Nurse Education and Mathematical Competency: Implementation of an Online, Self-Directed, Prerequisite Model
Abstract
:1. Introduction
2. Methods
3. Results
3.1. Rationale for Change
3.2. Transition to the New DCCT Model
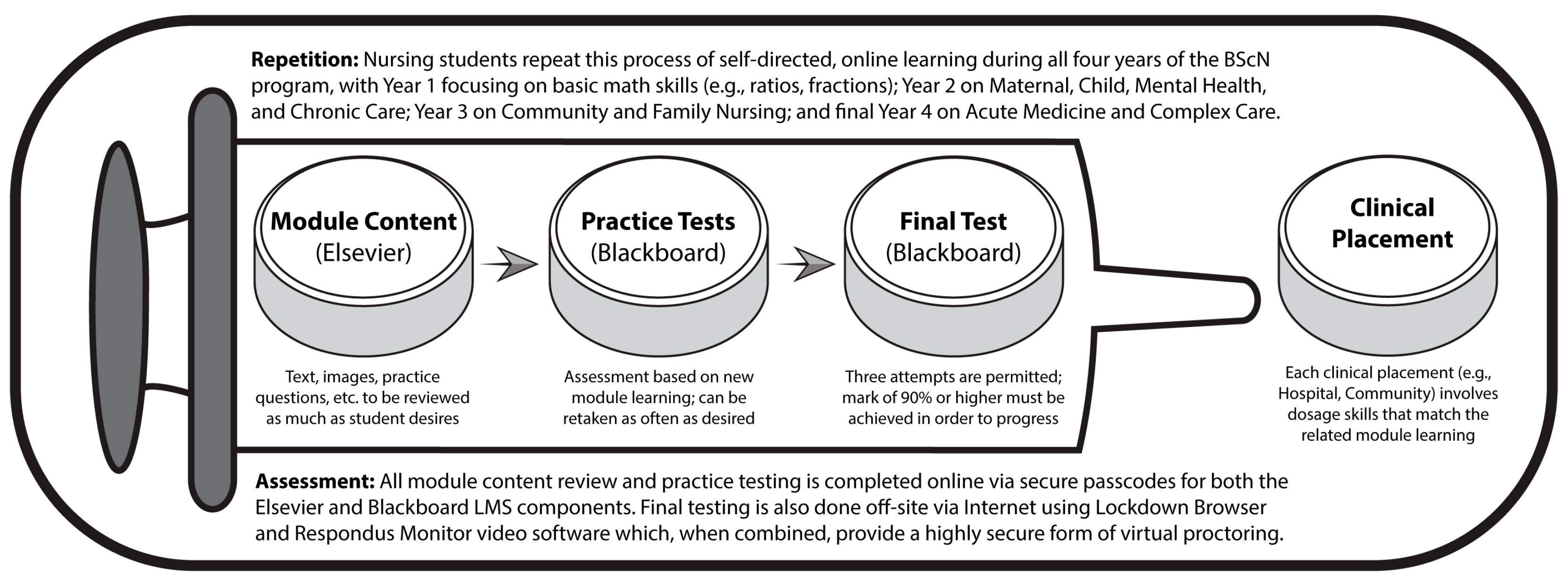
P15: That is when we began developing key spots in the program throughout the eight semesters where the math testing would be building the skills of the student, and constantly getting them to be repetitively learning and retaining the math skills right up until fourth year. Because when they graduate, they have to be able to determine what the right dosage would be to give to any patient. It’s something you learn but can then easily forget—so you have to maintain the skills throughout.
P02: I remember many faculty meetings where we spoke about the DCCT at length. We talked about what is the best way to implement this into the curriculum. Do you want to make it a stand-alone course? Will it be worth course credits?... We decided through many discussions that we would purchase this DCCT software and implement it as a stand-alone, pre-clinical requirement.
3.3. Ongoing Modifications to the DCCT Model
P03: When I left three years ago [ca. 2017], we did not have one single student who had to be withdrawn from clinical as a result of dosage calculation. We did have a few students who needed to do multiple re-writes, and so we put a remediation package together for them.... They had to go through the Elsevier program again, and all of the practice tests again, and then when I saw that they had passed those, then they would get a third attempt, and all of them passed.
P11: There’s a limitation on campus with the number of computer labs, and number of computers in each lab, and so it was very labour-intensive to have 300 students write tests on-site.... We’ve changed it so that they have the flexibility to write it when they’re ready.... and starting this academic year [2019–20], they test at home.... We use LockDown Browser as sort of the basis, then in first year, second semester they also use Respondus Monitor, a video proctoring software.
