Epidemiological Trends of Malaria in Five Years and under Children of Nsanje District in Malawi, 2015–2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Design
2.2. Geographic Location of Nsanje District
2.3. Source of Data and Procedure
2.4. Data Analysis and Procedure
3. Results
3.1. Trends of Malaria Morbidity and Mortality from 2015 to 2019
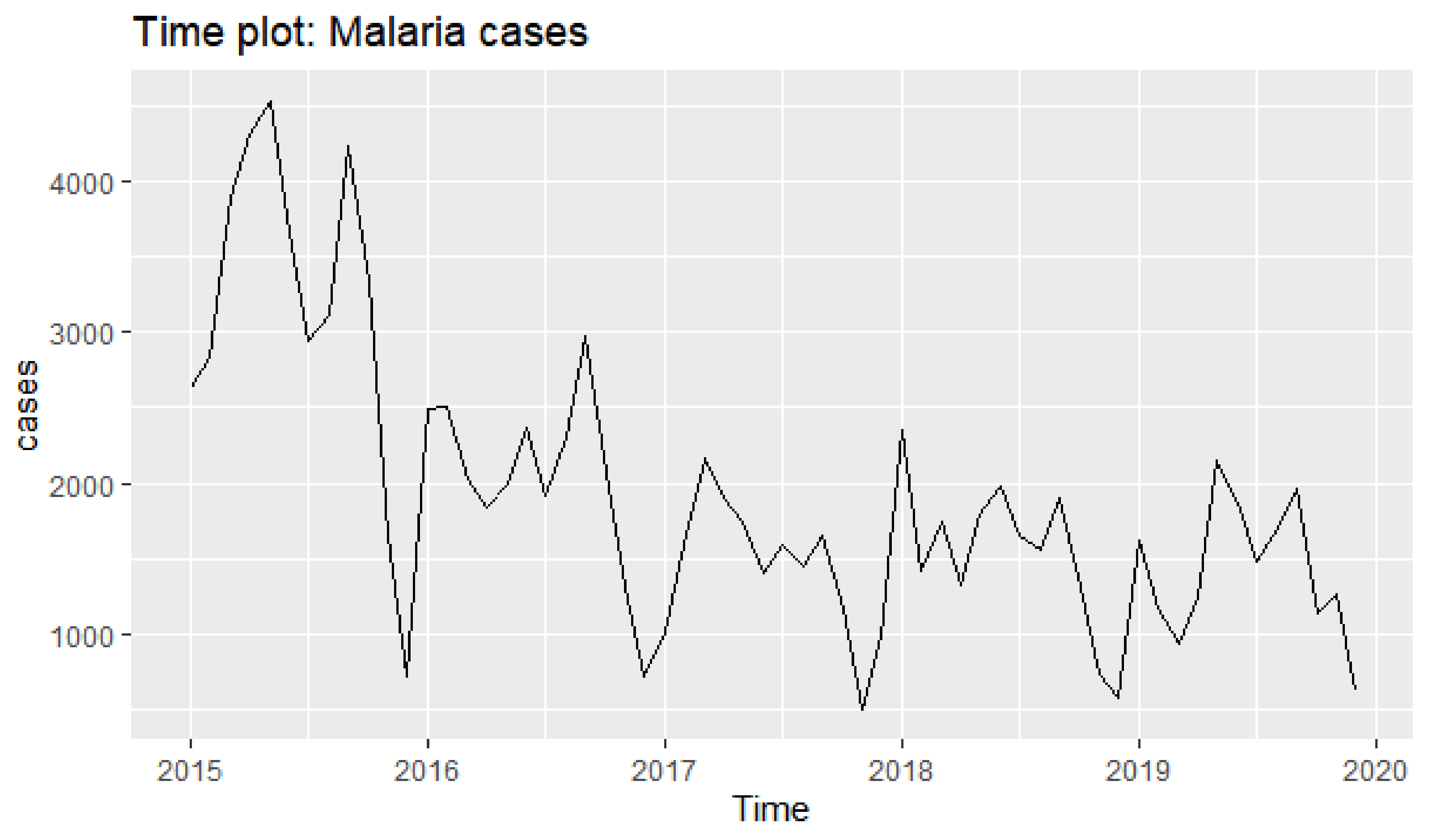
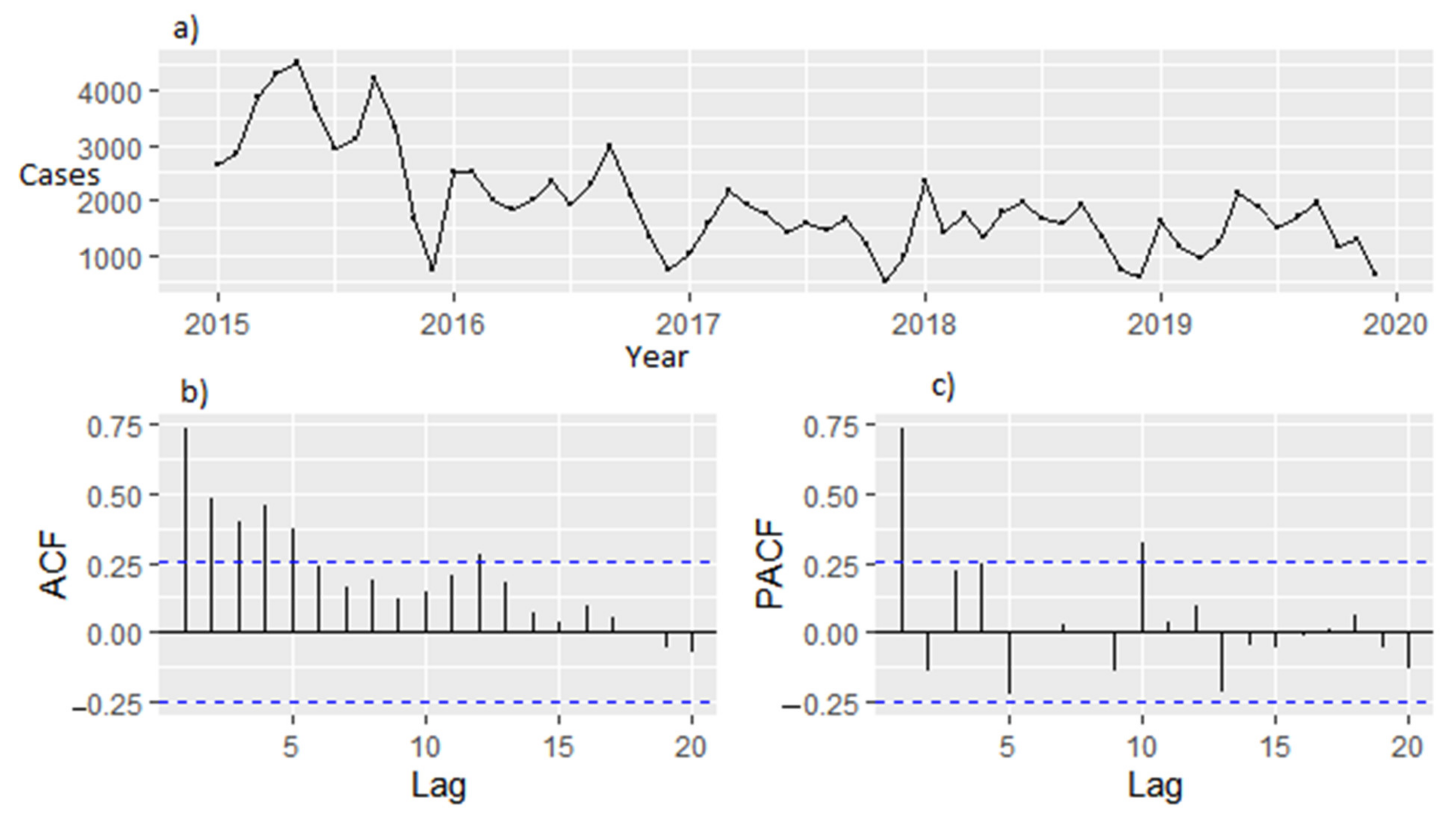
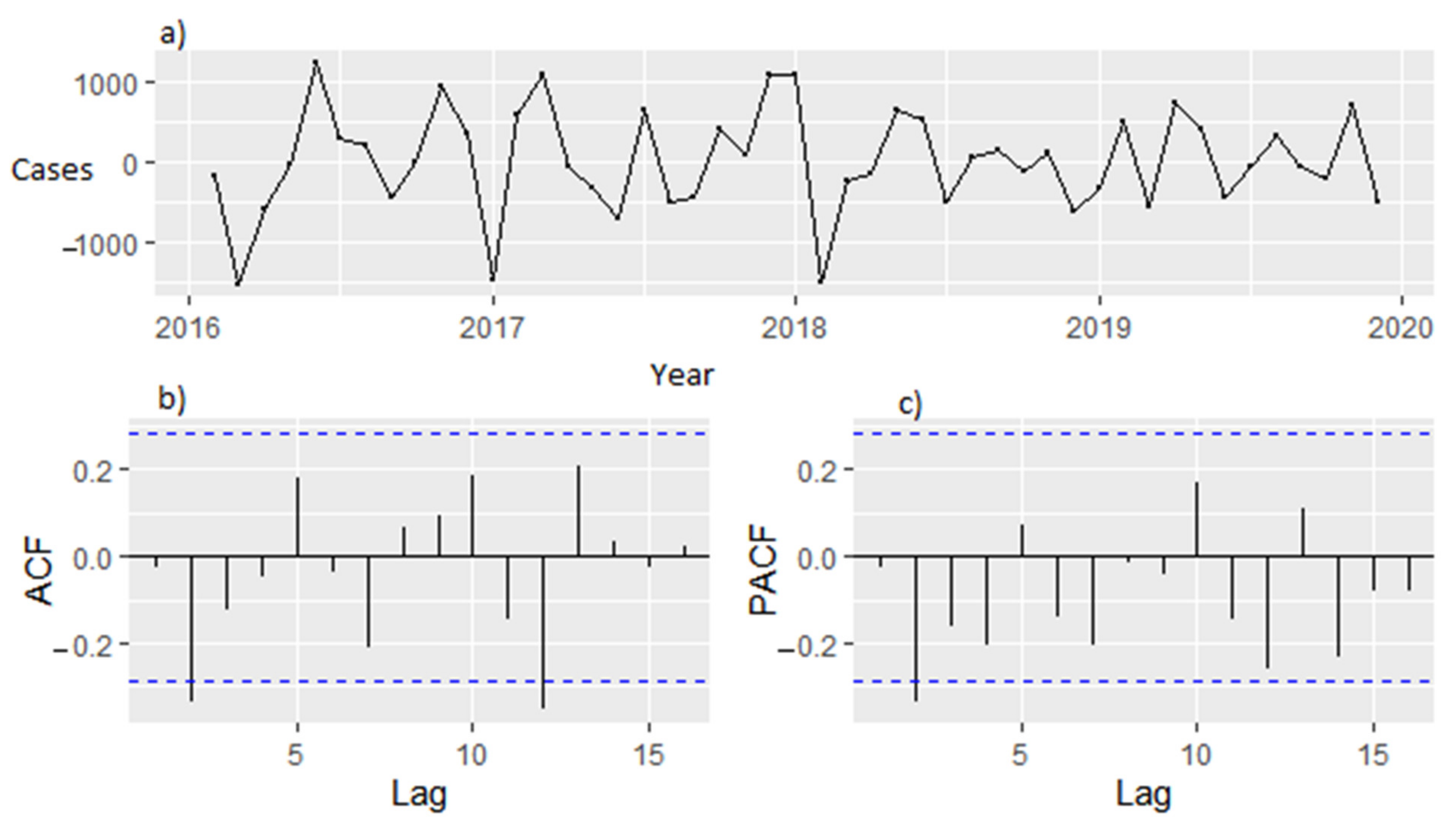
3.2. Time Series Analysis
3.3. Model Selection
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Autino, B.; Noris, A.; Russo, R.; Castelli, F. Epidemiology of malaria in endemic areas. Mediterr. J. Hematol. Infect. Dis. 2012, 4, e2012060. [Google Scholar] [CrossRef] [PubMed]
- Mushashu, U. Prevalence of Malaria Infection among under Fives and the Associated Factors in Muleba Distric-Kagera Region Tanzania. Ph.D. Thesis, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania, 2012; p. 72. [Google Scholar]
- CDC. About Malaria Biology. 2020. Available online: https://www.cdc.gov/globalhealth (accessed on 15 November 2021).
