Organizational Health Literacy in a Hospital—Insights on the Patients’ Perspective
Abstract
1. Introduction
1.1. Concept of Organizational Health Literacy
- Has leadership that makes health literacy integral to its mission, structure, and operations.
- Integrates health literacy into planning, evaluation measures, patient safety, and quality improvement.
- Prepares the workforce to be health literate and monitors progress.
- Includes populations served in the design, implementation, and evaluation of health information and services.
- Meets the needs of populations with a range of health literacy skills while avoiding stigmatization.
- Uses health literacy strategies in interpersonal communications and confirms understanding at all points of contact.
- Provides easy access to health information and services and navigation assistance.
- Designs and distributes print, audiovisual, and social media content that is easy to understand and act on.
- Addresses health literacy in high-risk situations, including care transitions and communications about medicines.
- Communicates clearly what health plans cover and what individuals will have to pay for services.
1.2. Organizational Health Literacy in Hospitals
1.3. Interventions, Barriers, and Facilitators of Organizational Health Literacy in Hospitals
1.4. Research Question
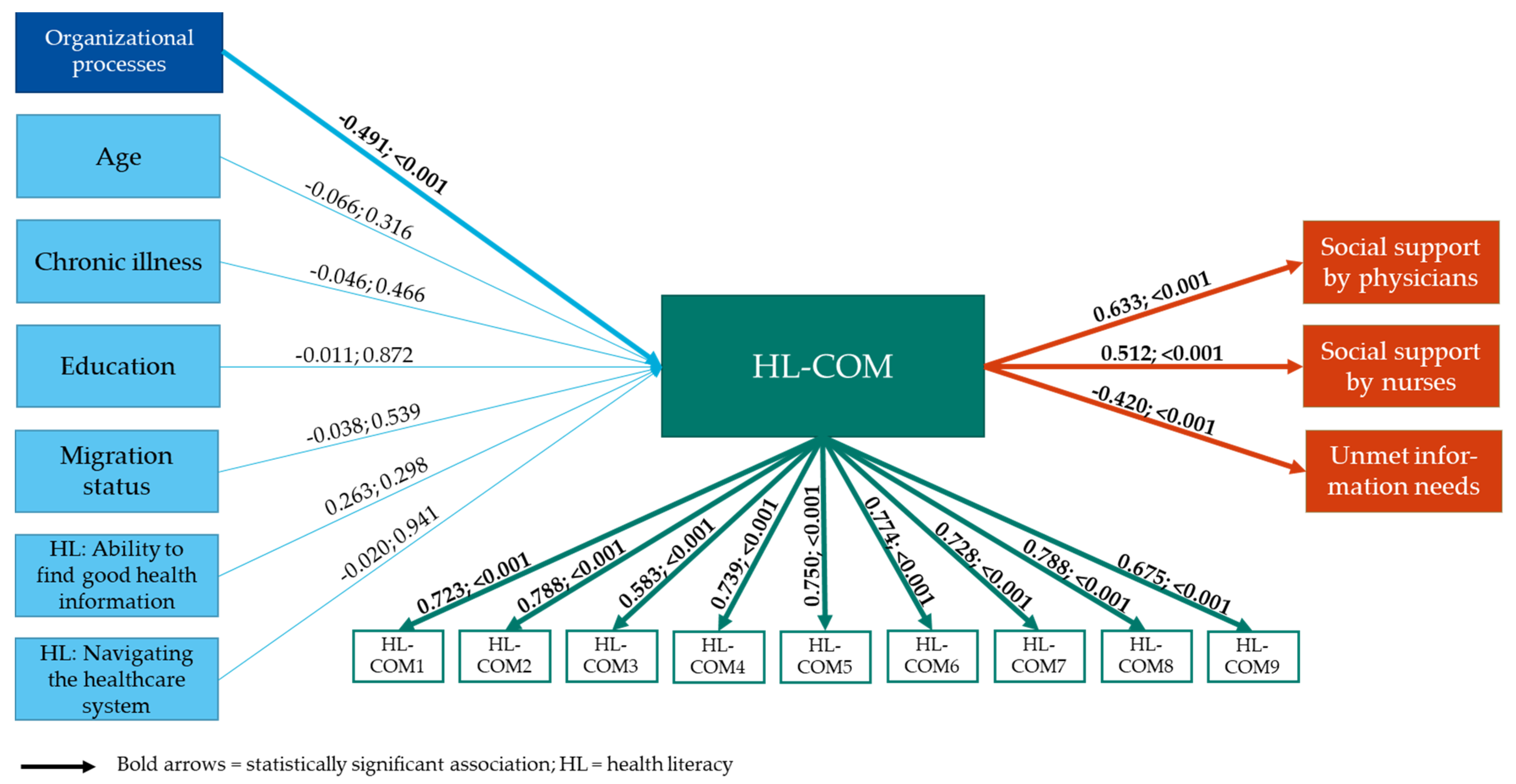
- Are individual patient characteristics, in terms of education, migration background, age, number of chronic diseases, and individual health literacy associated with the patients’ perception of health literacy-sensitive communication?
