Electronic Health Literacy in Individuals with Chronic Pain and Its Association with Psychological Function
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Sample Description
3.2. Internet Use for Seeking Health Information and eHealth Literacy Skills
3.3. Association between eHealth Literacy Skills, Participants’ Age, and Health-Related Outcomes
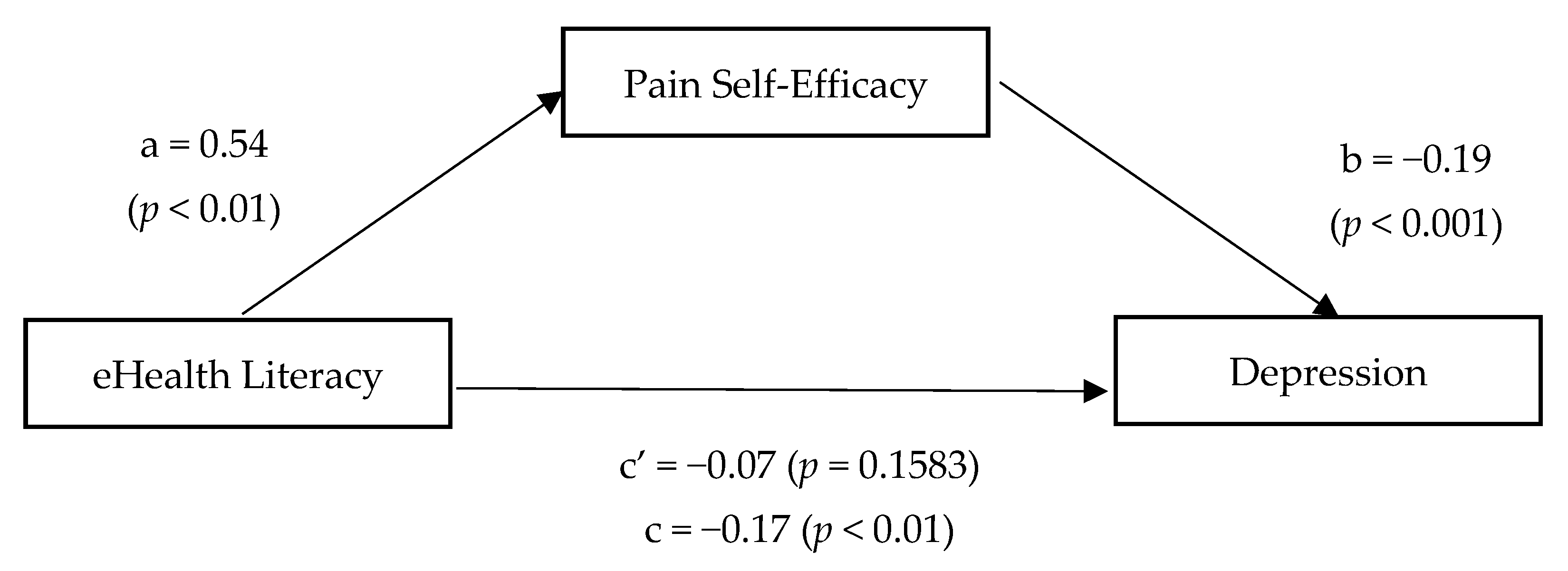
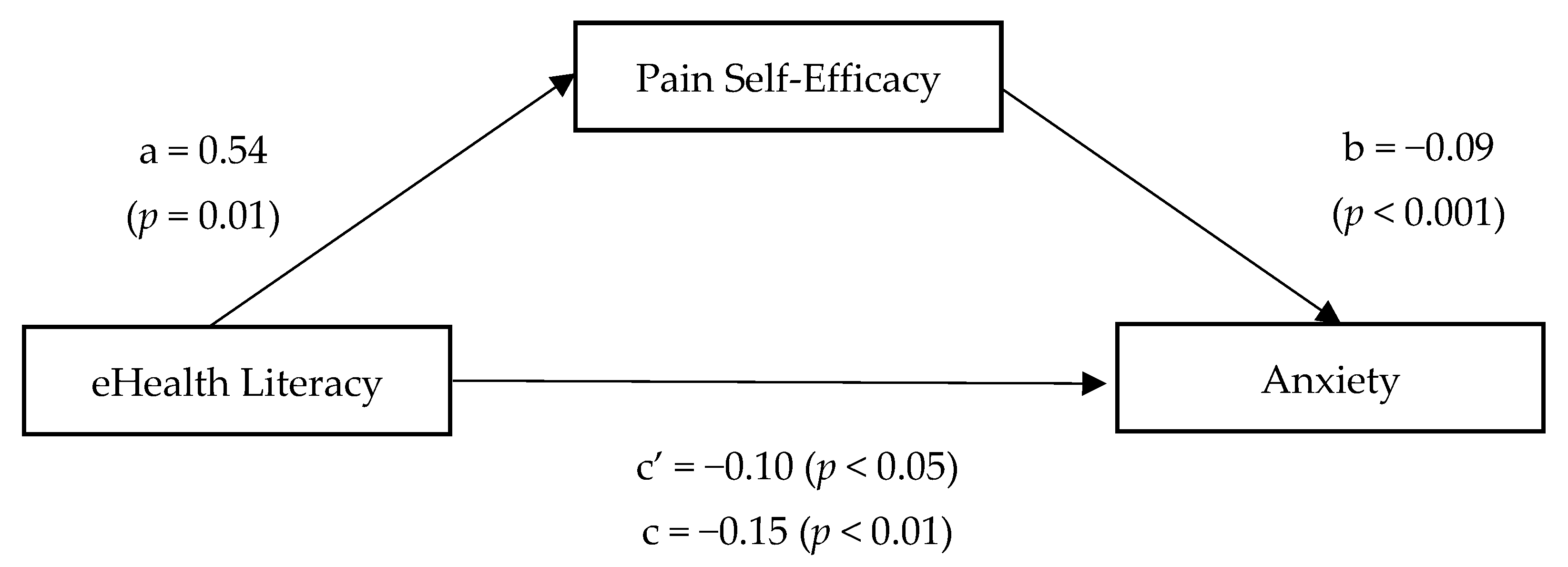
3.4. Self-Efficacy as a Mediator of the Relationship between eHealth Literacy and Health-Related Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abate, K.H.; Abd-Allah, F.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [Green Version]
- Phillips, C.J. The Cost and Burden of Chronic Pain. Rev. Pain 2009, 3, 2–5. [Google Scholar] [CrossRef] [Green Version]
- Henschke, N.; Kamper, S.J.; Maher, C.G. The epidemiology and economic consequences of pain. In Mayo Clinic Proceedings; Elsevier Ltd.: Amsterdam, The Netherlands, 2015; Volume 90, pp. 139–147. [Google Scholar]
- Breivik, H.; Eisenberg, E.; O’Brien, T. The individual and societal burden of chronic pain in Europe: The case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health 2013, 13, 1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finley, C.R.; Chan, D.S.; Garrison, S.; Korownyk, C.; Kolber, M.R.; Campbell, S.; Eurich, D.T.; Lindblad, A.J.; Vandermeer, B.; Allan, G.M. What are the most common conditions in primary care? Systematic review. Can. Fam. Physician 2018, 64, 832–840. [Google Scholar] [PubMed]
- Scascighini, L.; Toma, V.; Dober-Spielmann, S.; Sprott, H. Multidisciplinary treatment for chronic pain: A systematic review of interventions and outcomes. Rheumatology 2008, 47, 670–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serrat, M.; Almirall, M.; Musté, M.; Sanabria-Mazo, J.P.; Feliu-Soler, A.; Méndez-Ulrich, J.L.; Luciano, J.V.; Sanz, A. Effectiveness of a Multicomponent Treatment for Fibromyalgia Based on Pain Neuroscience Education, Exercise Therapy, Psychological Support, and Nature Exposure (NAT-FM): A Pragmatic Randomized Controlled Trial. J. Clin. Med. 2020, 9, 3348. [Google Scholar] [CrossRef]
- Aragonès, E.; López-Cortacans, G.; Caballero, A.; Piñol, J.L.; Sánchez-Rodríguez, E.; Rambla, C.; Tomé-Pires, C.; Miró, J. Evaluation of a multicomponent programme for the management of musculoskeletal pain and depression in primary care: A cluster-randomised clinical trial (the DROP study). BMC Psychiatry 2016, 16, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burns, J.W.; Van Dyke, B.P.; Newman, A.K.; Morais, C.A.; Thorn, B.E. Cognitive behavioral therapy (CBT) and pain education for people with chronic pain: Tests of treatment mechanisms. J. Consult. Clin. Psychol. 2020, 88, 1008–1018. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, A.; Yap, T.; Heaphy, N.; McCullough, M.J. Group pain education is as effective as individual education in patients with chronic temporomandibular disorders. J. Oral Pathol. Med. 2020, 49, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Marris, D.; Theophanous, K.; Cabezon, P.; Dunlap, Z.; Donaldson, M. The impact of combining pain education strategies with physical therapy interventions for patients with chronic pain: A systematic review and meta-analysis of randomized controlled trials. Physiother. Theory Pract. 2019, 37, 461–472. [Google Scholar] [CrossRef]
