Evaluation of the Effects of Telepsychotherapy in the Treatment and Prevention of Eating Disorders in Adolescents
Abstract
1. Introduction
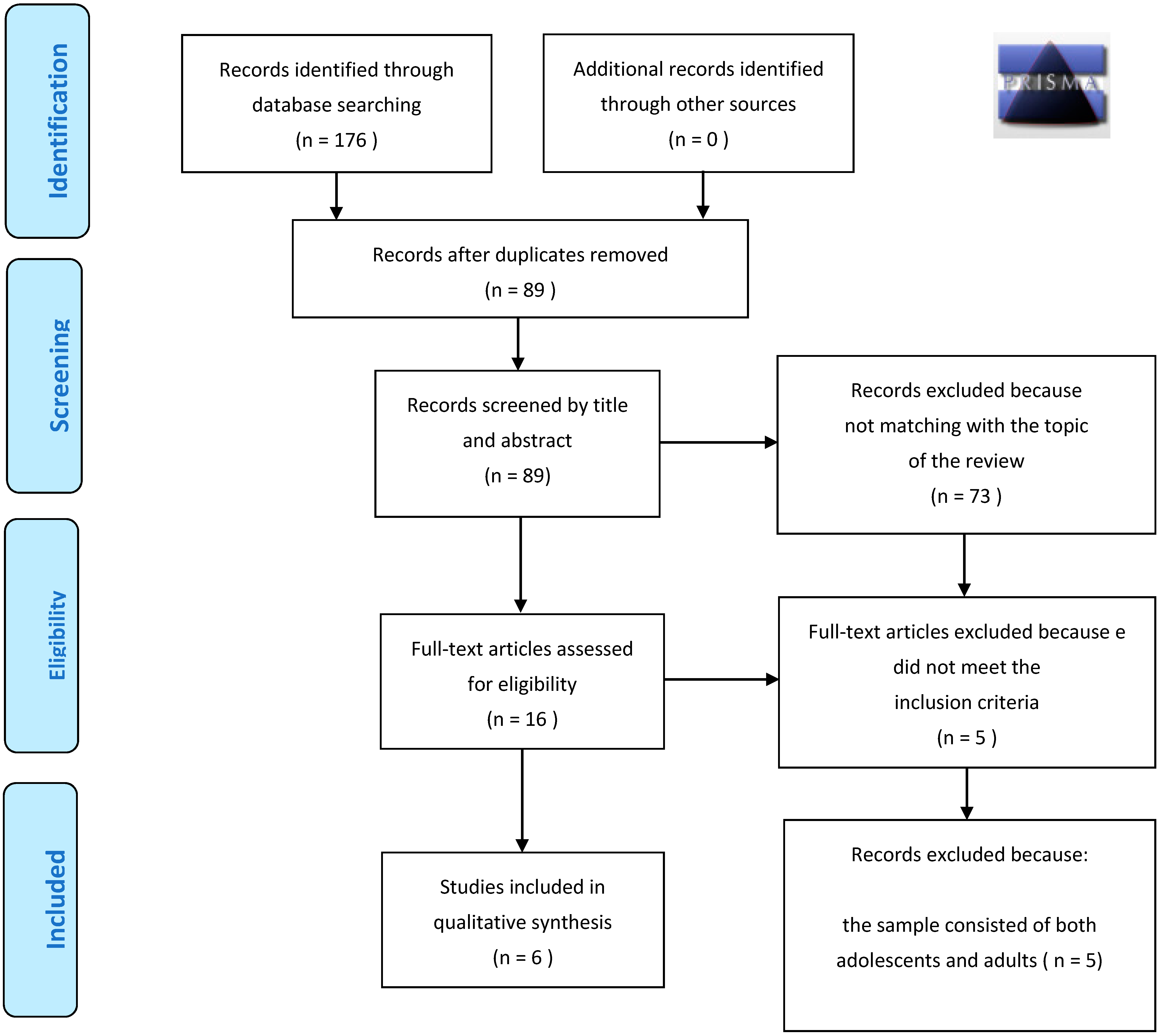
2. Materials and Methods
2.1. Research Object
2.2. Search Strategy
2.3. Elegibility Criteria
- Participants: adolescents diagnosed with eating disorders, as the main recipients of the interventions, and adolescents who met the risk criteria for anorexia, bulimia and binge eating disorder.