4. Discussion
4.1. Four Types of Student Learning Associated with the DCCT Model
P13: It’s really based on your time management skills as a student. This program is so time-consuming with clinical, which has the lab, as well as the other four courses. And then going to the hospital or long-term care facility as well, so it’s really hard to fit it all in.... It’s not like it’s super draining or demanding, but it’s just setting it up at the beginning of the semester to do it throughout the year, and not leaving it until the very end.
P11: I think one of the strengths is that it allows the students to take as much time as they need, and sort of adjust their studying to when it’s good for them. I’ve had students who have really, really struggled with their dosage, and who will contact me in January to start working through things, but then also students who are stronger who don’t need to take as much time, and they’ll start reviewing the modules only a few weeks before.
P12: It offers you four or five different ways to complete the same question, depending on your learning style.... It’s set up so that it presents ways to approach each of those questions with different math styles, like proportional, or dimensional, or ratio analysis. The idea is that you’re going to go through and you’re going to learn all four different ways first, and then you’re going to decide which one works best for you.
P07: I liked it when our instructors incorporated it into our labs, because we are learning the skills and so allowing you to integrate the dosage into it was very similar to simulating what you would have to do if you were to encounter that situation on a hospital floor, or when working as a nurse.
P10: I don’t think you can teach anything without context—that’s part of my own teaching philosophy. You know, you can theoretically do this stuff, but you need to use real experiences, or use case studies, which are great and safe contexts. So, I mean, you should be teaching the math skills kind of theoretically, but you have to push it into a practical context because nursing is nothing but, you know, practical knowledge.
P08: If somebody would say, “I’m really struggling with long division,” or something, then we would all start talking about that topic.... It was just whoever had already done the modules, or who understood it the best, would just explain it to everybody else, and if multiple people understood it, then they would just kind of break off into smaller groups and talk one-on-one with somebody.
P04: Yes, we would normally go get a room at the library and just study there together.... I think that group learning is probably the best way for nurses to learn. Say you have four people in a group, and you might have one person who feels super confident with the math, like they know what they’re doing; then you have another person who may be as confident, but doesn’t really know how to explain things to others; and then you’ll have one or two other people who have no idea what’s going on, and are just trying to stay above water.
4.2. Student Perceptions of Mathematical Confidence/Competency
P13: A lot of the healthcare facilities have automated dispensers, where all of the medication is pre-packaged... and they use the barcodes on patients’ wrists, and those on their medications to match up patients with the already prescribed pills. So, the nurse doesn’t really have to calculate.... With experience you’d be exposed to more and more, so you’d know the reasonable ranges without having to calculate it every time, but obviously it is still important to know how to do it.
P04: Everyone carries a cell-phone. It’s like it’s essential now to carry your cell-phone as a nurse.... If something comes up and a doctor is talking, and they say something that you’ve never heard of before, you can quickly Google it instead of looking stupid.
P06: Every nurse I’ve seen in practice has their cell-phone on them, using it for dosage calculations or to look up medications.... One of the applications that is loaded onto all of the hospital accounts is called UpToDate, where it has all of the information, like medication administration, processes, and common symptoms.
P07: I have not ever in my four years seen a nurse calculate with pencil-and-paper—I have always seen them use a calculator.... There’s a calculator at their dosage station, but for emergency situations they might have their phone in their pocket, and so they would just pull that out and use that as a calculator.
P09: Being tested yearly, it makes me feel like I’m being kept up-to-date.... I think [university] has a really good reputation for making good nurses, and it’s because of the way that we test here. It holds everybody accountable.... My friend, she hated dosage calculations—but I think, deep down, she does appreciate having to do it each year, because now she’s good at it.
4.3. Instructor Perceptions of Mathematical Confidence/Competency
P10: One is just knowing your basic math skills—so, whether or not you know two plus two equals 4, and then being able to check an answer for reasonableness. You also have a legislated responsibility to know how much of a drug should go into a patient, whether you received that from the pharmacy through a dispensing machine or prepared it yourself, and whether or not you use a calculator or not, you have a legal, ethical responsibility to know that it’s the correct drug, going to the correct patient, at the correct time.... Yes, even if you have a calculator, I mean, a human has still got to enter the numbers? So, go ahead and get your phone out, and do 25% of 37, you know, I would do that with a phone too, but I have to at least be able to go, “Yeah, I think that answer is correct because 37 is close to 40, so a quarter of that has to be just less than 10.” They should be able to know that.... And you know the bottom-line consequences, if you don’t know how much, or why, and you give someone the wrong drug, well, you’re legally responsible for that, and you could go to jail.... Human error is huge in the healthcare system.