- Anokye, R.; Acheampong, E.; Owusu, I.; Obeng, E.I. Time series analysis of malaria in Kumasi: Using ARIMA models to forecast future incidence. Cogent Soc. Sci. 2018, 4, 1461544. [Google Scholar] [CrossRef]
- Chilanga, E.; Collin-Vezina, D.; MacIntosh, H.; Mitchell, C.; Cherney, K. Prevalence and determinants of malaria infection among children of local farmers in Central Malawi. Malar. J. 2020, 19, 308. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. World Malaria Report 2018; WHO: Geneva, Switzerland, 2018; p. 210. [Google Scholar]
- World Health Organisation. World Malaria Report 2020 20 Years of Global Progress; WHO: Geneva, Switzerland, 2020; p. 299. [Google Scholar]
- UNICEF. Achieving the Malaria MGD Target Reversing the Incidence of Malaria 2000–2015; UNICEF: New York, NY, USA; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- UNICEF. Malaria a Major Cause of Child Death and Poverty in Africa; UNICEF: New York, NY, USA, 2010. [Google Scholar]
- Mathanga, D.P.; Tembo, A.K.; Mzilahowa, T.; Bauleni, A.; Mtimaukenena, K.; Taylor, T.E.; Valim, C.; Walker, E.D.; Wilson, M.L. Patterns and determinants of malaria risk in urban and peri-urban areas of Blantyre, Malawi. Malar. J. 2016, 15, 590. [Google Scholar] [CrossRef] [PubMed]
- Mathanga, D.P.; Walker, E.D.; Wilson, M.L.; Ali, D.; Taylor, T.E.; Laufer, M.K. Malaria control in Malawi: Current status and directions for the future. Acta Trop. 2012, 121, 212–217. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bennett, A.; Kazembe, L.; Mathanga, D.P.; Kinyoki, D.; Ali, D.; Snow, R.W.; Noor, A.M. Mapping malaria transmission intensity in Malawi, 2000–2010. Am. J. Trop. Med. Hyg. 2013, 89, 840–849. [Google Scholar] [CrossRef]
- Song, Z.; Jia, X.; Bao, J.; Yang, Y.; Zhu, H.; Shi, X. Spatio-Temporal Analysis of Influenza-Like Illness and Prediction of Incidence in High-Risk Regions in the United States from 2011 to 2020. Int. J. Environ. Res. Public Health 2021, 18, 7120. [Google Scholar] [CrossRef] [PubMed]
- Ebhuoma, O.; Gebreslasie, M.; Magubane, L. A Seasonal Autoregressive Integrated Moving Average (SARIMA) forecasting model to predict monthly malaria cases in KwaZulu-Natal, South Africa. South Afr. Med J. 2018, 108, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Kifle, M.M.; Teklemariam, T.T.; Teweldeberhan, A.M.; Tesfamariam, E.H.; Andegiorgish, A.K.; Kidane, E.A. Malaria Risk Stratification and Modeling the Effect of Rainfall on Malaria Incidence in Eritrea. J. Environ. Public Health 2019, 2019, 7314129. [Google Scholar] [CrossRef] [PubMed]
