Feasibility of Implementing Physical Activity Behavior Change Counseling in an Existing Cancer-Exercise Program
Abstract
:1. Introduction
2. Materials and Methods
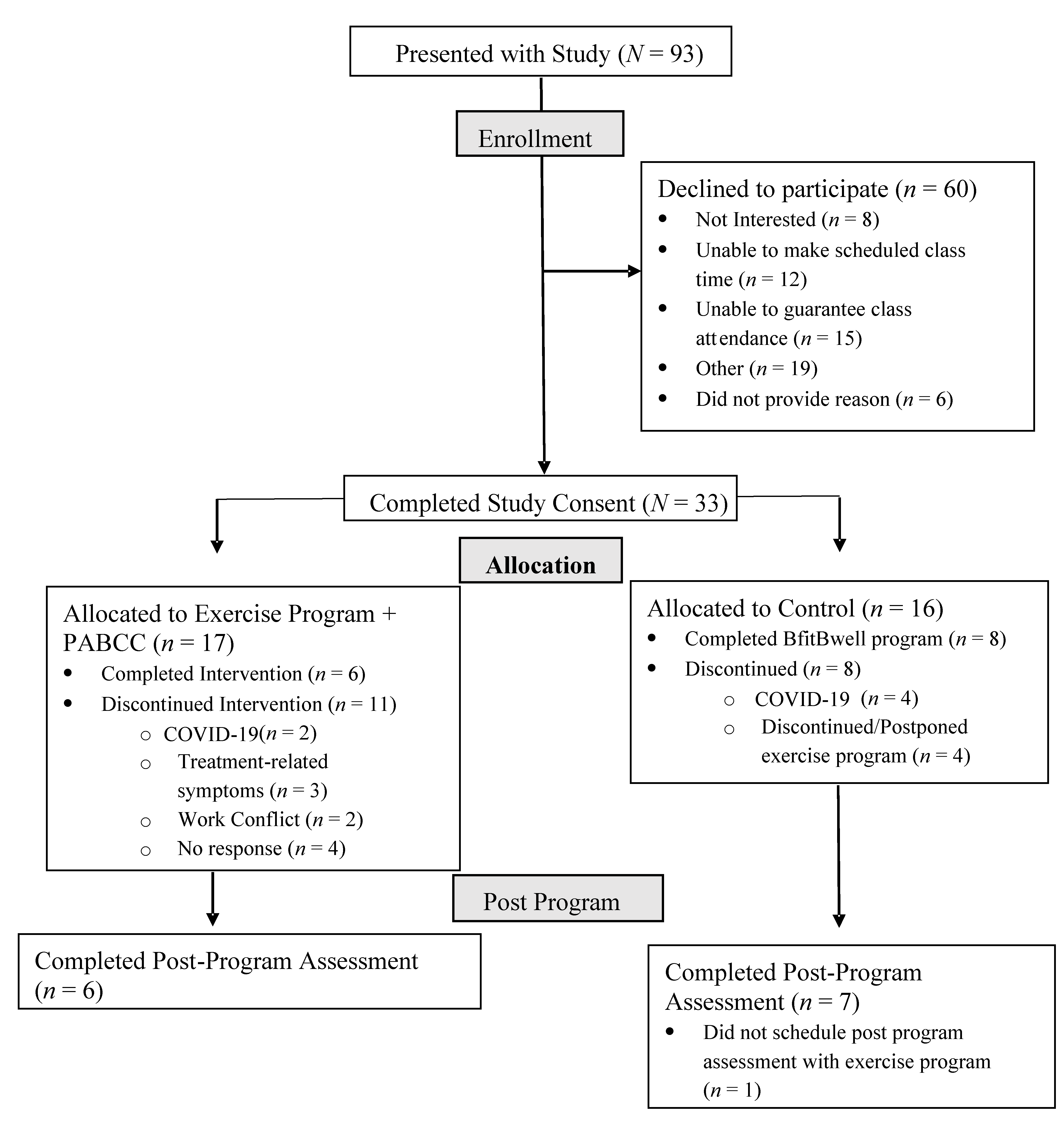
2.1. Study Design
2.2. The Exercise Program (Control)
2.3. The Exercise Program and Physical Activity Behavior Change Counseling (PABCC) Sessions (Intervention)
2.4. Focus Group with Exercise Program Staff
2.5. Measures
2.6. Statistical Analyses
3. Results
3.1. Study Evaluation Questionnaire
“I really liked hearing from [role model]. Testimonials from old participants is inspiring.”[4]
“I thought the sessions were very helpful and reinforced the importance of lifelong exercise…and its benefits on overall happiness.”[2]
“Barriers-identifying and talk about possible solutions. Positive aspects-why exercise is good and helps me feel better.”[3]
“Informal discussion with facilitator and other participant, inspiring visit from [role model], the Bfit alum.”[5]
“You’re [facilitator] really good at bringing people back to topic in a nice and patient way.”[1]
“I like all the interaction.”[3]
“There was a lot of redundancy that made some of the sessions less appealing to me.”[4]
“There were some aspects that seemed formulaic like questions/responses.”[2]
“Be closer to my home HA!”[1]
“Have some of the sessions via Skype or Zoom to avoid having to drive to Anschutz.”[5]
“Schedule it so that it could be done remotely so it wouldn’t complicate my schedule.”[3]
3.2. Focus Group with Exercise Program Staff Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Cancer Society, Cancer Treatment and Survivorship Facts and Figures 2019–2021. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-treatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2019-2021.pdf (accessed on 10 November 2019).
