Low QRS Voltage in Limb Leads Indicates Accompanying Precordial Voltage Attenuation Resulting in Underestimation of Left Ventricular Hypertrophy
Abstract
:1. Introduction
2. Materials and Methods
3. Results
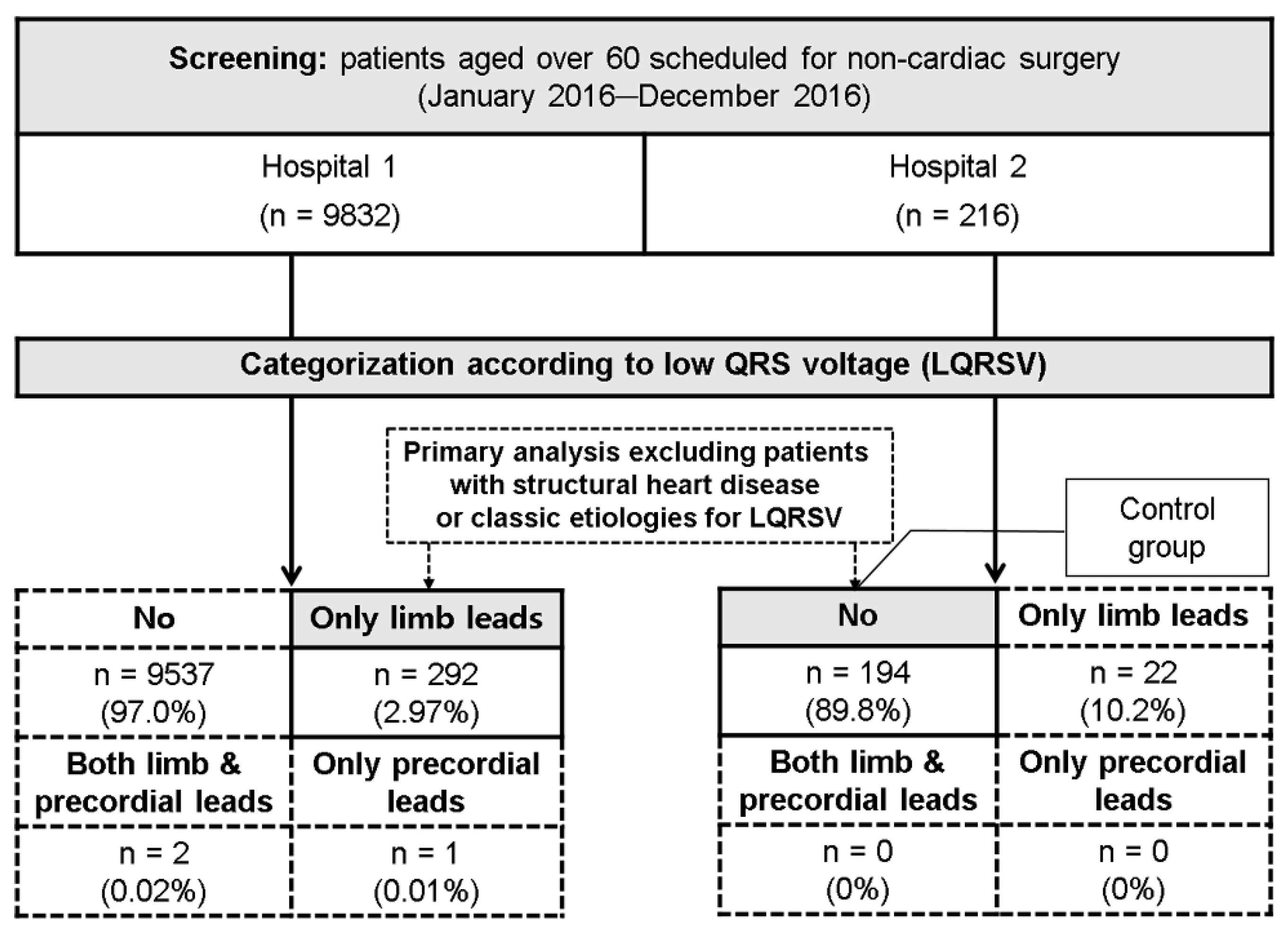
3.1. Patient Categorization and Baseline Characteristics
3.2. Analysis of Patients without Structural Heart Disease or Classic Etiologies of LQRSV
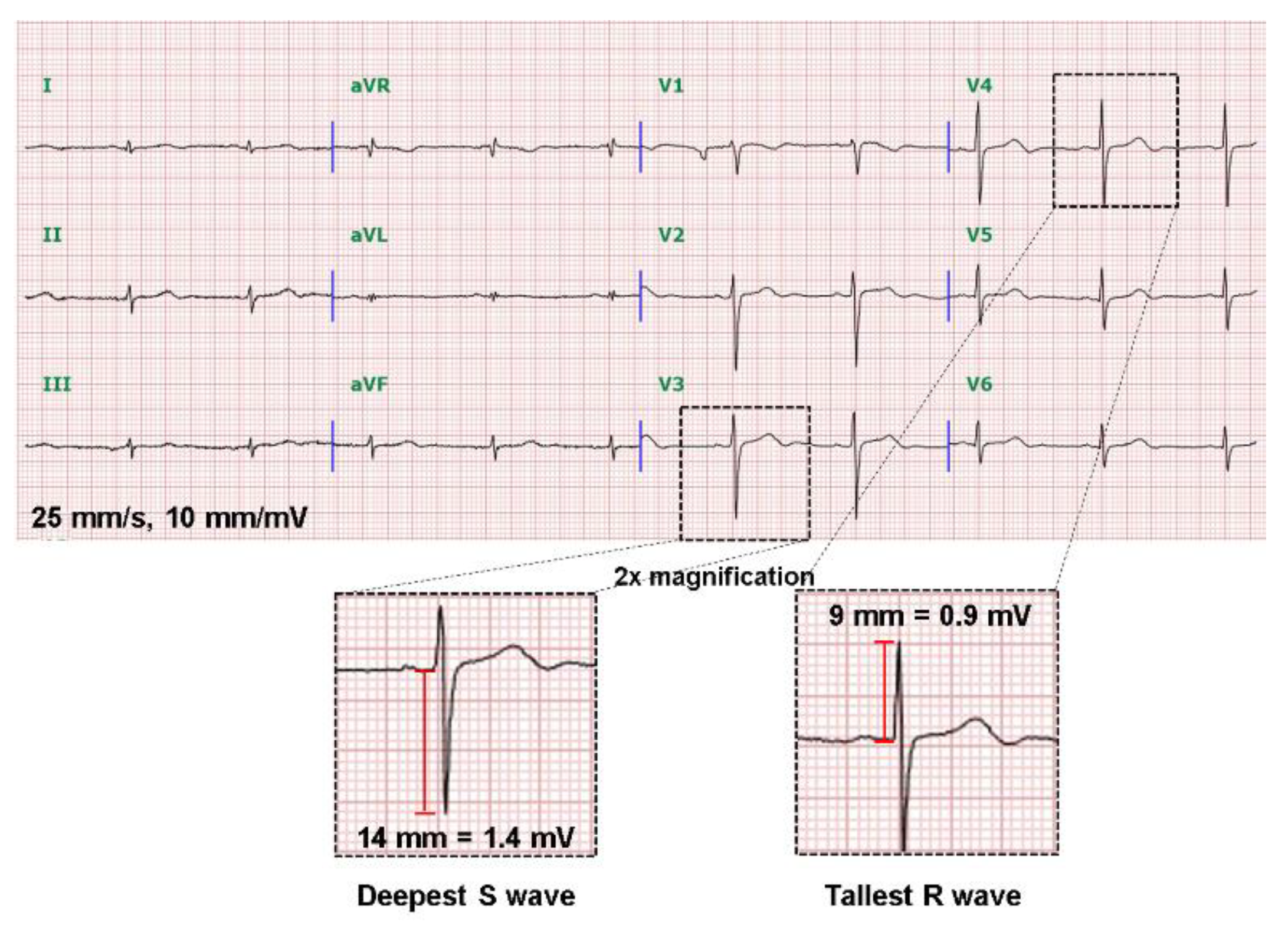
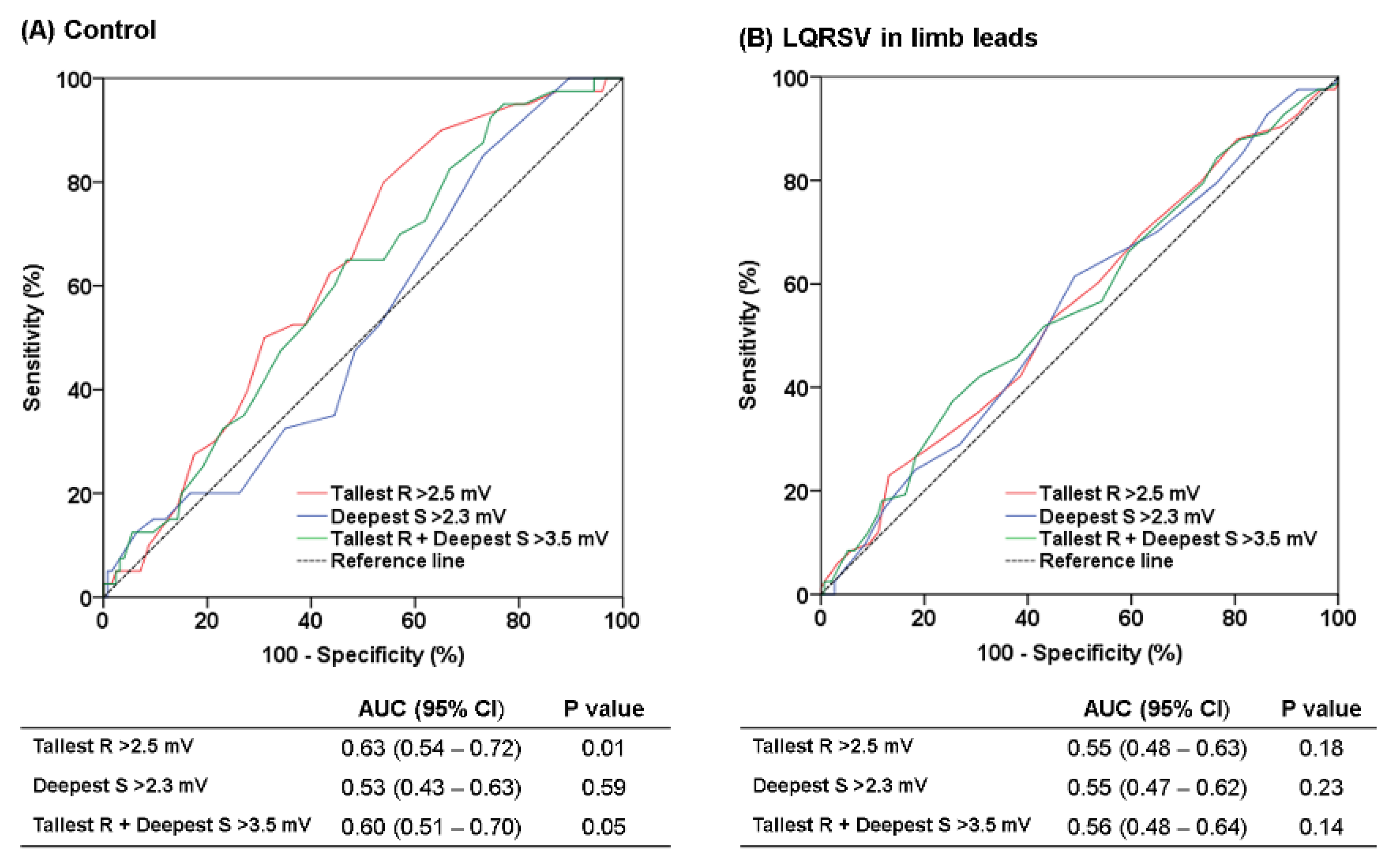
3.3. Diagnostic Performance of Precordial Voltages to Predict Echocardiographic LVH
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Madias, J.E. Low QRS voltage and its causes. J. Electrocardiol. 2008, 41, 498–500. [Google Scholar] [CrossRef]
- Chinitz, J.S.; Cooper, J.M.; Verdino, R.J. Electrocardiogram voltage discordance: Interpretation of low QRS voltage only in the limb leads. J. Electrocardiol. 2008, 41, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Alpert, M.A.; Terry, B.E.; Cohen, M.V.; Fan, T.; Painter, J.A.; Massey, C.V. The electrocardiogram in morbid obesity. Am. J. Cardiol. 2000, 85, 908–910. [Google Scholar] [CrossRef]
- Usoro, A.O.; Bradford, N.; Shah, A.J.; Soliman, E.Z. Risk of Mortality in Individuals With Low QRS Voltage and Free of Cardiovascular Disease. Am. J. Cardiol. 2014, 113, 1514–1517. [Google Scholar] [CrossRef] [PubMed]
- Mango, F.; Caselli, S.; Luchetti, A.; Pelliccia, A. Low QRS voltages in Olympic athletes: Prevalence and clinical correlates. Eur. J. Prev. Cardiol. 2020, 27, 1542–1548. [Google Scholar] [CrossRef]
- Kim, D.H.; Verdino, R.J. Electrocardiogram voltage discordance: Interpretation of low QRS voltage only in the precordial leads. J. Electrocardiol. 2017, 50, 551–554. [Google Scholar] [CrossRef]
- Macfarlane, P.W.; van Oosterom, A.; Pahlm, O.; Kligfield, P.; Janse, M.; Camm, J. Comprehensive Electrocardiology; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Kamath, S.A.; Neto, J.D.P.M.; Canham, R.M.; Uddin, F.; Toto, K.H.; Nelson, L.L.; Kaiser, P.A.; de Lemos, J.A.; Drazner, M.H. Low voltage on the electrocardiogram