- Larru, B.; Molyneux, E.; Ter Kuile, F.O.; Taylor, T.; Molyneux, M.; Terlouw, D.J. Malaria in infants below six months of age: Retrospective surveillance of hospital admission records in Blantyre, Malawi. Malar. J. 2009, 8, 310. [Google Scholar] [CrossRef] [PubMed]
- Bawah, A.; Ussher, F.; Alidu, H.; Kwasie, D. Hematological profile of children under five years with malaria at the Ho Municipality of Ghana. Edorium J. Pediatrics 2018, 2, 100004P05AB2018. [Google Scholar] [CrossRef]
- ICF; NSO. Malawi Demographic and Health Survey 2015-16; NSO: Zomba, Malawi; ICF: Rockville, MD, USA, 2017. [Google Scholar]
- National Malaria Control Programme (NMCP). Malawi Malaria Indicator Survey 2017; NMCP: Nairobi, Kenya, 2018. [Google Scholar]
- Barua, P.; Beeson, J.G.; Maleta, K.; Ashorn, P.; Rogerson, S.J. The impact of early life exposure to Plasmodium falciparum on the development of naturally acquired immunity to malaria in young Malawian children. Malar. J. 2019, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Kapesa, A.; Kweka, E.J.; Atieli, H.; Afrane, Y.A.; Kamugisha, E.; Lee, M.-C.; Zhou, G.; Githeko, A.K.; Yan, G. The current malaria morbidity and mortality in different transmission settings in Western Kenya. PLoS ONE 2018, 13, e0202031. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. World Malaria Report Briefing Kit; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Kalil, F.C.; Bedaso, H.M.; Wario, S.K. Trends of Malaria Morbidity and Mortality from 2010 to 2017 in Bale Zone, Ethiopia: Analysis of Surveillance Data. Infect. Drug Resist. 2020, 13, 4379–4387. [Google Scholar] [CrossRef] [PubMed]
- Habyarimana, F.; Ramroop, S. Prevalence and Risk Factors Associated with Malaria among Children Aged Six Months to 14 Years Old in Rwanda: Evidence from 2017 Rwanda Malaria Indicator Survey. Int. J. Environ. Res. Public Health 2020, 17, 7975. [Google Scholar] [CrossRef] [PubMed]
- Steynor, A.; Jack, C.; Wolski, P.; van Aardenne, L.; Lennard, C.; Ryan, S.J.; Ebi, K.; Allen, L.; Graff, N.; Zermoglio, F. The Influence of Climate on Malaria Incidence in Malaw: A Retrospective Analys. In Adaptation Thought Leadership and Assessments (ATLAS); Technical Report AIDOAA-I-14-00013; United States Agency for International Development: Washington, DC, USA.