P15: Just because a machine says it’s so, doesn’t mean it’s so. You have a 12-lead ECG, and some of those machines interpret what the findings are, but being a Critical Care Nurse and an expert in reading 12-lead ECG’s, I can tell you the ECG machine is wrong all the time.... In terms of the ADS machines, they have not always prevented medication incidents, and in fact, in some cases, they’ve created them.... You still have to open the drawer, check the med cart for what the patient is supposed to be getting at that point and time.... The meds aren’t necessarily going to be in the exact perfect dosage amounts either—they may need to be split, or you’ll have to give two instead of one, because they only come in 25 mg and you have to give 50, three times a day. If you can’t figure that out, then you’re in trouble.
P15: The new system provides an opportunity to do some self-directed learning, to really take some ownership and accountability for learning, and to be able to do it at their own pace in an environment of their choosing.... I think that this approach has reduced the anxiety overall, and gives them a repetitiveness that’s often required to retain these kinds of things.
5. Conclusions
- Focus on Calculation and Critical Thinking: Nursing practice invariably requires both mathematical and dosage calculation skills, as well as critical thinking skills such as mental estimation and the ability to check answers for reasonableness. Instructors were unanimous on this point, all indicating that nurses must possess both hand-written and technology-based dosage calculation competency.
- Focus on a Mandatory Prerequisite Structure: As opposed to a model wherein the dosage calculation component was a composite and assessed feature of clinical courses, dosage testing/competence is now also a prerequisite for each clinical admission. Instructors felt that insisting on this requirement helped students to understand the critical nature of dosage skills, and to increase their readiness.
- Focus on Practicum-Relevant Skills and Repetition: The dosage modules, involving content, practice questions, and tests, are purposefully aligned with relevant practicum placement skills, and students complete dosage modules throughout all four years. For example, Year 1 focuses on basic math skills (e.g., ratios, fractions); Year 2 on Maternal, Child, Mental Health, and Chronic Care; Year 3 on Community and Family Nursing; and final Year 4 on Acute Medicine and Complex Care. The majority of both students and instructors consistently spoke to the importance of repetition, throughout all four years, as being key to learning.
- Focus on Self-Directed, Personalized, Embedded, and Social Learning: Module learning is self-directed, personalized via selected solution methods, reinforced through demonstrations within the simulation labs, and often supported by informal peer-to-peer tutoring. The majority of participating students emphasized their appreciation of a self-directed program that allowed them to review content as many times as needed, and whenever most convenient to do so. Instructors stressed the importance of connecting the module dosage/math learning to nursing practice by way of the corresponding simulation lab experiences and were also not surprised to find students informally drawn together for purposes of review.
- Focus on Online Access and Secure Assessment: All dosage module work is completed online through secure access to the Elsevier Evolve portal and Blackboard LMS, including the final test using LockDown Browser and Respondus Monitor software. Perhaps the most important aspect of the new DCCT model, in light of current trends in online education, was the complete transition, over time, from onsite, computer lab-based assessment to secure, online, assessment practices including final tests. While both instructors and students shared initial reservations about such a transition, the majority of participants indicated that the benefits of such an approach, once established, far outweighed the previous model.
- Focus on a Designated Administrator and Student Supports: A Faculty Lead, through the designated workload, is strategically positioned to oversee the DCCT model, tracking all student progress, addressing technological/content issues, and providing student support. Instructors recounting the planning and implementation of the new DCCT model all stressed the importance of clearly establishing a recognized position in which a faculty member would feel well supported by the department, and from which they could offer student assistance.
- Focus on Cyclic and Data-Driven Program Evaluation: Ongoing review of the DCCT model is conducted through regular student surveys, student achievement data analysis, and faculty/clinical instructor input that is shared via email and at departmental meetings. All new programs or models need to be revisited and revised according to ongoing and careful review. Instructors in the study relied heavily on both formal (surveys) and informal (anecdotal) feedback from their students, and this information shared in departmental meetings, guided progress.
- Clinical Resources
- ▪
- Blackboard Learn: An Advanced LMShttps://www.blackboard.com/teaching-learning/learning-management/blackboard-learn (accessed 11 December 2021)
- ▪
- Elsevier Dosage and Solutions, Online Textbook Resourceshttps://www.elsevier.ca/ca/specialty.jsp?lid=4&sid=636 (accessed 11 December 2021)
- ▪
- Respondus Monitor & LockDown Browser: Assessment Tools for Learning Systemshttps://web.respondus.com/he/monitor/ (accessed 11 December 2021)
- ▪
- Wolters Kluwer UpToDate Clinical Decision Support Resource Softwarehttps://www.uptodate.com/home (accessed 11 December 2021)
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Survey Questions
- Q01.
- Program of Study: Please select the appropriate program identification.
