Validity and Reliability of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Determination of Key Barriers in East-Central Europe
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Procedure
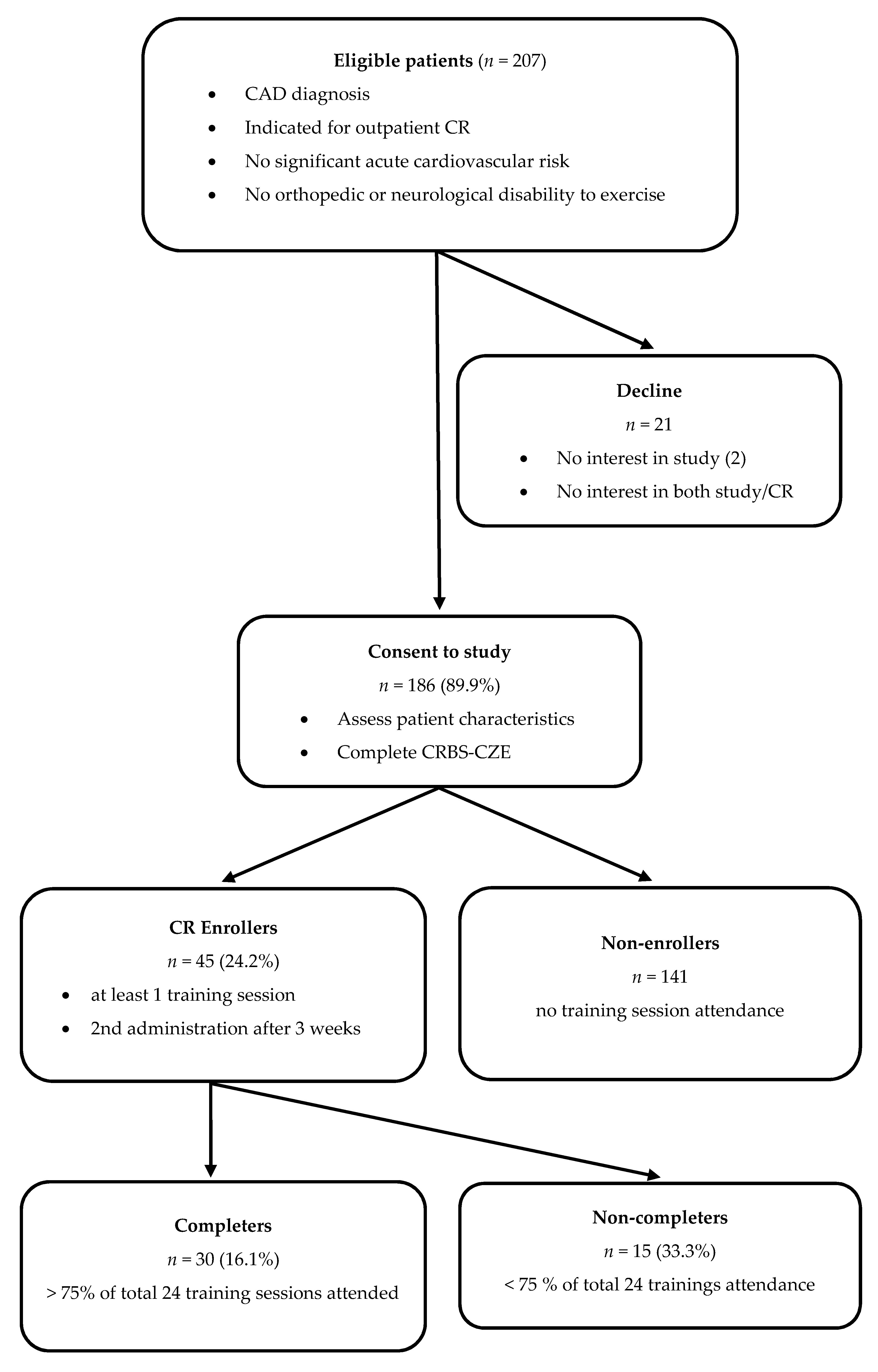
2.4. Participants
2.5. Measures
2.6. Analysis
3. Results
3.1. Factor Structure and Reliability
3.2. Criterion and Construct Validity
3.3. Repeat Administration of the CRBS-CZE
3.4. Greatest Barriers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases Country Profiles. 2018. Available online: https://www.who.int/nmh/publications/ncd-profiles-2018/en/ (accessed on 30 January 2021).