- Drakou, K.; Nikolaou, T.; Vasquez, M.; Petric, D.; Michaelakis, A.; Kapranas, A.; Papatheodoulou, A.; Koliou, M. The Effect of Weather Variables on Mosquito Activity: A Snapshot of the Main Point of Entry of Cyprus. Int. J. Environ. Res. Public Health 2020, 17, 1403. [Google Scholar] [CrossRef] [PubMed]

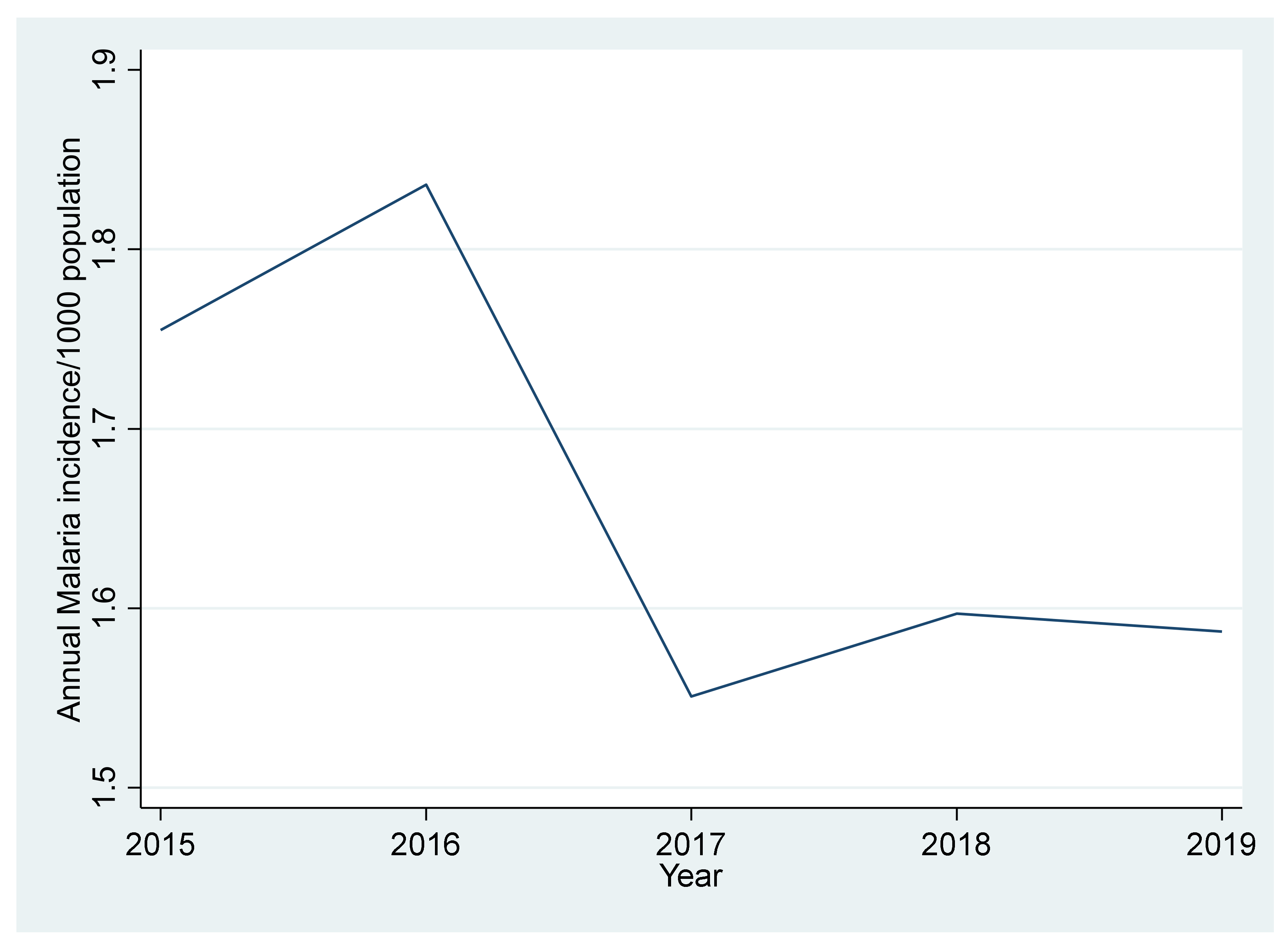


| Year | Population at Risk | No. of Cases (%) | No. of Deaths | Incidence Rate per 1000 Population | Death Rate per 100,000 Population | CFR in % |
|---|---|---|---|---|---|---|
| 2015 | 47,864 | 84(20.0) | 17 | 1.755 | 35.517 | 0.2 |
| 2016 | 49,059 | 90(21.4) | 13 | 1.836 | 26.499 | 0.144 |
| 2017 | 50,303 | 78(18.6) | 18 | 1.551 | 35.783 | 0.231 |
| 2018 | 52,597 | 84(20.0) | 10 | 1.597 | 19.012 | 0.119 |
| 2019 | 52,943 | 84(20.0) | 19 | 1.587 | 35.888 | 0.226 |
| Variable | Category | Number (%) | Mean Annual Malaria Incidence per 1000 Population |
|---|---|---|---|
| Gender | Male | 216(51.4) | 8.428 |
| Female | 204(48.6) | 7.259 | |
| Age group | (0–11) months | 40(9.5) | 1.164 |
| (12–23) months | 55(13.1) | 0.948 | |
| (24–35) months | 119(28.3) | 2.162 | |
| (36–47) months | 92(21.9) | 1.742 | |
| (48–69) months | 75(17.9) | 1.48 | |
| (60) months | 39(9.3) | 0.799 |
| Model | Estimate | t | Ljung–Box Q-Test | AIC | BIC | RMSE | MAPE | ||
|---|---|---|---|---|---|---|---|---|---|
| Statistics | |||||||||
| SARIMA(0,1,0)(1,1,0)12 | - | - | - | 14.498 | 0.206 | 14.498 | 0.206 | 14.498 | 0.206 |
| SAR1 | −0.485 | 3.485 | 0.000 | - | - | - | - | - | - |
| SARIMA(0,1,0)(0,1,1)12 | - | - | - | 17.857 | 0.0849 | 17.857 | 0.0849 | 17.857 | 0.0849 |
| SMA1 | −0.670 | −2.490 | 0.012 | - | - | - | - | - | - |
| SARIMA(0,1,1)(0,1,1)12 | - | - | - | 14.998 | 0.132 | 736.330 | 741.880 | 451.785 | 23.422 |
