial. Lancet (Lond. Engl.) 2018, 392, 1047–1057. [Google Scholar] [CrossRef]
- Russo, J.E.; McCool, R.R.; Davies, L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2016, 22, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Sayani, S.; Muzammil, M.; Saleh, K.; Muqeet, A.; Zaidi, F.; Shaikh, T. Addressing cost and time barriers in chronic disease management through telemedicine: An exploratory research in select low- and middle-income countries. Adv. Chronic Dis. 2019, 10, 2040622319891587. [Google Scholar] [CrossRef] [Green Version]
- Ward, I.M.; Schmidt, T.W.; Lappan, C.; Battafarano, D.F. How Critical is Tele-Medicine to the Rheumatology Workforce? Arthritis Care Res. 2016, 68, 1387–1389. [Google Scholar] [CrossRef] [Green Version]
- Rezaian, M.M.; Brent, L.H.; Roshani, S.; Ziaee, M.; Sobhani, F.; Dorbeigi, A.; Fatehi, Z.; Hardy, J.; Ragati Haghi, Y.; Maghsoudi, T.; et al. Rheumatology Care Using Telemedicine. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2020, 26, 335–340. [Google Scholar] [CrossRef]
- Welcker, M.; Mühlensiepen, F.; Knitza, J.; Popp, F.; Aries, P. Digitalization in rheumatological practice. Z. Rheumatol. 2021, 80, 835–845. [Google Scholar] [CrossRef]
- Najm, A.; Nikiphorou, E.; Kostine, M.; Richez, C.; Pauling, J.D.; Finckh, A.; Ritschl, V.; Prior, Y.; Balážová, P.; Stones, S.; et al. EULAR points to consider for the development, evaluation and implementation of mobile health applications aiding self-management in people living with rheumatic and musculoskeletal diseases. RMD Open 2019, 5, e001014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muehlensiepen, F.; Knitza, J.; Marquardt, W.; Engler, J.; Hueber, A.; Welcker, M. Acceptance of Telerheumatology by Rheumatologists and General Practitioners in Germany: Nationwide Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e23742. [Google Scholar] [CrossRef]
- Health Innovation Hub. DVG—A Summary of Germany’s New Law for Digital Health Applications. Available online: https://hih-2025.de/dvg-a-summary-of-germanys-new-law-for-digital-health-applications/ (accessed on 25 November 2021).
- Bruch, D.; Muehlensiepen, F.; Alexandrov, A.; Konstantinova, Y.; Voß, K.; Ronckers, C.; Neugebauer, E.; May, S. The impact of the COVID-19 pandemic on professional practice and patient volume in medical practices: A survey among German physicians and psychotherapists. Z. Evid. Qual. Gesundhwes 2021, 166, 27–35. [Google Scholar] [CrossRef]
- Kernder, A.; Morf, H.; Klemm, P.; Vossen, D.; Haase, I.; Mucke, J.; Meyer, M.; Kleyer, A.; Sewerin, P.; Bendzuck, G.; et al. Digital rheumatology in the era of COVID-19: Results of a national patient and physician survey. RMD Open 2021, 7, e001548. [Google Scholar] [CrossRef]
- Zentral Institut für Kassenärztliche Versorgung in Deutschland. With Second Corona Lockdown Starting in November 2020, Another Significant Decline in Outpatient Treatment Cases // Physician Practices with Vaccination Record against Influenza and Pneumococci. Available online: https://www.zi.de/presse/presseinformationen/19-april-2021 (accessed on 25 November 2021).
