Effect of Physical Activity on Cardiovascular Event Risk in a Population-Based Cohort of Patients with Type 2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Exposure
2.3. Outcomes
2.4. Confounders
2.5. Statistical Analysis
2.5.1. Cohort Design
2.5.2. Nested Case–Control Design
2.5.3. Complementary Analyses
3. Results
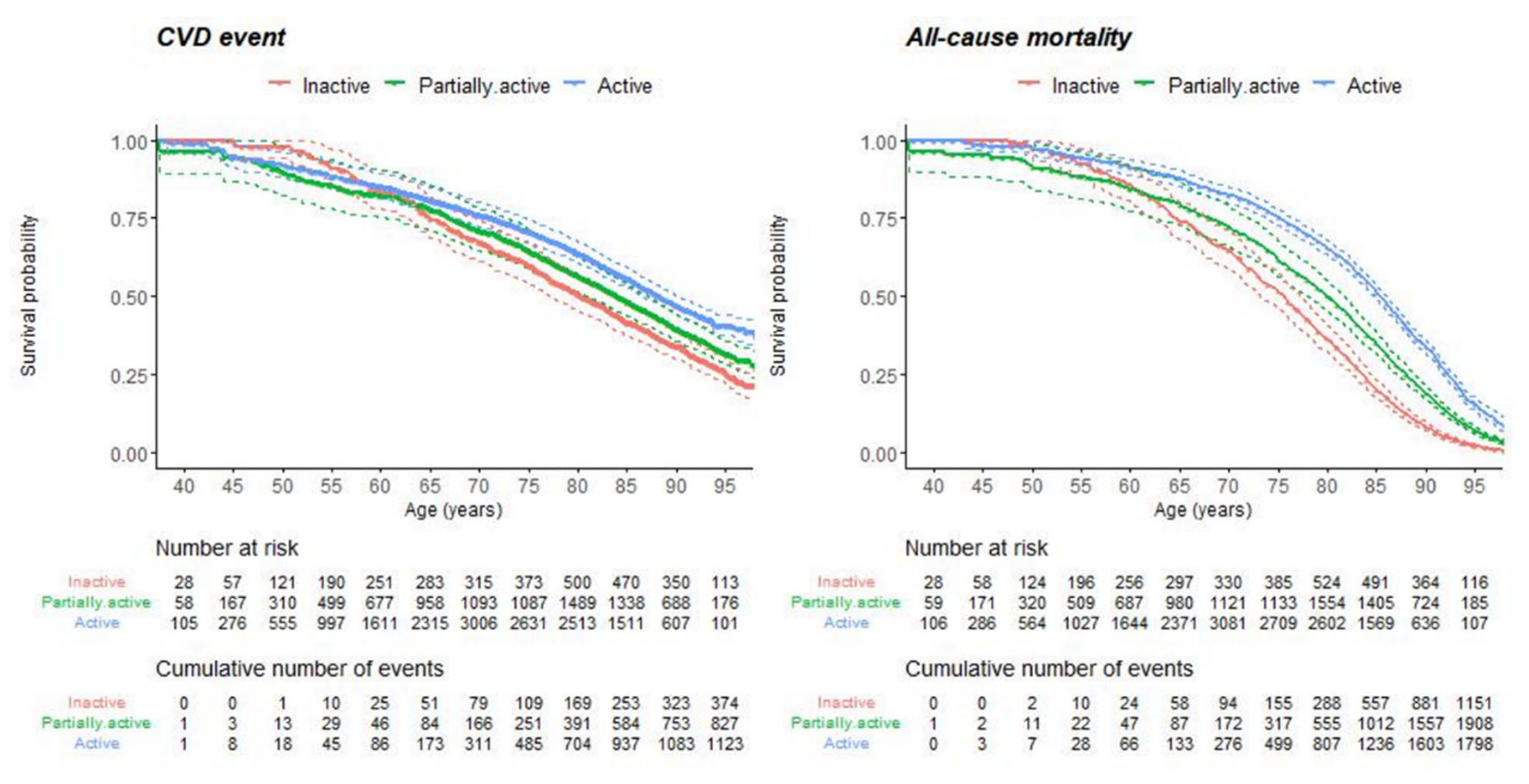
3.1. Cohort Design Results
3.2. Nested Case–Control Analysis Results
3.3. Complementary Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef]
- Lear, S.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Li, J.; Siegrist, J. Physical Activity and Risk of Cardiovascular Disease—A Meta-Analysis of Prospective Cohort Studies. Int. J. Environ. Res. Public Health 2012, 9, 391–407. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Brown, W.J.; Steene-Johannessen, J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.E.; Lee, I.-M. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850,060 participants. Br. J. Sports Med. 2019, 53, 886–894. [Google Scholar] [CrossRef]
- Chamnan, P.; Simmons, R.K.; Sharp, S.J.; Griffin, S.J.; Wareham, N.J. Cardiovascular risk assessment scores for people with diabetes: A systematic review. Diabetologia 2009, 52, 2001–2014. [Google Scholar] [CrossRef] [PubMed]
- Van Dieren, S.; Beulens, J.W.J.; Kengne, A.P.; Peelen, L.M.; Rutten, G.E.H.M.; Woodward, M.; van der Schouw, Y.; Moons, K.G.M. Prediction models for the risk of cardiovascular disease in patients with type 2 diabetes: A systematic review. BMJ J. Heart 2011, 98, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.; Cai, X.; Schumann, U.; Velders, M.; Sun, Z.; Steinacker, J.M. Impact of Walking on Glycemic Control and Other Cardiovascular Risk Factors in Type 2 Diabetes: A Meta-Analysis. PLoS ONE 2014, 9, e109767. [Google Scholar] [CrossRef] [PubMed]
- Pan, B.; Ge, L.; Xun, Y.-Q.; Chen, Y.-J.; Gao, C.-Y.; Han, X.; Zuo, L.-Q.; Shan, H.-Q.; Yang, K.-H.; Ding, G.-W.; et al. Exercise training modalities in patients with type 2 diabetes mellitus: A systematic review and network meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 72. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Elliott, E.; Naughton, G. Exercise for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2006, 19, CD002968. [Google Scholar] [CrossRef]
- Yang, Z.; Scott, C.A.; Mao, C.; Tang, J.; Farmer, A.J. Resistance Exercise Versus Aerobic Exercise for Type 2 Diabetes: A Systematic Review and Meta-Analysis. Sports Med. 2014, 44, 487–499. [Google Scholar] [CrossRef]
- Picard, M.; Tauveron, I.; Magdasy, S.; Benichou, T.; Bagheri, R.; Ugbolue, U.C.; Navel, V.; Dutheil, F. Effect of exercise training on heart rate variability in type 2 diabetes mellitus patients: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251863. [Google Scholar] [CrossRef]