- Q02.
- Current Year of Study: Please select your current year of study in the nursing program.
- Q03.
- Gender: Please indicate your gender.
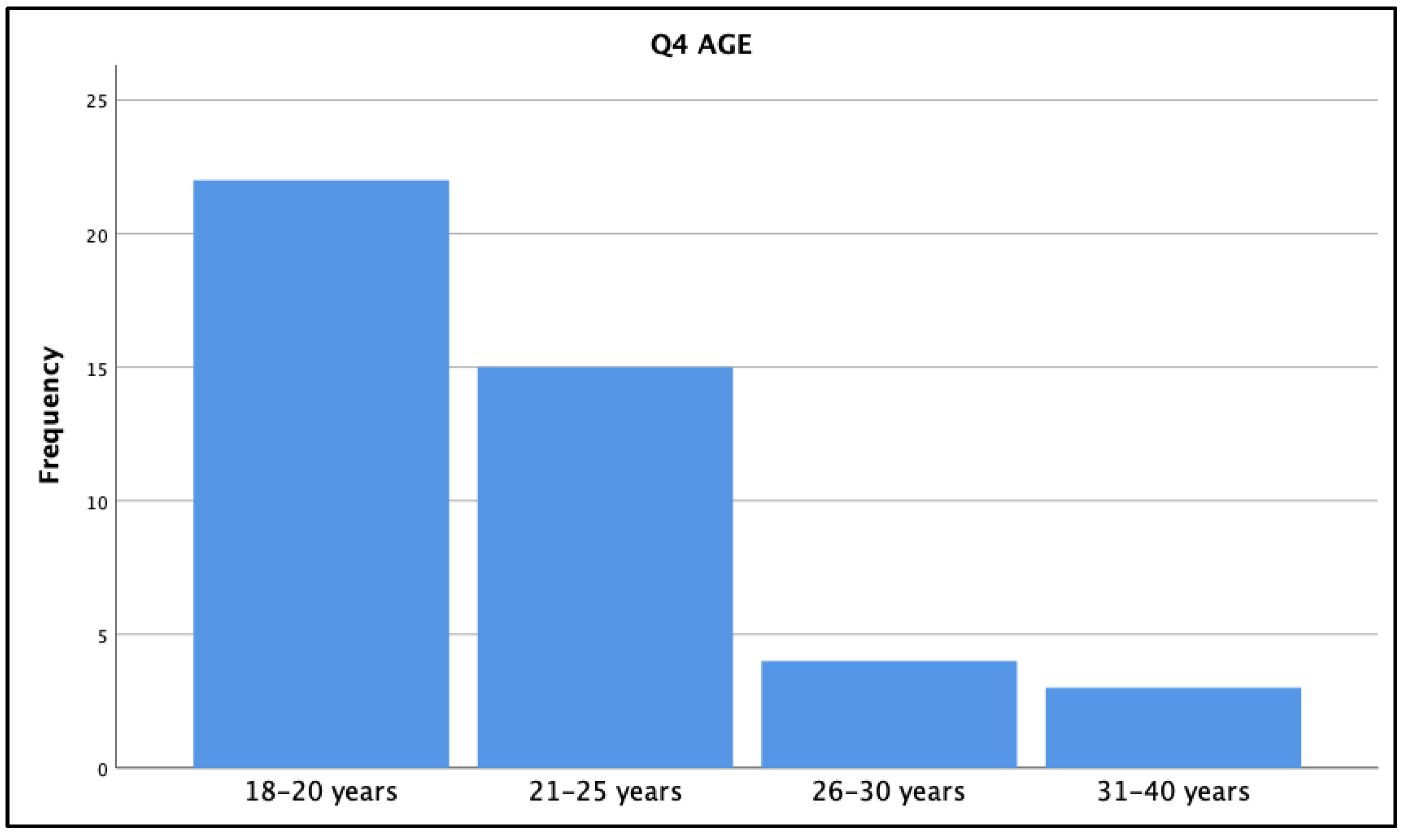
- Q04.
- Age: Please indicate your current age bracket.
- Q05.
- I encountered ‘glitches’ and problems with the purchased Elsevier online learning modules:
- Q06.
- I encountered ‘glitches’ and problems with the Blackboard component of the dosage course:
- Q07.
- I required technical assistance to maneuver through the purchased Elsevier online learning modules:
- Q08.
- I required technical assistance to maneuver through the dosage course:
- Q09.
- I have accessed additional help to understand the math content from (select all that apply):
- Q10.
- Help was readily available when I requested it from the Faculty Lead instructor:
- Q11.
- Help was readily available when I requested it from the Learning Systems Technologist:
- Q12.