- Intervention: included interventions using telepsychotherapy for the delivery of therapeutic treatments (CBT and FBT) through video conferencing, smartphone apps, online questionnaires for qualitative research, a web-based prevention program for parents of adolescents who met the risk criteria for anorexia, bulimia and binge eating disorderAN.
- Comparison: therapy as usual (TAU), wait-list control condition.
- Outcomes: body image satisfaction was considered for the results; increased body weight in an; reduction in psychopathological symptoms of the eating disorder (deliberate and planned weight control, food restriction due to weight concerns, excessive frequency of diets, vomiting, fasting, use of laxatives, tablets to lose weight, skipping meals) and secondary symptoms (anxiety, depression, self-esteem); reduction in anorexia, bulimia and binge eating disorderAN risk factors in prevention interventions.
- Study design: clinical trials, randomized clinical trial, review, systematic review, books and document.
2.4. Data Extraction
3. Results
3.1. Schemes
3.1.1. Heinicke et al. (2007)
3.1.2. Anastasiadou et al. (2020)
3.1.3. Anderson et al. (2017)
3.1.4. Jacobi et al. (2018)
3.1.5. Yaffa et al. (2021)
3.1.6. Wood S. et al. (2020)
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Global Observatory for eHealth. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Moessner, M.; Minarik, C.; Özer, F.; Bauer, S. Can an internet-based program for the prevention and early intervention in eating disorders facilitate access to conventional professional healthcare? J. Ment. Health. 2016, 25, 441–447. [Google Scholar] [CrossRef]
- Balestra, M. Telehealth and legal implications for nurse practitioners. J. Nurse Pract. 2018, 14, 33–39. [Google Scholar] [CrossRef]
- Sweeney, G.M.; Donovan, C.L.; March, S.; Forbes, Y. Logging into therapy: Adolescent perceptions of online therapies for mental health problems. Internet Interv. 2016, 15, 93–99. [Google Scholar] [CrossRef]
- Bauer, S.; Papezova, H.; Chereches, R.; Caselli, G.; McLoughlin, O.; Szumska, I.; Furth, E.; Ozer, F.; Moessner, M. Advances in the prevention and early intervention of eating disorders: The potential of internet-delivered approaches. Ment. Health Prev. 2013, 1, 26–32. [Google Scholar] [CrossRef]
- Bauer, S.; Moessner, M. Harnessing the power of technology for the treatment and prevention of eating disorders. Int. J. Eat. Disord. 2013, 46, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Shingleton, R.M.; Richards, L.K.; Thompson-Brenner, H. Using technology within the treatment of eating disorders: A clinical practice review. Psychotherapy 2013, 50, 576–582. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marks, I.; Cavanagh, K. Computer-aided psychological treatments: Evolving issues. Annu. Rev. Clin. Psychol. 2009, 5, 121–141. [Google Scholar] [CrossRef]
- Berger, T.; Andersson, G. Internetbasierte Psychotherapien: Besonderheiten und empirische Evidenz. Psychother. Psychosom. Med. Psychol. 2009, 59, 159–170. [Google Scholar] [CrossRef]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2020, 26, 377–379. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Raykos, B.C.; Erceg-Hurn, D.M.; Hill, J.; Campbell, B.; McEvoy, P.M. Positive outcomes from integrating telehealth into routine clinical practice for eating disorders during COVID-19. Int. J. Eat. Disord. 2021, 54, 1689–1695. [Google Scholar] [CrossRef]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 12 June 2021).