is a marker of disease severity and a risk factor for adverse outcomes in patients with heart failure due to systolic dysfunction. Am. Heart J. 2006, 152, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Porcel, J.M.; Vives, M. Etiology and Pleural Fluid Characteristics of Large and Massive Effusions. Chest 2003, 124, 978–983. [Google Scholar] [CrossRef]
- Karkhanis, V.S.; Joshi, J.M. Pleural effusion: Diagnosis, treatment, and management. OAEM 2012, 4, 31–52. [Google Scholar] [CrossRef] [Green Version]
- Celli, B.; MacNee, W.; Agusti, A.; Anzueto, A.; Berg, B.; Buist, A.; Calverley, P.; Chavannes, N.; Dillard, T.; Fahy, B.; et al. Standards for the diagnosis and treatment of patients with COPD: A summary of the ATS/ERS position paper. Eur. Respir. J. 2004, 23, 932–946. [Google Scholar] [CrossRef] [Green Version]
- Wagner, G.S. Marriott’s Practical Electrocardiography; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Wilson, F.N.; Johnston, F.D.; Rosenbaum, F.F.; Erlanger, H.; Kossmann, C.E.; Hecht, H.; Cotrim, N.; de Oliveira, R.M.; Scarsi, R.; Barker, P.S. The precordial electrocardiogram. Am. Heart J. 1944, 27, 19–85. [Google Scholar] [CrossRef] [Green Version]
- Sokolow, M.; Lyon, T.P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am. Heart J. 1949, 37, 161–186. [Google Scholar] [CrossRef]
- Grant, R.P. Clinical Electrocardiography; The Spatial Vector Approach; McGraw-Hill Book Company: New York, NY, USA, 1957. [Google Scholar]
- Sharma, S.; Drezner, J.A.; Baggish, A.; Papadakis, M.; Wilson, M.G.; Prutkin, J.M.; La Gerche, A.; Ackerman, M.J.; Börjesson, M.; Salerno, J.C.; et al. International recommendations for electrocardiographic interpretation in athletes. Eur. Heart J. 2018, 39, 1466–1480. [Google Scholar] [CrossRef]