- Ústav Zdravotnických Informací a Statistiky ČR. Zdravotnická Ročenka České Republiky. 2018. Available online: https://www.uzis.cz/res/f/008280/zdrroccz-2018.pdf (accessed on 30 January 2021).
- Český Statistický Úřad. Výsledky Zdravotnických Účtů ČR 2010–2018. Available online: https://www.czso.cz/documents/10180/122362658/26000520.pdf/ce8cd21a-9317-4b04-8e5d-441be5ea0c8b?version=1.1 (accessed on 30 January 2021).
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 30 January 2021).
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease Cochrane Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandercock, G.R.H.; Cardoso, F.; Almodhy, M.; Pepera, G. Cardiorespiratory fitness changes in patients receiving comprehensive outpatient cardiac rehabilitation in the UK: A multicentre study. Heart 2013, 99, 785–790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ji, H.; Fang, L.; Yuan, L.; Zhang, Q. Effects of Exercise-Based Cardiac Rehabilitation in Patients with Acute Coronary Syndrome: A Meta-Analysis. Med. Sci. Monit. 2019, 25, 5015–5027. [Google Scholar] [CrossRef] [PubMed]
- Babu, A.S.; Lopez-Jimenez, F.; Thomas, R.J.; Isaranuwatchai, W.; Herdy, A.H.; Hoch, J.S.; Grace, S.L. Advocacy for Outpatient Cardiac Rehabilitation Globally. BMC Health Serv. Res. 2016, 16, 471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neubeck, L.; Freedman, S.B.; Clark, A.M.; Briffa, T.; Bauman, A.; Redfern, J. Participating in Cardiac Rehabilitation: A Systematic Review and Meta-synthesis of Qualitative Data. Eur. J. Prev. Cardiol. 2012, 19, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.M.; King-Shier, K.M.; Thompson, D.R.; Spaling, M.A.; Duncan, A.S.; Stone, J.A.; Jaglal, S.B.; Angus, J.E. A Qualitative Systematic Review of Influences on Attendance at Cardiac Rehabilitation Programs After Referral. Am. Heart J. 2012, 164, 835–845. [Google Scholar] [CrossRef] [PubMed]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, Use, and Barriers to Cardiac Rehabilitation in LMIC. Glob. Heart. 2017, 12, 323–334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oosenbrug, E.; Marinho, R.P.; Zhang, J.; Marzolini, S.; Colella, T.J.F.; Pakosh, M.; Grace, S.L. Sex Differences in Cardiac Rehabilitation Adherence: A Meta-analysis. Can. J. Cardiol. 2016, 32, 1316–1324. [Google Scholar] [CrossRef] [PubMed]
- Doll, J.A.; Hellkamp, A.; Ho, P.M.; Kontos, M.C.; Whooley, M.A.; Peterson, E.D.; Wang, T.Y. Participation in Cardiac Rehabilitation Programs Among Older Patients After Acute Myocardial Infarction. JAMA Intern. Med. 2015, 175, 1700–1702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruano-Ravina, A.; Pena-Gil, C.; Abu-Assi, E.; Raposeiras, S.; van’t Hof, A.; Meindersma, E.; Prescott, E.I.B.; González-Juanatey, J.R. Participation and Adherence to Cardiac Rehabilitation Programs. A systematic review. Int. J. Cardiol. 2016, 223, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.M.; King-Shier, K.M.; Duncan, A.; Spaling, M.; Stone, J.A.; Jaglal, S.; Angus, J. Factors Influencing Referral to Cardiac Rehabilitation and Secondary Prevention Programs: A Systematic Review. Eur. J. Prev. Cardiol. 2013, 20, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Witvrouwen, I.; Van Craenenbroeck, E.M.; Abreu, A.; Moholdt, T.; Kränkel, N. Exercise Training in Women with Cardiovascular Disease: Differential Response and Barriers—Review and Perspective. Eur. J. Prev. Cardiol. 2019, 28, 779–790. [Google Scholar] [CrossRef] [PubMed]
- Winnige, P.; Batalik, L.; Filakova, K.; Hnatiak, J.; Dosbaba, F.; Grace, S.L. Translation and Validation of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Protocol to Determine the Key Barriers in East-Central Europe. Medicine 2020, 99, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Shanmugasegaram, S.; Gagliese, L.; Oh, P.; Stewart, D.E.; Brister, S.J.; Chan, V.; Grace, S.L. Psychometric Validation of the Cardiac Rehabilitation Barriers Scale. Clin. Rehabil. 2012, 26, 152–164. [Google Scholar] [CrossRef] [Green Version]
- Mezzani, A.; Hamm, L.F.; Jones, A.M.; McBride, P.E.; Moholdt, T.; Stone, J.A.; Urhausen, A.; Williams, M.A. Aerobic Exercise Intensity Assessment and Prescription in Cardiac Rehabilitation: A Joint Position Statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation and the Canadian Association of Cardiac Rehabilitation. Eur. J. Prev. Cardiol. 2013, 20, 442–467. [Google Scholar]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. ESC Scientific Document Group. 2016 European Guidelines on Cardiovascular Disease Prevention in Clinical Practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the Special Contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar]
- Heart Foundation. A Pathway to Cardiac Recovery Standardised Program Content for Phase II Cardiac Rehabilitation. Available online: https://globalcardiacrehab.com/resources/Documents/CardRehabModules_COMBINED_FINAL.pdf (accessed on 5 December 2021).
