Distribution and Location Stability of the Australian Ophthalmology Workforce: 2014–2019
Abstract
:1. Introduction
2. Methods
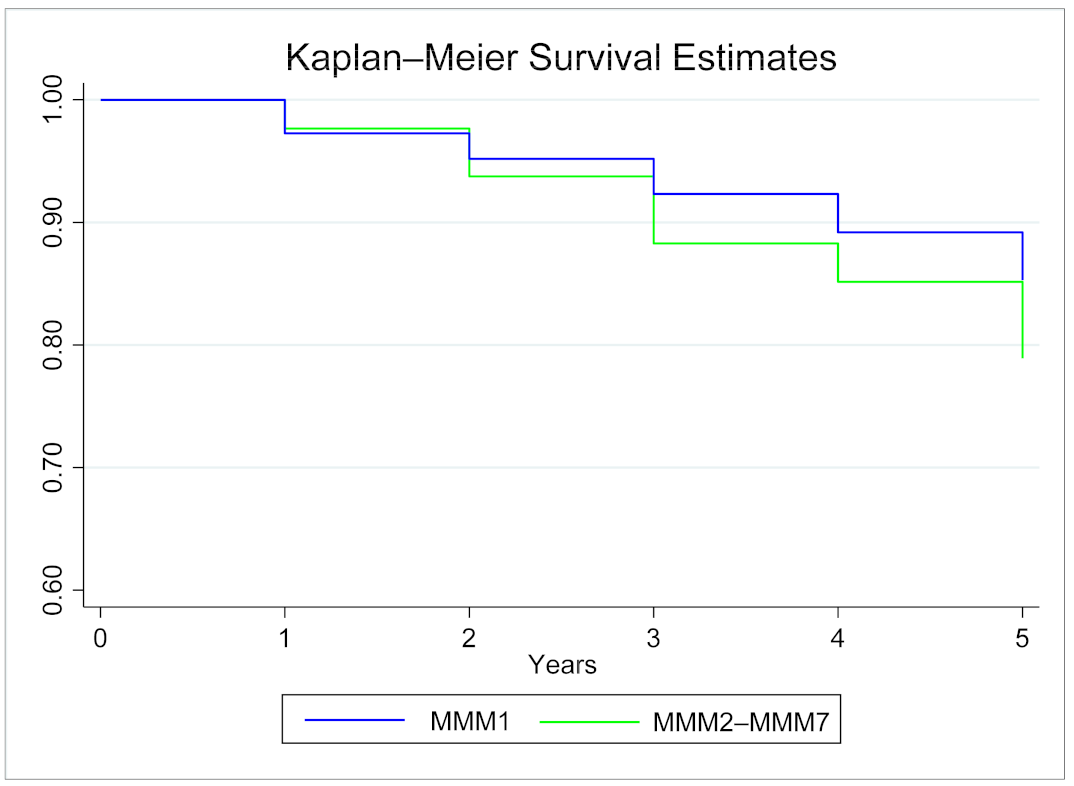
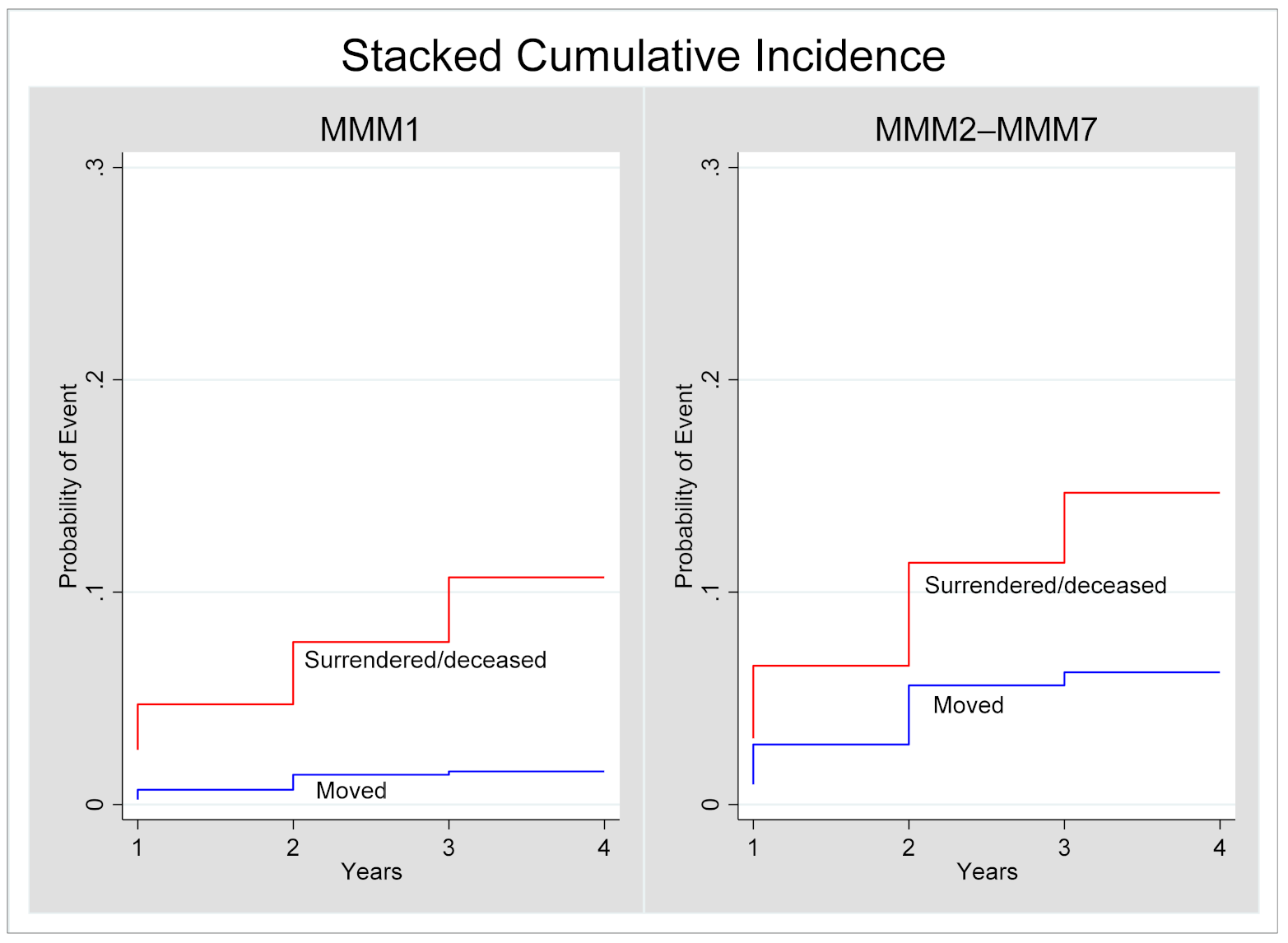
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Glossary
| ABS | Australian Bureau of Statistics |
| ACT | Australian Capital Territory |
| AHPRA | Australian Health Practitioners Regulation Agency |
| MMM | Modified Monash Model |
| NSW | New South Wales |
| NT | Northern Territory |
| PPP | Primary Place of Practice |
| RANZCO | Royal Australian and New Zealand College of Ophthalmologists |
| SA | South Australia |
| STP | Specialist Training Program |
| QLD | Queensland |
| TAS | Tasmania |
| VIC | Victoria |
| WA | Western Australia |
References
- McCarty, C.A.; Fu, C.L.; Taylor, H.R. Epidemiology of pterygium in Victoria, Australia. Br. J. Ophthalmol. 2000, 84, 289–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keel, S.; Xie, J.; Foreman, J.; Van Wijngaarden, P.; Taylor, H.R.; Dirani, M. The prevalence of diabetic retinopathy in Australian adults with self-reported diabetes: The National Eye Health Survey. Ophthalmology 2017, 124, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Keel, S.; McGuiness, M.B.; Foreman, J.; Taylor, H.R.; Dirani, M. The prevalence of visually significant cataract in the Australian National Eye Health Survey. Eye 2019, 33, 957–964. [Google Scholar] [CrossRef]
- Landers, J.; Henderson, T.; Craig, J. Prevalence and associations of cataract in indigenous Australians within central Australia: The Central Australian Ocular Health Study. Clin. Exp. Ophthalmol. 2010, 38, 387–392. [Google Scholar] [CrossRef]
- Brazionis, L.; Jenkins, A.; Keech, A.; Ryan, C.; Brown, A.; Boffa, J.; Bursell, S. The CRE in Diabetic Retinopathy and the TEAMSnet Study Group Diabetic retinopathy in a remote Indigenous primary healthcare population: A Central Australian diabetic retinopathy screening study in the Telehealth Eye and Associated Medical Services Network project. Diabet. Med. 2018, 35, 630–639. [Google Scholar] [CrossRef]
- Foreman, J.; Xie, J.; Keel, S.; van Wijngaarden, P.; Sandhu, S.S.; Ang, G.S.; Gaskin, J.F.; Crowston, J.; Bourne, R.; Taylor, H.R.; et al. The prevalence and causes of vision loss in Indigenous and non-Indigenous Australians: The National eye health survey. Ophthalmology 2017, 124, 1743–1752. [Google Scholar] [CrossRef] [Green Version]
- Keel, S.; Foreman, J.; Xie, J.; Taylor, H.R.; Dirani, M. Prevalence and associations of presenting near-vision impairment in the Australian National Eye Health Survey. Eye 2018, 32, 506–514. [Google Scholar] [CrossRef]