- Hedman, K.; Moneghetti, K.J.; Hsu, D.; Christle, J.W.; Patti, A.; Ashley, E.; Hadley, D.; Haddad, F.; Froelicher, V. Limitations of Electrocardiography for Detecting Left Ventricular Hypertrophy or Concentric Remodeling in Athletes. Am. J. Med. 2020, 133, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Maisch, B.; Seferović, P.M.; Ristić, A.D.; Erbel, R.; Rienmüller, R.; Adler, Y.; Tomkowski, W.Z.; Thiene, G.; Yacoub, M.H.; Priori, S.G.; et al. Guidelines on the Diagnosis and Management of Pericardial Diseases Executive SummaryThe Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Eur. Heart J. 2004, 25, 587–610. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Lumlertgul, S.; Chenthanakij, B.; Madias, J.E. ECG Leads I and II to Evaluate Diuresis of Patients with Congestive Heart Failure Admitted to the Hospital via the Emergency Department. Pacing Clin. Electrophysiol. 2009, 32, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Madias, J.E. Superiority of the limb leads over the precordial leads on the 12-lead ECG in monitoring fluctuating fluid overload in a patient with congestive heart failure. J. Electrocardiol. 2007, 40, 395–399. [Google Scholar] [CrossRef]
- Hancock, E.W.; Deal, B.J.; Mirvis, D.M.; Okin, P.; Kligfield, P.; Gettes, L.S. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part V: Electrocardiogram Changes Associated With Cardiac Chamber Hypertrophy A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J. Am. Coll. Cardiol. 2009, 53, 992–1002. [Google Scholar] [CrossRef] [Green Version]
- Mathew, J.; Sleight, P.; Lonn, E.; Johnstone, D.; Pogue, J.; Yi, Q.; Bosch, J.; Sussex, B.; Probstfield, J.; Yusuf, S. Reduction of Cardiovascular Risk by Regression of Electrocardiographic Markers of Left Ventricular Hypertrophy by the Angiotensin-Converting Enzyme Inhibitor Ramipril. Circulation 2001, 104, 1615–1621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prineas, R.J.; Rautaharju, P.M.; Grandits, G.; Crow, R. Independent risk for cardiovascular disease predicted by modified continuous score electrocardiographic criteria for 6-year incidence and regression of left ventricular hypertrophy among clinically disease free men: 16-year follow-up for the multiple risk factor intervention trial. J. Electrocardiol. 2001, 34, 91–101. [Google Scholar] [CrossRef]