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The Role of Cardiac Rehabilitation in Improving Cardiovascular Outcomes. Nat. Rev. Cardiol. 2021. [Google Scholar] [CrossRef]
- Hatcher, L. A Step-by-Step Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling; SAS Institute Inc.: Cary, NC, USA, 1994. [Google Scholar]
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Medina-Inojosa, J.R.; Grace, S.L.; Supervia, M.; Stokin, G.; Bonikowske, A.; Thomas, R.; Lopez-Jimenez, F. Dose of Cardiac Rehabilitation Reduces Mortality and Morbidity: A Population-based Study. JAHA 2021, 10, e021356. [Google Scholar] [CrossRef] [PubMed]
- Chai, L.S.; Siop, S.; Putit, Z.; Lim, L.; Gunggu, A.; Tie, S.F. Translation, Adaptation and Validation of the Malay Version of the Cardiac Rehabilitation Barriers Scale. J. Nurs. Res. 2020, 28, e64. [Google Scholar] [CrossRef]
- Ghisi, G.L.M.; Santo, R.Z.; Schveitzer, V.; Barros, A.L.; Recchia, T.L.; Oh, P.; Benetti, M.; Grace, S.L. Development and Validation of the Brazilian Portuguese Version of the Cardiac Rehabilitation Barriers Scale. Arq. Bras. Cardiol. 2012, 98, 344–352. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Fowokan, A.; Grace, S.L.; Ding, B.; Meng, S.; Chen, X.; Xia, Y.; Zhang, Y. Translation, Cross-Cultural Adaptation, and Psychometric Validation of the Chinese/Mandarin Cardiac Rehabilitation Barriers Scale (CRBS-C/M). Rehabil. Res. Pract. 2021, 9, 1–14. [Google Scholar] [CrossRef]
- Ghanbari, M.; Mirzaei, M.; Vafaii Nasab, M.; Grace, S.L.; Okati-Aliabad, H.; Madadizadeh, F.; Dadras, H.; Amrolahi, N.; Entezari, M.; Sadrbafghi, S.M. Cross-cultural Adaptation and Psychometric Validation of the Persian version of the Cardiac Rehabilitation Barriers Scale (CRBS-P). BMJ Open 2020, 10, e034552. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.; Park, H.W.; Lee, Y.; Grace, S.L.; Kim, W.S. Translation, Cross-cultural Adaptation and Psychometric Validation of the Korean-Language Cardiac Rehabilitation Barriers Scale (CRBS-K). BMJ Open 2017, 10, 858–867. [Google Scholar]
- Jácome Hortúa, A.M.; Angarita-Fonseca, A.; Villamizar Jaimes, C.J.; Martínez Marín, R.d.P.; Dutra de Souza, H.C.; de Paula Facioli, T.; Sánchez-Delgado, J.C. Reliability of the Scale of Barriers for Cardiac Rehabilitation in the Colombian Population. Int. J. Environ. Res. Public Health 2021, 18, 4351. [Google Scholar] [CrossRef]
- Grace, S.L.; Gravely-Witte, S.; Kayaniyil, S.; Brual, J.; Suskin, N.; Stewart, D.E. A Multisite Examination of Sex Differences in Cardiac Rehabilitation Barriers by Participation Status. J. Womens Health 2009, 18, 209–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Movsisyan, N.K.; Vinciguerra, M.; Lopez-Jimenez, F.; Kunzova, S.; Homolka, M.; Jaresova, J.; Cífková, R.; Sochor, O. Kardiovize Brno 2030, A Prospective Cardiovascular Health Study in Central Europe: Methods, Baseline Findings and Future Directions. Eur. J. Prev. Cardiol. 2018, 25, 54–64. [Google Scholar] [CrossRef] [Green Version]