- Chu, P.; Gotink, R.; Yeh, G.Y.; Goldie, S.J.; Hunink, M.G.M. The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Prev. Cardiol. 2016, 23, 291–307. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.Z.A.; Karam, J.A.; Zeb, A.; Ullah, R.; Shah, A.; Haq, I.U.; Ali, I.; Darain, H.; Chen, H. Movement is Improvement: The Therapeutic Effects of Exercise and General Physical Activity on Glycemic Control in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Diabetes Ther. 2021, 12, 707–732. [Google Scholar] [CrossRef] [PubMed]
- Miele, E.M.; Headley, S.A.E. The Effects of Chronic Aerobic Exercise on Cardiovascular Risk Factors in Persons with Diabetes Mellitus. Curr. Diabetes Rep. 2017, 17, 97. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Schlesinger, S.; Leitzmann, M.F.; Tonstad, S.; Norat, T.; Riboli, E.; Vatten, L.J. Physical activity and the risk of heart failure: A systematic review and dose–response meta-analysis of prospective studies. Eur. J. Epidemiol. 2021, 36, 367–381. [Google Scholar] [CrossRef]
- Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.-M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; Rosengren, A.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Kaizu, S.; Kishimoto, H.; Iwase, M.; Fujii, H.; Ohkuma, T.; Ide, H.; Jodai, T.; Kikuchi, Y.; Idewaki, Y.; Hirakawa, Y.; et al. Impact of Leisure-Time Physical Activity on Glycemic Control and Cardiovascular Risk Factors in Japanese Patients with Type 2 Diabetes Mellitus: The Fukuoka Diabetes Registry. PLoS ONE 2014, 9, e98768. [Google Scholar] [CrossRef] [PubMed]
- Sluik, D.; Buijsse, B.; Muckelbauer, R.; Kaaks, R.; Teucher, B.; Johnsen, N.F.; Tjonneland, A.; Overvad, K.; Østergaard, J.N.; Amiano, P.; et al. Physical Activity and Mortality in Individuals with Diabetes Mellitus. Arch. Intern. Med. 2012, 172, 1285–1295. [Google Scholar] [CrossRef] [PubMed]
- Galbete, A.; Tamayo, I.; Librero, J.; Enguita-Germán, M.; Cambra, K.; Ibáñez-Beroiz, B. Cardiovascular risk in patients with type 2 diabetes: A systematic review of prediction models. Diabetes Res. Clin. Pract. 2021, 2021, 109089. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Action Plan on Physical Activity 2018–2030; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Cambra, K.; Galbete, A.; Forga, L.; Lecea, O.; Ariz, M.J.; Moreno-Iribas, C.; Aizpuru, F.; Ibañez, B. Sex and age differences in the achievement of control targets in patients with type 2 diabetes: Results from a population-based study in a South European region. BMC Fam. Pract. 2016, 17, 144. [Google Scholar] [CrossRef]