- I found the independent and self-directed nature of the dosage program to be:
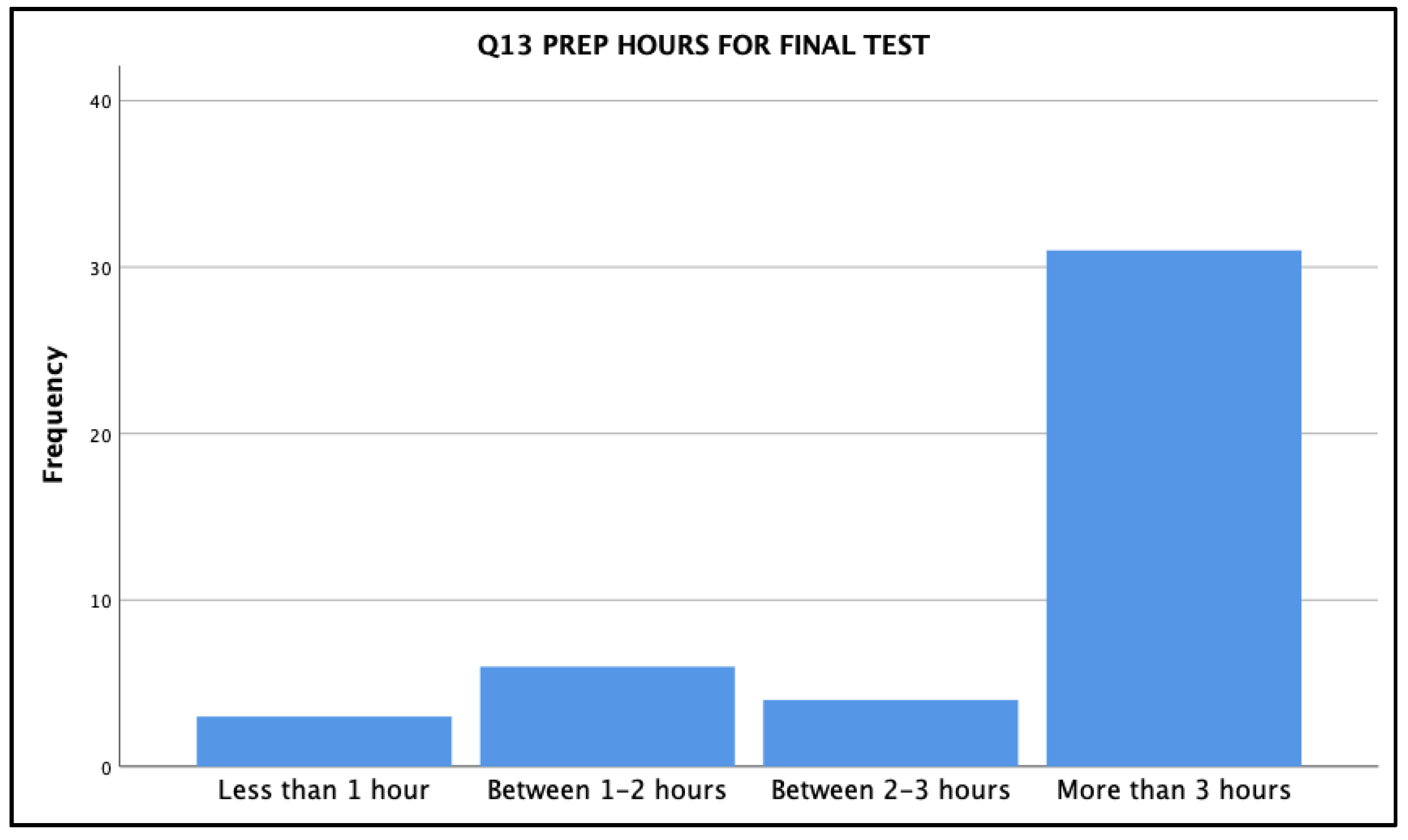
- Q13.
- On average, how many hours of studying does it take you to prepare for a DCCT final test?
- Q14.
- I found the time allotted to prepare for each module to be:
- Q15.