- Pesah, E.; Supervia, M.; Turk-Adawi, K.; Grace, S.L. A Review of Cardiac Rehabilitation Delivery Around the World. Prog. Cardiovasc. Dis. 2017, 60, 267–280. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Supervia, M.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.S.; et al. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine 2019, 13, 31–45. [Google Scholar] [CrossRef] [Green Version]
- Brual, J.; Gravely-Witte, S.; Suskin, N.; Stewart, D.E.; Macpherson, A.; Grace, S.L. Drive Time to Cardiac Rehabilitation: At What Point Does it Affect Utilization? Int. J. Health Geogr. 2010, 9, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Ades, P.A.; Waldmann, M.L.; McCann, W.J.; Weaver, S.O. Predictors of Cardiac Rehabilitation Participation in Older Coronary Patients. Arch. Intern. Med. 1992, 152, 1033–1035. [Google Scholar] [CrossRef]
- Bäck, M.; Caldenius, V.; Svensson, L.; Lundberg, M. Perceptions of Kinesiophobia in Relation to Physical Activity and Exercise After Myocardial Infarction: A Qualitative Study. Phys. Ther. 2020, 100, 2110–2119. [Google Scholar] [CrossRef]
- Grace, S.L.; Kotseva, K.; Whooley, M.A. Cardiac Rehabilitation: Under-utilized Globally. Curr. Cardiol. Rep. 2021, 23. [Google Scholar] [CrossRef] [PubMed]
- Shanmugasegaram, S.; Oh, P.; Reid, R.D.; McCumber, T.; Grace, S.L. A Comparison of Barriers to Use of Home- versus Site-based Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2013, 33, 297–302. [Google Scholar] [CrossRef]
- Bakhshayeh, S.; Sarbaz, M.; Kimiafar, K.; Vakilian, F.; Eslami, S. Barriers to Participation in Center-based Cardiac Rehabilitation Programs and Patients’ Attitudes Toward Home-based Cardiac Rehabilitation Programs. Physiother. Theory Pract. 2021, 37, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Dalal, H.; Jolly, K.; Zawada, A.; Dean, S.G.; Cowie, A.; Norton, R.J. Home-based vs. centre-based cardiac rehabilitation. Cochrane Database Syst. Rev. 2015, 18. [Google Scholar]
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, 69–89. [Google Scholar] [CrossRef] [PubMed]
- Batalik, L.; Dosbaba, F.; Hartman, M.; Batalikova, K.; Spinar, J. Benefits and Effectiveness of Using a Wrist Heart Rate Monitor as a Telerehabilitation Device in Cardiac Patients: A Randomized Controlled Trial. Medicine 2020, 99, e19556. [Google Scholar] [CrossRef]
- Batalik, L.; Dosbaba, F.; Hartman, M.; Konecny, V.; Batalikova, K.; Spinar, J. Long-term exercise effects after cardiac telerehabilitation in patients with coronary artery disease: 1-year follow-up results of the randomized study. Eur. J. Phys. Rehabil. Med. 2021, 57, 807–814. [Google Scholar] [CrossRef]
- Batalik, L.; Pepera, G.; Papathanasiou, J.; Rutkowski, S.; Líška, D.; Batalikova, K.; Hartman, M.; Felšőci, M.; Dosbaba, F. Is the Training Intensity in Phase Two Cardiovascular Rehabilitation Different in Telehealth versus Outpatient Rehabilitation? J. Clin. Med. 2021, 10, 4069. [Google Scholar] [CrossRef]