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Le Grange, D.; et al. COVID-19 and implications for eating disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef]
- Phillipou, A.; Meyer, D.; Neill, E.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Rossell, S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020, 53, 1158–1165. [Google Scholar] [CrossRef] [PubMed]
- Hinojo-Lucena, F.J.; Aznar-Díaz, I.; Cáceres-Reche, M.P.; Trujillo-Torres, J.M.; Romero-Rodríguez, J.M. Problematic Internet Use as a Predictor of Eating Disorders in Students: A Systematic Review and Meta-Analysis Study. Nutrients 2019, 11, 2151. [Google Scholar] [CrossRef]
- Wilksch, S.; O’Shea, A.; Ho, P.; Byrne, S.; Wade, T. The relationship between social media use and disordered eating in young adolescents. Int. J. Eat. Disord. 2019, 53, 96–106. [Google Scholar] [CrossRef]
- Santarossa, S.; Woodruff, S.J. SocialMedia: Exploring the Relationship of Social Networking Sites on Body Image, Self-Esteem, and Eating Disorders. Soc. Media Soc. 2017, 3, 205630511770440. [Google Scholar] [CrossRef]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.Q.; Chen, J.C.; Liu, M.; Chen, X.; Chen, J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Liu, Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020, 289, 113070. [Google Scholar] [CrossRef]
- Stice, E.; Marti, C.N.; Shaw, H.; Jaconis, M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J. Abnorm. Psychol. 2009, 118, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Spettigue, W.; Obeid, N.; Erbach, M.; Feder, S.; Finner, N.; Harrison, M.E.; Isserlin, L.; Robinson, A.; Norris, M.L. The impact of COVID-19 on adolescents with eating disorders: A cohort study. J. Eat. Disord. 2021, 9, 65. [Google Scholar] [CrossRef] [PubMed]
- Graell, M.; Moron-Nozaleda, G.; Camarneiro, R.; Villasenor, A.; Yanez, S.; Munoz, R.; Martinez-Nunez, B.; Miguelez-Fernandez, C.; Munoz, M.; Faya, M. Children and adolescents with eating disorders during COVID-19 confinement: Difficulties and future challenges. Eur. Eat. Disord. Rev. 2020, 28, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.; Touyz, S.W.; Beumont, P.J.; Fairburn, C.G.; Griffiths, R.; Butow, P.; Russell, J.; Schotte, D.E.; Gertler, R.; Basten, C. Comparison of group and individual cognitive-behavioral therapy for patients with bulimia nervosa. Int. J. Eat. Disord. 2003, 33, 241–256. [Google Scholar] [CrossRef]
- Nevonen, L.; Broberg, A.G. A comparison of sequenced individual and group psychotherapy for patients with bulimia nervosa. Int. J. Eat. Disord. 2006, 39, 117–127. [Google Scholar] [CrossRef]
- Agras, W.S.; Walsh, T.; Fairburn, C.G.; Wilson, G.T.; Kraemer, H.C. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Arch. Gen. Psychiatry 2000, 57, 459–466. [Google Scholar] [CrossRef]
- Le Grange, D.; Lock, J.; Agras, W.S.; Bryson, S.W.; Jo, B. Randomized Clinical Trial of Family-Based Treatment and Cognitive-Behavioral Therapy for Adolescent Bulimia Nervosa. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 886–894.e2. [Google Scholar] [CrossRef]
- Lock, J. Adjusting cognitive behavior therapy for adolescents with bulimia nervosa: Results of case series. Am. J. Psychother. 2005, 59, 267–281. [Google Scholar] [CrossRef]
- Le Grange, D.; Crosby, R.D.; Rathouz, P.J.; Leventhal, B.L. A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Arch. Gen. Psychiatry 2007, 64, 1049–1056. [Google Scholar] [CrossRef]
- Nyman-Carlsson, E.; Norring, C.; Engström, I.; Gustafsson, S.A.; Lindberg, K.; Paulson-Karlsson, G.; Nevonen, L. Individual cognitive behavioral therapy and combined family/individual therapy for young adults with Anorexia nervosa: A randomized controlled trial. Psychother. Res. J. Soc. Psychother. Res. 2020, 30, 1011–1025. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Rothwell, E.R. Apps and eating disorders: A systematic clinical appraisal. Int. J. Eat. Disord. 2015, 48, 1038–1046. [Google Scholar] [CrossRef]
- Aardoom, J.J.; Dingemans, A.E.; Van Furth, E.F. E-Health Interventions for Eating Disorders: Emerging Findings, Issues, and Opportunities. Curr. Psychiatry Rep. 2016, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Brede, M.; Ianni, A.; Mentzakis, E. Social interactions in online eating disorder communities: A network perspective. PLoS ONE 2018, 13, e0200800. [Google Scholar] [CrossRef] [PubMed]
- Moghimi, E.; Davis, C.; Rotondi, M. The Efficacy of eHealth Interventions for the Treatment of Adults Diagnosed with Full or Subthreshold Binge Eating Disorder: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e17874. [Google Scholar] [CrossRef]
- Mitchell, J.E.; Crosby, R.D.; Wonderlich, S.A.; Crow, S.; Lancaster, K.; Simonich, H.; Swan-Kremeier, L.; Lysne, C.; Myers, T.C. A randomized trial comparing the efficacy of cognitive-behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav. Res. Ther. 2008, 46, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Ahmadiankalati, M.; Steins-Loeber, S.; Paslakis, G. Review of Randomized Controlled Trials Using e-Health Interventions for Patients with Eating Disorders. Front. Psychiatry 2020, 11, 568. [Google Scholar] [CrossRef]
- Dölemeyer, R.; Tietjen, A.; Kersting, A.; Wagner, B. Internet-based interventions for eating disorders in adults: A systematic review. BMC Psychiatry 2013, 13, 207. [Google Scholar] [CrossRef]
- Aardoom, J.J.; Dingemans, A.E.; Spinhoven, P.; van Ginkel, J.R.; de Rooij, M.; van Furth, E.F. Web-Based Fully Automated Self-Help with Different Levels of Therapist Support for Individuals With Eating Disorder Symptoms: A Randomized Controlled Trial. J. Med. Internet Res. 2016, 18, e159. [Google Scholar] [CrossRef]
- PRISMA Statement. [Online]. Available online: http://prisma-statement.org (accessed on 13 June 2021).