- Taylor, H.R.; Xie, J.; Fox, S.; Dunn, R.A.; Arnold, A.L.; Keeffe, J.E. The prevalence and causes of vision loss in Indigenous Australians: The National Indigenous Eye Health Survey. Med. J. Aust. 2010, 192, 312–318. [Google Scholar] [CrossRef] [Green Version]
- Kelaher, M.; Ferdinand, A.; Taylor, H. Access to eye health services among indigenous Australians: An area level analysis. BMC Ophthalmol. 2012, 12, 51. [Google Scholar] [CrossRef] [Green Version]
- Boudville, A.I.; Anjou, M.D.; Taylor, H.R. Improving eye care for Indigenous Australians in primary health care settings. Aust. J. Rural Health 2013, 21, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Australia’s Future Health Workforce—Ophthalmology; Department of Health: Canberra, Australia, 2018. [Google Scholar]
- Gruen, R.L.; Weeramanthri, T.S.; Bailie, R. Outreach and improved access to specialist services for indigenous people in remote Australia: The requirements for sustainability. J. Epidemiol. Community Health 2002, 56, 517–521. [Google Scholar] [CrossRef]
- Glasson, N.M.; Crossland, L.J.; Larkins, S. An Innovative Australian Outreach Model of Diabetic Retinopathy Screening in Remote Communities. J. Diabetes Res. 2016, 2016, 1267215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Connor, P.M.; Harper, C.A.; Brunton, C.L.; Clews, S.J.; Haymes, S.A.; Keeffe, J.E. Shared care for chronic eye diseases: Perspectives of ophthalmologists, optometrists and patients. Med. J. Aust. 2012, 196, 646–650. [Google Scholar] [CrossRef] [Green Version]
- Australian Government Department of Health. Modified Monash Model. Available online: https://www.health.gov.au/health-topics/health-workforce/health-workforce-classifications/modified-monash-model (accessed on 17 June 2021).
- Canadian Institute for Health Information. Supply, Distribution and Migration of Canadian Physicians; Canadian Institute for Health Information: Ottawa, ON, Canada, 2012. [Google Scholar]
- Karan, A.; Negandhi, H.; Hussain, S.; Zapata, T.; Mairembam, D.; De Graeve, H.; Buchan, J.; Zodpey, S. Size, composition and distribution of health workforce in India: Why, and where to invest? Hum. Resour. Health 2021, 19, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Barreto, T.; Jetty, A.; Eden, A.R.; Petterson, S.; Bazemore, A.; Peterson, L.E. Distribution of Physician Specialties by Rurality. J. Rural Health 2021, 37, 714–722. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Modified Monash Model Fact Sheet. Available online: https://www.health.gov.au/resources/publications/modified-monash-model-fact-sheet (accessed on 23 November 2021).