- Besnier, F.; Gayda, M.; Nigam, A.; Juneau, M.; Bherer, L. Cardiac Rehabilitation During Quarantine in COVID-19 Pandemic: Challenges for Center-Based Programs. Arch. Phys. Med. Rehabil. 2020, 101, 1835–1838. [Google Scholar] [CrossRef] [PubMed]
- Scherrenberg, M.; Wilhelm, M.; Hansen, D.; Völler, H.; Cornelissen, V.; Frederix, I.; Kemps, H.; Dendale, P. The Future is Now: A Call for Action for Cardiac Telerehabilitation in the COVID-19 Pandemic from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020, 28, 524–540. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Mean (SD) or Frequency (%) | Mean Total CRBS Score (SD) by Characteristic † | t/r | p | |
|---|---|---|---|---|---|
| Sociodemographic | |||||
| Age (mean ± SD) | 59.5 ± 8.8 | NA | 0.02 | 0.718 | |
| Sex (n, % female) | 45 (24.1) | 1.86 (0.42) | 1.84 (0.49) | 0.25 | 0.795 |
| Marital status ∥ (n, % married) | 155 (83.3) | 1.89 (0.48) | 1.82 (0.42) | 0.73 | 0.462 |
| Educational attainment ∥ (n, % > high school) | 34 (18.2) | 1.69 (0.42) | 1.91 (0.48) | 2.51 | 0.012 |
| Work status ∥ (n, % employed) | 125 (67.2) | 1.84 (0.48) | 1.88 (0.46) | 0.55 | 0.582 |
| Individual income ∥ (n, % > 33,697 CZK/month) | 41 (22.0) | 1.72 (0.45) | 1.90 (0.47) | 2.13 | 0.047 |
| Rurality ∥ (n, % > 30 min commute time to CR one-way by usual mode) | 109 (58.6) | 2.11 (0.44) | 1.58 (0.39) | 8.44 | <0.001 |
| Clinical | |||||
| Referral indication of CAD ° (n, % yes) | 77 (41.3) | 1.92 (0.53) | 1.84 (0.42) | 1.17 | 0.240 |
| Post-acute myocardial infarction (n, % yes) | 99 (53.2) | 1.96 (0.49) | 1.78 (1.20) | 2.53 | 0.012 |
| Angina pectoris (n, % yes) | 22 (11.8) | 1.81 (0.46) | 1.88 (0.47) | 0.63 | 0.526 |
| Current/previous PCI (n, % yes) | 159 (85.4) | 1.93 (0.48) | 1.90 (0.60) | 0.20 | 0.838 |
| Current/previous CABG (n, % yes) | 6 (3.2) | NR | |||
| Current/previous HF (n, % yes) | 3 (1.6) | NR | |||
| Current/previous arrhythmia (n, % yes) | 15 (8.1) | NR | |||
| Current/previous valve issue (n, % yes) | 6 (3.2) | NR | |||
| Risk factors | |||||
| BMI (mean ± SD) | 29.5 ± 4.6 | NA | −0.01 | 0.860 | |
| Waist circumference (mean ± SD) | 106 ± 12 | NA | −0.02 | 0.734 | |
| Family history of CAD ∥ (n, % yes) | 119 (63.9) | 1.75 (0.39) | 2.06 (0.55) | 4.36 | <0.001 |
| Hypertension ∥ (n, % yes) | 117 (62.9) | 1.83 (0.43) | 1.95 (0.53) | 1.63 | 0.104 |
| Dyslipidemia ∥ (n, % yes) | 112 (60.2) | 1.79 (0.45) | 1.99 (0.48) | 2.92 | 0.003 |
| Diabetes ∥ (n, % yes) | 43 (23.1) | 1.83 (0.40) | 1.88 (0.49) | 0.61 | 0.539 |
| Heart-healthy behaviors | |||||
| Physical activity ∥ (n, % inactive §) | 88 (47.3) | 1.90 (0.49) | 1.84 (0.45) | 0.87 | 0.383 |
| Tobacco use ∥ (n, % current) | 72 (38.7) | 1.97 (0.47) | 1.81 (0.47) | 2.36 | 0.019 |
| Use of alcohol ∥ (n, % harmful ‡) | 32 (17.2) | 2.11 (0.52) | 1.83 (0.46) | 3.10 | 0.002 |
| Psychosocial well-being | |||||
| Stress ∥ (VAS, 1–10; mean ± SD) | 4.1 ± 2.4 | NA | −0.11 | 0.111 | |
| Depression and/or anxiety (n, % yes, diag./self-report ∥) | 13 (6.9)/21 (11.2) | NR/1.77 (0.44) | NR/1.88 (0.48) | 1.05 | 0.293 |