- Okin, P.M.; Devereux, R.B.; Jern, S.; Kjeldsen, S.E.; Julius, S.; Nieminen, M.S.; Snapinn, S.; Harris, K.E.; Aurup, P.; Edelman, J.M.; et al. Regression of Electrocardiographic Left Ventricular Hypertrophy During Antihypertensive Treatment and the Prediction of Major Cardiovascular Events. JAMA 2004, 292, 2343–2349. [Google Scholar] [CrossRef] [Green Version]
- Okin, P.M.; Hille, D.A.; Kjeldsen, S.E.; Devereux, R.B. Combining ECG Criteria for Left Ventricular Hypertrophy Improves Risk Prediction in Patients With Hypertension. J. Am. Heart Assoc. 2017, 6, e007564. [Google Scholar] [CrossRef] [Green Version]
- Verdecchia, P.; Dovellini, E.V.; Gorini, M.; Gozzelino, G.; Lucci, D.; Milletich, A.; Maggioni, A.P. Comparison of electrocardiographic criteria for diagnosis of left ventricular hypertrophy in hypertension: The MAVI study. Ital. Heart J. Off. J. Ital. Fed. Cardiol. 2000, 1, 207–215. [Google Scholar]
- Romhilt, D.W.; Bove, K.E.; Norris, R.J.; Conyers, E.; Conradi, S.; Rowlands, D.T.; Scott, R.C. A Critical Appraisal of the Electrocardiographic Criteria for the Diagnosis of Left Ventricular Hypertrophy. Circulation 1969, 40, 185–196. [Google Scholar] [CrossRef] [Green Version]
- Schillaci, G.; Verdecchia, P.; Borgioni, C.; Ciucci, A.; Guerrieri, M.; Zampi, I.; Battistelli, M.; Bartoccini, C.; Porcellati, C. Improved electrocardiographic diagnosis of left ventricular hypertrophy. Am. J. Cardiol. 1994, 74, 714–719. [Google Scholar] [CrossRef]
- Shao, Q.; Meng, L.; Tse, G.; Sawant, A.C.; Zhuo Yi Chan, C.; Bazoukis, G.; Baranchuk, A.; Li, G.; Liu, T. Newly proposed electrocardiographic criteria for the diagnosis of left ventricular hypertrophy in a Chinese population. Ann. Noninvasive Electrocardiol. Off. J. Int. Soc. Holter Noninvasive Electrocardiol. Inc. 2019, 24, e12602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peguero, J.G.; Presti, S.L.; Perez, J.; Issa, O.; Brenes, J.C.; Tolentino, A. Electrocardiographic Criteria for the Diagnosis of Left Ventricular Hypertrophy. J. Am. Coll. Cardiol. 2017, 69, 1694–1703. [Google Scholar] [CrossRef] [PubMed]