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496. [Google Scholar] [CrossRef]
- Feng, P.W.; Ahluwalia, A.; Feng, H.; Adelman, R.A. National Trends in the United States Eye Care Workforce from 1995 to 2017. Am. J. Ophthalmol. 2020, 218, 128–135. [Google Scholar] [CrossRef]
- Department of Health. Factsheet, Allied Health 2019. Canberra: Department of Health. 2019. Available online: https://hwd.health.gov.au/resources/publications/factsheet-alld-2019.html (accessed on 28 April 2021).
- Chapman, N.A.; Anstice, N.S.; Jacobs, R.J. Geographic distribution of eye-care practitioners in Aotearoa/New Zealand: Implications for future eye health workforce. Clin. Exp. Optometry 2020, 103, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Keefe, J.E.; Weih, L.A.M.; McCarthy, C.; Taylor, H.R. Utilisation of eye care services by urban and rural Australians. Br. J. Ophthalmol. 2002, 86, 24–27. [Google Scholar] [CrossRef]
- Lo, T.C.S.; Rogers, S.L.; Hall, A.J.; Lim, L. Differences in practice of ophthalmology by gender in Australia. Clin. Exp. Ophthalmol. 2019, 47, 840–846. [Google Scholar] [CrossRef] [PubMed]
- May, J.; Walker, J.; McGrail, M.; Rolley, F. It’s more than money: Policy options to secure medical specialist workforce for regional centres. Aust. Health Rev. 2017, 41, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.; May, J.; Pegram, R.; Shires, L. ‘It’s mostly about the job’—Putting the lens on specialist rural retention. Rural. Remote Health 2020, 20, 5299. [Google Scholar] [CrossRef]
- Centre for Rural Health and RANZCO. Specialist Training Program Evaluation: Ophthalmology; University of Tasmania: Launceston, Australia, 2021. [Google Scholar]
| Characteristic | n = 948 (%) |
|---|---|
| Sex | |
| Male | 767 (80.9) |
| Female | 181 (19.1) |
| Years since primary qualification (median, IQR) | 35 (25, 44) |
| Country of primary qualification | |
| Australia | 746 (78.7) |
| United Kingdom | 62 (6.5) |
| India | 36 (3.8) |
| South Africa | 32 (3.4) |
| New Zealand | 29 (3.1) |
| Other | 22 (2.3) |
| Unknown | 21 (2.2) |
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|
| State | ||||||
| NSW | 340 (35.9) | 335 (35.3) | 333 (35.1) | 325 (34.3) | 314 (33.1) | 325 (34.3) |
| VIC | 219 (23.1) | 219 (23.1) | 218 (23.0) | 217 (22.9) | 212 (22.4) | 213 (22.5) |
| QLD | 163 (17.2) | 156 (16.5) | 154 (16.2) | 153 (16.1) | 144 (15.2) | 152 (16.0) |
| WA | 71 (7.5) | 73 (7.7) | 68 (7.2) | 66 (7.0) | 66 (7.0) | 70 (7.4) |