| CR utilization | |||||
| Enrollment (n, % yes) | 45 (24.2) | 1.61 (0.46) | 1.96 (0.44) | 4.65 | <0.001 |
| Adherence (mean % of sessions completed ± SD) | 70.8 ± 29.8% | NA | −0.51 | <0.001 | |
| Completion (n, % yes) | 30 (16.1) | 1.41 (0.36) | 1.99 (0.45) | 6.70 | <0.001 |
| 1st Administration (pre-CR) (n = 186) | 2nd Administration (during CR) (n = 42) | Mean Change ± SD § | Paired t-Test Value for Change § | |||||
|---|---|---|---|---|---|---|---|---|
| CRBS Item | Mean Score | SD | Not Applicable n (%) | Mean Score | SD | Not Applicable n (%) | ||
| 01 … of distance | 3.08 | 1.70 | 7 (3.8%) | 1.71 | 1.33 | 0 | −0.36 ± 0.90 | 2.23 * |
| 02 … of cost | 1.97 | 1.19 | 8 (4.3%) | 1.32 | 0.71 | 1 (2.4%) | −0.22 ± 0.82 | 1.69 |
| 03 … of transportation problems | 2.17 | 1.47 | 6 (3.2%) | 1.12 | 0.39 | 1 (2.4%) | −0.27 ± 0.58 | 2.88 * |
| 04 … of family responsibilities | 1.88 | 1.24 | 2 (1.1%) | 1.29 | 0.59 | 0 | −0.40 ± 0.82 | 3.07 * |
| 05 … I didn’t know about CR | 1.49 | 0.92 | 15 (8.1%) | 1.00 | 0.00 | 0 | −0.38 ± 0.78 | 3.07 * |
| 06 … I don’t need CR | 1.91 | 1.12 | 26 (14%) | 1.29 | 0.90 | 4 (9.5%) | −0.07 ± 0.95 | 0.48 |
| 07 … I already exercise at home or in my community | 1.99 | 1.41 | 9 (4.8%) | 1.41 | 1.09 | 1 (2.4%) | −0.14 ± 0.59 | 1.45 |
| 08 … of severe weather | 1.79 | 0.83 | 108 (58.1%) † | 1.20 | 0.63 | 1 (2.4%) | −0.05 ± 0.74 | 0.41 |
| 09 … I find exercise tiring or painful | 1.62 | 0.92 | 10 (5.4%) | 1.32 | 0.77 | 1 (2.4%) | −0.29 ± 0.96 | 1.92 |
| 10 … of travel | 1.96 | 1.29 | 11 (5.9%) | 1.80 | 0.96 | 2 (4.8%) | −0.10 ± 1.08 | 0.59 |
| 11 … of time constraints | 2.37 | 1.55 | 6 (3.2%) | 1.50 | 0.87 | 2 (4.8%) | −0.35 ± 1.11 | 2.00 * |
| 12 … of work responsibilities | 2.78 | 1.39 | 42 (22.6%) | 1.63 | 1.13 | 2 (4.8%) | −0.52 ± 1.13 | 2.88 * |
| 13 … I don’t have the energy | 1.79 | 0.96 | 10 (5.4%) | 1.17 | 0.53 | 1 (2.4%) | −0.34 ± 0.83 | 2.56 * |
| 14 … other health problems prevent me from going | 2.13 | 1.13 | 65 (34.9%) | 1.59 | 1.13 | 2 (4.8%) | −0.05 ± 1.37 | 0.25 |
| 15 … I am too old | 1.40 | 0.73 | 21 (11.3%) | 1.03 | 0.15 | 4 (9.5%) | −0.22 ± 0.58 | 2.33 * |
| 16 … my doctor did not feel it was necessary | 1.20 | 0.34 | 140 (75.3%) † | 1.09 | 0.30 | 19 (45.2%) † | −0.13 ± 0.75 | 1.08 |
| 17 … many people with heart problems don’t go, and they are fine | 1.67 | 0.98 | 65 (34.9%) | 1.24 | 0.41 | 25 (59.5%) † | −0.40 ± 0.84 | 2.22 * |
| 18 … I can manage on my own | 1.90 | 1.10 | 51 (27.4%) | 1.37 | 0.88 | 15 (35.7%) | −0.13 ± 1.16 | 0.71 |
| 19 … I think I was referred but the rehab program didn’t contact me | 1.29 | 0.19 | 172 (92.5%) † | 1.00 | 0.00 | 0 | −0.33 ± 0.40 | 4.97 ** |
| 20 … it took too long to get referred and into the program | 1.38 | 0.81 | 31 (16.7%) | 1.24 | 0.61 | 21 (50.0%) † | −0.25 ± 0.78 | 2.00 * |
| 21 … I prefer to take care of my health alone | 1.54 | 1.03 | 31 (16.7%) | 1.32 | 0.90 | 5 (11.9%) | −0.56 ± 0.94 | 3.64 ** |