- Angeli, F.; Verdecchia, P.; Angeli, E.; Poeta, F.; Sardone, M.; Bentivoglio, M.; Prosciutti, L.; Cocchieri, M.; Zollino, L.; Bellomo, G.; et al. Day-to-day variability of electrocardiographic diagnosis of left ventricular hypertrophy in hypertensive patients. Influence of electrode placement. J. Cardiovasc. Med. 2006, 7, 812–816. [Google Scholar] [CrossRef] [PubMed]
- Cyrille, N.B.; Goldsmith, J.; Alvarez, J.; Maurer, M.S. Prevalence and Prognostic Significance of Low QRS Voltage Among the Three Main Types of Cardiac Amyloidosis. Am. J. Cardiol. 2014, 114, 1089–1093. [Google Scholar] [CrossRef]
| LQRSV in Limb Leads (n = 236) | Control (n = 167) | p Value | |
|---|---|---|---|
| Demographic data | |||
| Age (year) | 71.1 ± 6.7 | 71.3 ± 6.1 | 0.78 |
| Male | 142 (60.2) | 80 (47.9) | 0.02 |
| Height (cm) | 160.5 ± 9.2 | 159.2 ± 8.7 | 0.15 |
| Weight (kg) | 60.9 ± 9.9 | 58.8 ± 9.4 | 0.04 |
| BMI (kg/m2) | 23.5 ± 2.7 | 23.2 ± 2.8 | 0.18 |
| Hypertension | 115 (48.7) | 82 (49.1) | 0.94 |
| Diabetes | 65 (27.5) | 40 (24.0) | 0.42 |
| Echocardiographic parameters | |||
| LV ejection fraction (%) | 64.9 ± 5.7 | 65.3 ± 6.2 | 0.50 |
| LV end-diastolic dimension (mm) | 47.2 ± 4.2 | 47.5 ± 5.2 | 0.71 |
| LV end-systolic dimension (mm) | 28.2 ± 3.4 | 30.3 ± 4.2 | <0.001 |
| LV mass index (g/m2) | 100.9 ± 22.9 | 93.5 ± 18.4 | 0.001 |
| Echocardiographic LVH 1 | 79 (33.5) | 40 (24.0) | 0.04 |
| Electrocardiographic parameters | |||
| Baseline rhythm | |||
| Sinus | 215 (91.1) | 160 (96.4) | 0.04 |
| Atrial fibrillation | 21 (8.9) | 6 (3.6) | 0.04 |
| QRS duration (ms) | 88.1 ± 9.3 | 89.6 ± 12.5 | 0.16 |
| Precordial R/S transition zone | |||
| Normal | 163 (69.1) | 128 (77.1) | 0.08 |
| Early (V1 or V2) | 12 (5.1) | 19 (11.4) | 0.02 |
| Late (V5 or V6) | 58 (24.6) | 19 (11.4) | 0.001 |
| Frontal QRS axis | 27.0 ± 41.5 | 38.0 ± 31.7 | 0.004 |
| Normal (−30–90°) | 207 (87.7) | 160 (96.4) | 0.002 |
| Left axis deviation | 18 (7.6) | 3 (1.8) | 0.01 |
| Right axis deviation | 11 (4.7) | 3 (1.8) | 0.12 |
| Precordial voltages (mm) † | |||
| Tallest R wave | 13.5 ± 4.3 | 18.5 ± 6.7 | <0.001 |