- Cooper, K.; Smith, B.H.; Hancock, E. Patients’ perceptions of self-management of chronic low back pain: Evidence for enhancing patient education and support. Physiotherapy 2009, 95, 43–50. [Google Scholar] [CrossRef]
- Ziebland, S.; Lavie-Ajayi, M.; Lucius-Hoene, G. The role of the internet for people with chronic pain: Examples from the DIPEx international project. Br. J. Pain 2014, 9, 62–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Boer, M.J.; Versteegen, G.J.; van Wijhe, M. Patients’ use of the Internet for pain-related medical information. Patient Educ. Couns. 2007, 68, 86–97. [Google Scholar] [CrossRef]
- Bailey, S.J.; Lachapelle, D.L.; Lefort, S.M.; Gordon, A.; Hadjistavropoulos, T. Evaluation of chronic pain-related information available to consumers on the internet. Pain Med. 2013, 14, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, T.B.; Haigh, F.; Seabrook, A.; Schug, S.A. The quality of internet-sourced information for patients with chronic pain is poor. Clin. J. Pain 2009, 25, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Norman, C.D.; Skinner, H.A. eHealth literacy: Essential skills for consumer health in a networked world. J. Med. Internet Res. 2006, 8, e9. [Google Scholar] [CrossRef] [PubMed]
- Paige, S.R.; Stellefson, M.; Krieger, J.L.; Anderson-Lewis, C.; Cheong, J.W.; Stopka, C. Proposing a transactional model of eHealth literacy: Concept analysis. J. Med. Internet Res. 2018, 20, e10175. [Google Scholar] [CrossRef] [PubMed]
- Lacey, R.J.; Campbell, P.; Lewis, M.; Protheroe, J. The Impact of Inadequate Health Literacy in a Population with Musculoskeletal Pain. HLRP Health Lit. Res. Pract. 2018, 2, e215–e220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, A.H.; Bakhshaie, J.; Orr, M.F.; Ditre, J.W.; Zvolensky, M.J. Health Literacy, Opioid Misuse, and Pain Experience among Adults with Chronic Pain. Pain Med. 2020, 21, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Mackey, L.M.; Blake, C.; Casey, M.B.; Power, C.K.; Victory, R.; Hearty, C.; Fullen, B.M. The impact of health literacy on health outcomes in individuals with chronic pain: A cross-sectional study. Physiotherapy 2019, 105, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Mackey, L.M.; Blake, C.; Squiers, L.; Casey, M.B.; Power, C.; Victory, R.; Hearty, C.; Fullen, B.M. An investigation of healthcare utilization and its association with levels of health literacy in individuals with chronic pain. Musculoskelet. Care 2019, 17, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Turner, B.J.; Liang, Y.; Rodriguez, N.; Bobadilla, R.; Simmonds, M.J.; Yin, Z. Randomized Trial of a Low-Literacy Chronic Pain Self-Management Program: Analysis of Secondary Pain and Psychological Outcome Measures. J. Pain 2018, 19, 1471–1479. [Google Scholar] [CrossRef]