- Heinicke, B.E.; Paxton, S.J.; McLean, S.A.; Wertheim, E.H. Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: A randomized controlled trial. J. Abnorm. Child Psychol. 2007, 35, 379–391. [Google Scholar] [CrossRef]
- Evans, C.; Dolan, B. Body shape questionnaire: Derivation of shortened “alternate forms”. Int. J. Eat. Disord. 1993, 13, 315–321. [Google Scholar] [CrossRef]
- Van Strien, T.; Frijters, J.E.R.; Bergers, G.P.A.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- Paxton, S.J.; Wertheim, E.H.; Gibbons, K.; Szmukler, G.I.; Hillier, L.; Petrovich, J.C. Body image satisfaction, dieting beliefs and weight loss behaviors in adolescent girls and boys. J. Youth Adolesc. 1991, 20, 361–379. [Google Scholar] [CrossRef] [PubMed]
- Garner, D.M.; Olmsted, M.P.; Polivy, J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int. J. Eat. Disord. 1983, 2, 15–34. [Google Scholar] [CrossRef]
- Beck, A.T.; Rial, W.Y.; Rickels, K. Short form of Depression Inventory: Cross-validation. Psychol. Rep. 1974, 34, 1184–1186. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadou, D.; Folkvord, F.; Brugnera, A.; Cañas Vinader, L.; SerranoTroncoso, E.; Carretero Jardí, C.; Linares Bertolin, R.; Muñoz Rodríguez, R.; Martínez Nuñez, B.; Graell Berna, M.; et al. An mHealth intervention for the treatment of patients with an eating disorder: A multicenter randomized controlled trial. Int. J. Eat. Disord. 2020, 53, 1120–1131. [Google Scholar] [CrossRef]
- Peláez-Fernández, M.A.; Javier Labrador, F.; Raich, R.M. Validation of eating disorder examination questionnaire (EDE-Q)–Spanish version– for screening eating disorders. Span. J. Psychol. 2012, 15, 817–824. [Google Scholar] [CrossRef]
- Bauer, S.; Winn, S.; Schmidt, U.; Kordy, H. Construction, scoring and validation of the short evaluation of eating disorders (SEED). Eur. Eat. Disord. Rev. 2005, 13, 191–200. [Google Scholar] [CrossRef]
- Wiebe, J.S.; Penley, J.A. A psychometric comparison of the beck depression inventory-II in English and Spanish. Psychol. Assess. 2005, 17, 481–485. [Google Scholar] [CrossRef]
- Spielberger, C.; Gorsuch, R.; Lushene, R. STAI. In Cuestionario de Ansiedad Estado/Rasgo; Tecnicos Especialistas Asociados (TEA): Madrid, Spain, 1982. (In Spanish) [Google Scholar]
- EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Anderson, K.E.; Byrne, C.E.; Crosby, R.D.; Le Grange, D. Utilizing Telehealth to deliver family-based treatment for adolescent anorexia nervosa. Int. J. Eat. Disord. 2017, 50, 1235–1238. [Google Scholar] [CrossRef]
- Lock, J.; Le Grange, D. Treatment Manual for Anorexia Nervosa: A Family-Based Approach; The Guilford Press: New York, NY, USA, 2000. [Google Scholar]
- Cooper, Z.; Fairburn, C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int. J. Eat. Disord. 1987, 6, 1–8. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Rosenberg, M. Conceiving the Self; Basic Books: New York, NY, USA, 1979. [Google Scholar]
- Lecrubier, Y.; Sheehan, D.V.; Weiller, E.; Amorim, P.; Bonora, I.; Sheehan, K.H.; Janavs, J.; Dunbar, G.C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Jacobi, C.; Hütter, K.; Völker, U.; Möbius, K.; Richter, R.; Trockel, M.; Jones Bell, M.; Lock, J.; Taylor, C.B. Efficacy of a Parent-Based, Indicated Prevention for Anorexia Nervosa: Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e296. [Google Scholar] [CrossRef] [PubMed]
- Paul, T.; Thiel, A. Eating Disorder Inventory-2; Deutsche Version; Hogrefe: Göttingen, Germany, 2004; p. 62. [Google Scholar]