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musanti, R.; Murley, B. Community-Based Exercise Programs for Cancer Survivors. Clin. J. Oncol. Nurs. 2016, 20, S25–S30. [Google Scholar] [CrossRef] [PubMed]
- Swartz, M.C.; Lewis, Z.H.; Lyons, E.J.; Jennings, K.; Middleton, A.; Deer, R.R.; Arnold, D.; Dresser, K.; Ottenbacher, K.J.; Goodwin, J.S. Effect of Home- and Community-Based Physical Activity Interventions on Physical Function Among Cancer Survivors: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 1652–1665. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.L.; Cartmel, B.; Harrigan, M.; Li, F.; Sanft, T.; Shockro, L.; O’Connor, K.; Campbell, N.; Tolaney, S.M.; Mayer, E.L.; et al. Effect of the LIVESTRONG at the YMCA exercise program on physical activity, fitness, quality of life, and fatigue in cancer survivors. Cancer 2017, 123, 1249–1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Covington, K.R.; Hidde, M.C.; Pergolotti, M.; Leach, H.J. Community-based exercise programs for cancer survivors: A scoping review of practice-based evidence. Support. Care Cancer 2019, 27, 4435–4450. [Google Scholar] [CrossRef] [PubMed]
- Grimmett, C.; Corbett, T.; Brunet, J.; Shepherd, J.; Pinto, B.M.; May, C.R.; Foster, C. Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 37. [Google Scholar] [CrossRef] [Green Version]
- Spark, L.C.; Reeves, M.M.; Fjeldsoe, B.S.; Eakin, E.G. Physical activity and/or dietary interventions in breast cancer survivors: A systematic review of the maintenance of outcomes. J. Cancer Surviv. 2013, 7, 74–82. [Google Scholar] [CrossRef]
- Turner, R.R.; Steed, L.; Quirk, H.; Greasley, R.U.; Saxton, J.M.; Taylor, S.J.; Rosario, D.J.; Thaha, M.A.; Bourke, L. Interventions for promoting habitual exercise in people living with and beyond cancer. Cochrane Database Syst. Rev. 2018, 9, CD010192. [Google Scholar] [CrossRef] [PubMed]
- Stacey, F.G.; James, E.L.; Chapman, K.; Courneya, K.S.; Lubans, D.R. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J. Cancer Surviv. 2015, 9, 305–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marker, R.J.; Cox-Martin, E.; Jankowski, C.M.; Purcell, W.T.; Peters, J.C. Evaluation of the effects of a clinically implemented exercise program on physical fitness, fatigue, and depression in cancer survivors. Support. Care Cancer 2018, 26, 1861–1869. [Google Scholar] [CrossRef]
- Rogers, L.Q.; Courneya, K.S.; Anton, P.M.; Hopkins-Price, P.; Verhulst, S.; Vicari, S.K.; Robbs, R.S.; Mocharnuk, R.; McAuley, E. Effects of the BEAT Cancer physical activity behavior change intervention on physical activity, aerobic fitness, and quality of life in breast cancer survivors: A multicenter randomized controlled trial. Breast Cancer Res. Treat. 2015, 149, 109–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, L.Q.; McAuley, E.; Anton, P.M.; Courneya, K.S.; Vicari, S.; Hopkins-Price, P.; Verhulst, S.; Mocharnuk, R.; Hoelzer, K. Better exercise adherence after treatment for cancer (BEAT Cancer) study: Rationale, design, and methods. Contemp. Clin. Trials 2012, 33, 124–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarons, G.A.; Sklar, M.; Mustanski, B.; Benbow, N.; Brown, C.H. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implement. Sci. 2017, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- McAuley, E. Self-efficacy and the maintenance of exercise participation in older adults. J. Behav. Med. 1993, 16, 103–113. [Google Scholar] [CrossRef]
- McAuley, E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J. Behav. Med. 1992, 15, 65–88. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Shephard, R.J. A simple method to assess exercise behavior in the community. Can. J. Appl. Sport Sci. 1985, 10, 141–146. [Google Scholar] [PubMed]
- Amireault, S.; Godin, G.; Lacombe, J.; Sabiston, C.M. Validation of the Godin-Shephard Leisure-Time Physical Activity Questionnaire classification coding system using accelerometer assessment among breast cancer survivors. J. Cancer Surviv. 2015, 9, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Amireault, S.; Godin, G.; Lacombe, J.; Sabiston, C.M. The use of the Godin-Shephard Leisure-Time Physical Activity Questionnaire in oncology research: A systematic review. BMC Med. Res. Methodol. 2015, 15, 60. [Google Scholar] [CrossRef] [Green Version]