- Valizadeh-Haghi, S.; Rahmatizadeh, S. eHealth literacy and general interest in using online Health information: A survey among patients with dental diseases. Online J. Public Health Inform. 2018, 10, e219. [Google Scholar] [CrossRef] [PubMed]
- Cherid, C.; Baghdadli, A.; Wall, M.; Mayo, N.E.; Berry, G.; Harvey, E.J.; Albers, A.; Bergeron, S.G.; Morin, S.N. Current level of technology use, health and eHealth literacy in older Canadians with a recent fracture—a survey in orthopedic clinics. Osteoporos. Int. 2020, 31, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Shiferaw, K.B.; Tilahun, B.C.; Endehabtu, B.F.; Gullslett, M.K.; Mengiste, S.A. E-health literacy and associated factors among chronic patients in a low-income country: A cross-sectional survey. BMC Med. Inform. Decis. Mak. 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hoogland, A.I.; Mansfield, J.; Lafranchise, E.A.; Bulls, H.W.; Johnstone, P.A.; Jim, H.S.L. eHealth literacy in older adults with cancer. J. Geriatr. Oncol. 2020, 11, 1020–1022. [Google Scholar] [CrossRef] [PubMed]
- Hsu, W.C. The effect of age on electronic health literacy: Mixed-method study. J. Med. Internet Res. 2019, 21, e11480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.Y.; Ganji, M.; Griffiths, M.D.; Bravell, M.E.; Broström, A.; Pakpour, A.H. Mediated effects of insomnia, psychological distress and medication adherence in the association of eHealth literacy and cardiac events among Iranian older patients with heart failure: A longitudinal study. Eur. J. Cardiovasc. Nurs. 2020, 19, 155–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filabadi, Z.; Estebsari, F.; Milani, A.; Feizi, S.; Nasiri, M. Relationship between electronic health literacy, quality of life, and self-efficacy in Tehran, Iran: A community-based study. J. Educ. Health Promot. 2020, 9, 175. [Google Scholar] [CrossRef]
- Yang, S.C.; Luo, Y.F.; Chiang, C.H. The associations among individual factors, ehealth literacy, and health-promoting lifestyles among college students. J. Med. Internet Res. 2017, 19, e15. [Google Scholar] [CrossRef]
- Mitsutake, S.; Shibata, A.; Ishii, K.; Oka, K. Associations of eHealth literacy with health behavior among adult internet users. J. Med. Internet Res. 2016, 18, e192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pourrazavi, S.; Kouzekanani, K.; Bazargan-Hejazi, S.; Shaghaghi, A.; Hashemiparast, M.; Fathifar, Z.; Allahverdipour, H. Theory-based E-health literacy interventions in older adults: A systematic review. Arch. Public Heal. 2020, 78, 72. [Google Scholar] [CrossRef] [PubMed]
- Rabenbauer, L.M.; Mevenkamp, N. Factors in the Effectiveness of e-Health Interventions for Chronic Back Pain: How Self-Efficacy Mediates e-Health Literacy and Healthy Habits. Telemed. Health 2020, 27, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Erdfelder, E.; Faul, F.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef]