| CRBS-CZE Item | Perceived Need § | Logistical Factors † | Work/Time Conflicts ‡ | Comorbidities/Health System Factors ∥ |
|---|---|---|---|---|
| 17 … many people with heart problems don’t go, and they are fine | 0.71 § | 0.08 | −0.12 | −0.02 |
| 07 … I already exercise at home or in my community | 0.69 § | 0.24 | 0.31 | −0.03 |
| 06 … I don’t need cardiac rehab | 0.65 § | 0.08 | 0.26 | 0.23 |
| 21 … I prefer to take care of my health alone | 0.60 § | −0.04 | 0.06 | 0.06 |
| 18 … I can manage on my own | 0.42 § | 0.22 | 0.18 | 0.06 |
| 03 … of transportation problems | −0.04 | 0.82 † | −0.02 | 0.09 |
| 01 … of distance | 0.07 | 0.78 † | 0.05 | 0.10 |
| 02 … of cost | 0.17 | 0.65 † | 0.20 | 0.11 |
| 08 … of severe weather | 0.11 | 0.59 † | 0.18 | −0.11 |
| 05 … I didn’t know about cardiac rehab | 0.04 | 0.21 † | 0.17 | −0.03 |
| 11 … of time constraints | 0.28 | 0.17 | 0.73 ‡ | −0.15 |
| 12 … of work responsibilities | 0.13 | 0.17 | 0.66 ‡ | −0.22 |
| 10 … of travel | 0.06 | 0.03 | 0.56 ‡ | 0.07 |
| 13 … I don’t have the energy | −0.23 | 0.03 | 0.53 ‡ | 0.37 |
| 04 … of family responsibilities | 0.19 | 0.18 | 0.48 ‡ | 0.06 |
| 14 … other health problems prevent me from going | 0.08 | 0.19 | 0.05 | 0.57 ∥ |
| 16 … my doctor did not feel it was necessary | 0.37 | 0.14 | 0.02 | 0.51 ∥ |
| 19 … I think I was referred but the rehab program didn’t contact me | 0.35 | −0.13 | −0.11 | 0.51 ∥ |
| 20 … it took too long to get referred and into the program | 0.19 | −0.02 | −0.13 | 0.44 ∥ |
| 09 … I find exercise tiring or painful | −0.21 | 0.08 | 0.40 | 0.41 ∥ |
| 15 … I am too old | 0.09 | 0.26 | 0.23 | 0.38 ∥ |
| Variance explained | 18.85% | 9.22% | 7.64% | 7.15% |
| Eigenvalues | 3.96 | 1.94 | 1.60 | 1.50 |
| Reliability | 0.64 | 0.69 | 0.72 | 0.44 |
| Perceived Need | Logistical | Work/Time Conflicts | Comorbidities/Health System Factors | |
|---|---|---|---|---|
| Education | ||||
| University Education (n = 34) | 1.65 (0.56) | 1.62 (0.57) | 1.95 (0.62) | 1.43 (0.31) |
| No university (n = 152) | 1.76 (0.54) | 2.05 (0.68) ** | 2.10 (0.77) | 1.63 (0.39) * |
| Income | ||||
| Higher income (n = 41) | 1.72 (0.57) | 1.61 (0.57) | 2.00 (0.70) | 1.47 (0.28) |
| Lower income (n = 145) | 1.79 (0.55) | 1.96 (0.61) * | 2.17 (0.80) | 1.63 (0.40) * |
| Rurality | ||||
| Urban (n = 77) | 1.55 (0.51) | 1.48 (0.44) | 1.79 (0.63) | 1.47 (0.37) |
| Rural (n = 109) | 1.91 (0.55) ** | 2.34 (0.63) ** | 2.29 (0.76) ** | 1.73 (0.37) ** |
| AMI | ||||
| Post-AMI (n = 99) | 1.84 (0.57) | 2.06 (0.71) | 2.16 (0.76) | 1.59 (0.34) |
| No AMI (n = 87) | 1.67 (0.51) * | 1.86 (0.62) * | 1.99 (0.73) | 1.60 (0.42) |
| Family history of CAD | ||||
| Yes (n = 119) | 1.59 (0.44) | 1.84 (0.56) | 1.95 (0.66) | 1.48 (0.33) |
| No (n = 87) | 1.96 (0.65) ** | 2.20 (0.81) ** | 2.30 (0.84) * | 1.76 (0.43) ** |
| Dyslipidemia | ||||
| Yes (n = 112) | 1.70 (0.56) | 1.82 (0.60) | 2.02 (0.75) | 1.54 (0.41) |
| No (n = 74) | 1.80 (0.52) | 2.21 (0.73) ** | 2.18 (0.74) | 1.67 (0.33) * |