- Is the hospital’s process organization as perceived by patients associated with health literacy-sensitive communication?
- 3.
- Is health literacy-sensitive communication associated with social support provided by physicians and nurses?
- 4.
- Is health literacy-sensitive communication associated with unmet information needs of patients?
2. Materials and Methods
2.1. Study Site
2.2. Sample
2.3. Recruitment
2.4. Measures
2.5. Data Analysis
2.6. Ethical Considerations and Trial Registration
3. Results
4. Discussion
4.1. Interpretation within the Context of the Wider Literature
4.2. Strengths and Limitations
4.3. Implications for Practice and Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Simonds, S.K. Health Education as Social Policy. Health Educ. Monogr. 1974, 2, 1–10. [Google Scholar] [CrossRef]
- U.S. Department of Education. Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey; NCES 93275; U.S. Department of Education: Washington, DC, USA, 1993.
- HLS-EU Consortium. Comparative Report of Health Literacy in Eight EU Member States, The European Health Literacy Survey HLS-EU. 2012. Available online: http://cpme.dyndns.org:591/adopted/2015/Comparative_report_on_health_literacy_in_eight_EU_member_states.pdf (accessed on 25 September 2021).
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Nationaler Aktionsplan Gesundheitskompetenz. Available online: https://www.nap-gesundheitskompetenz.de/ (accessed on 7 June 2021).
- Ernstmann, N.; Bauer, U.; Berens, E.-M.; Bitzer, E.M.; Bollweg, T.M.; Danner, M.; Dehn-Hindenberg, A.; Dierks, M.L.; Farin, E.; Grobosch, S.; et al. DNVF Memorandum Gesundheitskompetenz (Teil 1)—Hintergrund, Relevanz, Gegenstand und Fragestellungen in der Versorgungsforschung. Gesundheitswesen 2020, 82, e77–e93. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Kilfoyle, K.A.; Vitko, M.; O’Conor, R.; Bailey, S.C. Health Literacy and Women’s Reproductive Health: A Systematic Review. J. Women’s Health 2016, 25, 1237–1255. [Google Scholar] [CrossRef]
- Al Sayah, F.; Majumdar, S.R.; Williams, B.; Robertson, S.; Johnson, J.A. Health Literacy and Health Outcomes in Diabetes: A Systematic Review. J. Gen. Intern. Med. 2013, 28, 444–452. [Google Scholar] [CrossRef]
- Cajita, M.I.; Cajita, T.R.; Han, H.-R. Health Literacy and Heart Failure: A Systematic Review. J. Cardiovasc. Nurs. 2016, 31, 121–130. [Google Scholar] [CrossRef]
- Fleary, S.A.; Joseph, P.; Pappagianopoulos, J.E. Adolescent health literacy and health behaviors: A systematic review. J. Adolesc. 2018, 62, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Bröder, J.; Okan, O.; Bauer, U.; Bruland, D.; Schlupp, S.; Bollweg, T.M.; Saboga-Nunes, L.; Bond, E.; Sørensen, K.; Bitzer, E.-M.; et al. Health literacy in childhood and youth: A systematic review of definitions and models. BMC Public Health 2017, 17, 361. [Google Scholar] [CrossRef]
- Fernández-Gutiérrez, M.; Bas-Sarmiento, P.; Albar-Marín, M.J.; Paloma-Castro, O.; Romero-Sánchez, J.M. Health literacy interventions for immigrant populations: A systematic review. Int. Nurs. Rev. 2018, 65, 54–64. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E.; et al. Health literacy interventions and outcomes: An updated systematic review. Evid. Rep. Technol. Assess. 2011, 199, 1–941. [Google Scholar]
- Liu, H.; Zeng, H.; Shen, Y.; Zhang, F.; Sharma, M.; Lai, W.; Zhao, Y.; Tao, G.; Yuan, J.; Zhao, Y. Assessment Tools for Health Literacy among the General Population: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 1711. [Google Scholar] [CrossRef] [PubMed]