| SA | 68 (7.2) | 66 (7.0) | 64 (6.8) | 59 (6.2) | 55 (5.8) | 55 (5.8) |
| TAS | 17 (1.8) | 16 (1.7) | 16 (1.7) | 18 (1.9) | 16 (1.7) | 20 (2.1) |
| ACT | 13 (1.4) | 13 (1.4) | 13 (1.4) | 12 (1.3) | 12 (1.3) | 14 (1.5) |
| NT | 5 (0.5) | 5 (0.5) | 4 (0.4) | 4 (0.4) | 4 (0.4) | 6 (0.6) |
| MMM Category | ||||||
| MMM1 | 768 (81.0) | 757 (79.9) | 744 (78.5) | 723 (76.3) | 698 (73.6) | 721 (75.9) |
| MMM2 | 64 (6.8) | 63 (6.6) | 63 (6.6) | 69 (7.3) | 66 (7.0) | 76 (8.0) |
| MMM3 | 55 (5.8) | 54 (5.7) | 54 (5.7) | 52 (5.5) | 51 (5.4) | 52 (5.5) |
| MMM4 | † | † | † | 5 (0.5) | 6 (0.6) | 5 (0.5) |
| MMM5 | † | † | † | † | † | † |
| MMM6 | † | † | † | † | 0 | † |
| MMM7 | 0 | 0 | 0 | 0 | 0 | 0 |
| Missing | 52 (5.5) | 65 (6.9) | 78 (8.2) | 94 (9.9) | 125 (13.2) | 93 (9.8) |
| Stayed MMM1 (n = 655) | Stayed MMM2–MMM7 (n = 105) | |
|---|---|---|
| Sex | ||
| Male (n = 767) | 514 (78.5) | 95 (90.5) |
| Female (n = 181) | 141 (21.5) | 10 (9.5) |
| Years since primary qualification | ||
| 11–20 years (n = 87) | 64 (9.9) | † |
| 21–30 years (n = 276) | 215 (33.2) | 30 (28.8) |
| 31–40 years (n = 260) | 189 (29.2) | 51 (49.0) |
| 41–50 years (n = 192) | 126 (19.5) | 17 (16.3) |
| >50 years (n = 122) | 53 (8.2) | † |
| Country of primary qualification | ||
| Australia, NZ (n = 775) | 549 (85.8) | 81 (79.4) |
| Other (n = 152) | 91 (14.2) | 21 (20.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allen, P.; Jessup, B.; Khanal, S.; Baker-Smith, V.; Obamiro, K.; Barnett, T. Distribution and Location Stability of the Australian Ophthalmology Workforce: 2014–2019. Int. J. Environ. Res. Public Health 2021, 18, 12574. https://doi.org/10.3390/ijerph182312574
Allen P, Jessup B, Khanal S, Baker-Smith V, Obamiro K, Barnett T. Distribution and Location Stability of the Australian Ophthalmology Workforce: 2014–2019. International Journal of Environmental Research and Public Health. 2021; 18(23):12574. https://doi.org/10.3390/ijerph182312574
Chicago/Turabian StyleAllen, Penny, Belinda Jessup, Santosh Khanal, Victoria Baker-Smith, Kehinde Obamiro, and Tony Barnett. 2021. "Distribution and Location Stability of the Australian Ophthalmology Workforce: 2014–2019" International Journal of Environmental Research and Public Health 18, no. 23: 12574. https://doi.org/10.3390/ijerph182312574
APA StyleAllen, P., Jessup, B., Khanal, S., Baker-Smith, V., Obamiro, K., & Barnett, T. (2021). Distribution and Location Stability of the Australian Ophthalmology Workforce: 2014–2019. International Journal of Environmental Research and Public Health, 18(23), 12574. https://doi.org/10.3390/ijerph182312574