- Norman, C.D.; Skinner, H.A. eHEALS: The eHealth literacy scale. J. Med. Internet Res. 2006, 8, e27. [Google Scholar] [CrossRef] [Green Version]
- Richtering, S.S.; Hyun, K.; Neubeck, L.; Coorey, G.; Chalmers, J.; Usherwood, T.; Peiris, D.; Chow, C.K.; Redfern, J. eHealth Literacy: Predictors in a Population With Moderate-to-High Cardiovascular Risk. JMIR Hum. Factors 2017, 4, e4. [Google Scholar] [CrossRef] [PubMed]
- Shiferaw, K.B.; Mehari, E.A. Internet use and ehealth literacy among health-care professionals in a resource limited setting: A cross-sectional survey. Adv. Med. Educ. Pract. 2019, 10, 563–570. [Google Scholar] [CrossRef] [Green Version]
- Brørs, G.; Wentzel-Larsen, T.; Dalen, H.; Hansen, T.B.; Norman, C.D.; Wahl, A.; Norekvål, T.M. Psychometric properties of the norwegian version of the electronic health literacy scale (eheals) among patients after percutaneous coronary intervention: Cross-sectional validation study. J. Med. Internet Res. 2020, 22, e1731. [Google Scholar] [CrossRef] [PubMed]
- Paige, S.R.; Krieger, J.L.; Stellefson, M.; Alber, J.M. eHealth literacy in chronic disease patients: An item response theory analysis of the eHealth literacy scale (eHEALS). Patient Educ. Couns. 2017, 100, 320–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.Y.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. Psychometric Evaluation of the Persian eHealth Literacy Scale (eHEALS) Among Elder Iranians With Heart Failure. Eval. Health Prof. 2020, 43, 222–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paramio, G.; Almagro, B.J.; Hernando, Á.; Aguaded, J.I. Validación de la escala eHealth Literacy (eHEALS) en población universitaria española. Rev. Esp. Salud Publica 2015, 89, 329–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terol-Cantero, M.; Cabrera-Perona, V.; Martín-Aragón, M. Revisión de estudios de la Escala de Ansiedad y Depresión Hospitalaria (HAD) en muestras españolas. Ann. Psicol. 2015, 31, 494–503. [Google Scholar] [CrossRef] [Green Version]
- Nicholas, M.K. The pain self-efficacy questionnaire: Taking pain into account. Eur. J. Pain 2007, 11, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Castarlenas, E.; Solé, E.; Galán, S.; Racine, M.; Jensen, M.P.; Miró, J. Construct Validity and Internal Consistency of the Catalan Version of the Pain Self-Efficacy Questionnaire in Young People With Chronic Pain. Eval. Health Prof. 2020, 43, 213–221. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Ryan, K.M. Pain assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. 1994, 23, 129–138. [Google Scholar]
- Ger, L.P.; Ho, S.T.; Sun, W.Z.; Wang, M.S.; Cleeland, C.S. Validation of the brief pain inventory in a Taiwanese population. J. Pain Symptom Manag. 1999, 18, 316–322. [Google Scholar] [CrossRef]