- Med, J.K.P.; Hasan, S.M.; Barnsley, J.; Berta, W.; Fazelzad, R.; Papadakos, C.J.; Giuliani, M.E.; Howell, D. Health literacy and cancer self-management behaviors: A scoping review. Cancer 2018, 124, 4202–4210. [Google Scholar] [CrossRef]
- Buja, A.; Rabensteiner, A.; Sperotto, M.; Grotto, G.; Bertoncello, C.; Cocchio, S.; Baldovin, T.; Contu, P.; Lorini, C.; Baldo, V. Health Literacy and Physical Activity: A Systematic Review. J. Phys. Act. Health 2020, 17, 1259–1274. [Google Scholar] [CrossRef] [PubMed]
- Oldach, B.R.; Katz, M.L. Health literacy and cancer screening: A systematic review. Patient Educ. Couns. 2014, 94, 149–157. [Google Scholar] [CrossRef]
- Geboers, B.; Brainard, J.S.; Loke, Y.K.; Jansen, C.J.M.; Salter, C.; Reijneveld, S.A.; De Winter, A.F. The association of health literacy with adherence in older adults, and its role in interventions: A systematic meta-review. BMC Public Health 2015, 15, 903. [Google Scholar] [CrossRef]
- Mackey, L.M.; Doody, C.; Werner, E.L.; Fullen, B. Self-Management Skills in Chronic Disease Management: What Role Does Health Literacy Have? Med. Decis. Mak. 2016, 36, 741–759. [Google Scholar] [CrossRef]
- Van Der Heide, I.; Rademakers, J.; Schipper, M.; Droomers, M.; Sørensen, K.; Uiters, E. Health literacy of Dutch adults: A cross sectional survey. BMC Public Health 2013, 13, 179. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Schaeffer, D.; Berens, E.-M.; Vogt, D. Health Literacy in the German Population. Dtsch. Aerzteblatt Int. 2017, 114, 53–60. [Google Scholar] [CrossRef]
- Naus, T. Health literacy in EU immigrants: A systematic review and integration of interventions for a comprehensive health literacy strategy. Eur. J. Public Health 2016, 26, 26. [Google Scholar] [CrossRef]
- Berens, E.-M.; Vogt, D.; Messer, M.; Hurrelmann, K.; Schaeffer, D. Health literacy among different age groups in Germany: Results of a cross-sectional survey. BMC Public Health 2016, 16, 1151. [Google Scholar] [CrossRef]
- Kobayashi, L.C.; Wardle, J.; Wolf, M.S.; Von Wagner, C. Aging and Functional Health Literacy: A Systematic Review and Meta-Analysis. J. Gerontol. Ser. B 2016, 71, 445–457. [Google Scholar] [CrossRef] [PubMed]
- Allegrante, J.P.; Wells, M.T.; Peterson, J.C. Interventions to Support Behavioral Self-Management of Chronic Diseases. Annu. Rev. Public Health 2019, 40, 127–146. [Google Scholar] [CrossRef]
- Grady, P.A.; Gough, L.L. Self-Management: A Comprehensive Approach to Management of Chronic Conditions. Am. J. Public Health 2014, 104, e25–e31. [Google Scholar] [CrossRef]
- Liu, L.; Qian, X.; Chen, Z.; He, T. Health literacy and its effect on chronic disease prevention: Evidence from China’s data. BMC Public Health 2020, 20, 690. [Google Scholar] [CrossRef]
- Palumbo, R. Examining the impacts of health literacy on healthcare costs. An evidence synthesis. Health Serv. Manag. Res. 2017, 30, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Rudd, R.E.; Renzulli, D.; Pereira, A.; Daltory, L. Literacy demands in health care settings: The patient perspective. In Understanding Health Literacy: Implications for Medicine and Public Health; Schwartzberg, J.G., VanGeest, J., Wang, C., Eds.; American Medical Association: Chicago, IL, USA, 2005; ISBN 1579476309. [Google Scholar]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Baker, D.W. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006, 21, 878–883. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Organizational Change to Improve Health Literacy: Workshop Summary; National Academies Press: Washington, DC, USA, 2013. [Google Scholar]