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogner, A.; Littig, B.; Menz, W. Interviewing Experts; Palgrave Macmillan: London, UK, 2009. [Google Scholar]
- Robinson, O.C. Sampling in Interview-Based Qualitative Research: A Theoretical and Practical Guide. Qual. Res. Psychol. 2014, 11, 25–41. [Google Scholar] [CrossRef]
- Krueger, R.A.; Casey, M.A. Focus Groups: A Practical Guide for Applied Research, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- Kuckartz, U. Qualitative Inhaltsanalyse, 4th ed.; Beltz Juventa: Weinheim, Germany, 2018. [Google Scholar]
- Kurkowski, S.; Radon, J.; Vogt, A.R.; Weber, M.; Stiel, S.; Ostgathe, C.; Heckel, M. Hospital end-of-life care: Families’ free-text notes. BMJ Support. Palliat. Care 2020. [Google Scholar] [CrossRef]
- Matsumoto, R.A.; England, B.R.; Mastarone, G.; Richards, J.S.; Chang, E.; Wood, P.R.; Barton, J.L. Rheumatology Clinicians’ Perceptions of Telerheumatology Within the Veterans Health Administration: A National Survey Study. Mil. Med. 2020, 185, e2082–e2087. [Google Scholar] [CrossRef] [PubMed]
- Nazeha, N.; Pavagadhi, D.; Kyaw, B.M.; Car, J.; Jimenez, G.; Car, L.T. A Digitally Competent Health Workforce: Scoping Review of Educational Frameworks. J. Med. Internet Res. 2020, 22, e22706. [Google Scholar] [CrossRef] [PubMed]
- Mühlensiepen, F.; Kurkowski, S.; Krusche, M.; Mucke, J.; Prill, R.; Heinze, M.; Welcker, M.; Schulze-Koops, H.; Vuillerme, N.; Schett, G.; et al. Digital Health Transition in Rheumatology: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 2636. [Google Scholar] [CrossRef]
- de Thurah, A.; Stengaard-Pedersen, K.; Axelsen, M.; Fredberg, U.; Schougaard, L.M.V.; Hjollund, N.H.I.; Pfeiffer-Jensen, M.; Laurberg, T.B.; Tarp, U.; Lomborg, K.; et al. Tele-Health Followup Strategy for Tight Control of Disease Activity in Rheumatoid Arthritis: Results of a Randomized Controlled Trial. Arthritis Care Res. 2018, 70, 353–360. [Google Scholar] [CrossRef] [Green Version]
- Agha, Z.; Schapira, R.M.; Laud, P.W.; McNutt, G.; Roter, D.L. Patient satisfaction with physician-patient communication during telemedicine. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2009, 15, 830–839. [Google Scholar] [CrossRef] [PubMed]
- Piga, M.; Cangemi, I.; Mathieu, A.; Cauli, A. Telemedicine for patients with rheumatic diseases: Systematic review and proposal for research agenda. Semin. Arthritis Rheum. 2017, 47, 121–128. [Google Scholar] [CrossRef] [PubMed]
- McDougall, J.A.; Ferucci, E.D.; Glover, J.; Fraenkel, L. Telerheumatology: A Systematic Review. Arthritis Care Res. 2017, 69, 1546–1557. [Google Scholar] [CrossRef]
- Kulcsar, Z.; Albert, D.; Ercolano, E.; Mecchella, J.N. Telerheumatology: A technology appropriate for virtually all. Semin. Arthritis Rheum. 2016, 46, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Knitza, J.; Simon, D.; Lambrecht, A.; Raab, C.; Tascilar, K.; Hagen, M.; Kleyer, A.; Bayat, S.; Derungs, A.; Amft, O.; et al. Mobile Health Usage, Preferences, Barriers, and eHealth Literacy in Rheumatology: Patient Survey Study. JMIR mHealth uHealth 2020, 8, e19661. [Google Scholar] [CrossRef] [PubMed]
- Edwards, L.; Thomas, C.; Gregory, A.; Yardley, L.; O’Cathain, A.; Montgomery, A.A.; Salisbury, C. Are people with chronic diseases interested in using telehealth? A cross-sectional postal survey. J. Med. Internet Res. 2014, 16, e123. [Google Scholar] [CrossRef] [Green Version]
- Bhaskar, S.; Bradley, S.; Chattu, V.K.; Adisesh, A.; Nurtazina, A.; Kyrykbayeva, S.; Sakhamuri, S.; Yaya, S.; Sunil, T.; Thomas, P.; et al. Telemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front. Public Health 2020, 8, 556720. [Google Scholar] [CrossRef]
- Mehta, B.; Jannat-Khah, D.; Fontana, M.A.; Moezinia, C.J.; Mancuso, C.A.; Bass, A.R.; Antao, V.C.; Gibofsky, A.; Goodman, S.M.; Ibrahim, S. Impact of COVID-19 on vulnerable patients with rheumatic disease: Results of a worldwide survey. RMD Open 2020, 6, e001378. [Google Scholar] [CrossRef]
- Miloslavsky, E.M.; Bolster, M.B. Addressing the rheumatology workforce shortage: A multifaceted approach. Semin. Arthritis Rheum. 2020, 50, 791–796. [Google Scholar] [CrossRef]
- Choi, B.C.; Pak, A.W. A catalog of biases in questionnaires. Prev. Chronic Dis. 2005, 2, A13. [Google Scholar]