- I found the time allotted to write the actual DCCT test each year, in general, to be:
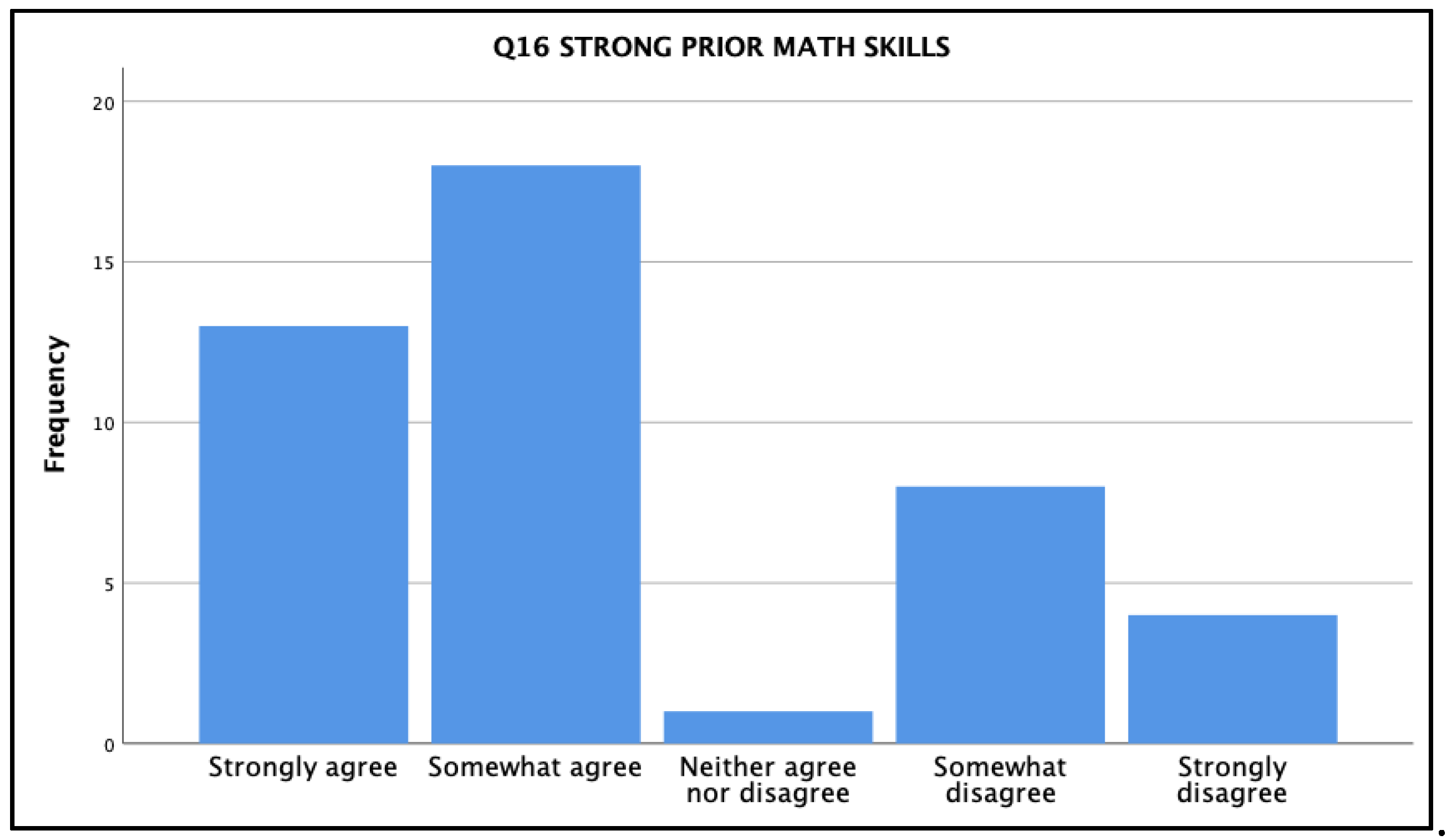
- Q16.
- Prior to starting in my nursing program, I felt I had strong mathematical skills.
- Q17.
- I believe the dosage program has helped me with my understanding of medication administration.
- Q18.
- I believe the dosage program has helped me with my overall math skill development.
- Q19.
- The Blackboard quizzes that prepared me to write the final DCCT test were:
- Q20.
- The mathematical content covered in the dosage course aligns well with the knowledge and skills that I will need in the clinical setting.
- Q21.
- I was able to use the math skills learned in the dosage program in my clinical area in a timely manner (i.e., I felt confident with my math skills in order to perform related tasks).
- Q22.
- The dosage program, in combination with my clinical courses, make me feel confident with my ability to safely give medications in the clinical setting.
- Q23.
- In your opinion, what has been the most beneficial aspect of the dosage course experience?
- Q24.
- In your opinion, what has been the most challenging aspect of the dosage course experience?
- Q25.
- Please use this open response box to share any further comments you may have about your overall experience with the dosage course material, related testing, instructor/technologist supports, etc.? Please be specific about the year or years of the program you are discussing.
Appendix B. Interview Questions
- How long have you been associated with the Nursing Program/School at Nipissing U?