- Read, S.H.; van Diepen, M.; Colhoun, H.M.; Halbesma, N.; Lindsay, R.S.; McKnight, J.A.; McAllister, D.A.; Pearson, E.R.; Petrie, J.R.; Philip, S.; et al. Performance of Cardiovascular Disease Risk Scores in People Diagnosed with Type 2 Diabetes: External Validation Using Data from the National Scottish Diabetes Register. Diabetes Care 2018, 41, 2010–2018. [Google Scholar] [CrossRef]
- Berkman, L.F.; Leo-Summers, L.; Horwitz, R.I. Emotional Support and Survival after Myocardial Infarction. Ann. Intern. Med. 1992, 117, 1003–1009. [Google Scholar] [CrossRef]
- Abellán van Kan, G.; Abizanda Soler, P.; Alastuey Giménez, C.; Albó Poquí, A.; Alfaro Acha, A.; Alonso Álvarez, M.; Alonso Renedo, J.; Álvarez Martín, A.; Álvarez Nebreda, L.; Amblàs Novellas, J.; et al. Tratado de Geriatría para Residentes; Sociedad Española de Geriatría y Gerontología (SEGG): Madrid, Spain, 2018; Volume 30, pp. 313–323. Available online: https://www.anme.com.mx/libros/Tratado%20de%20Geriatr%EDa%20para%20Residentes.pdf (accessed on 8 November 2021).
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef] [PubMed]
- Canchola, A.J.; Stewart, S.L.; Bernstein, L.; West, D.W.; Ross, R.K.; Deapen, D.; Pinder, R.; Reynolds, P.; Wright, W.; Anton-Culver, H.; et al. Cox Regression Using Different Time-Scales. Available online: https://www.lexjansen.com/wuss/2003/DataAnalysis/i-cox_time_scales.pdf (accessed on 8 November 2021).
- Andersen, K.; Mariosa, D.; Adami, H.-O.; Held, C.; Ingelsson, E.; Lagerros, Y.T.; Nyren, O.; Ye, W.; Bellocco, R.; Sundström, J. Dose–Response Relationship of Total and Leisure Time Physical Activity to Risk of Heart Failure. Circ. Hearth Fail. 2014, 7, 701–708. [Google Scholar] [CrossRef]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liśkiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’. Int. J. Epidemiol. 2017, 45, 1887–1894. [Google Scholar] [CrossRef]
- Amini, H.; Habibi, S.; Islamoglu, A.H.; Isanejad, E.; Uz, C.; Daniyari, H. COVID-19 pandemic-induced physical inactivity: The necessity of updating the Global Action Plan on Physical Activity 2018–2030. Environ. Health Prev. Med. 2021, 26, 32. [Google Scholar] [CrossRef]
- Kim, M.-K.; Han, K.; Cho, J.-H.; Kwon, H.-S.; Yoon, K.-H.; Lee, S.-H. A model to predict risk of stroke in middle-aged adults with type 2 diabetes generated from a nationwide population-based cohort study in Korea. Diabetes Res. Clin. Pract. 2020, 163, 108157. [Google Scholar] [CrossRef] [PubMed]
- Brotons, C.; Moral, I.; Fernández, D.; Puig, M.; Bonacho, E.C.; Muñoz, P.M.; Romero, C.C.; Aguado, L.J.Q. Estimación del riesgo cardiovascular de por vida (IBERLIFERISK): Una herramienta nueva en prevención primaria de las enfermedades cardiovasculares. Revista Española de Cardiología 2019, 72, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Honda, T.; Chen, S.; Hata, J.; Yoshida, D.; Hirakawa, Y.; Furuta, Y.; Shibata, M.; Sakata, S.; Kitazono, T.; Ninomiya, T. Development and Validation of a Risk Prediction Model for Atherosclerotic Cardiovascular Disease in Japanese Adults: The Hisayama Study. J. Atheroscler. Thromb. 2021, 61960. [Google Scholar] [CrossRef]