- Hohwü, L.; Lyshol, H.; Gissler, M.; Jonsson, S.H.; Petzold, M.; Obel, C. Web-based versus traditional paper questionnaires: A mixed-mode survey with a Nordic perspective. J. Med. Internet Res. 2013, 15, e173. [Google Scholar] [CrossRef] [PubMed]

| # | Date | Role/Profession | Age | Gender | TM User 1 |
|---|---|---|---|---|---|
| 1 | 28 November 2017 | Rheumatologist | 49 | F | Yes |
| 2 | 5 December 2017 | Patient | 51 | F | No |
| 3 | 31 January 2018 | Patient | 58 | F | No |
| 4 | 8 February 2018 | Patient | 81 | F | No |
| 5 | 8 February 2018 | General practitioner | 70 | F | No |
| 6 | 22 February 2018 | Rheumatologist | 69 | M | Yes |
| 7 | 7 March 2018 | Digital health developer | 47 | F | N/A |
| 8 | 8 March 2018 | Rheumatologist | 45 | F | Yes |
| 9 | 23 March 2018 | Rheumatologist | 47 | M | Yes |
| 10 | 28 March 2018 | Digital health developer | 51 | F | N/A |
| 11 | 9 April 2018 | General Practitioner | 43 | F | Yes |
| 12 | 19 April 2018 | Digital health developer | 50 | F | N/A |
| 13 | 23 April 2018 | Patient | 76 | F | No |
| 14 | 23 April 2018 | Rheumatologist | 52 | F | No |
| 15 | 15 November 2018 | General practitioner | 37 | M | Yes |
| 16 | 21 February 2019 | Statutory health insurance representative | 45 | F | N/A |
| 17 | 18 March 2019 | Digital health developer | 30 | M | N/A |
| 18 | 9 May 2019 | Patient | 52 | F | Yes |
| 19 | 9 May 2019 | Statutory health insurance representative | 32 | F | N/A |
| 20 | 27 June 2019 | Representatives of regional association of statutory health insurance physicians | 53 | M | N/A |
| 21 | 2 July 2019 | General practitioner | 41 | M | Yes |
| 22 | 4 July 2019 | Digital health developer | 66 | M | N/A |
| 23 | 11 July 2019 | Representatives of regional association of statutory health insurance physicians | 35 | F | N/A |
| 24 | 11 July 2019 | Digital health developer | 65 | F | N/A |
| 25 | 17 July 2019 | Rheumatology assistant | 51 | F | Yes |
| 26 | 18 July 2019 | Rheumatologist | 34 | M | Yes |
| 27 | 18 July 2019 | General practitioner | 32 | F | Yes |
| Total | |
|---|---|
| “Would you like your rheumatologist to offer you telemedicine services?” | 663 |
| Yes | 139 (21.0%) |
| No | 286 (43.1%) |
| I do not know | 238 (35.9%) |
| “Would you like your rheumatologist to give you recommendations on digital services?” | 661 |
| Yes | 320 (48.4%) |
| No | 211 (31.9%) |
| I do not know | 130 (19.7%) |
| “Would you be willing to pay privately for telemedicine services?” | 675 |
| Yes | 25 (3.7%) |
| No | 518 (76.7%) |
| I do not know | 132 (19.6%) |
| “Do you document your health status?” | 662 |
| Yes, via paper | 158 (23.9%) |
| Yes, digitally | 59 (8.8%) |
| No | 445 (67.2%) |
| Opportunities | Barriers | ||
|---|---|---|---|
| Qualitative Interviews | Patient |
|
|
| Professional Stakeholder |
|
| |
| Survey Data | Patient |
|
|
| Focus Groups | Patient |
|
|
| Physician |
|
| |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muehlensiepen, F.; Knitza, J.; Marquardt, W.; May, S.; Krusche, M.; Hueber, A.; Schwarz, J.; Vuillerme, N.; Heinze, M.; Welcker, M. Opportunities and Barriers of Telemedicine in Rheumatology: A Participatory, Mixed-Methods Study. Int. J. Environ. Res. Public Health 2021, 18, 13127. https://doi.org/10.3390/ijerph182413127
Muehlensiepen F, Knitza J, Marquardt W, May S, Krusche M, Hueber A, Schwarz J, Vuillerme N, Heinze M, Welcker M. Opportunities and Barriers of Telemedicine in Rheumatology: A Participatory, Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2021; 18(24):13127. https://doi.org/10.3390/ijerph182413127
Chicago/Turabian StyleMuehlensiepen, Felix, Johannes Knitza, Wenke Marquardt, Susann May, Martin Krusche, Axel Hueber, Julian Schwarz, Nicolas Vuillerme, Martin Heinze, and Martin Welcker. 2021. "Opportunities and Barriers of Telemedicine in Rheumatology: A Participatory, Mixed-Methods Study" International Journal of Environmental Research and Public Health 18, no. 24: 13127. https://doi.org/10.3390/ijerph182413127
APA StyleMuehlensiepen, F., Knitza, J., Marquardt, W., May, S., Krusche, M., Hueber, A., Schwarz, J., Vuillerme, N., Heinze, M., & Welcker, M. (2021). Opportunities and Barriers of Telemedicine in Rheumatology: A Participatory, Mixed-Methods Study. International Journal of Environmental Research and Public Health, 18(24), 13127. https://doi.org/10.3390/ijerph182413127