| Deepest S wave | 12.2 ± 3.9 | 11.8 ± 4.3 | 0.33 |
| Tallest R+ deepest S wave | 25.7 ± 6.2 | 30.4 ± 8.7 | <0.001 |
| PR interval (ms) | 173.0 ± 24.3 | 170.4 ± 22.0 | 0.29 |
| Corrected QT interval (ms) | 430.8 ± 26.0 | 439.5 ± 27.0 | 0.001 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | |
| Demographic data | ||||
| Age (year) | 0.996 (0.966–1.027) | 0.783 | ||
| Male | 1.643 (1.101–2.451) | 0.015 | 2.714 (1.444–5.101) | 0.002 |
| Height (cm) | 1.016 (0.994–1.039) | 0.15 | ||
| Weight (kg) | 1.022 (1.001–1.044) | 0.037 | 1.010 (0.977–1.045) | 0.558 |
| BMI (kg/m2) | 1.052 (0.977–1.132) | 0.177 | ||
| Hypertension | 0.985 (0.663–1.465) | 0.941 | ||
| Diabetes | 1.207 (0.765–1.904) | 0.419 | ||
| Echocardiographic parameters | ||||
| LV ejection fraction (%) | 0.989 (0.956–1.022) | 0.501 | ||
| LV end-diastolic dimension (mm) | 1.008 (0.966–1.052) | 0.714 | ||
| LV end-systolic dimension (mm) | 0.864 (0.817–0.914) | <0.001 | 0.713 (0.650–0.781) | <0.001 |
| LV mass index (g/m2) | 1.017 (1.007–1.027) | 0.001 | 1.058 (1.040–1.076) | <0.001 |
| Electrocardiographic parameters | ||||
| Baseline atrial fibrillation | 2.605 (1.028–6.602) | 0.044 | 4.584 (1.372–15.316) | 0.013 |
| QRS duration (ms) | 0.987 (0.969–1.006) | 0.167 | ||
| Late R/S transition | 2.521 (1.437–4.423) | 0.001 | 1.046 (0.492–2.223) | 0.98 |
| Left axis deviation | 4.514 (1.308–15.581) | 0.017 | 1.504 (0.368–6.152) | 0.57 |
| Precordial tallest R voltages (mm) | 0.836 (0.798–0.876) | <0.001 | 0.783 (0.734–0.837) | <0.001 |
| PR interval (ms) | 1.005 (0.996–1.014) | 0.29 | ||
| Corrected QT interval (ms) | 0.988 (0.980–0.995) | 0.002 | 0.988 (0.978–0.998) | 0.017 |
| Sensitivity (%) | Specificity (%) | LR+ | LR− | McNemar Test 1 | |
|---|---|---|---|---|---|
| LQRSV in limb leads | |||||
| Tallest R > 25 mm 95% confidence interval | 0.0 (0/83 × 100) [0.0–4.4] | 100 (153/153 × 100) [97.6–100] | Not applicable | 1.00 | Not applicable |
| Deepest S > 23 mm 95% confidence interval | 0.0 (0/83 × 100) [0.0–4.4] | 98.7 (151/153 × 100) [95.4–99.8] | 0.00 | 1.01 | <0.001 |