- Manuel, D.G.; Tuna, M.; Bennett, C.; Hennessy, D.; Rosella, L.; Sanmartin, C.; Tu, J.V.; Perez, R.; Fisher, S.; Taljaard, M. Development and validation of a cardiovascular disease risk-prediction model using population health surveys: The Cardiovascular Disease Population Risk Tool (CVDPoRT). Can. Med. Assoc. J. 2018, 190, 871–882. [Google Scholar] [CrossRef] [PubMed]
- Nobel, L.; Mayo, N.E.; Hanley, J.; Nadeau, L.; Daskalopoulou, S.S. MyRisk_Stroke Calculator: A Personalized Stroke Risk Assessment Tool for the General Population. J. Clin. Neurol. 2014, 10, 1–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Artigao-Ródenas, L.M.; Carbayo-Herencia, J.A.; Palazón-Bru, A.; Garrote, J.A.D.; Sanchis-Domènech, C.; Aguiar, I.V.; Gil-Guillén, V.F. Construction and Validation of a 14-Year Cardiovascular Risk Score for Use in the General Population. Medicine 2015, 94, e1980. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Variable | Total n (%) | Levels | Inactive | Partially Active | Active |
|---|---|---|---|---|---|
| Total n (%) | 26,587 (100.0) | 3362 (12.6) | 8371 (31.5) | 14,854 (55.9) | |
| Age | 26,587 (100.0) | Mean (SD) | 74.1 (13.5) | 72.1 (12.5) | 68.7 (11.1) |
| Sex | 26,587 (100.0) | Male | 1431 (42.6) | 3966 (47.4) | 9207 (62.0) |
| Female | 1931 (57.4) | 4405 (52.6) | 5647 (38.0) | ||
| BMI | 19,753 (74.3) | Mean (SD) | 32.9 (7.3) | 31.2 (6.0) | 29.8 (5.2) |
| Smoking status | 25,395 (95.5) | Non-smoker | 2162 (67.4) | 5147 (64.1) | 7981 (56.4) |
| Ex-smoker | 515 (16.0) | 1614 (20.1) | 3774 (26.7) | ||
| Smoker | 533 (16.6) | 1266 (15.8) | 2403 (17.0) | ||
| Alcohol | 24,843 (93.4) | No | 2322 (75.1) | 5547 (70.6) | 8740 (62.9) |
| Yes | 770 (24.9) | 2308 (29.4) | 5156 (37.1) | ||
| Duration T2D | 26,587 (100.0) | Median(IQR) | 7.7 (4.4–11.9) | 7.6 (4.1–11.6) | 7.1 (3.8–10.8) |
| Education | 26,083 (98.1) | No | 1418 (43.0) | 3170 (38.6) | 4737 (32.5) |
| Level | Primary School | 1553 (47.1) | 4179 (50.9) | 7952 (54.5) | |
| High School | 203 (6.2) | 575 (7.0) | 1287 (8.8) | ||
| University level | 123 (3.7) | 284 (3.5) | 602 (4.1) | ||
| HDL | 20,354 (76.6) | Mean (SD) | 46.2 (13.7) | 48.8 (13.9) | 49.8 (14.1) |
| LDL | 19,896 (74.8) | Mean (SD) | 108.4 (33.6) | 110.2 (32.3) | 110.7 (30.9) |
| TGC | 20,231 (76.1) | Median (IQR) | 135.0 (98–186) | 130.0 (95–179) | 120.0 (87–167) |
| SBP | 23,558 (88.6) | Mean (SD) | 75.4 (11.4) | 75.8 (10.5) | 76.4 (10.2) |
| DBP | 23,560 (88.6) | Mean (SD) | 135.4 (18.3) | 136.4 (17.8) | 135.4 (16.5) |
| HTA treatment | 26,587 (100.0) | No | 1419 (42.2) | 3612 (43.1) | 5649 (38.0) |