- Majedi, H.; Dehghani, S.S.; Soleyman-Jahi, S.; Emami Meibodi, S.A.; Mireskandari, S.M.; Hajiaghababaei, M.; Tafakhori, A.; Mendoza, T.R.; Cleeland, C.S. Validation of the Persian Version of the Brief Pain Inventory (BPI-P) in Chronic Pain Patients. J. Pain Symptom Manag. 2017, 54, 132–138.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira, K.A.; Teixeira, M.J.; Mendonza, T.R.; Cleeland, C.S. Validation of brief pain inventory to Brazilian patients with pain. Support. Care Cancer 2011, 19, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Miró, J.; Gertz, K.J.; Carter, G.T.; Jensen, M.P. Pain location and functioning in persons with spinal cord injury. PM R 2014, 6, 690–697. [Google Scholar] [CrossRef] [Green Version]
- Badia, X.; Muriel, C.; Gracia, A.; Núñez-Olarte, J.M.; Perulero, N.; Gálvez, R.; Carulla, J.; Cleeland, C.S. Validación española del cuestionario Brief Pain Inventory en pacientes con dolor de causa neoplásica. Med. Clin. 2003, 120, 52–59. [Google Scholar] [CrossRef]
- Ares, J.D.A.; Prado, L.M.C.; Verdecho, M.A.C.; Villanueva, L.P.; Hoyos, M.D.V.; Herdman, M.; Lugilde, S.T.; Rivera, I.V. Validation of the Short Form of the Brief Pain Inventory (BPI-SF) in Spanish Patients with Non-Cancer-Related Pain. Pain Pract. 2015, 15, 643–653. [Google Scholar] [CrossRef]
- Expósito-Vizcaíno, S.; Sánchez-Rodríguez, E.; Miró, J. The role of physical, cognitive and social factors in pain interference with activities of daily living among individuals with chronic cancer pain. Eur. J. Cancer Care 2020, 29, e13203. [Google Scholar] [CrossRef] [PubMed]
- Rouvinen, H.; Jokiniemi, K.; Sormunen, M.; Turunen, H. Internet use and health in higher education students: A scoping review. Health Promot. Int. 2021. [Google Scholar] [CrossRef]
- Milne, R.A.; Puts, M.T.E.; Papadakos, J.; Le, L.W.; Milne, V.C.; Hope, A.J.; Catton, P.; Giuliani, M.E. Predictors of High eHealth Literacy in Primary Lung Cancer Survivors. J. Cancer Educ. 2015, 30, 685–692. [Google Scholar] [CrossRef]
- Choi, M. Association of ehealth use, literacy, informational social support, and health-promoting behaviors: Mediation of health self-efficacy. Int. J. Environ. Res. Public Health 2020, 17, 7890. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.H.; Yehle, K.S.; Plake, K.S.; Rathman, L.D.; Heinle, J.W.; Frase, R.T.; Anderson, J.G.; Bentley, J. The role of health literacy, depression, disease knowledge, and self-efficacy in self-care among adults with heart failure: An updated model. Hear. Lung 2020, 49, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Geboers, B.; De Winter, A.F.; Luten, K.A.; Jansen, C.J.M.; Reijneveld, S.A. The association of health literacy with physical activity and nutritional behavior in older adults, and its social cognitive mediators. J. Health Commun. 2014, 19, 61–76. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Brennan, D.S.; Parker, E.J.; Mills, H.; Jamieson, L. Does self-efficacy mediate the effect of oral health literacy on self-rated oral health in an Indigenous population? J. Public Health Dent. 2016, 76, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Yu, X. The mediating effect of self-efficacy on the relationship between health literacy and health status in Korean older adults: A short report. Aging Ment. Health 2010, 14, 870–873. [Google Scholar] [CrossRef] [PubMed]