| Use of tobacco | ||||
| Smokers (n = 72) | 1.77 (0.50) | 2.14 (0.74) | 2.20 (0.73) | 1.64 (0.33) |
| Non/former smokers (n = 114) | 1.72 (0.58) | 1.87 (0.62) * | 2.01 (0.75) | 1.56 (0.40) |
| Use of alcohol | ||||
| No harmful use (n = 154) | 1.68 (0.52) | 1.96 (0.68) | 2.03 (0.72) | 1.55 (0.37) |
| Harmful use (n = 32) | 1.91 (0.45) * | 2.45 (0.89) ** | 2.34 (0.68) * | 1.86 (0.44) ** |
| Enrollment | ||||
| CR Enrollees (n = 45) | 1.57 (0.59) | 1.53 (0.55) | 1.70 (0.58) | 1.45 (0.41) |
| Non-enrollees (n = 141) | 1.76 (0.52) * | 2.16 (0.66) ** | 2.21 (0.76) ** | 1.60 (0.36) * |
| Completion | ||||
| CR Completers (n = 30) | 1.28 (0.35) | 1.30 (0.38) | 1.53 (0.51) | 1.31 (0.33) |
| Non-completers (n = 136) | 1.86 (0.55) ** | 2.13 (0.65) ** | 2.19 (0.74) ** | 1.69 (0.37) ** |
| 1st Administration | 2nd Administration | |||
|---|---|---|---|---|
| Total (n = 42) | Completers (n = 30) | Non-Completers (n = 12) | ||
| Total | 1.58 (0.47) | 1.32 (0.29) * | 1.19 (0.15) | 1.63 (0.39) †† |
| Perceived need | 1.54 (0.60) | 1.27 (0.42) * | 1.12 (0.15) | 1.67 (0.76) †† |
| Logistical | 1.49 (0.55) | 1.27 (0.37) * | 1.12 (0.15) | 1.63 (0.51) †† |
| Work/time conflicts | 1.69 (0.60) | 1.43 (0.44) * | 1.29 (0.31) | 1.75 (0.56) † |
| Comorbidities/health system factors | 1.42 (0.41) | 1.21 (0.27) * | 1.15 (0.17) | 1.44 (0.42) † |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Winnige, P.; Filakova, K.; Hnatiak, J.; Dosbaba, F.; Bocek, O.; Pepera, G.; Papathanasiou, J.; Batalik, L.; Grace, S.L. Validity and Reliability of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Determination of Key Barriers in East-Central Europe. Int. J. Environ. Res. Public Health 2021, 18, 13113. https://doi.org/10.3390/ijerph182413113
Winnige P, Filakova K, Hnatiak J, Dosbaba F, Bocek O, Pepera G, Papathanasiou J, Batalik L, Grace SL. Validity and Reliability of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Determination of Key Barriers in East-Central Europe. International Journal of Environmental Research and Public Health. 2021; 18(24):13113. https://doi.org/10.3390/ijerph182413113
Chicago/Turabian StyleWinnige, Petr, Katerina Filakova, Jakub Hnatiak, Filip Dosbaba, Otakar Bocek, Garyfallia Pepera, Jannis Papathanasiou, Ladislav Batalik, and Sherry L. Grace. 2021. "Validity and Reliability of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Determination of Key Barriers in East-Central Europe" International Journal of Environmental Research and Public Health 18, no. 24: 13113. https://doi.org/10.3390/ijerph182413113
APA StyleWinnige, P., Filakova, K., Hnatiak, J., Dosbaba, F., Bocek, O., Pepera, G., Papathanasiou, J., Batalik, L., & Grace, S. L. (2021). Validity and Reliability of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Determination of Key Barriers in East-Central Europe. International Journal of Environmental Research and Public Health, 18(24), 13113. https://doi.org/10.3390/ijerph182413113