| Yes | 1943 (57.8) | 4759 (56.9) | 9205 (62.0) | ||
| HTA | 26,587 (100.0) | No | 1308 (38.9) | 3014 (36.0) | 6060 (40.8) |
| Yes | 2054 (61.1) | 5357 (64.0) | 8794 (59.2) | ||
| Albumin/creatinine | 16,225 (61.0) | Median (IQR) | 9.6 (4.0–30.1) | 8.0 (3.9–23.0) | 6.0 (3.0–14.9) |
| Total Chol | 21,713 (81.7) | Median (IQR) | 182.0(155–210) | 186.0 (161–212) | 185.0 (162–210) |
| Cardiac freq. | 20,441 (76.9) | Mean (SD) | 74.0 (66.0–82.0) | 72.0 (65.0–80.0) | 72.0 (64.0–80.0) |
| HbA1c | 18,553 (69.8) | Median (IQR) | 6.8 (6.2–7.9) | 6.8 (6.2–7.7) | 6.7 (6.1–7.5) |
| History of CVD | 26,587 (100.0) | No | 2178 (64.8) | 6053 (72.3) | 11,783 (79.3) |
| Yes | 1184 (35.2) | 2318 (27.7) | 3071 (20.7) | ||
| aCharlson | 26,587 (100.0) | 1–2 | 1739 (51.7) | 4760 (56.9) | 9427 (63.5) |
| 3–4 | 1243 (37.0) | 2879 (34.4) | 4576 (30.8) | ||
| 5–8 | 355 (10.6) | 674 (8.1) | 796 (5.4) |
| Models | Units | CVD | Mortality |
|---|---|---|---|
| 1 Model 1 | Inactive | Ref. | Ref. |
| Partially active | 0.81 (0.72–0.92, p = 0.001) | 0.65 (0.61–0.70, p < 0.001) | |
| Active | 0.65 (0.58–0.73, p < 0.001) | 0.44 (0.41–0.47, p < 0.001) | |
| 2 Model 2 | Inactive | Ref. | Ref. |
| Partially active | 0.88 (0.78–1.00, p = 0.043) | 0.67 (0.63–0.72, p < 0.001) | |
| Active | 0.74 (0.65–0.83, p < 0.001) | 0.45 (0.42–0.49, p < 0.001) | |
| 3 Model 3 | Inactive | Ref. | Ref. |
| Partially active | 0.87 (0.74–1.03, p = 0.097) | 0.75 (0.67–0.83, p < 0.001) | |
| Active | 0.72 (0.61–0.84, p < 0.001) | 0.51 (0.46–0.57, p < 0.001) |
| CVD | All-Cause Mortality | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Levels | Controls | Cases | p-Value δ | Controls | Cases | p-Value δ |
| Total n (%) | 4032 (65.7) | 2104 (34.3) | 8727 (65.6) | 4583 (34.4) | |||
| Age | Mean (SD) | 75.0 (9.9) | 75.0 (10.1) | 0.890 | 79.4 (9.0) | 79.5 (9.1) | 0.474 |
| Sex | Male | 2402 (59.6) | 1255 (59.6) | 0.977 | 4685 (53.7) | 2469 (53.9) | 0.850 |
| Female | 1630 (40.4) | 849 (40.4) | 4042 (46.3) | 2114 (46.1) | |||
| Education | No | 1632 (40.5) | 847 (40.3) | 0.505 | 4133 (47.4) | 2161 (47.2) | 0.300 |
| Level | Primary School | 2171 (53.8) | 1123 (53.4) | 4268 (48.9) | 2218 (48.4) | ||
| High School | 176 (4.4) | 101 (4.8) | 210 (2.4) | 131 (2.9) | |||
| University | 53 (1.3) | 33 (1.6) | 116 (1.3) | 73 (1.6) | |||
| Duration T2D | Median (IQR) | 8.0 (5.0–12.0) | 9.0 (6.0 to 12.0) | 0.219 | 9.0 (6.0–13.0) | 9.0 (6.0–13.0) | 0.468 |
| History of CVD | No | 2195 (54.4) | 1128 (53.6) | 0.555 | 5063 (58.0) | 2621 (57.2) | 0.369 |
| Yes | 1837 (45.6) | 976 (46.4) | 3664 (42.0) | 1962 (42.8) | |||
| Smoking | Non-smoker | 2368 (61.3) | 1197 (59.9) | 0.001 | 5767 (68.4) | 2884 (66.0) | <0.001 |
| Ex-smoker | 1009 (26.1) | 481 (24.1) | 1894 (22.5) | 968 (22.1) | |||