- Xesfingi, S.; Vozikis, A. eHealth Literacy: In the Quest of the Contributing Factors. Interact. J. Med. Res. 2016, 5, e16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, X.; Zhang, R. Association Between eHealth Literacy in Online Health Communities and Patient Adherence: Cross-sectional Questionnaire Study. J. Med. Internet Res. 2021, 23, e14908. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E. eHealth literacy: Extending the digital divide to the realm of health information. J. Med. Internet Res. 2012, 14, e19. [Google Scholar] [CrossRef] [PubMed]
| Descriptive Characteristic | ||
|---|---|---|
| Participants (N) | 161 | |
| Mean age in years (range; SD) | 44.63 (24–68; 9.55) | |
| Gender, N (%) | Female | 154 (96) |
| Male | 7 (4) | |
| Education level, N (%) | Did not complete primary education | 63 (39) |
| Completed primary education | 20 (12) | |
| Completed secondary education | 52 (32) | |
| Completed bachelor’s degree | 17 (11) | |
| Post-bachelor education | 4 (3) | |
| On medical leave due to pain? N (%) | No | 113 (70) |
| Yes | 48 (30) | |
| Have a specific pain diagnoses? N (%) | No | 17 (11) |
| Yes | 144 (89) | |
| Location of the most frequent chronic pain, N (%) | Head, face, and mouth | 11 (7) |
| Cervical region | 17 (11) | |
| Upper shoulder and upper limbs | 48 (30) | |
| Thoracic region | 4 (3) | |
| Abdominal region | 3 (2) | |
| Lower back, lumbar spine, sacrum, and coccyx | 57 (35) | |
| Lower limbs | 2 (1) | |
| Pelvic region | 2 (1) | |
| Anal, perineal, and genital region | 17 (11) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castarlenas, E.; Sánchez-Rodríguez, E.; Roy, R.; Tomé-Pires, C.; Solé, E.; Jensen, M.P.; Miró, J. Electronic Health Literacy in Individuals with Chronic Pain and Its Association with Psychological Function. Int. J. Environ. Res. Public Health 2021, 18, 12528. https://doi.org/10.3390/ijerph182312528
Castarlenas E, Sánchez-Rodríguez E, Roy R, Tomé-Pires C, Solé E, Jensen MP, Miró J. Electronic Health Literacy in Individuals with Chronic Pain and Its Association with Psychological Function. International Journal of Environmental Research and Public Health. 2021; 18(23):12528. https://doi.org/10.3390/ijerph182312528
Chicago/Turabian StyleCastarlenas, Elena, Elisabet Sánchez-Rodríguez, Rubén Roy, Catarina Tomé-Pires, Ester Solé, Mark P. Jensen, and Jordi Miró. 2021. "Electronic Health Literacy in Individuals with Chronic Pain and Its Association with Psychological Function" International Journal of Environmental Research and Public Health 18, no. 23: 12528. https://doi.org/10.3390/ijerph182312528
APA StyleCastarlenas, E., Sánchez-Rodríguez, E., Roy, R., Tomé-Pires, C., Solé, E., Jensen, M. P., & Miró, J. (2021). Electronic Health Literacy in Individuals with Chronic Pain and Its Association with Psychological Function. International Journal of Environmental Research and Public Health, 18(23), 12528. https://doi.org/10.3390/ijerph182312528