- Brach, C.; Keller, D.; Hernandez, L.; Baur, C.; Parker, R.; Dreyer, B.; Schyve, P.; Lemerise, A.J.; Schillinger, D. Ten Attributes of Health Literate Health Care Organizations; NAM Perspectives: Washington, DC, USA, 2012; Volume 2. [Google Scholar] [CrossRef]
- Howe, C.J.; Adame, T.; Lewis, B.; Wagner, T. Original Research: Assessing Organizational Focus on Health Literacy in North Texas Hospitals. AJN, Am. J. Nurs. 2020, 120, 24–33. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Romiti, A.; Ierardi, F.; Innocenti, M.; Del Riccio, M.; Frandi, S.; Bachini, L.; Zanobini, P.; Gemmi, F.; Lorini, C. Health-Literate Healthcare Organizations and Quality of Care in Hospitals: A Cross-Sectional Study Conducted in Tuscany. Int. J. Environ. Res. Public Health 2020, 17, 2508. [Google Scholar] [CrossRef] [PubMed]
- Hayran, O.; Ataç, Ö.; Orhan, Ö. Assessment of Organizational Health Literacy in a Group of Public, Private and University Hospitals in Istanbul. J. Health Syst. Policies (JHESP) 2019, 1, 47–59. [Google Scholar]
- Hayran, O.; Özer, O. Organizational health literacy as a determinant of patient satisfaction. Public Health 2018, 163, 20–26. [Google Scholar] [CrossRef]
- Kowalski, C.; Lee, S.-Y.D.; Schmidt, A.; Wesselmann, S.; Wirtz, M.A.; Pfaff, H.; Ernstmann, N. The health literate health care organization 10 item questionnaire (HLHO-10): Development and validation. BMC Health Serv. Res. 2015, 15, 47. [Google Scholar] [CrossRef]
- Zanobini, P.; Lorini, C.; Baldasseroni, A.; Dellisanti, C.; Bonaccorsi, G. A Scoping Review on How to Make Hospitals Health Literate Healthcare Organizations. Int. J. Environ. Res. Public Health 2020, 17, 1036. [Google Scholar] [CrossRef] [PubMed]
- Farmanova, E.; Bonneville, L.; Bouchard, L. Organizational Health Literacy: Review of Theories, Frameworks, Guides, and Implementation Issues. Inq. J. Health Care Organ. Provis. Financ. 2018, 55, 46958018757848. [Google Scholar] [CrossRef]
- Kaper, M.; Sixsmith, J.; Meijering, L.; Vervoordeldonk, J.; Doyle, P.; Barry, M.M.; De Winter, A.F.; Reijneveld, S.A. Implementation and Long-Term Outcomes of Organisational Health Literacy Interventions in Ireland and The Netherlands: A Longitudinal Mixed-Methods Study. Int. J. Environ. Res. Public Health 2019, 16, 4812. [Google Scholar] [CrossRef]
- Palumbo, R. Leveraging Organizational Health Literacy to Enhance Health Promotion and Risk Prevention: A Narrative and Interpretive Literature Review. Yale J. Biol. Med. 2021, 94, 115–128. [Google Scholar] [PubMed]
- Meggetto, E.; Kent, F.; Ward, B.; Keleher, H. Factors influencing implementation of organizational health literacy: A realist review. J. Health Organ. Manag. 2020, 34, 385–407. [Google Scholar] [CrossRef]
- Weaver, N.L.; Wray, R.J.; Zellin, S.; Gautam, K.; Jupka, K. Advancing Organizational Health Literacy in Health Care Organizations Serving High-Needs Populations: A Case Study. J. Health Commun. 2012, 17, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Jessup, R.L.; Osborne, R.H.; Buchbinder, R.; Beauchamp, A. Using co-design to develop interventions to address health literacy needs in a hospitalised population. BMC Health Serv. Res. 2018, 18, 989. [Google Scholar] [CrossRef]
- Dietscher, C.; Lorenc, J.; Pelikan, J.M. Piloting of the “Self-Assessment Tool to Investigate the Organizational Health Literacy of Hospitals” following the Vienna Concept of a Health Literate Health Care Organization; Ludwig Boltzmann Institute: Vienna, Austria, 2015. [Google Scholar]