| Smoker | 489 (12.6) | 319 (16.0) | 767 (9.1) | 519 (11.9) | |||
| Alcohol | No | 2533 (66.3) | 1361 (68.4) | 0.116 | 5882 (71.0) | 3174 (73.7) | 0.002 |
| Yes | 1285 (33.7) | 628 (31.6) | 2402 (29.0) | 1133 (26.3) | |||
| BMI | Mean (SD) | 30.2 (5.5) | 29.9 (5.1) | 0.086 | 29.6 (5.4) | 29.4 (6.0) | 0.108 |
| HTA | No | 901 (22.3) | 413 (19.6) | 0.015 | 1790 (20.5) | 1075 (23.5) | <0.001 |
| Yes | 3131 (77.7) | 1691 (80.4) | 6937 (79.5) | 3508 (76.5) | |||
| aCharlson | 1–2 | 1569 (38.9) | 803 (38.2) | 0.286 | 2848 (32.6) | 1473 (32.1) | 0.174 |
| 3–4 | 1856 (46.0) | 957 (45.5) | 4616 (52.9) | 2393 (52.2) | |||
| 5–6 | 607 (15.1) | 344 (16.3) | 1263 (14.5) | 717 (15.6) | |||
| PA | Inactive | 518 (12.8) | 340 (16.2) | <0.001 | 1336 (15.3) | 1128 (24.6) | <0.001 |
| Partially active | 1376 (34.1) | 749 (35.6) | 3174 (36.4) | 1779 (38.8) | |||
| Active | 2138 (53.0) | 1015 (48.2) | 4217 (48.3) | 1676 (36.6) | |||
| Models | Units | CVD | Mortality |
|---|---|---|---|
| 1 Model 1 | Inactive | Ref. | Ref. |
| Partially active | 0.84 (0.71–0.99, p = 0.033) | 0.65 (0.58–0.71, p < 0.001) | |
| Active | 0.72 (0.61–0.84, p < 0.001) | 0.43 (0.39–0.48, p < 0.001) | |
| 2 Model 2 | Inactive | Ref. | Ref. |
| Partially active | 0.84 (0.66–1.07, p = 0.160) | 0.72 (0.61–0.85, p < 0.001) | |
| Active | 0.71 (0.56–0.91, p < 0.008) | 0.50 (0.42–0.59, p < 0.001) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Enguita-Germán, M.; Tamayo, I.; Galbete, A.; Librero, J.; Cambra, K.; Ibáñez-Beroiz, B. Effect of Physical Activity on Cardiovascular Event Risk in a Population-Based Cohort of Patients with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2021, 18, 12370. https://doi.org/10.3390/ijerph182312370
Enguita-Germán M, Tamayo I, Galbete A, Librero J, Cambra K, Ibáñez-Beroiz B. Effect of Physical Activity on Cardiovascular Event Risk in a Population-Based Cohort of Patients with Type 2 Diabetes. International Journal of Environmental Research and Public Health. 2021; 18(23):12370. https://doi.org/10.3390/ijerph182312370
Chicago/Turabian StyleEnguita-Germán, Mónica, Ibai Tamayo, Arkaitz Galbete, Julián Librero, Koldo Cambra, and Berta Ibáñez-Beroiz. 2021. "Effect of Physical Activity on Cardiovascular Event Risk in a Population-Based Cohort of Patients with Type 2 Diabetes" International Journal of Environmental Research and Public Health 18, no. 23: 12370. https://doi.org/10.3390/ijerph182312370
APA StyleEnguita-Germán, M., Tamayo, I., Galbete, A., Librero, J., Cambra, K., & Ibáñez-Beroiz, B. (2021). Effect of Physical Activity on Cardiovascular Event Risk in a Population-Based Cohort of Patients with Type 2 Diabetes. International Journal of Environmental Research and Public Health, 18(23), 12370. https://doi.org/10.3390/ijerph182312370