- Altstötter-Gleich, C.; Bergemann, N. Testgüte einer deutschsprachigen Version der Mehrdimensionalen Perfektionismus Skala von Frost, Marten, Lahart und Rosenblate (MPS-F). Diagnostica 2006, 52, 105–118. [Google Scholar] [CrossRef]
- Lock, J.; Le Grange, D. Help Your Teenager Beat an Eating Disorder; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Jacobi, C.; Morris, L.; Beckers, C.; Bronisch-Holtze, J.; Winter, J.; Winzelberg, A.J.; Taylor, C.B. Maintenance of internet-based prevention: A randomized controlled trial. Int. J. Eat. Disord. 2007, 40, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Yaffa, S.; Adi, E.L.; Itai, P.; Marit, J.M.; Doron, G.; Daniel, S. Treatment of eating disorders in adolescents during the COVID-19 pandemic: A case series. J. Eat. Disord. 2021, 9, 17. [Google Scholar] [CrossRef]
- Schmidt, U.; Wade, T.D.; Treasure, J. The Maudsley model of anorexia nervosa treatment for adults (MANTRA): Development, key features, and preliminary evidence. J. Cogn. Psychother. 2014, 28, 48–71. [Google Scholar] [CrossRef]
- Wood, S.M.; White, K.; Peebles, R.; Pickel, J.; Alausa, M.; Mehringer, J.; Dowshen, N. Outcomes of a Rapid Adolescent Telehealth Scale-Up During the COVID-19 Pandemic. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2020, 67, 172–178. [Google Scholar] [CrossRef]
- Crow, S.J.; Mitchell, J.E.; Crosby, R.D.; Swanson, S.A.; Wonderlich, S.; Lancanster, K. The cost effectiveness of cognitive behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav. Res. Ther. 2009, 47, 451.e3. [Google Scholar] [CrossRef]
- Khairat, S.; Haithcoat, T.; Liu, S.; Zaman, T.; Edson, B.; Gianforcaro, R.; Shyu, C.-R. Advancing health equity and access using telemedicine: A geospatial assessment. J. Am. Med. Inform. Assoc. 2019, 26, 796.e805. [Google Scholar] [CrossRef] [PubMed]
- Woo, K.; Dowding, D. Factors Affecting the Acceptance of Telehealth Services by Heart Failure Patients: An Integrative Review. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2018, 24, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Caponnetto, P.; Milazzo, M. Cyber Health Psychology (2019): The use of new technologies at the service of psychologycal well being and health empowerment. Health Psychol. Res. 2019, 7, 8559. [Google Scholar] [CrossRef] [PubMed]
| Authors | Year | Title | Nation | Type of Study | Sample | Measures | Follow Up | Results |
|---|---|---|---|---|---|---|---|---|
| Heinicke, B. E., Paxton, S. J., McLean, S. A., and Wertheim, E. H. | 2007 | Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: a randomized controlled trial. | Australia | Randomized Controlled Trial | 73 | BMI BSQ-SF DEBQ-R EDI-B SATAQ BDI-SF | 2 months 6 months | Significant improvements in measures of body dissatisfaction and symptoms of disordered eating (T2) in the intervention group undergoing CBT-like online sessions. These results were also maintained in the follow-up at 2 and 6 months. |
| Anastasiadou, D., Folkvord, F., Brugnera, A., Cañas Vinader, L., SerranoTroncoso, E., Carretero Jardí, C., Linares Bertolin, R., Muñoz Rodríguez, R., Martínez Nuñez, B., Graell Berna, M., Torralbas-Ortega, J., Torrent-Solà, L., Puntí-Vidal, J., Carrera Ferrer, M., Muñoz Domenjó, A., Diaz Marsa, M., Gunnard, K., Cusido, J., Arcal Cunillera, J., & Lupiañez-Villanueva, F | 2020 | An mHealth intervention for the treatment of patients with an eating disorder: A multicenter randomized controlled trial. | Spain | Randomizes controlled trial | 106 | EDE-Q SEED BDI-II STAI EQ-5D-5L | NO | Significant reductions in primary and secondary outcomes were observed for participants in both groups, with no differences between the experimental and control groups, demonstrating that the combined intervention between CBT and smartphone apps does not provide further improvements in symptoms. |