- Trezona, A.; Dodson, S.; Osborne, R.H. Development of the Organisational Health Literacy Responsiveness (Org-HLR) self-assessment tool and process. BMC Health Serv. Res. 2018, 18, 694. [Google Scholar] [CrossRef]
- Ernstmann, N.; Halbach, S.; Kowalski, C.; Pfaff, H.; Ansmann, L. Measuring attributes of health literate health care organizations from the patients’ perspective: Development and validation of a questionnaire to assess health literacy-sensitive communication (HL-COM). Z. Evidenz Fortbild. Qual. Gesundh. 2017, 121, 58–63. [Google Scholar] [CrossRef]
- Feldman-Stewart, D.; Brundage, M.; Tishelman, C. A conceptual framework for patient-professional communication: An application to the cancer context. Psycho-Oncology 2005, 14, 801–809. [Google Scholar] [CrossRef]
- Ansmann, L.; Wirtz, M.A.; Kowalski, C.; Pfaff, H.; Visser, A.; Ernstmann, N. The impact of the hospital work environment on social support from physicians in breast cancer care. Patient Educ. Couns. 2014, 96, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Lubasch, J.; Lee, S.; Kowalski, C.; Beckmann, M.; Pfaff, H.; Ansmann, L. Hospital Processes and the Nurse-Patient Interaction in Breast Cancer Care. Findings from a Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 8224. [Google Scholar] [CrossRef]
- Honavar, S.G. Patient–physician relationship—Communication is the key. Indian J. Ophthalmol. 2018, 66, 1527–1528. [Google Scholar] [CrossRef] [PubMed]
- Caplan, G. Support Systems and Community Mental Health, Lectures on Concept Development; Behavioral Publications: Pasadena, CA, USA, 1974. [Google Scholar]
- Lubasch, J.S.; Voigt-Barbarowicz, M.; Lippke, S.; De Wilde, R.L.; Griesinger, F.; Lazovic, D.; Villegas, P.C.O.; Roeper, J.; Salzmann, D.; Seeber, G.H.; et al. Improving professional health literacy in hospitals: Study protocol of a participatory codesign and implementation study. BMJ Open 2021, 11, e045835. [Google Scholar] [CrossRef]
- Dillman, D.A. Mail and Telephone Surveys: The Total Design Method; John Wiley & Sons: New York, NY, USA, 1978; ISBN 0471215554. [Google Scholar]
- Bradburn, N.M.; Sudman, S.; Wansink, B. Asking questions: The Definitive Guide to Questionnaire Design for Market Research, Political Polls, and Social and Health Questionnaires; John Wiley & Sons: New York, NY, USA, 2004; ISBN 978-0-7879-7088-8. [Google Scholar]
- Groves, R.M.; Fowler, F.J.; Couper, M.P.; Lepkowski, J.M.; Singer, E.; Tourangeau, R. Survey Methodology, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2011; ISBN 9780470465462. [Google Scholar]
- Prüfer, P.; Rexroth, M. Two-phase pretesting. In Querschnitt: Festschrift für Max Kaase; Mohler, P.P., Ed.; ZUMA: Mannheim, Germany, 2000; ISBN 3924220204. [Google Scholar]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [PubMed]
- Nolte, S.; Osborne, R.H.; Dwinger, S.; Elsworth, G.R.; Conrad, M.L.; Rose, M.; Härter, M.; Dirmaier, J.; Zill, J.M. German translation, cultural adaptation, and validation of the Health Literacy Questionnaire (HLQ). PLoS ONE 2017, 12, e0172340. [Google Scholar] [CrossRef]
- Ansmann, L.; Kowalski, C.; Pfaff, H. Ten Years of Patient Surveys in Accredited Breast Centers in North Rhine-Westphalia. Geburtshilfe Frauenheilkd. 2016, 76, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Pfaff, H. (Ed.) The Cologne Patient Questionnaire (CPQ): Development and Validation of a Questionnaire to Assess Patient Involvement as a Therapist; Asgard-Verlag: Sankt Augustin, Germany, 2003; ISBN 3537743718. [Google Scholar]