- Vaismoradi, M.; Jones, J.; Turunen, H.; Snelgrove, S. Theme development in qualitative content analysis and thematic analysis. J. Nurs. Educ. Pract. 2016, 6, 100. [Google Scholar] [CrossRef] [Green Version]
- Saldana, J. The Coding Manual for Qualitative Researchers; Sage: Los Angeles, CA, USA, 2009. [Google Scholar]
- Beidas, R.S.; Paciotti, B.; Barg, F.; Branas, A.R.; Brown, J.C.; Glanz, K.; DeMichele, A.; DiGiovanni, L.; Salvatore, D.; Schmitz, K.H. A hybrid effectiveness-implementation trial of an evidence-based exercise intervention for breast cancer survivors. J. Natl. Cancer Inst. Monogr. 2014, 50, 338–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, M.A.; Bayes, S.; Newton, R.U.; Zissiadis, Y.; Spry, N.A.; Taaffe, D.R.; Hart, N.H.; Davis, M.; Eiszele, A.; Galvão, D.A. We have the program, what now? Development of an implementation plan to bridge the research-practice gap prevalent in exercise oncology. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 128. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice With a 20-Year Review. Front. Public Health 2019, 7, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, C.M.; Dennehy, C.A.; Roozeboom, M.; Carter, S.D. A model program: Exercise intervention for cancer rehabilitation. Integr. Cancer Ther. 2002, 1, 76–82. [Google Scholar] [CrossRef] [PubMed]
- RE-AIM. Available online: www.RE-AIM.org (accessed on 27 November 2021).
- Qu, H.; Shewchuk, R.; Hu, X.; Baumann, A.A.; Martin, M.Y.; Pisu, M.; Oster, R.A.; Rogers, L.Q. Input from multiple stakeholder levels prioritizes targets for improving implementation of an exercise intervention for rural women cancer survivors. Implement. Sci. Commun. 2020, 1, 97. [Google Scholar] [CrossRef] [PubMed]
- Rogers, L.Q.; Goncalves, L.; Martina, M.Y.; Pisu, M.; Smith, T.L.; Hessong, D.; Oster, R.A.; Qu, H.Y.; Shewchuk, R.; Iqbal, F.; et al. Beyond efficacy: A qualitative organizational perspective on key implementation science constructs important to physical activity intervention translation to rural community cancer care sites. J. Cancer Surviv. 2019, 13, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Who | What | How | |
|---|---|---|---|
| Acceptability | Participants | Factors influencing study participation | Number who enrolled in study out of number offered, and reasons for declining to participate |
| Acceptability | Participants | Adherence to PABCC sessions | Attendance tracking |
| Acceptability | Participants | Perceptions of delivery, facilitator, content, time burden, etc. | Study evaluation questionnaire including closed (i.e., Likert scale) and open-ended questions completed post-program |
| Feasibility | Participants | Representativeness | Compare study participant characteristics (i.e., sex, age, diagnosis, current treatment status, etc.) to previous participants enrolled in BfitBwell |
| Feasibility | Study Coordinator | Adaptations to PABCC sessions, time, costs | Tracking any changes to slides and handouts; hours training on study protocol and delivering PABCC sessions; costs |
| Feasibility | Study Coordinator | Process Fidelity (i.e., were the PABCC sessions delivered as planned) | Fidelity checklist completed after every PABCC session |
| Feasibility and Acceptability | Exercise Program Staff | Session content, delivery modality, staff training/time, appropriateness of perceived fit with current program, barriers to implementation, intent to continue | Focus Group |
| Study Participants N = 33 a | Exercise Program Registry N = 524 a | |
|---|---|---|
| n (%) | ||
| Sex | ||
| Female | 21 (63.6%) | 308 (63.6%) |
| Male | 12 (36.4%) | 176 (36.4%) |
| Race | ||
| Asian | 1 (3.1%) | 19 (4.3%) |
| Black/African American | 1 (3.1%) | 21 (4.7%) |
| White | 30 (93.8%) | 373 (84.2%) |
| Cancer Diagnosis | ||
| Breast | 11 (39.3%) | 141 (30.6%) |