- Can you please describe your recollection of how the mathematics component of the undergrad nursing program was structured in the past (if applicable), and then also how and why it was changed with the introduction of the mandatory, non-credit, self-directed DCCT program?
- What observations have you made regarding the nursing student attitudes and skills relating to the mathematics required for nursing throughout the past decade (before and after the change)?
- In the current DCCT system, what strengths do you think support the use of this approach?
- In the current DCCT system, what areas of improvement do you think might be considered?
- In your view, how prepared are the graduating nurses for the NUCLEX and nursing practice in terms of their required mathematical skills and confidence relating to these skills?
- Do you have any other comments that you’d like to share relating to mathematics for nursing?
- Based on your survey/questionnaire comment, [selected survey quotation deemed of further interest to the research team], can you please provide us with more information regarding your perceptions on this first issue.
- Based on your survey/questionnaire comment, [second selected quotation deemed of further interest to the research team], can you please provide us with more information regarding your perceptions on this second issue.
- Do you have any other comments that you’d like to share relating to mathematics for nursing?
References
- Bagnasco, A.; Galaverna, L.; Aleo, G.; Grugnetti, A.; Rosa, F.; Sasso, L. Mathematical calculation skills required for drug administration in undergraduate nursing students to ensure patient safety: A descriptive study—drug calculation skills in nursing students. Nurse Educ. Pract. 2016, 16, 33–39. [Google Scholar] [CrossRef]
- World Health Organization. Medication Without Harm: WHO Global Patient Safety Challenge; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- College of Nurses of Ontario. Entry to Practice Competencies for Registered Nurses; College of Nurses of Ontario: Toronto, ON, Canada; Available online: https://www.cno.org/globalassets/docs/reg/41037-entry-to-practice-competencies-2020.pdf (accessed on 11 December 2021).
- Johnson, J.; Kareem, A.; White, D.; Ngwakongnwi, E.M.; Mohammadpour, M.; Rizkika, N.; Ouattas, R.; Shahrour, Y.; Ali, R.; Roshanuddin, J. Nursing students’ perspectives on learning math for medication calculations in Canadian nursing program in Qatar. Nurse Educ. Pract. 2020, 49, 102885. [Google Scholar] [CrossRef] [PubMed]
- Gunes, U.Y.; Baren, L.; Yilmaz, D. Mathematical and drug calculation skills of nursing students in Turkey. Int. J. Caring Sci. 2016, 9, 220–227. [Google Scholar]
- Williams, B.; Davis, S. Maths anxiety and medication dosage calculation errors: A scoping review. Nurse Educ. Pract. 2016, 20, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Valdez, L.P.; de Guzman, A.; Escolar-Chua, R. A structural equation modeling of the factors affecting student nurses’ medication errors. Nurse Educ. Today 2013, 33, 222–228. [Google Scholar] [CrossRef]
- Maley, B.; Rafferty, M. Can math competency predict success in nursing school? Teach. Learn. Nurs. 2019, 14, 198–202. [Google Scholar] [CrossRef]
- Ralph, N.; Graham, C.; Beccaria, L.; Rogers, C. Entry requirements in nursing: Results from a national survey of nurse academics on entry requirements in Australian bachelor of nursing programs. Collegian 2019, 26, 140–145. [Google Scholar] [CrossRef] [Green Version]
- Harvey, S.; Murphy, F.; Lake, R.; Jenkins, L.; Cavanna, A.; Tait, M. Diagnosing the problem: Using a tool to identify pre-registration nursing students’ mathematical ability. Nurse Educ. Pract. 2010, 10, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Roykenes KSmith, K.; Larsen, T. ‘It is the situation that makes it difficult’: Experiences of nursing students faced with a high-stakes drug calculation test. Nurse Educ. Pract. 2014, 14, 350–356. [Google Scholar] [CrossRef]
- Koharchik, L.; Hardy, E.; King, M.; Garibo, Y. Evidence-based approach to improve nursing student dosage calculation proficiency. Teach. Learn. Nurs. 2014, 9, 69–74. [Google Scholar] [CrossRef]
- McCollum, P.; Rogers, K. Practice makes perfect. Nurs. Stand. 2013, 27. [Google Scholar] [CrossRef]
- Ramjan, L.; Stewart, L.; Salammonson, Y.; Morris, M.M.; Armstrong, L.; Sanchez, P.; Flannery, L. Identifying strategies to assist final semester nursing students to develop numeracy skills: A mixed methods study. Nurse Educ. Today 2014, 34, 405–412. [Google Scholar] [CrossRef]