| Anderson, K. E., Byrne, C. E., Crosby, R. D., and Le Grange, D. | 2017 | Utilizing Telehealth to deliver family-based treatment for adolescent anorexia nervosa. | USA | Clinical trial | 10 | BMI EDE BDI RSE MINI-kid | 6 months | The percentage of mBMI improved significantly from basaline to the end of treatment, and from baseline to FU, with medium-large effect sizes. Reduction in secondary symptoms (depression). |
| Jacobi, C., Hütter, K., Völker, U., Möbius, K., Richter, R., Trockel, M., Jones Bell, M., Lock, J., & Taylor, C. B. | 2018 | Efficacy of a Parent-Based, Indicated Prevention for Anorexia Nervosa: Randomized Controlled Trial | Germany | Randomized controlled trial | 66 Families with high risk’s daughters for AN. | WCS EDI-2 MPS-F EDE PMI | 6 months 12 months | The girls in the intervention group gained significantly more weight, although the size of the effect falls within the medium-small range. Parental participation in prevention intervention was very low |
| Yaffa S. Adi E Itai P. Marit J. Doron G. Daniel S. | 2021 | Treatment of eating disorders in adolescents during the COVID-19 pandemic: a case series | Israel | Case report | 4 patients with ED | NO | The use of multidisciplinary interurban telemedicine treatment resulted in an improvement in the condition in three of the four adolescents living in well-organized families, only one teenager showed no improvement. | |
| Wood M., M.S.H.P MD., White K., M.P.H MD., Peebles R., Pickel MD J., Alausa M., Mehringer J., Dowshen N., M.S.H.P. MD. | 2020 | Outcomes of a Rapid Adolescent Telehealth Scale-Up During the COVID-19 Pandemic | USA | Clinica Trial | 392 | No | In 331 unique patients, with an 82% appointment completion rate. Video visits were conducted for eating disorders (39%), contraception/menstrual disorders (22%), gender-affirming care (17%), general adolescent medicine (15%), HIV treatment (6%), and substance abuse (1%). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maglia, M.; Corello, G.; Caponnetto, P. Evaluation of the Effects of Telepsychotherapy in the Treatment and Prevention of Eating Disorders in Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 12573. https://doi.org/10.3390/ijerph182312573
Maglia M, Corello G, Caponnetto P. Evaluation of the Effects of Telepsychotherapy in the Treatment and Prevention of Eating Disorders in Adolescents. International Journal of Environmental Research and Public Health. 2021; 18(23):12573. https://doi.org/10.3390/ijerph182312573
Chicago/Turabian StyleMaglia, Marilena, Graziana Corello, and Pasquale Caponnetto. 2021. "Evaluation of the Effects of Telepsychotherapy in the Treatment and Prevention of Eating Disorders in Adolescents" International Journal of Environmental Research and Public Health 18, no. 23: 12573. https://doi.org/10.3390/ijerph182312573
APA StyleMaglia, M., Corello, G., & Caponnetto, P. (2021). Evaluation of the Effects of Telepsychotherapy in the Treatment and Prevention of Eating Disorders in Adolescents. International Journal of Environmental Research and Public Health, 18(23), 12573. https://doi.org/10.3390/ijerph182312573