| Hematological | 5 (17.9%) | 38 (8.2%) |
| Ovarian | 2 (7.1%) | 15 (3.3%) |
| Prostate | 2 (7.1%) | 37 (8%) |
| Other | 8 (28.6%) | 230 (49.9%) |
| On Treatment during Program | ||
| Yes | 21 (63.6%) | 316 (64.2%) |
| No | 12 (36.4%) | 175 (35.6%) |
| Mean ± SD | ||
| Age (years) | 54.3 ± 12.4 | 55.5 ± 14.1 |
| Body Mass Index (kg/m2) | 28.2 ± 7.2 | 26.9 ± 6.2 |
| Exercise Program + PABCC (n = 6) | Control (n = 7) | |||
|---|---|---|---|---|
| Measure | Pre | Post | Pre | Post |
| Exercise Self-Efficacy (ESE) a | 79.2 (27.4) | 64.6 (28.7) | 88.2 (12.6) | 88.5 (14.7) |
| Barriers Self-Efficacy (BARSE) b | 46.5 (20.4) | 56.5 (18.6) | 56.2 (25.8) | 58.6 (26.6) |
| MVPA (minutes per week) | 133.3 (48.0) | 241.7 (160.3) | 232.9 (317.9) | 271.4 (321.1) |
| Question | Answer: Probably Yes, Yes, or Definitely Yes n (%) |
|---|---|
| Did you enjoy the behavior change counseling sessions? | 6 (100%) |
| Was attending the behavior change counseling sessions an added time burden to you? | 5 (83.3%) |
| Do you think attending behavior change counseling sessions improved your ability to continue exercising after the end of the BfitBwell program? | 5 (83.3%) |
| Did the facilitator and group environment of the behavior change counseling sessions provide you with a sense of community and support that you found beneficial? | 6 (100%) |
| Did the facilitator effectively deliver information and generate open discussion? | 6 (100%) |
| After completing discussion sessions, do you feel confident that you have the knowledge and skills to exercise safely and effectively without professional guidance in another setting (e.g., home, fitness center, etc.)? | 6 (100%) |
| Themes and Subthemes | Question(s) | Representative Quotes |
|---|---|---|
| Theme 1: Positive Cancer Survivor Feedback | ||
| Staff believe PABCC is beneficial to program and participants |
|
|
| PABCC sessions align with direction and mission of the facility |
|
|
| Theme 2: Barriers to Implementing PABCC Sessions in the BfitBwell Program | ||
| Staff Capacity |
|
|
| Exercise program interns not suitable for delivering PABCC sessions |
|
|
| Cost to hire new staff |
|
|
| Contribution of additional resources from Cancer Center or Wellness Center |
|
|
| Accessibility to survivors |
|
|
| Theme 3: Alternative PABCC Session Implementation Strategies | ||
| Alternative delivery modality |
|
|
| Current staff optimal delivery personnel |
| |
| Fee for service |
|
|
| Hire intern in alternative field |
|
|
| Theme 4: Collaboration between Healthcare Professionals | ||
| Lack of perceived value of exercise by physicians |
|
|
| Support for PABCC from program advocates and Wellness Center leadership |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGinnis, E.L.; Rogers, L.Q.; Fruhauf, C.A.; Jankowski, C.M.; Crisafio, M.E.; Leach, H.J. Feasibility of Implementing Physical Activity Behavior Change Counseling in an Existing Cancer-Exercise Program. Int. J. Environ. Res. Public Health 2021, 18, 12705. https://doi.org/10.3390/ijerph182312705
McGinnis EL, Rogers LQ, Fruhauf CA, Jankowski CM, Crisafio ME, Leach HJ. Feasibility of Implementing Physical Activity Behavior Change Counseling in an Existing Cancer-Exercise Program. International Journal of Environmental Research and Public Health. 2021; 18(23):12705. https://doi.org/10.3390/ijerph182312705
Chicago/Turabian StyleMcGinnis, Emma L., Laura Q. Rogers, Christine A. Fruhauf, Catherine M. Jankowski, Mary E. Crisafio, and Heather J. Leach. 2021. "Feasibility of Implementing Physical Activity Behavior Change Counseling in an Existing Cancer-Exercise Program" International Journal of Environmental Research and Public Health 18, no. 23: 12705. https://doi.org/10.3390/ijerph182312705
APA StyleMcGinnis, E. L., Rogers, L. Q., Fruhauf, C. A., Jankowski, C. M., Crisafio, M. E., & Leach, H. J. (2021). Feasibility of Implementing Physical Activity Behavior Change Counseling in an Existing Cancer-Exercise Program. International Journal of Environmental Research and Public Health, 18(23), 12705. https://doi.org/10.3390/ijerph182312705