| MA1 | 0.204 | 0.790 | 0.429 | - | - | - | - | - | - |
| SMA1 | −0.799 | −1.600 | 0.110 | - | - | - | - | - | - |
| SARIMA(0,1,2)(0,1,1)12 | - | - | - | 8.681 | 0.4670 | 726.420 | 733.820 | 403.909 | 21.447 |
| MA1 | −0.078 | −0.610 | 0.542 | - | - | - | - | - | - |
| MA2 | −0.554 | −4.652 | 3.292 | - | - | - | - | - | - |
| SMA1 | −0.730 | −2.165 | 0.030 | - | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gondwe, T.; Yang, Y.; Yosefe, S.; Kasanga, M.; Mulula, G.; Luwemba, M.P.; Jere, A.; Daka, V.; Mudenda, T. Epidemiological Trends of Malaria in Five Years and under Children of Nsanje District in Malawi, 2015–2019. Int. J. Environ. Res. Public Health 2021, 18, 12784. https://doi.org/10.3390/ijerph182312784
Gondwe T, Yang Y, Yosefe S, Kasanga M, Mulula G, Luwemba MP, Jere A, Daka V, Mudenda T. Epidemiological Trends of Malaria in Five Years and under Children of Nsanje District in Malawi, 2015–2019. International Journal of Environmental Research and Public Health. 2021; 18(23):12784. https://doi.org/10.3390/ijerph182312784
Chicago/Turabian StyleGondwe, Theodore, Yongi Yang, Simeon Yosefe, Maisa Kasanga, Griffin Mulula, Mphatso Prince Luwemba, Annie Jere, Victor Daka, and Tobela Mudenda. 2021. "Epidemiological Trends of Malaria in Five Years and under Children of Nsanje District in Malawi, 2015–2019" International Journal of Environmental Research and Public Health 18, no. 23: 12784. https://doi.org/10.3390/ijerph182312784
APA StyleGondwe, T., Yang, Y., Yosefe, S., Kasanga, M., Mulula, G., Luwemba, M. P., Jere, A., Daka, V., & Mudenda, T. (2021). Epidemiological Trends of Malaria in Five Years and under Children of Nsanje District in Malawi, 2015–2019. International Journal of Environmental Research and Public Health, 18(23), 12784. https://doi.org/10.3390/ijerph182312784