- Sherriff, K.; Burston, S.; Wallis, M. Effectiveness of a computer-based medication calculation education and testing programme for nurses. Nurse Educ. Today 2012, 32, 46–51. [Google Scholar] [CrossRef]
- Mills, S. Teaching and learning medication calculations: A grounded theory of conceptual understanding. Int. J. Nurs. Educ. Scholarsh. 2016, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mackie, J.E.; Bruce, C.D. Increasing nursing students’ understanding and accuracy with medical dose calculations: A collaborative approach. Nurse Educ. Today 2016, 40, 146–153. [Google Scholar] [CrossRef]
- Creswell, J. Qualitative Inquiry and Research Design: Choosing among Five Approaches, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Denzin, N.K.; Lincoln, Y.S. (Eds.) The Sage Handbook of Qualitative Research, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- Yin, R.K. Case Study Research: Design and Methods, 4th ed.; Sage: Thousand Oaks, CA, USA, 2019. [Google Scholar]
- Jarvis, D.H.; Kozuskanich, A.; Law, B.; McCullough, K.D. The techno-numerate nurse: Results of a study exploring nursing student and nurse perceptions of workplace mathematics and technology demands. Qual. Adv. Nurs. Educ. 2014, 1, 5. [Google Scholar] [CrossRef] [Green Version]
- Hunter Revell, S.M.; McCurry, M.K. Effective pedagogies for teaching math to nursing students: A literature review. Nurse Educ. Today 2013, 33, 1352–1356. [Google Scholar] [CrossRef]
- Karen, S.; Marianne, W.; Sarah, B. Medication calculation competencies for registered nurses: A literature review. Aust. J. Adv. Nurs. 2011, 28, 75–83. [Google Scholar]
- Coyne, E.; Needham, J.; Rands, H. Enhancing student nurses’ medication calculation knowledge: Integrating theoretical knowledge into practice. Nurse Educ. Today 2013, 33, 1014–1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dilles, T.; Vander Stichele, R.R.; Van Nortel, L.; Elseviers, M.M. Nursing students’ pharmacological knowledge and calculation skills: Ready for practice? Nurse Educ. Today 2011, 31, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, K.J.; Boyle, M.J.; Williams, B.; Fairhall, R. Numeracy skills of nursing students. Nurse Educ. Today 2011, 31, 815–818. [Google Scholar] [CrossRef] [PubMed]
- Grugnetti, A.M.; Bagnasco, A.; Rosa, F. Effectiveness of a clinical skills workshop for drug-dosage calculation in a nursing program. Nurse Educ. Today 2014, 34, 619–624. [Google Scholar] [CrossRef]
- Whitehair, L.; Provost, S.; Hurley, J. Identification of prescribing errors by pre-registration student nurses: A cross-sectional observational study utilising a prescription medication quiz. Nurse Educ. Today 2014, 34, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Wright, K. Student nurses’ perceptions of how they learn drug calculation skills. Nurse Educ. Today 2012, 32, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.G.; Curtis, A.; Harris, L.C. Improving dose calculation pass rates with peer tutoring. J. Nurs. Educ. 2019, 58, 188. [Google Scholar] [CrossRef]
- Coben, D.; Weeks, K. Meeting the mathematical demands of the safety-critical workplace: Medication dosage calculation problem-solving for nursing. Educ. Stud. Math. 2014, 86, 253–270. [Google Scholar] [CrossRef]
- Pauly-O’Neill, S.; Prion, S. Using integrated simulation in a nursing program to improve medication administration skills in the pediatric population. Nurs. Educ. Perspect. 2013, 34, 148–153. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarvis, D.H.; McCullough, K.D.; McParland, T.R. Nurse Education and Mathematical Competency: Implementation of an Online, Self-Directed, Prerequisite Model. Int. J. Environ. Res. Public Health 2021, 18, 13106. https://doi.org/10.3390/ijerph182413106
Jarvis DH, McCullough KD, McParland TR. Nurse Education and Mathematical Competency: Implementation of an Online, Self-Directed, Prerequisite Model. International Journal of Environmental Research and Public Health. 2021; 18(24):13106. https://doi.org/10.3390/ijerph182413106
Chicago/Turabian StyleJarvis, Daniel H., Karey D. McCullough, and Tammie R. McParland. 2021. "Nurse Education and Mathematical Competency: Implementation of an Online, Self-Directed, Prerequisite Model" International Journal of Environmental Research and Public Health 18, no. 24: 13106. https://doi.org/10.3390/ijerph182413106
APA StyleJarvis, D. H., McCullough, K. D., & McParland, T. R. (2021). Nurse Education and Mathematical Competency: Implementation of an Online, Self-Directed, Prerequisite Model. International Journal of Environmental Research and Public Health, 18(24), 13106. https://doi.org/10.3390/ijerph182413106