| Tallest R + deepest S > 35 mm 95% confidence interval | 8.4 (7/83 × 100) [3.5–16.6] | 93.5 (0/83 × 100) [88.3–96.8] | 1.29 | 0.98 | <0.001 |
| Control | |||||
| Tallest R > 25 mm 95% confidence interval | 17.5 (7/40 × 100) [7.3–32.8] | 85.0 (108/127 × 100) [77.6–90.8] | 1.17 | 0.97 | 0.07 |
| Deepest S > 23 mm 95% confidence interval | 2.5 (1/40 × 100) [0.1–13.2] | 99.2 (125/126 × 100) [95.7–99.9] | 3.13 | 0.98 | <0.001 |
| Tallest R + deepest S > 35 mm 95% confidence interval | 32.5 (13/40 × 100) [18.6–49.1] | 77.0 (97/126 × 100) [68.7–84.0] | 1.41 | 0.88 | 0.89 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gwag, H.-B.; Lee, S.-H.; Kim, H.-J.; Kim, J.-S.; On, Y.-K.; Park, S.-J.; Park, K.-M. Low QRS Voltage in Limb Leads Indicates Accompanying Precordial Voltage Attenuation Resulting in Underestimation of Left Ventricular Hypertrophy. Int. J. Environ. Res. Public Health 2021, 18, 12867. https://doi.org/10.3390/ijerph182412867
Gwag H-B, Lee S-H, Kim H-J, Kim J-S, On Y-K, Park S-J, Park K-M. Low QRS Voltage in Limb Leads Indicates Accompanying Precordial Voltage Attenuation Resulting in Underestimation of Left Ventricular Hypertrophy. International Journal of Environmental Research and Public Health. 2021; 18(24):12867. https://doi.org/10.3390/ijerph182412867
Chicago/Turabian StyleGwag, Hye-Bin, Su-Hyun Lee, Hyeon-Jun Kim, June-Soo Kim, Young-Keun On, Seung-Jung Park, and Kyoung-Min Park. 2021. "Low QRS Voltage in Limb Leads Indicates Accompanying Precordial Voltage Attenuation Resulting in Underestimation of Left Ventricular Hypertrophy" International Journal of Environmental Research and Public Health 18, no. 24: 12867. https://doi.org/10.3390/ijerph182412867
APA StyleGwag, H.-B., Lee, S.-H., Kim, H.-J., Kim, J.-S., On, Y.-K., Park, S.-J., & Park, K.-M. (2021). Low QRS Voltage in Limb Leads Indicates Accompanying Precordial Voltage Attenuation Resulting in Underestimation of Left Ventricular Hypertrophy. International Journal of Environmental Research and Public Health, 18(24), 12867. https://doi.org/10.3390/ijerph182412867