- Ommen, O.; Wirtz, M.A.; Janssen, C.; Neumann, M.; Ernstmann, N.; Pfaff, H. Validation of a theory-based instrument measuring patient-reported psychosocial care by physicians using a multiple indicators and multiple causes model. Patient Educ. Couns. 2010, 80, 100–106. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Press: New York, NY, USA, 2016; 534p. [Google Scholar]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling, 4th ed.; Routledge Taylor & Francis Group: New York, NY, USA; London, UK, 2016; ISBN 9781138811904. [Google Scholar]
- Ansmann, L.; Kowalski, C.; Ernstmann, N.; Ommen, O.; Pfaff, H. Patients’ perceived support from physicians and the role of hospital characteristics. Int. J. Qual. Health Care 2012, 24, 501–508. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dad, T.; Tighiouart, H.; Lacson, E., Jr.; Meyer, K.B.; Weiner, D.E.; Richardson, M.M. Hemodialysis patient characteristics associated with better experience as measured by the In-center Hemodialysis Consumer Assessment of Healthcare Providers and Systems (ICH CAHPS) survey. BMC Nephrol. 2018, 19, 340. [Google Scholar] [CrossRef]
- Van Der Veer, S.N.; Arah, O.A.; Visserman, E.; Bart, H.A.J.; De Keizer, N.F.; Abu-Hanna, A.; Heuveling, L.M.; Stronks, K.; Jager, K.J. Exploring the relationships between patient characteristics and their dialysis care experience. Nephrol. Dial. Transplant. 2012, 27, 4188–4196. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nowak, M.; Swora, M.; Karbach, U.; Pfaff, H.; Ansmann, L. Associations between hospital structures, processes and patient experiences of preparation for discharge in breast cancer centers: A multilevel analysis. Health Care Manag. Rev. 2021, 46, 98–110. [Google Scholar] [CrossRef]
| Response Options 1 | |||||||
|---|---|---|---|---|---|---|---|
| Item | Content | 1 | 2 | 3 | 4 | Mean Score | |
| HL-COM1 | I was made to feel that it is important for me to understand the information about my disease and treatment. | n a | 9 | 31 | 113 | 53 | 3.03 |
| % | 4.3 | 14.8 | 54.1 | 25.4 | |||
| HL-COM2 | I was asked if I understood all information or documents. | n a | 12 | 47 | 85 | 64 | 2.96 |
| % | 5.7 | 22.5 | 40.7 | 31.6 | |||
| HL-COM3 | Verbal information about my disease and treatment was additionally provided in writing. | n a | 25 | 47 | 67 | 68 | 2.86 |
| % | 12.0 | 22.5 | 32.1 | 32.5 | |||
| HL-COM4 | Terms and abbreviations were explained to me. | n a | 18 | 50 | 99 | 41 | 2.78 |
| % | 8.6 | 23.9 | 47.4 | 19.6 | |||
| HL-COM5 | People spoke slowly and clearly to me. | n a | 5 | 27 | 94 | 82 | 3.21 |
| % | 2.4 | 12.9 | 45.0 | 39.2 | |||
| HL-COM6 | I was encouraged to ask questions if I didn’t understand something. | n a | 10 | 53 | 78 | 67 | 2.97 |
| % | 4.8 | 25.4 | 37.3 | 32.1 | |||
| HL-COM7 | Written materials were additionally explained to me. | n a | 15 | 54 | 94 | 43 | 2.81 |
| % | 7.2 | 25.8 | 45.0 | 20.6 | |||
| HL-COM8 | When signing consent forms, efforts were made to ensure that I understood everything. | n a | 6 | 40 | 92 | 68 | 3.08 |
| % | 2.9 | 19.1 | 44.0 | 32.5 | |||
| HL-COM9 | My results were explained comprehensively to me. | n a | 6 | 37 | 96 | 68 | 3.09 |
| % | 2.9 | 17.7 | 45.9 | 32.5 | |||
| n a | % | ||
|---|---|---|---|
| Sex | Female | 132 | 63.2 |
| Male | 75 | 35.9 | |
| Diverse | 1 | 0.5 | |
| Missing | 1 | 0.5 | |
| Age | 18–29 years | 18 | 8.6 |
| 30–39 years | 19 | 9.1 | |
| 40–49 years | 41 | 19.6 | |
| 50–59 years | 57 | 27.3 | |
| 60 years or older | 74 | 35.4 | |
| Education | Lower secondary school education or less | 41 | 19.6 |
| Intermediate secondary school education | 81 | 38.8 | |
| University entrance qualification | 87 | 41.6 | |
| Migration status | Without | 190 | 90.9 |
| With | 19 | 9.1 | |
| Health insurance status | Public | 164 | 78.5 |
| Public with additional private insurance | 15 | 7.2 | |
| Private | 29 | 13.9 | |
| Other | 1 | 0.5 |
| n a | % | ||
|---|---|---|---|
| Number of chronic diseases | 0 | 50 | 23.9 |
| 1 | 63 | 30.1 | |
| 2 | 55 | 26.3 | |
| 3 | 17 | 8.1 | |
| 4 | 17 | 8.1 | |
| >4 | 7 | 3.4 | |
| Chronic diseases (multiple answers possible) | High blood pressure | 63 | 30.1 |
| Overweight/obesity | 48 | 23.0 | |
| Cancer | 45 | 21.5 | |
| Mental illness | 32 | 15.3 | |
| Cardiovascular disease | 24 | 11.5 | |
| Lung disease (chronic bronchitis/COPD/asthma) | 18 | 8.6 | |
| Arthritis or rheumatism | 16 | 7.7 | |
| Diabetes | 13 | 6.2 | |
| Kidney disease | 7 | 3.3 | |
| Stroke | 4 | 1.9 | |
| Other diseases | 61 | 29.2 | |
| No chronic disease | 52 | 23.9 | |
| Clinical division in which the patient was treated | Oncology | 2 | 1.0 |
| Visceral surgery | 54 | 25.8 | |
| Gynecology | 72 | 34.4 | |
| Orthopedics | 81 | 38.8 | |
| Number of nights spent in hospital | ≤3 | 71 | 33.9 |
| 4–6 | 75 | 35.9 | |
| 7–9 | 39 | 18.7 | |
| >9 | 20 | 8.8 | |
| Missing | 4 | 1.9 |
| Possible Range | Mean | SD 1 | Observed Range | Min | Max | Cronbachs‘ α | |
|---|---|---|---|---|---|---|---|
| Health literacy-sensitive communication | 1–4 | 2.98 | 0.65 | 3.00 | 1.00 | 4.00 | 0.911 |
| Process organization | 1–4 | 1.76 | 0.65 | 3.00 | 1.00 | 4.00 | 0.842 |
| Social support provided by physicians | 1–4 | 3.16 | 0.70 | 3.00 | 1.00 | 4.00 | 0.924 |
| Social support provided by nurses | 1–4 | 3.51 | 0.64 | 2.67 | 1.33 | 4.00 | 0.928 |
| Unmet information needs | 0–7 | 1.59 | 1.92 | 7.00 | 0.00 | 7.00 | - |
| Health literacy: Navigating the healthcare system | 1–5 | 3.63 | 0.57 | 3.17 | 1.67 | 4.83 | 0.833 |
| Health literacy: Ability to find good health information | 1–5 | 3.67 | 0.58 | 3.20 | 1.60 | 4.80 | 0.823 |
| X2 | Df | Cronbachs’ α | RMSEA | SRMR | TLI | CFI | |
|---|---|---|---|---|---|---|---|
| Threshold | ≥0.7 | ≤0.08 | ≤0.08 | ≥0.90 | ≥0.90 | ||
| SEM | 832 | 521 | 0.911 | 0.048 | 0.070 | 0.920 | 0.926 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lubasch, J.S.; Voigt-Barbarowicz, M.; Ernstmann, N.; Kowalski, C.; Brütt, A.L.; Ansmann, L. Organizational Health Literacy in a Hospital—Insights on the Patients’ Perspective. Int. J. Environ. Res. Public Health 2021, 18, 12646. https://doi.org/10.3390/ijerph182312646
Lubasch JS, Voigt-Barbarowicz M, Ernstmann N, Kowalski C, Brütt AL, Ansmann L. Organizational Health Literacy in a Hospital—Insights on the Patients’ Perspective. International Journal of Environmental Research and Public Health. 2021; 18(23):12646. https://doi.org/10.3390/ijerph182312646
Chicago/Turabian StyleLubasch, Johanna Sophie, Mona Voigt-Barbarowicz, Nicole Ernstmann, Christoph Kowalski, Anna Levke Brütt, and Lena Ansmann. 2021. "Organizational Health Literacy in a Hospital—Insights on the Patients’ Perspective" International Journal of Environmental Research and Public Health 18, no. 23: 12646. https://doi.org/10.3390/ijerph182312646
APA StyleLubasch, J. S., Voigt-Barbarowicz, M., Ernstmann, N., Kowalski, C., Brütt, A. L., & Ansmann, L. (2021). Organizational Health Literacy in a Hospital—Insights on the Patients’ Perspective. International Journal of Environmental Research and Public Health, 18(23), 12646. https://doi.org/10.3390/ijerph182312646






